Abstract
Myelodysplastic syndrome (MDS) is a hemopoietic stem cell disorder that is potentially curable by transplantation of normal hemopoietic stem cells. The optimum timing, however, and the best conditioning strategy have remained controversial. Both conventional and reduced-intensity/nonmyeloablative regimens have been used successfully. Among selected patients with less advanced/low-risk MDS (< 5% marrow myeloblasts), 3-year survivals of 65% to 75% are achievable with HLA-matched related and unrelated donors. Among patients with more advanced/ high-risk disease (≥ 5% marrow blasts; high International Prognostic Scoring System [IPSS] scores), the probability of post-transplant relapse ranges from 10% to 40%, and, as a result, relapse-free survival is inferior. In addition to disease stage, co-morbid conditions, pre-transplant chemotherapy, conditioning regimen, source of stem cells, and post-transplant immunosuppression affect transplant outcome. Reduced-intensity conditioning regimens are associated with a decrease in non-relapse mortality and allow for successful hemopoietic stem cell transplants even in patients 60–70 years of age. Graft-versus-host disease, both acute and chronic, and post-transplant relapse remain challenging problems.
Hemopoietic cell transplantation (HCT) has curative potential for patients with myelodysplastic syndrome (MDS). However, the indications and, in particular, the timing of HCT for MDS have remained controversial. First, MDS occurs predominantly in older patients, and transplant-related morbidity and mortality have often been high in that age group. Second, MDS may progress slowly over many years, and a high-risk procedure such as HCT may be ill-advised early in the course.1 Third, as our understanding of the pathophysiology of MDS has improved, several non-transplant strategies have emerged that have shown efficacy in improving or stabilizing hematologic parameters and, in subgroups of patients, appear to have induced true remissions, at least transiently. Various classification schemes and prognostic scoring systems2 have aided in the decision-making process. It is likely, however, that the identification of risk factors currently not considered in the classification, the use of non-transplant modalities, and, finally, novel transplant approaches will require frequent reassessment of the best treatment strategy.
General Considerations
Until recently few patients above the age of 55 years were offered HCT from allogeneic donors. This policy was based on the increased severity and frequency of transplant-related non-relapse morbidity and mortality (NRM) with increasing age. NRM, such as organ toxicity and infections, was related not only to the intensity of the transplant conditioning regimens but also to graft-versus-host disease (GVHD), which remains the most frequent complication after allogeneic HCT. Even in the most favorable groups of patients overall NRM has been in the range of 25%–30%. A recent analysis used a Markov model to determine the relevance of International Prognostic Scoring System (IPSS) scores2 for the decision as to when patients with MDS should be transplanted. Only patients transplanted from HLA-identical siblings were considered.1 Results suggest that patients in IPSS risk groups intermediate-2 and high (most of whom will have more than 5% myeloblasts in the marrow) will have the best overall life expectancy if they proceed to transplantation without delay (assuming they are candidates to start with). Of course, these data apply to a cohort of patients, but not necessarily to individual patients. Patients with low to intermediate-1 risk disease may have the longest life expectancy if HCT is delayed, maybe by several years, while the disease is closely monitored for progression.1 However, some of these patients may have severe neutropenia or transfusion-dependent thrombocytopenia, and a delay of HCT may not be in their best interest. It is, of course, possible that subgroups of patients will have substantial improvements of their cytopenias with novel non-transplant therapy. It is also important to note that the above decision analysis did not consider factors such as co-morbid conditions, which are likely to affect transplant outcome.3
Since a major problem with more advanced MDS is the risk of post-transplant relapse, one strategy might be to administer pre-transplant “debulking” chemotherapy. However, the role of intensive remission-induction (and consolidation) chemotherapy before HCT has remained controversial. Yakoub-Agha et al showed that patients with secondary MDS who achieved remissions with pre-transplant chemotherapy had a substantially better relapse-free survival after HCT than patients who did not achieve a remission.4 However, patients who were given induction chemotherapy and failed to respond had a lower probability of a successful post-transplant course than would be expected in patients who were not treated pre-transplant. A retrospective analysis of results in patients transplanted at the Fred Hutchinson Cancer Research Center (FHCRC) suggests that pre-transplant chemotherapy reduced the risk of post-transplant relapse but failed to show an advantage for post-transplant relapse-free survival (RFS). These observations suggest that responses to pre-transplant chemotherapy may select for “treatment sensitive” patients who might have fared better post-transplant, even without prior therapy.5 Controlled studies comparing HCT with and with-out prior chemotherapy are necessary to definitively answer the question regarding the role of pre-transplant induction chemotherapy. Such a trial has been initiated by the European Bone Marrow Transplant (EBMT) group. However, as shown in Table 1 , factors other than induction chemotherapy need to be considered, and the decision regarding the optimum strategy may not depend on the disease risk alone but also on the patient age, type of donor, and other features.
