Abstract
This article discusses changes in the way hematopoietic stem cell allotransplants may be carried out in the future to treat patients with malignant hematological diseases. Specifically, the focus has shifted away from attempts at eradicating underlying diseases through toxic high-dose chemoradiation therapy towards using the stem cell donor's immune cells for that purpose (allogeneic graft-versus-tumor effect).
The non-myeloablative transplant approaches hold promise in reducing the morbidity and mortality associated with conventional high-dose chemoradiation therapy, and they allow allogeneic transplants in elderly or medically infirm patients who are at present not candidates for transplantation. In the future, specific graft-versus-tumor responses may become possible by eliciting donor T cell responses to tumor-associated minor histocompatibility antigens.
In Section I, Dr. Rainer Storb describes experimental studies in random-bred dogs that rely on non-cytotoxic immunosuppressive agents to establish stable allografts. Powerful postgrafting immunosuppression, traditionally directed at preventing graft-versus-host disease (GVHD), is also used to overcome host-versus-graft (HVG) reactions, thereby dramatically reducing the need for intensive immunosuppressive conditioning programs. Preclinical canine studies have been translated into the clinical setting for treatment of elderly or medically infirm patients with malignant hematological diseases. The pretransplant conditioning has been reduced to a single dose of 2 Gy total body irradiation (TBI) with or without fludarabine. The lack of toxicity makes it possible for transplants to be conducted in the outpatient setting. Multicenter trials have been initiated, and more than 300 patients have been successfully treated with hematopoietic stem cell grafts both from related and unrelated HLA-matched donors.
In Section II, Dr. Richard Champlin describes clinical studies with therapeutic strategies that utilize relatively non-toxic, nonmyeloablative disease-specific preparative regimens incorporating fludarabine, together with other chemotherapeutic agents, to achieve disease suppression and engraftment of allogeneic hematopoietic cells and to allow subsequent infusions of donor lymphocytes. Remissions have been seen in patients with acute myelocytic, chronic myelocytic, chronic lymphocytic, leukemias, lymphomas, and myelomas.
In Section III, Dr. Stanley Riddell and colleagues describe studies on isolation of T cells reactive with minor histocompatibility (H) antigens and involved both in GVHD and graft-versus-leukemia (GVL) responses. For example, the gene encoding a novel H-Y antigen in humans has been identified and shown to exhibit restricted tissue expression. Acute myelocytic leukemia stem cells were demonstrated to express the H-Y antigen and additional minor H antigens, and engraftment of such cells in NOD/SCID mice could be selectively prevented by minor antigen-specific T-cell clones. An autosomal encoded human minor H antigen associated with chronic GVHD has been demonstrated. A trial evaluating therapy of relapsed acute myelocytic leukemia or acute lymphoblastic leukemia after allogeneic stem cell transplantation with T-cell clones specific for recipient minor H antigens has been initiated.
I. Hematopoietic Cell Transplantation in Elderly Patients with Hematologic Cancer: Substituting Graft-versus-Tumor Effects for High-Dose Cytotoxic Therapy
Rainer F. Storb, MD*
Fred Hutchinson Cancer Research Center, 1100 Fairview North, D1-100, P.O. Box 19024, Seattle WA 98109-1024
Conventional allogeneic hematopoietic stem cell transplantation (HSCT) for human patients with marrow-based diseases, such as leukemias and B-cell malignancies, involve conditioning with very high doses of systemic chemotherapeutic agents with or without ionizing total body irradiation (TBI) to both eradicate the patients' underlying diseases and suppress their immune responses so they don't reject the subsequent allografts. The allografts serve to “rescue” patients from the marrow lethal effects of the conditioning regimens.1 Consequently, the conditioning therapy's intensity would be limited only by toxicities to non-marrow organs, such as gut, lung, kidney, heart, and liver. These toxicities have restricted HSCT to younger, medically fit patients, with treatment administered in specialized hospital wards. Almost no allogeneic HSCT have been carried out in patients > 60 years old, and relatively few in patients older than 50 years. Since median ages at diagnoses of patients with acute myelocytic leukemias (AML), chronic myelocytic leukemias (CML), chronic lymphocytic leukemias (CLL), non-Hodgkin lymphomas (NHL), and multiple myelomas (MM) range from 65–70 years, it follows that conventional allogeneic HSCT benefit only a minority of patients with candidate diseases.
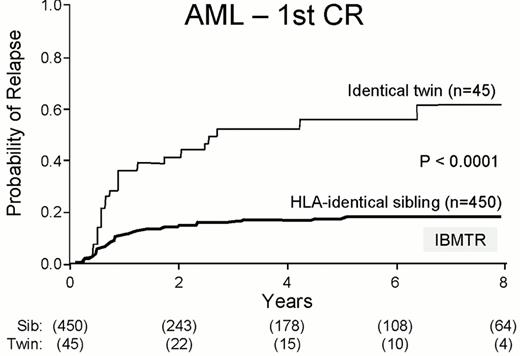
At least two findings have raised questions whether current concepts of allogeneic HSCT are universally valid. First, it has become clear that many hematological cancers cannot always be eradicated by high doses of chemoradiation conditioning, even though regimens may have been intensified to levels at which serious organ toxicities are encountered.1,2 For example, an IBMTR analysis showed that more than 60% of patients with AML in first remission (Figure 1 ) and CML in chronic phase given intensive conditioning treatment followed by monozygous twin HSCT relapse with their diseases, and less than 40% are cured.3 Second, many of the observed cures after allogeneic HSCT are likely due to immunological graft-versus-tumor reactions.4-,7 The IBMTR analysis showed relapse rates of only 20% and 10%, respectively, for patients with AML in first remission and CML in chronic phase given HLA-identical sibling HSCT.3 Thus, graft-versus-tumor effects directed at minor non-HLA antigens and/or leukemia-associated antigens seemed as potent in eradicating malignancies as toxic high-dose therapy. These findings led to the use of donor lymphocyte infusions (DLI) to reinduce remissions in patients whose diseases have relapsed after conventional HSCT.8,9 These observations, together with a better understanding of how to control both host and donor immune cell functions, resulted in a re-evaluation of how to perform allogeneic HSCT in the future. Specifically, instead of relying on tumor eradication through intensive and toxic chemoradiation, the HSCT donor's immune cells might be used for that purpose, invoking graft-versus-tumor effects. Removing the high-dose cytotoxic therapy would allow treatment of those patients who are too old or medically infirm to qualify for conventional HSCT.
This article reviews results with a nonmyeloablative HSCT approach that has been used by collaborating investigators at the Fred Hutchinson Cancer Research Center, University of Washington, Children's Hospital and Regional Medical Center, and Veterans Administration Medical Center, Seattle; Stanford University, Palo Alto, CA; University of Leipzig, Germany; City of Hope National Medical Center, Duarte, CA; University of Colorado, Denver; University of Torino, Italy; University of Arizona, Tucson; Baylor University, Dallas, TX; University of Utah, Salt Lake City; and Oregon Health Sciences University, Portland, and which is based on extensive preclinical studies.
Preclinical Studies
In the major histocompatibility complex identical HSCT setting, two immunological barriers must be overcome. One is the rejection barrier, or host-versus-graft reaction; the other is the graft-versus-host reaction. Both reactions are effected by T lymphocytes, suggesting that agents given after HSCT to control graft-versus-host reactions might also be able to modulate host-versus-graft reactions. The latter feature would allow minimizing the high-dose therapy given before HSCT for host immunosuppression.