Transplant Strategies
Source of stem cells
A large retrospective survey of the EBMT group compared results with marrow and granulocyte colony-stimulating factor (G-CSF)-mobilized peripheral blood progenitor cells (PBPC) for allogeneic HCT from HLA-identical siblings in patients with MDS (total-body irradiation [TBI]- or chemotherapy-based conditioning regimens). The incidence of treatment failure in all MDS subgroups (other than refractory anemia) was lower with PBPC than with marrow,6 similar to our own observation.7 The incidences of acute GVHD with marrow and PBPC were comparable, while chronic GVHD was more frequent with PBPC. A recent analysis from the FHCRC in patients with MDS transplanted with PBPC from related or unrelated donors showed cumulative incidences of acute and chronic GVHD of 80% and 82%, respectively.8 In a concurrent protocol enrolling patients with MDS and other myeloid malignancies, which used an identical transplant regimen but with the addition of Thymoglobulin (THY) pre-transplant, the incidences of acute and chronic GVHD were 44% and 34%, respectively, comparable to what has been achieved with bone marrow as a source of stem cells. Of course, while GVHD per se is undesirable, a greater allogeneic effect of PBPCs may also account for the higher engraftment and lower relapse rate (compared to marrow), particularly in patients prepared with reduced-intensity conditioning regimens (see below).
Importantly, overall results at our Center with transplants from unrelated donors selected on the basis of high-resolution HLA typing have been comparable to those with HLA genotypically identical siblings. In fact, there is evidence of a lower incidence of post-HCT relapse with unrelated donors.
Cellular immunotherapy
While HCT, by definition, is cellular immunotherapy, historically, conditioning regimens were built on the principle that greater intensity would result in greater (leukemic) cell kill and, as a result, lower relapse rates. However, relapses occurred even with regimens that were associated with prohibitive regimen-related morbidity and mortality. Therefore, other strategies were sought. Slavin and colleagues were among the first to show that the administration of viable donor cells after the actual HCT might be effective in preventing recurrence in patients who were at risk for relapse.11 Kolb and colleagues have systematically investigated this strategy and showed recently12 that durable remissions were achieved in patients with high-risk acute myeloid leukemia (AML) or MDS who were conditioned with reduced-intensity regimens and received prophylactic donor lymphocyte infusions.
The use of G-CSF-mobilized PBPC, although developed on the basis of a different rationale, apparently offers stronger graft-versus-leukemia (MDS) effects and greater “vigor” of engraftment,13 albeit at the price of a higher incidence of GVHD, particularly in its chronic form.14 As discussed above, a recent study in patients with MDS and other myeloid diseases suggests that pre-transplant administration of THY is beneficial in reducing the incidence of chronic GVHD in this setting.8
“Conventional” HCT
Low risk/“less advanced” MDS.
The best results with allogeneic HCT are achieved in patients with low myeloblast counts in the marrow (refractory anemia [RA]/RA with ringed sideroblasts [RARS], refractory cytopenia with multi-lineage dysplasia [RCMD], or RCMD with ringed sideroblasts [RCMD-RS]) and without poor-risk clonal cytogenetic abnormalities. The data from the decision analysis discussed above1 suggest that patients with less advanced disease who are eligible for HCT should be followed closely for signs of disease progression in order not to lose the advantage of transplantation during the less advanced phase of the disease. The important point is that as the prognosis without HCT worsens, the probability of a successful transplant also declines.