Animal models have demonstrated a dose response relationship with respect to TBI and allogeneic engraftment. In random-bred dogs, a single TBI dose of 920 cGy, corresponding to 1,500 cGy fractionated TBI, resulted in engraftment of DLA-identical littermate marrow in virtually all cases. When the dose was decreased by 50%, the majority of dogs rejected their grafts. Using this dose, the addition of postgrafting prednisone did not enhance engraftment, but cyclosporine (CSP) given for 5 weeks led to engraftment in all of the animals.10 When the TBI dose was decreased further to 200 cGy, CSP only allowed engraftment for 3-4 months, after which grafts were rejected. The combination of methotrexate and CSP resulted in engraftment in two out of five animals, but the rest rejected.
The novel immunosuppressant, mycophenolate mofetil (MMF), which blocks de novo purine synthesis, was shown to be synergistic with CSP in studies of graft-versus-host disease (GVHD) prevention. Using 4 weeks of MMF and 5 weeks of CSP, the combination was evaluated for its effect on engraftment. It was found that 11/12 animals successfully established long-term grafts after 200 cGy TBI.11 After 2 years of observation, mixed donor/host chimerism was maintained. When the dose of TBI was further decreased to 100 cGy, long-term engraftment did not occur, suggesting a delicate balance between the host and the graft.
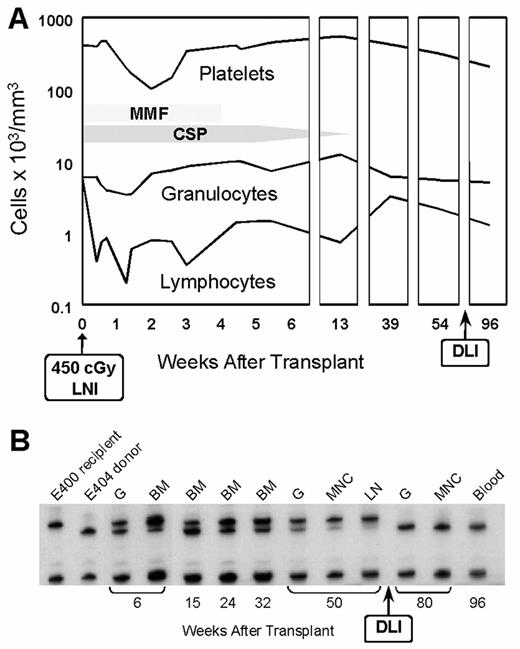
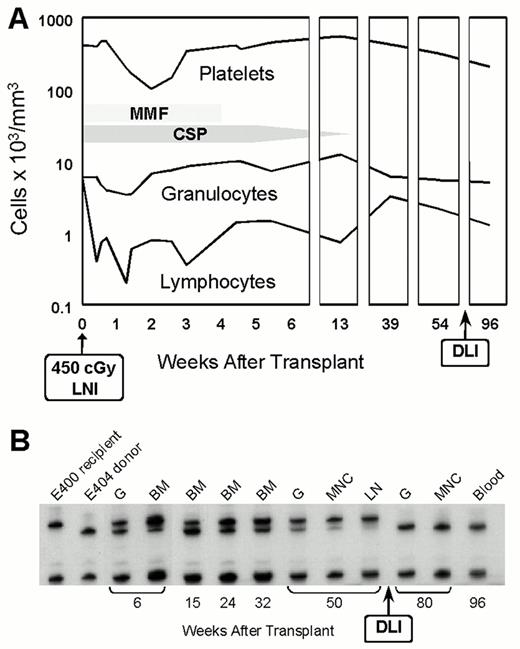
To distinguish whether TBI was important for creating marrow space or whether its major role was to provide host immunosuppression, we irradiated the central lymph node chain from the neck down to the upper abdomen with 450 cGy before HSCT and then administered MMF and CSP.12 The hematologic toxicity was mild, with platelet nadirs of 100,000/μL and granulocyte nadirs of 3,000-5,000/μL (Figure 2 ). At 6 weeks posttransplant, donor cells were present in nonirradiated marrow spaces, suggesting that radiation was not necessary to create space. After 1 year, DLI were given to the animals and, within 9 weeks, recipient cells disappeared as assessed by microsatellite markers, indicating complete allografts. Therefore, allografts had been established without systemic cytotoxic therapy.
The findings suggested that the last vestiges of cytotoxic therapy contained in current regimens might be eliminated in the future. For example, allografts in patients with malignant diseases might be accomplished by inducing specific host-versus-graft non-responsiveness through triggering the host's T-cell receptors with donor antigen while simultaneously blocking costimulatory signals through CD28 and CD40L. Studies in mice and dogs have already shown the feasibility of such an approach.13,14 Alternatively, host T cells might be specifically eliminated using a monoclonal antibody to the T-cell receptor, which is coupled to a short-lived (47 min) α-emitting radionuclide, Bismuth-213. α-emitters deposit their considerable energy within a 50–70 micron radius, and cells that have been irradiated do not undergo DNA repair. Thus, long-term radiation damage is not expected to occur. One or more of these approaches could be combined with “megadoses” of hematopoietic stem cells, shown to overcome engraftment barriers on their own. Avoiding cytotoxic agents in the future is likely to avert the short- and long-term sequelae typically associated with hematopoietic cell grafts outside of those from GVHD.
Clinical Trials
Candidates for nonmyeloablative HSCT included patients who were elderly and could not undergo conventional HSCT, as well as patients with poor organ function. Generally, patients were no longer responding to conventional therapy. We assumed that graft-versus-tumor effects might be more easily established using minimal conditioning due to the persistence of host dendritic cells capable of presenting the minor host-specific peptides to the incoming donor T cells. In high-dose conditioning regimens, these dendritic populations are likely eliminated with myeloablation.
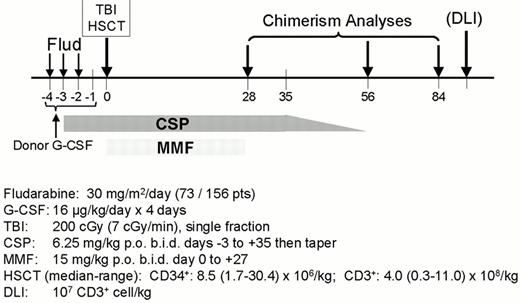
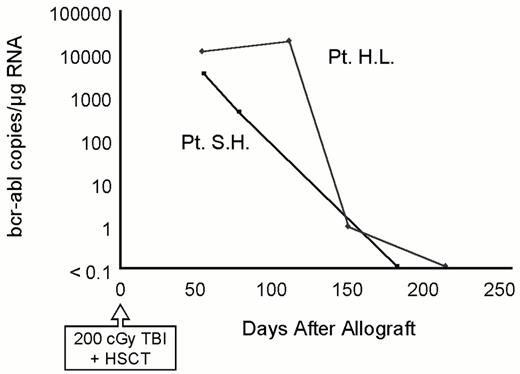
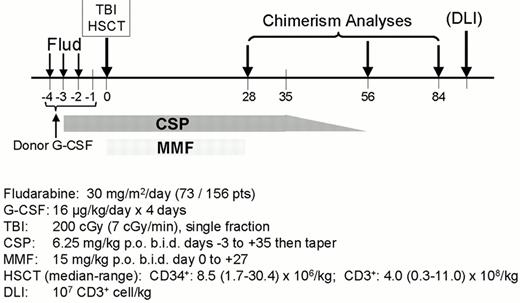
HLA-identical sibling HSCT
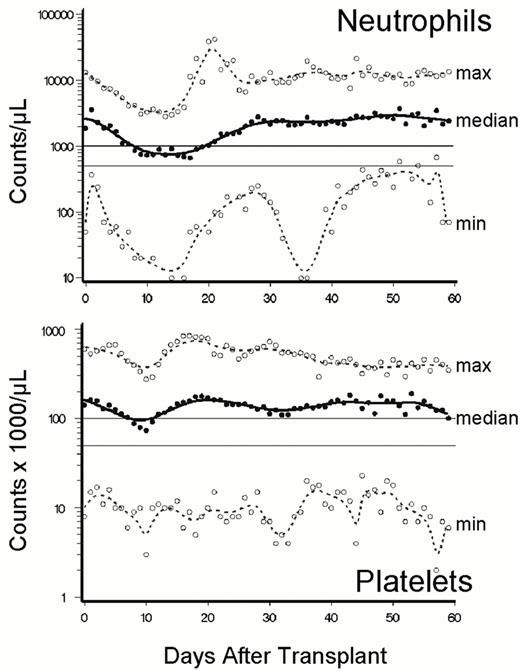
Table 1 provides details on the first 156 patients given sibling grafts.15,16 (and unpublished) The treatment protocol is shown in Figure 3 . Seventy-three patients were conditioned with 200 cGy TBI alone, and 18% experienced non-fatal graft rejections. With the addition of fludarabine, rejections have become the exception. Neutropenias and thrombocytopenias were mild after transplant (Figure 4 ) and patients were initially mixed donor/host chimeras (Figure 5 ). Most patients did not need platelet transfusions, and few received red blood cell transfusions. The majority of HSCT were done entirely in the outpatient setting. Typical side effects of HSCT, such as alopecia, mucositis, diarrhea, veno-occlusive disease of the liver, were absent. There were significantly fewer bacterial infections than seen after conventional HSCT. Grade II-IV acute GVHD occurred in 57% of patients, with 37% having grade II, 13% grade III, and 7% grade IV disease. Chronic GVHD was seen in 65% of patients; however, it responded well to therapy. Fatal progression of underlying diseases occurred in 18% of patients. Non-relapse mortality was 20%. With a median follow-up of 220 (range 100-1026) days, 62% of patients were alive, and progression-free survival was 50%. Complete remissions generally occurred slowly over periods of months as illustrated in Figure 6 .
Unrelated HLA-matched HSCT
Under a similar protocol that extended the postgrafting immunosuppression with MMF and CSP to 96 and 180 days, respectively, 36 patients, 6–65 (median 48) years old, were given unrelated donor HSCT after conditioning with fludarabine and 200 cGy TBI.17 The incidence of rejection was 11%. Acute GVHD was seen in 56% of patients, all of which was of grade II severity. Non-relapse mortality occurred in three (8%) patients, and four patients (11%) died of relapse. With a median follow-up of 167 (range 18–427) days, 27 (75%) patients were alive, with 20 (56%) patients in complete remissions.
Conclusions
The preliminary studies presented here allowed several conclusions. First, the nonmyeloablative regimen used was safe and minimally toxic even in patients otherwise excluded from allogeneic HSCT because of age or medical infirmity. Typical side effects of conventional HSCT were not encountered. Patients did not become severely pancytopenic. As a result, 57% of eligible patients were treated entirely as outpatients, with others having relatively short hospitalizations. The need for transfusion requirements was decreased. Second, most HLA-matched related recipients had stable engraftment despite using only 200 cGy TBI conditioning. The initially observed 18% graft rejection rate was obviated by the addition of three doses of fludarabine immediately preceding TBI. This has allowed sustained engraftment also with HLA-identical unrelated HSCT. Third, acute GVHD was seen in approximately half of the patients, though it mostly appeared to be of moderate severity. Nevertheless, we have extended the period of postgrafting immunosuppression from initially 35 days to now a minimum of 84 days after transplant in order to reduce the risk of GVHD. The optimal duration of postgrafting immunosuppression still remains to be determined. Fourth, the initially observed mixed donor/host hematopoietic chimerism was unstable in most patients, progressing to full-donor chimerism in virtually all of the fludarabine-treated patients, obviating the need for DLI. Fifth, impressive antitumor responses have been seen with complete remissions in 66% of those patients who had measurable disease before transplant. For example, 8 of the 10 patients with CML who stably engrafted were already negative for BCR/ABL, one is negative for the Philadelphia chromosome, and one, a patient with accelerated phase, has stable disease. Of note, accomplishment of complete remissions might take months, and in some cases, exceeded 1 year. The durability of these remissions is still unknown given that the longest follow-up is only approaching 3 years.
II. Chemotherapy Based Nonmyeloablative Preparative Regimens for Allogeneic Hematopoietic Transplantation
Richard Champlin, MD*
Department of Bone Marrow Transplantation, M.D. Anderson Cancer Center, University of Texas, 1515 Holcombe Blvd., Box 24, Houston TX 77030-4095
Dr. Champlin receives research support from Berlex Laboratories.
Traditionally, the goal of the preparative regimen has been eradication of the malignancy as well as providing sufficient immunosuppression to prevent graft rejection. Highly intensive myeloablative regimens have been employed to maximize cytoreduction of the malignancy.
High dose myeloablative therapy with allogeneic hematopoietic transplantation carries a high risk of treatment related complications ranging from 10 to > 50% depending on histocompatibility, age, comorbidities and disease factors. The therapeutic benefit of allogeneic marrow transplantation for many diagnoses is largely related to an associated immune-mediated graft-versus-malignancy effect. This realization has led to development of less toxic, nonmyeloablative preparative regimens to achieve engraftment and allow development of graft-versus-malignancy effects as a primary form of therapy.1 For many nonmalignant disorders, it is not necessary to ablate diseased tissues; it is only necessary to achieve mixed chimerism to provide a source of normal hematopoietic cells.
Two general strategies have emerged. One category is based upon immunosuppressive chemotherapeutic drugs, usually a purine analog in combination with an alkylating agent. The other approach is based upon low dose total body radiation. This section will focus on the chemotherapy based regimens.
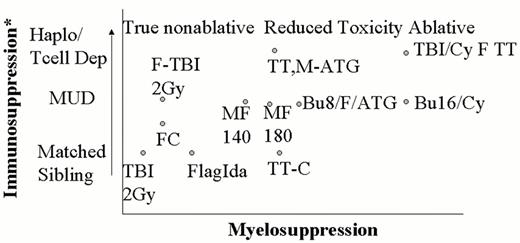
Definition of Nonmyeloablative versus Reduced Toxicity Regimens
A number of regimens have been proposed to reduce the toxicity associated with allogeneic transplantation (see Figure 7 ). As a working definition, a truly nonmyeloablative regimen should not eradicate host hematopoiesis and should allow relatively prompt hematopoietic recovery (< 28 days) without a transplant.1 Upon engraftment mixed chimerism should be present. If the graft is rejected, prompt autologous recovery should occur. Conversely, an ablative regimen requires hematopoietic transplantation for recovery and complete chimerism occurs upon engraftment. Many of the reduced toxicity regimens referred to as nonmyeloablative have not been documented to meet these criteria. These regimens require a transplant for hematologic recovery, and if the graft is rejected, prolonged aplasia typically occurs. These should be referred to as “reduced toxicity” ablative regimens.
The intensity of immunosuppression required for engraftment depends on the immunocompetence of the recipient, histocompatibility and the composition of the transplant. Initial studies focused on patients with an HLA matched sibling donor. More intensive regimens are required for engraftment in settings of greater genetic disparity including unrelated donor or HLA-nonidentical transplants.