Sierra et al, on behalf of the International Bone Marrow Transplant Registry (IBMTR), reported results in 452 patients with MDS transplanted from HLA-identical siblings; 140 (31%) had less than 5% marrow blasts at HCT.15 Three-year RFS was age dependent, 72% for patients younger than 18 years and 45% for older patients. For the entire cohort of 452 patients, the 3-year transplant-related mortality (TRM) was 37%, relapse incidence 23%, and RFS 40%. Multivariate analyses showed younger age and platelet counts > 109/L were associated with lower TRM and higher RFS. High marrow blast count, high IPSS risk, and T-cell depletion of transplanted cells increased the risk of relapse 2- to 6-fold. Among 510 patients with MDS transplanted from unrelated donors (National Marrow Donor Program), those conditioned with busulfan (BU) plus cyclophosphamide (CY) [BUCY] fared better than patients prepared with other, generally TBI-containing regimens.16 RFS and relapse rate in patients with RA were 40% and 5%, respectively.16
We used a BUCY regimen in which sequential BU doses (oral administration) were adjusted to maintain steady-state plasma levels of 800–900 ng/mL (targeted BUCY).7 The majority of patients received bone marrow as a source of stem cells. The probability of 3-year RFS was 68% among 69 patients (up to 66 years of age) with RA/ RARS transplanted from HLA-identical sibling donors, and 70% with unrelated donors. NRM (combined for related and unrelated transplants) was 12% at 100 days, and 31% at 3 years; relapse occurred in 5% of patients. Results from that trial are summarized in Table 2 . A recent trial using PBPC as a source of stem cells confirms those data, with 78% RFS at 1 year; however, the incidence of acute GVHD was 85%.8
High risk/“advanced” MDS.
Post-transplant relapse rates of 15% to 80% have been reported in patients with more advanced MDS (≥ 5% marrow myeloblasts; high-risk cytogenetic abnormalities).7,16,17 Studies in the 1980s using CY- and TBI-containing regimens reported 30%–40% RFS. To determine if more intensive conditioning would improve results by lowering the relapse rate, 31 patients with RA with excess blasts (RAEB), RAEB in transformation (RAEB-T), or chronic myelomonocytic leukemia (CMML), to be transplanted from related or unrelated donors at the FHCRC, were prepared with a regimen that combined BU (7 mg/kg), CY (120 mg/kg), and TBI (6 × 200 cGy). Compared to historical controls conditioned with CY (120 mg/kg) and TBI (6 × 200 cGy), the cumulative incidence of relapse was indeed lower (28% vs 54%), but NRM was markedly increased (68% vs 36%), and RFS at 3 years was not improved (23% vs 30%).
The report by Sierra et al, mentioned above,15 also presented results in 312 patients with advanced MDS (RAEB, RAEB-T, CMML). Most of these patients had been conditioned with TBI-based regimens, and all were transplanted from HLA-identical siblings. Risk factors were those discussed above. Compared to patients with < 5% marrow blasts, the relative risk of relapse was 2.9 for patients with 5%–20% blasts, and 6.3 for patients with > 20% blasts. About 75% of all relapses occurred within 12 months of transplantation. RFS was 63% for patients younger than 18 years and 33% for older patients.15 RFS for patients who had been treated with chemotherapy and had <5% marrow blasts at HCT was 55%, compared to 26% in patients with 5% or more myeloblasts. An EBMT trial included 118 patients (69 conditioned with TBI) who received HLA-matched unrelated donor transplants. RFS at 2 years was 27%, 8%, and 27%, respectively, for patients with RAEB, RAEB-T and MDS that had transformed to AML (tAML).18
As CY is not stem cell toxic, another trial of 60 patients with RAEB, RAEB-T, CMML, or tAML (20 related, 40 unrelated donors) used BU plus TBI (without CY).19 The Kaplan-Meier estimate of survival at 3 years was 26%, while the relapse incidence of 25% was comparable to that observed previously with a regimen combining BU + TBI with CY.20 Overall NRM was 38% at 100 days. Particularly disappointing were results with unrelated donors. However, the data showed that CY was not required to achieve engraftment of donor cells, and suggested that high-dose TBI, as used conventionally, may not be the optimum modality for conditioning, given the high TRM.