The general treatment scheme of a nonablative regimen is illustrated in Figure 8 (see color page 552). The nonablative preparative regimen does not completely eliminate host normal and malignant cells. An allogeneic graft-versus-hematopoietic effect occurs in which donor cells eradicate residual host hematopoiesis. Graft-versus-malignancy effects generally occur after development of full donor T-cell chimerism.2
Potential Advantages and Disadvantages of Nonablative Regimens
Nonablative regimens have been studied as a means to reduce regimen related toxicity in patients considered ineligible for myeloablative preparative regimens because of advanced age or comorbidities. It may also reduce the incidence and severity of acute GVHD, since its clinical manifestations partly result from the toxicity of the preparative regimen and subsequent cytokine release as well as the alloreactivity of the graft. Residual host T cells may also inhibit development of GVHD. Infectious complications may also be reduced. Neutropenia is reduced or eliminated by most nonablative regimens. In addition, since the nonablative preparative regimen does not immediately eliminate host derived immunocompetent cells, these cells can contribute to host defense in the early post-transplant period.
There are also potential disadvantages of using nonablative preparative regimens. Higher doses of busulfan or total body radiation have been shown to reduce the risk of relapse in CML and AML. Approximately one-third of patients with good risk leukemias are cured with high dose therapy and syngeneic transplants in which graft-versus-leukemia (GVL) effects would not be expected to occur.3 Young patients without comorbidities tolerate supralethal regimens well and reducing toxicity may not improve their survival. Reliance on the antimalignancy effects of alloreactive T cells may increase morbidity due to chronic GVHD.
Disease Susceptibility to Graft-versus-Malignancy Effects
There are major differences among malignancies in their susceptibility to GVL effects and, hence, their sensitivity to nonmyeloablative allogeneic transplants (see Table 2 ). CML has been the disease in which GVL effects are best documented.4 The majority of patients who relapse into chronic phase following an allogeneic transplant achieve durable complete remission with DLI. Indolent lymphoid malignancies also appear very sensitive to graft-versus-malignancy effects. Allogeneic transplants are associated with a substantially lower relapse rate than purged autologous transplants. Selected patients with CLL or low-grade lymphoma have responded to DLI or modification of immunosuppressive therapy.5 In preliminary studies of nonablative allogeneic transplants, many patients with low-grade lymphoma, mantle cell lymphoma or CLL have achieved durable remissions.6 These highly sensitive malignancies share several common characteristics. These are indolent disorders that are not immediately life threatening, thus giving time for a graft-versus-malignancy effect to develop. In CML and lymphoma, the malignant cells are derived from antigen presenting cells, B-lymphocytes in the case of lymphoid malignancies and dendritic cells that can be generated from CML.7 Their responsiveness to GVL may in part relate to effective in vivo antigen presentation.
A second category of malignancies can be identified that have intermediate sensitivity to GVL effects, including AML, multiple myeloma, Hodgkin's disease and intermediate-grade lymphoma.4 ALL and high grade lymphoma appear relatively insensitive to GVL effects, although patients with GVHD do have a reduced risk of relapse. The malignant lymphoblasts typically lack costimulatory molecules and do not effectively stimulate an immune response. The rapid rate of proliferation of these malignancies may also outpace a developing immune response; only rare patients have responded to DLI. Graft-versus-tumor effects may also occur against solid tumors, although few studies with allogeneic transplantation have been performed. Pilot studies in breast cancer have reported antitumor responses in patients with GVHD, suggesting a graft-versus-adenocarcinoma effect.8 Major antitumor responses have been reported in renal cell carcinoma, usually concomitant with development of acute GVH.9 Further studies are required to determine whether graft-versus-tumor effects will be sufficiently active to justify the added morbidity related to allogeneic transplantation.
Drugs Used in Nonablative Regimens
Most chemotherapy based nonablative preparative regimens have utilized purine analogs and alkylating agents, usually cyclophosphamide, melphalan or busulfan. Purine analogs (fludarabine, pentostatin or cladribine) have activity against a wide range of hematologic malignancies and are sufficiently immunosuppressive in standard doses to allow engraftment of HLA compatible hematopoietic progenitor cells.
The drugs involved in the individual regimens have generally been chosen to have some activity against the target malignancy as well as providing immunosuppression to prevent graft rejection. Ideally the regimen would prevent disease progression long enough to allow an effective graft-versus-malignancy effect to develop. Most studies of nonmyeloablative hematopoietic transplants have been performed in elderly or medically debilitated patients unable to tolerate an ablative preparative regimen. Some studies have included younger patients with standard eligibility criteria; differences in patient selection generally preclude meaningful comparisons among regimens.
Giralt et al initially evaluated use of standard dose purine analog based chemotherapy as a nonablative preparative regimen in patients with advanced myeloid leukemias.10 The regimen has been studied as a treatment for AML without transplantation and includes fludarabine 30 mg/m2/d x 4 days, cytarabine 1 g/m2/day x 4 days and idarubicin 12 mg/m2/d x 3 days. Thirty-six patients with AML, myelodysplasia or CML, aged 55 to 75 years, were treated.11 Patients with residual or recurrent disease received additional DLI or second nonablative transplants. Ninety-one percent of patients had initial engraftment with donor-derived cells. Treatment related mortality was 20%. Acute GVHD grade 2–4 occurred in 32%, and chronic GVHD in 52%. Eighty-eight percent achieved complete remission. Thirteen patients were alive in remission with a median follow-up of 11.5 months, range 4–40 months. The projected disease free survival of patients who were in remission or had < 10% bone-marrow blasts at the time of transplant was 40% beyond 2 years. The outcome of patients with refractory leukemia at transplant was poor; < 10% remained in remission at one year. These results are consistent with the premise that the disease must be controlled for at least several months to allow GVL effects to develop.12 These data indicate that nonmyeloablative allogeneic transplants are feasible in elderly patients with acceptable toxicity and GVHD rates.
Giralt et al subsequently reported a study combining melphalan (180 mg/m2) and fludarabine (125 mg/m2) for treatment of advanced acute leukemia; this is a more intensive regimen that should be considered a “reduced toxicity” ablative regimen. It is sufficiently immunosuppressive to allow for engraftment from unrelated donors as well as matched siblings. The additional cytoreduction resulted in improved disease-free survival in AML patients, particularly in those transplanted in relapse,13 and suggests that cytoreduction of the malignancy by the preparative regimen has value. Patients with refractory relapse have 25% extended disease free survival, and 56% of patients with chemotherapy sensitive disease remained in continuous remission beyond one year. These results are similar to those achieved with ablative preparative regimens in younger but otherwise similar patients.
Slavin et al reported use of a reduced toxicity preparative regimen consisting of busulfan (8 mg/kg), fludarabine and antithymocyte globulin.14 Although less toxic than commonly used ablative preparative regimens, this regimen produces marked myelosuppression and has not been administered without hematopoietic transplantation. Results of this regimen have been particularly encouraging in CML.
Khouri et al reported the use of fludarabine (90–125 mg/m2) plus cyclophosphamide (2 g/m2) in patients with lymphoid malignancies;6 this regimen has been effective to achieve engraftment and its use has been extended to a range of malignancies by a number of investigators.2,15 Khouri et al also treated 15 patients with far advanced CLL or transformed lymphoma using a nonmyeloablative regimen of fludarabine/cyclophosphamide or fludarabine, cytarabine, cisplatin.6 All patients had failed to respond or recurred after primary chemotherapy. Eleven of the 15 patients had durable engraftment, with 50 to 100% donor cells at one month post-transplant, typically converting to 100% over the next two months spontaneously or after infusion of additional DLI. Hematopoietic recovery was prompt and no non-hematologic toxicity ≥ grade 2 occurred. All 11 patients with engraftment responded, and 8 achieved complete remission. Maximal responses were slow to develop and gradually occured over a period of one year. Extending these studies to low-grade lymphoma, 20 additional patients received fludarabine, cyclophosphamide +/- rituximab, followed by allogeneic blood stem cell transplantation. This produced minimal toxicity and a median of 6 days with neutropenia. All achieved engraftment and complete remission with minimal treatment related morbidity.16 Updated results indicate 80% disease free survival beyond 2 years with all surviving patients having disease undetectable by polymerase chain reaction. These data compare favorably to high dose cyclophosphamide-total body radiation regimens in which treatment related mortality rates typically exceed 40%.17 Other small studies have had similar findings.2 This same approach has also produced encouraging results in patients with recurrent mantle cell lymphoma and chemosensitive patients with recurrent intermediate grade lymphomas.
Allogeneic bone marrow transplantation is associated with a high risk of treatment-related mortality in multiple myeloma, in some studies up to 70%. Use of a nonablative preparative regimen may reduce this morbidity while still inducing a graft-versus-myeloma effect. Giralt et al explored a regimen of melphalan (140 mg/m2) and fludarabine (120 mg/m2). Seven of 13 patients with far advanced myeloma achieved complete remission.18 Others reported similar results.19 This promising approach requires further study. Encouraging results have also been reported in patients with Hodgkin disease.20,21 A novel strategy under study in these two diagnoses is the use of tandem autologous and allogeneic transplantation. High dose therapy with autologous transplant is initially performed to cytoreduce the malignancy, followed by a nonablative allogeneic transplant with the goal of eradicating minimal residual disease. The relative efficacy of this tandem procedure versus a single transplant needs to be determined.
Mechanism of Graft-versus-Malignancy Effects
Clinically, malignancy specific reactivity can only rarely be demonstrated after allogeneic hematopoietic transplantation. Donor derived T cell clones from allogeneic chimeras typically react against both host normal hematopoietic cells and the leukemia, suggesting that hematopoietic minor histocompatibility antigens may be targeted. Several candidate minor histocompatibility antigens have been proposed. Abnormally or over-expressed cellular constituents could also serve as a target antigen for GVL. Proteinase-3, a serine protease present in myeloid primary granules, is overexpressed in CML and some cases of AML; it may serve as a target for an antileukemic immune response. Peptide antigens derived from proteinase 3 can stimulate generation of autologous or allogeneic T cell cytotoxicity against the leukemia.22 Other candidate overexpressed genes include myeloperoxidase and WT1. Thus, graft-versus-malignancy could involve broad reactivity overlapping with GVHD, or restricted antihematopoietic or disease specific responses. The potential target antigens for graft- versus-solid tumor effects are unknown, but overexpressed tissue antigens or polymorphic tissue restricted minor histocompatibility antigens could be involved. It is also possible that GVHD could produce antitumor effects through cytokines or a mechanism other than specific T cell cytotoxicity.
Graft-versus-malignancy responses often occur coincident with or following GVHD. However, some patients achieve a GVL response, i.e., remission of their leukemia, without developing GVHD. Although this is consistent with the premise that different target antigens may be involved with each process, responses could result from greater sensitivity of malignant cells than visceral tissues to a common immunologic mechanism.
Separation of Graft-versus-Malignancy from GVHD
A fundamental goal is to separate the beneficial GVL effect from the adverse manifestations of GVHD. A number of approaches have been studied. Given the interplay between GVL and GVHD, use of posttransplant immunosuppressive therapy can have both positive and negative effects. Immunosuppressive therapy given early post-transplant may inhibit GVL; two randomized studies report lower relapse rates in patients in AML receiving low dose rather than full dose cyclosporine after ablative BMT.23 A variety of posttransplant regimens have been utilized with nonablative transplants, ranging from full dose tacrolimus and methotrexate, abbreviated courses of these agents or the combination of cyclosporine and mycophenolate mofetil.24 As indicated, acute GVHD tends to be less severe after a nonablative preparative regimen, but GVHD frequently occurs after early termination of immunosuppressive therapy and is often problematic, particularly in older or debilitated patients. Inclusion of Campath-1H has recently been reported to produce a low rate of GVHD;25 it is uncertain whether this agent will adversely effect immune recovery or GVL effects after nonmyeloablative transplants.
GVHD is initiated by alloreactive T cells. A novel strategy is to achieve an initial tolerant graft followed by infusion of engineered T or NK cell populations targeting the malignancy. Possibilities include an initial T cell depleted graft or combining CD34+ cells from the donor with nonalloreactive T cells directed against a third party or specific target antigens Another strategy is to transduce donor T cells with a suicide gene, such as Herpes simplex virus thymidine kinase, which confers sensitivity to ganciclovir treatment.
An ideal cellular therapy would consist of leukemia-specific effectors devoid of graft-versus-host activity. T cell clones or lines have been successfully used for treatment of Epstein-Barr virus related lymphoproliferative disease and cytomegalovirus infections occurring after allogeneic bone marrow transplantation. Falkenburg et al reported a single case of a patient with CML who responded to an infusion of T cell lines raised against the leukemia.26 The technology for development of therapeutic T cell clones is demanding, and this approach is not sufficiently developed to allow for large-scale clinical trials. Alternatively T cells reactive against overexpressed malignancy-related antigens could be selected, expanded and parenterally administered as adoptive cellular therapy. Nonablative hematopoietic transplants may become a platform for administration of cellular immunotherapy. Transplantation of allogeneic CD34+ stem cells could be combined with engineered malignancy or infection-specific effectors devoid of graft-versus-host activity.
Conclusion
In conclusion, use of relatively nontoxic, nonmyeloablative or “reduced toxicity” preparative regimens allows engraftment and generation of graft-versus-malignancy effects. This approach is potentially curative for susceptible malignancies and reduces the risks of treatment-related morbidity. This strategy can extend the use of allotransplantation for older patients and those with comorbidities that preclude high dose chemoradiotherapy. The indications for a nonmyeloablative allogeneic transplant versus alternative transplant and nontransplant strategies need to be defined for each target malignancy in controlled clinical trials.
III. Minor Histocompatibility Antigens—Major Targets of Graft-versus-Leukemia Responses
Stanley R. Riddell, MD,*
Fred Hutchinson Cancer Research Center, 1100 Fairview Avenue N, D3-100, Seattle WA 98108-1024
The eradication of leukemia after allogeneic HSCT results both from the cytotoxic chemoradiotherapy administered prior to transplant and immunologic mechanisms mediated by effector cells contained in or derived from the stem cell graft.1 Two important clinical developments have evolved from identification of this immune mediated GVL effect. The first is the use of DLI to treat patients with posttransplant leukemic relapse.2-,5 With DLI, the majority of patients with recurrent CML after HSCT achieve a complete remission and a smaller but significant fraction of patients with other malignancies respond to therapy.3,6 The second is the development of allogeneic HSCT using less toxic nonmyeloablative conditioning regimens.7-,12 With this approach, low doses of irradiation and chemotherapy, which alone are not sufficient to eradicate tumors, are administered to facilitate graft acceptance, and tumor regression is induced by donor immune cells. Nonmyeloablative transplants have significant activity for patients with CML, CLL, myeloma, lymphoma, and renal cell carcinoma.7-,12 The potent antitumor effects observed after DLI and allogeneic HSCT in a variety of advanced malignancies represent a remarkable demonstration of the curative potential of immunotherapy in contrast to the difficulty of eliciting effective autologous antitumor immune responses to tumor associated antigens by vaccination or cellular therapy.13 However, with current approaches to allogeneic HSCT it has not been possible to separate the beneficial GVL effect from deleterious GVHD.