Reduced-Intensity and Nonmyeloablative Conditioning
In view of the above data, there has been considerable interest in developing less toxic regimens. However, because of concern about increasing the risk of relapse, many investigators have taken a cautious stepwise approach of modifying rather than drastically changing conventional transplant regimens.
Russell et al used intravenous (i.v.) fludarabine (Flu), given over 5 days, and i.v. BU, 3.2 mg/kg, given once a day on 4 consecutive days (concurrently with Flu), combined with THY, 4.5 mg/kg, plus methotrexate (MTX) and cyclosporine (CSP) for GVHD prophylaxis.21 The study enrolled 70 patients with various diagnoses, including MDS, and patients were given marrow or PBPC as a source of stem cells. The day-100 mortality was 2% with related and 8% with unrelated donors. There were 2 cases of graft failure (from unrelated donors). The incidence of acute GVHD was 8%, and chronic GVHD 36%. Projected RFS at 2 years was 74% for low-risk and 65% for high-risk disease.21 As patients with various diagnoses were included in this trial (and several other trials discussed here), results must be interpreted cautiously in regards to the outcome with MDS specifically. A recently concluded FHCRC trial of targeted (oral) BUCY in patients with high-risk MDS also incorporated THY in a dose escalation design.8 While the rates of GVHD observed at FHCRC were higher than in the study by Russell et al, they were lower than in concurrent trials not using THY. NRM at 100 days was 12%, and 1-year RFS 56%.
A trial in 96 patients at the M.D. Anderson Cancer Center, including 22 patients with MDS, used i.v. Flu at 40 mg/m2/day combined with i.v. BU at 130 mg/m2/day for 4 consecutive days (very similar to the Russell study); no THY was administered.22 The incidence of acute GVHD (grades II–IV) was 25% for related and 44% for unrelated transplant recipients. Regimen-related mortality was 5% at 100 days.
Ho et al reported on 62 patients (24 with HLA-identical siblings and 38 with matched unrelated donors) conditioned with a regimen including Flu, BU, and Campath antibody (alemtuzumab) rather than antithyrmocyte globulin.23 Patients with excess myeloblasts had received chemotherapy before transplantation, and response or non-response to this approach may have biased the selection of patients for transplantation. The day-100 NRM was 0% for HLA-identical siblings, and 11% for unrelated donor transplants. The incidence of relapse ranged from 7% to 50% for intermediate-1 to high-risk IPSS groups. There were 26 patients who received donor lymphocyte infusions at a median of 273 days after HCT to induce disease remission or convert to donor chimerism. RFS ranged from 86% for IPSS low-risk patients to 33% among patients with IPSS high-risk MDS. Thus, available data show very encouraging results with Flu/BU regimens of various intensities, which may be further enhanced by the addition of polyclonal or monoclonal antibodies.
Taking yet another approach, Chan and colleagues combined 2 days of photopheresis of the patient with the infusion of pentostatin, 4 mg/m2, as continuous infusion for 2 days, and 3 × 200 cGy of TBI to prepare 18 patients with MDS (all FAB categories) for HCT from related or unrelated donors.24 MTX plus CSP was given as GVHD prophylaxis. Patients were 30–70 (median 54) years old. Sixteen patients achieved full donor chimerism, and all patients survived beyond day 100. Relapse occurred in 2 patients. RFS at 1 year was 64%. Additional studies will be needed to determine the place for this strategy in the treatment of MDS. This approach is now being tested in an Eastern Cooperative Oncology Group (ECOG) Phase II trial.
De Lima and colleagues recently presented a comparison of two regimens: Flu, 120 mg/m2, plus cytosine arabinoside, 4 g/m2, and idarubicin, 36 mg/m2 (FAI), versus Flu 100–150 mg/m2, plus melphalan, 140 or 180 mg/m2 (FM).25 Among 94 patients in this report, 26 had MDS. The more intensive FM regimen was significantly associated with a higher degree of donor cell engraftment and a lower incidence of relapse (30% vs 61%) but also with a higher incidence of TRM (P = 0.036). The 3-year overall survival rates were 30% and 35% for the FAI and the FM regimens, respectively. The result of this retrospective comparison underscores the need for prospective randomized trials.