Effector Mechanisms in the Graft-versus-Leukemia Response
A more complete understanding of the cellular mechanisms operative in an allogeneic GVL response should provide critical insights into the requirements for effective antitumor immunity and potentially permit separation of GVL from GVHD. The association of GVL activity with GVHD has implicated donor T cells reacting with minor histocompatibility (H) antigens expressed by recipient cells as major contributors to the GVL effect. The first clinical demonstration of GVL activity was observed after allogeneic HSCT for advanced leukemia in which the probability of leukemic relapse was found to be significantly lower in those patients who developed acute and/or chronic GVHD.14,15 Analysis of patients with CML, AML, or ALL treated with either allogeneic unmodified HSCT, allogeneic T cell depleted HSCT, or syngeneic HSCT showed that the risk of relapse was lowest for patients who received allogeneic unmodified HSCT and developed acute and/or chronic GVHD.1,16 Transplantation with syngeneic or T cell depleted allogeneic marrow to avoid GVHD was associated with a higher risk of relapse unless the conditioning regimen was intensified.1,17,18 However, GVHD is not a prerequisite for GVL activity. A reduction in relapse was evident in the subset of CML and AML patients who received allogeneic unmodified HCT but did not develop GVHD, and remissions have been observed after DLI in the absence of significant GVHD.1,3 This suggested that there may be antigenic determinants recognized by T cells that would permit the separation of GVL responses from GVHD.
There is evidence that effector mechanisms other than T cells may also contribute to GVL activity either directly or as a consequence of inflammation induced by allogeneic T cells. NK cells lyse leukemic cells in vitro and may be particularly effective for inducing GVL activity after T cell depleted haploidentical transplant where disparity between killer inhibitory receptors (KIRs) expressed by donor NK cells and HLA molecules on recipient leukemic cells favors NK activation.19,20 Recently, antibody responses to nonpolymorphic proteins expressed in leukemic cells have been detected in CML patients who have relapsed after an allogeneic HSCT and then achieved remission with DLI.21 Thus, while allogeneic T cells are central to the GVL effect after HLA matched HSCT and will be the subject of the remainder of this review, other effector mechanisms may contribute to antitumor activity in selected circumstances.
Target Antigens for T Cells in Graft-versus-Leukemia Responses
Clinical and animal studies have identified donor CD8+ cytotoxic T cells (CTL) and CD4+ helper T cells (Th) as the primary mediators of GVHD and GVL responses after allogeneic HCT between HLA identical individuals.22 CD8+ and CD4+ T cells recognize antigenic peptides displayed on the surface of target cells bound to class I or class II MHC molecules, respectively.23,24 One approach for separating GVL from GVHD is to identify peptides that are recognized by T cells and presented by leukemic cells but not by tissues that are a target of GVHD. Several broad categories of proteins may give rise to antigens that could be targets of a selective GVL response. These include a) tumor-specific proteins resulting from chromosome translocations, such as bcr/abl or PML/RARα, or from mutations such as p21 ras;25-,27 b) normal proteins that are overexpressed in leukemic cells such as WT-1 or proteinase 3;28-,32 and c) minor H antigens that are selectively expressed in recipient hematopoietic cells, including leukemic cells, but not in nonhematopoietic cells.33- 37
The first two categories of antigens are not alloantigens and therefore could be relevant for immunotherapy in the absence of allogeneic HCT. However, it is conceivable that providing allogeneic cells that have not been previously exposed to the tumor may facilitate eliciting a T cell response to these proteins. Proteins such as p21 ras and bcr/abl are attractive targets for a GVL response because of their tumor-specific expression and involvement in the malignant phenotype. Unfortunately, there is little evidence as yet for activation of donor T cells reactive with such antigens after allogeneic HSCT.38 Studies to elicit bcr/abl-specific responses by vaccination of CML patients with synthetic peptides are in progress.39,40 The results of these studies should help clarify the immunogenicity of this protein and its relevance as a target for immunotherapy.
Normal proteins that are overexpressed in leukemic cells have been proposed as targets for GVL responses. Proteinase 3 (PR-3) is a serine protease expressed in normal myeloid differentiation and overexpressed in CML and AML progenitors. CD8+ T cell responses to PR-3 were initially demonstrated by stimulating lymphocytes from normal individuals with a peptide that was predicted to bind to HLA A2.30 These T cells lysed CML cells and inhibited leukemic colony formation, demonstrating that leukemic cells presented this antigen to T cells.30-,32 Moreover, PR-3 reactive T cells had no effect on normal hematopoietic progenitors in vitro.31 A recent study demonstrated expansion of PR-3 reactive T cells in patients who responded to allogeneic HCT, DLI, or interferon, supporting the hypothesis that these T cells may participate in a GVL response without affecting normal hematopoiesis or causing GVHD.41 Similar to PR-3, WT-1 is expressed at high levels in some leukemias but at low levels in normal hematopoietic cells.28,42 CD8+ T cell responses to WT-1 have also been elicited in vitro and inhibit leukemic colony formation without affecting normal colony growth.28,29,43 Vaccination and T cell therapy trials targeting PR-3 and WT-1 have been proposed. The development of expression array technology to identify genes that are overexpressed in leukemic cells may identify additional antigens in this category or future studies.
The third and broadest class of antigens for a GVL response is minor H antigens. The potency of the GVL effect in allogeneic compared with syngeneic HCT emphasizes the critical importance of minor H antigens for immune mediated eradication of tumors. Minor H antigens are derived from proteins that differ between the donor and recipient due to polymorphism in the genome.44-,49 These polymorphisms may encode changes in amino acid sequence that result in altered binding of the peptides to MHC, contact between the MHC/peptide complex and the T cell receptor, or differential processing of the protein.44- 50 Thus, even though HLA matched siblings express identical MHC molecules on the surface of their cells, the repertoire of peptides displayed in the MHC binding groove may differ substantially due to genetic differences outside the MHC.
Cell culture techniques for characterizing T cell responses to minor H antigens after allogeneic HSCT have been developed. Studies analyzing minor H antigen-specific T cell responses have already provided several insights into their potential as targets for GVL therapy. First, minor H antigen-specific T cell clones that lyse recipient hematopoietic cells but not nonhematopoietic cells can be isolated from the majority of HLA identical HSCT recipients.34,51 The observation that expression of some minor H antigens was tissue restricted was not surprising because hematopoietic and nonhematopoietic tissues express distinct genetic programs that dictate their phenotype and function. However, these results identified a potential strategy for the selective targeting of recipient hematopoietic cells, including leukemic cells, without causing GVHD. Second, there are a very large number of minor H antigens in the human population. Goulmy et al have described minor H antigens encoded by autosomes (HA-1 to HA-7) and H-Y antigens encoded by the Y chromosome genes SMCY and DFFRY.33 Our group has defined 38 novel minor H antigens recognized by CD8+ T cells based on differences in the class I HLA restricting allele and/or the pattern of recognition of cells from unrelated individuals sharing the HLA restricting allele (34; Warren EH, Riddell SR, unpublished data). Finally, minor H antigens are inherited in a Mendelian fashion.33 Thus, once a sufficient number of minor H antigens are identified and determined to be involved in GVL responses, tissue typing of donors and recipients can be used to identify appropriate targets for therapy.
Identification of Minor H Antigen Genes
The isolation of T cell clones that recognize minor H antigens has provided reagents for characterizing tissue expression of the antigen and for gene identification. The identification of genes encoding minor H antigens recognized by CD8+ T cells has progressed more quickly although strategies for antigen identification for CD4+ T cells have recently been developed.52 Three methods are being applied to the discovery of genes encoding human minor H antigens recognized by CD8+ T cells. These include peptide elution and mass spectrometry,53 cDNA expression cloning,54 and genetic linkage analysis.55 Goulmy and Engelhard have eluted peptides from class I MHC molecules, separated fractions that reconstitute T cell recognition, and sequenced the active peptides by mass spectrometry.44,45,47,48,56 Their studies have identified the amino acid sequence for 5 minor H antigens. A search of DNA and protein databases revealed that Y chromosome genes SCMCY and DFFRY encode 3 of the minor H antigens. SMCY and DFFRY are broadly expressed in both hematopoietic and nonhematopoietic tissues, suggesting that T cell responses to these antigens may mediate GVHD in addition to GVL activity.48,56 Indeed, the development of T cell responses to the SMCY/HLA A2 minor H antigen was associated with the development of acute GVHD after HCT from a female donor to a male recipient.57
An HLA A2-restricted minor H antigen, termed HA-1, was found to be encoded by an autosomal gene (KIAA0223), and another, termed HA-2, had homology to a sequence in the class II myosin gene.44,45 Both of these minor H antigens are selectively expressed in hematopoietic cells and have been proposed as targets for a GVL response. HA-1 incompatibility was associated with a lower rate of leukemic relapse in one small study, but other studies have linked HA-1 incompatibility with GVHD.57-,59 This was surprising based on its tissue expression. However, HA-1 is highly expressed in dendritic cells (DC), which have a critical role in the induction of GVHD.60 Thus, it is conceivable that local inflammation initiated by T cells responding to HA-1 expressed by recipient DC in tissues might lead to recruitment of T cells responding to other minor H antigens expressed on epithelial cells. Additional studies are needed to resolve the role of this minor H antigen in GVHD and GVL responses.
In collaboration with the Engelhard laboratory, we have also used peptide elution to discover an HLA A2-restricted minor H antigen, termed HA-8, which is encoded by the KIAA0020 gene.50 KIAA0020 is broadly expressed in both hematopoietic and nonhematopoietic cells. Preliminary studies examining 577 HLA A2+ allogeneic HCT recipients demonstrated that recipients who express HA-8 and have HA-8 negative donors have an increased risk of both acute and chronic GVHD (61; Akatsuka Y, unpublished data). The broad tissue distribution of KIAA0020 and the clinical association of HA-8 incompatibility with GVHD suggest HA-8 would not be suitable as a GVL target.
Our lab has also used the cDNA expression cloning methodology pioneered by Boon et al54 to identify 4 novel genes encoding minor H antigens. One of the genes identified is the Y chromosome gene UTY that encodes a peptide presented by HLA B8.49 In contrast to CTL specific for SMCY, which are associated with GVHD, the CTL specific for UTY were isolated from an allogeneic HSCT recipient without GVHD and lysed hematopoietic cells including leukemic blasts but not skin fibroblasts. By RNA analysis, UTY is highly expressed in hematopoietic cells and is low in most nonhematopoietic tissues. Thus, we have searched for additional epitopes in UTY that may be presented by other common HLA alleles. Three transcripts of UTY encode proteins of 1079, 1240, and 1347 amino acids, respectively.62 The coding sequence of all three UTY transcripts is identical over the first 1079 amino acids, and transcripts 2 and 3 are identical over 1240 amino acids. Comparison of UTY with the UTX homologue encoded by the X chromosome showed only 80-84% homology, suggesting there will be epitopes presented by other HLA alleles. This was validated by the recent discovery of a UTY peptide presented by HLA B60.63 Thus, UTY may be broadly applicable for a GVL response in male recipients of HCT from female donors. The genes encoding three additional minor H antigens that are encoded by autosomes and selectively presented to CTL by hematopoietic cells and leukemic blasts have recently been identified with this approach.
A third approach for identifying minor H antigen genes involves genetic linkage analysis using Epstein-Barr virus transformed B cell lines established from the Centre d'Etude Polymorphism Humain (CEPH) reference families that have been extensively mapped for genetic markers. Completion of the Human Genome Project should increase the probability that this approach will identify candidate genes rather than simply provide a chromosomal location of the minor H antigen, and it is anticipated that it will be more extensively used in the future.55
Expression of Minor H Antigens on Leukemic Cells
An essential criterion for selection of minor H antigens to induce a GVL response is expression of the antigen on leukemic cells. The sensitivity of leukemic cells to minor H antigen-specific T cells has relied on assays of the ability to T cells to lyse radiolabeled leukemic blasts or to inhibit leukemic colony formation in soft agar.34,64,65 However, it is unclear if these assays detect recognition of leukemic stem cells. Transplantation of human leukemia into NOD/SCID mice has identified a putative stem cell, which is essential for establishing leukemic hematopoiesis.66,67 The NOD/SCID model has now been adapted for studies to assess recognition of this SCID leukemic initiating cell (SL-IC) by minor H antigen-specific CTL.68 Studies in our lab examining CD8+ CTL specific for five distinct minor H antigens, including the antigen encoded by UTY, demonstrate that SL-IC could be specifically eliminated by minor H antigen-specific CTL.68
Strategies for Exploiting the GVL Effect
Donor lymphocyte infusions
Relapse of the malignancy remains a frequent cause of treatment failure for patients who undergo allogeneic HSCT. The recognition that donor T cells mediate a GVL effect led to efforts to augment this effect in patients with advanced disease by infusing additional donor lymphocytes early post transplant. This was complicated by a high incidence of severe GVHD and an increase in non-relapse mortality.69 However, DLI given later after HSCT to patients with relapsed leukemia have induced GVL effects with more modest toxicity. Approximately 75% of patients with recurrence of CML in the chronic phase and up to 25% of patients with AML or ALL have achieved a complete remission after DLI.2-,5 GVHD remains a major complication of DLI occurring in 50-65% of patients and contributes to an 18% probability of death in remission at one year.3 Efforts to control GVHD while preserving antileukemic activity of DLI using graded doses of lymphocytes or depletion of the CD8+ T cell subset have been partially effective but have not permitted the complete separation of GVL from GVHD.70,71 The results of DLI validate the concept that the GVL effect can be augmented by immunotherapy, but the development of GVHD in the majority of treated patients and the low response rate in patients with acute leukemia remain significant limitations.
Suicide genes
Methods have been developed to introduce genes into T cells and confer novel functions. The HSV thymidine kinase (HSV-TK) gene has been evaluated as an inducible suicide gene to regulate the survival of donor T cells and ameliorate GVHD. Unlike the mammalian TK, HSV-TK efficiently phosphorylates ganciclovir leading to the formation of toxic diphosphate and triphosphate moieties that interfere with DNA replication in dividing cells. HSV-TK was introduced into T cells in adoptive transfer studies of virus-specific CTL in nontransplant patients. In this setting, the transduced T cells were eliminated by an immune response to the foreign TK transgene product.72 A similar outcome was observed in HSCT recipients of unmodified stem cell grafts who received TK-modified DLI to treat leukemic relapse more than one year after transplant (Flowers MED, Riddell SR, unpublished data). However, Bordignon et al used HSV-TK modified DLI to treat relapsed leukemia or Epstein-Barr virus (EBV) lymphoproliferative disease in recipients of T cell depleted allogeneic HSCT and observed immune responses to the transgene product in only a minor subset of patients.73 Moreover, their study demonstrated the successful ablation of transduced T cells and reversal of GVHD with ganciclovir administration.
Alternative transgenes for inducing cell suicide that may be less immunogenic are in development. One approach, based on the expression of Fas that naturally signals apoptosis in T lymphocytes, uses a fusion gene that encodes 3 human proteins.74 These include the extracellular and transmembrane domains of the human low affinity nerve growth factor receptor (LNGFR) to provide a marker for selection, two copies of human FKBP12 containing a single point mutation to provide high affinity binding to a drug AP1903, and the intracellular domain of Fas to signal cell death. This fusion gene is inert until addition of AP1903, which binds AP1903, clusters the chimeric Fas molecules, and induces apoptosis.74 This approach does not require cell division for the induction of cell death, and the human origin of the transgene product should reduce the probability it will be immunogenic.
Antigen-specific T cell clones
The use of antigen-specific T cell clones rather than polyclonal donor lymphocytes might provide a more potent antileukemic effect and reduce the risk of GVHD. cytomegalovirus (CMV) and EBV-specific T cells have been isolated from allogeneic donors, cultured in vitro and adoptively transferred to the respective recipient without causing GVHD. Moreover, these studies have demonstrated that transferred T cells can persist in vivo, migrate to sites of antigen, and exert effector function.75- 77 The identification of minor H antigens and leukemia associated proteins such as WT-1 and PR-3 suggests a similar approach may be used to augment the GVL effect without causing GVHD. Initial studies to assess the adoptive transfer of T cell clones to patients with posttransplant leukemic relapse are already in progress and should provide insight into the safety of this approach.
Studies in animal models and in humans have identified obstacles that may limit the therapeutic success of T cell transfer. The elimination of leukemia may require prolonged persistence of the transferred T cells, suggesting that CD4+ Th cells or interleukin (IL)-2 may be required.78 Tumors may evade T cell recognition by loss of antigen or MHC expression,79 or by inducing functional anergy in tumor-reactive T cells.80 Thus, to provide insights into limitations of antigen-specific T cell therapy for leukemia, it will be essential to monitor persistence, migration, and function of transferred T cells and to examine alterations in tumor cells if relapse occurs after therapy. This information can then be used to guide subsequent studies and hopefully lead to the successful incorporation of specific T cell therapy into allogeneic HSCT regimens.
Probability of relapse in patients with AML in 1st complete remission given high-dose conventional hematopoietic stem cell transplant (HSCT).(adapted from 3)
Probability of relapse in patients with AML in 1st complete remission given high-dose conventional hematopoietic stem cell transplant (HSCT).(adapted from 3)
(A) Peripheral blood granulocyte, platelet, and lymphocyte changes in dog E400 conditioned with 450 cGy lymph node irradiation (LNI) and given a marrow graft from a DLA-identical littermate on day 0, followed by postgrafting MMF/CSP for 4 and 14.3 weeks, respectively.12
(B) Results of testing for microsatellite markers of donor and recipient cells before transplantation (left) and recipient cells after marrow transplantation (right).
Abbreviations: G, granulocytes; BM, bone marrow; MNC, mononuclear cells; LNI, lymph node irradiation; DLI, donor lymphocyte infusion; CSP, cyclosporine; MMR, mycophenolate mofetil
(A) Peripheral blood granulocyte, platelet, and lymphocyte changes in dog E400 conditioned with 450 cGy lymph node irradiation (LNI) and given a marrow graft from a DLA-identical littermate on day 0, followed by postgrafting MMF/CSP for 4 and 14.3 weeks, respectively.12
(B) Results of testing for microsatellite markers of donor and recipient cells before transplantation (left) and recipient cells after marrow transplantation (right).
Abbreviations: G, granulocytes; BM, bone marrow; MNC, mononuclear cells; LNI, lymph node irradiation; DLI, donor lymphocyte infusion; CSP, cyclosporine; MMR, mycophenolate mofetil
Treatment protocol for HLA-matched related hematopoietic stem cell transplant (HSCT).
Abbreviations: See Figure 2.
Treatment protocol for HLA-matched related hematopoietic stem cell transplant (HSCT).
Abbreviations: See Figure 2.
Neutrophil and platelet changes among the first 87 patients given 200 cGy TBI ± fludarabine and mycophenolate mofetil/cyclosporine after HLA-matched related hematopoietic stem cell transplant.
Neutrophil and platelet changes among the first 87 patients given 200 cGy TBI ± fludarabine and mycophenolate mofetil/cyclosporine after HLA-matched related hematopoietic stem cell transplant.
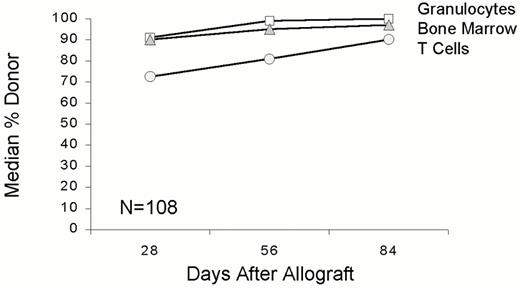
Donor chimerism results in the first 108 patients given 200 cGy TBI ± fludarabine before and mycophenolate mofetil/cyclosporine after HLA-matched related hematopoietic stem cell transplant.
Donor chimerism results in the first 108 patients given 200 cGy TBI ± fludarabine before and mycophenolate mofetil/cyclosporine after HLA-matched related hematopoietic stem cell transplant.
Examples of declines in bcr/abl RNA levels in two patients with chronic myelogenous leukemia given HLA-matched related hematopoietic stem cell transplant.
Examples of declines in bcr/abl RNA levels in two patients with chronic myelogenous leukemia given HLA-matched related hematopoietic stem cell transplant.
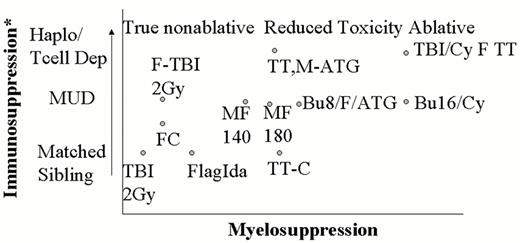
Commonly used nonablative or reduced toxicity regimens.
Nonablative regimens do not eradicate host hematopoiesis and immunity, and autologous recovery occurs if the graft is rejected. Many regimens proposed to reduce toxicity still require transplantation to be safely administered, and graft rejection results in prolonged pancytopenia; these regimens should be considered reduced toxicity ablative regimens. Increased intensity of immunosuppression is necessary for engraftment of unrelated donor or haploidentical transplants.
Abbreviations: Flag-ida, fludarabine, cytosine arabinoside, idarubicin; FC, fludarabine cyclophosphamide; MF, melphalan-fludarabine; TBI, total body radiation; F-TBI, fludarabine-TBI; TT-C, thiotepa-cyclophosphamide; TT-M-ATG, thiotepa-melphalan-antithymocyte globulin; BU, busulfan; CY, cyclophosphamide; Haplo T Cell Dep, haploidentical T cell depleted, MUD, matched unrelated donor.
Commonly used nonablative or reduced toxicity regimens.
Nonablative regimens do not eradicate host hematopoiesis and immunity, and autologous recovery occurs if the graft is rejected. Many regimens proposed to reduce toxicity still require transplantation to be safely administered, and graft rejection results in prolonged pancytopenia; these regimens should be considered reduced toxicity ablative regimens. Increased intensity of immunosuppression is necessary for engraftment of unrelated donor or haploidentical transplants.
Abbreviations: Flag-ida, fludarabine, cytosine arabinoside, idarubicin; FC, fludarabine cyclophosphamide; MF, melphalan-fludarabine; TBI, total body radiation; F-TBI, fludarabine-TBI; TT-C, thiotepa-cyclophosphamide; TT-M-ATG, thiotepa-melphalan-antithymocyte globulin; BU, busulfan; CY, cyclophosphamide; Haplo T Cell Dep, haploidentical T cell depleted, MUD, matched unrelated donor.