A more drastic approach at dose reduction was taken by Storb and colleagues, who initially used solely 200 cGy of TBI, subsequently combined with Flu, 3 × 30 mg/m2, for transplant conditioning. One report by this group included 78 patients with MDS (45 related, 33 unrelated transplants; 46 were IPSS low/intermediate-1, and 32 intermediate-2/ high or unknown). Graft failure occurred in 6%, and 43% of patients relapsed. The NRM was 14% at day 100, and 25% at 1 year. Approximately 20% of patients were surviving at 3 years (25% with low-risk, and 10% with high-risk disease).26 An analysis of those data (and results in additional disease categories) suggested that the administration of pre-HCT chemotherapy and low marrow myeloblast counts were associated with more favorable outcome.27 Post-transplant administration of mycophenolate mofetil 3 times a day (instead of twice) also resulted in higher donor cell chimerism and a lower incidence of disease progression, particularly in patients with unrelated donor transplants.27
What is the “best” strategy?
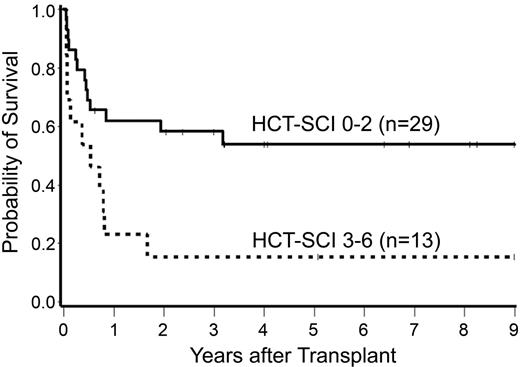
The above data indicate that a standard regimen for allogeneic transplants in patients with MDS (if, indeed, one regimen were suitable for all patients) has yet to be established. In an attempt to provide additional insights, Alyea et al compared results with myeloablative and nonmyeloablative transplants carried out at the Dana Farber Cancer Institute for patients with various diseases.28 There was no significant difference in long-term RFS between the two groups, although the causes of failure differed.28 Scott et al arrived at similar conclusions in an analysis of results in 172 patients with MDS transplanted at the FHCRC.29 It is important to note, of course, that patients conditioned with nonmyeloablative regimens and included in those analyses were enrolled in nonmyeloablative protocols because their advanced age or co-morbid medical conditions30 prevented enrollment on conventional protocols. As illustrated in Figure 1 , pre-HCT co-morbid conditions have a significant impact on transplant outcome. Thus, the patient cohorts considered in the retrospective analyses were not truly comparable. Only prospective randomized trials will be able to answer the important questions as to whether reduction in NRM is achievable without increasing the probability of relapse after reduced-intensity/nonmyeloablative conditioning, and whether such an approach leads to improved RFS.
Post-transplant relapse
Patients with disease recurrence after conventional HCT represent a group of patients in whom reduced-intensity conditioning regimens in preparation for a second transplant deserve to be further explored. Preliminary data suggest, indeed, that such an approach is well tolerated and lasting remissions can be obtained.29
Treatment-related (secondary) MDS
Secondary MDS remains a difficult disease to treat. While HCT is the only modality that offers long-term success, results to date have been less than encouraging. Chemo-radiotherapy given for the patients’ original disease compromises their ability to tolerate HCT. Of particular interest in this context is MDS after autologous HCT for non-Hodgkin lymphoma (NHL), which has been reported to occur in as many as 10% of patients by 10 years after autologous HCT.31 In one report, RFS at 2 years after allogeneic HCT for patients with secondary MDS was 28%, and NRM was 49%.4 We analyzed results in 111 cases transplanted at the FHCRC and observed a 5-year RFS of 8% for patients conditioned with high-dose TBI, and 30% for patients prepared with a targeted (oral) BUCY regimen.32 The incidence of relapse was disease stage dependent, and was 0% for patients with < 5% marrow blasts, and 40% for patients with > 20% blasts.
Conclusions and Outlook
HCT offers potentially curative therapy for patients with MDS. Results have improved progressively over the past decade. Regimens not incorporating high-dose TBI appear to be better tolerated than high-dose TBI regimens, primarily owing to a reduction in TRM. A broad scale of regimens, ranging from “modified” conventional to reduced-intensity to nonmyeloablative regimens, has been developed; one size does not appear to fit all. Rather, patient age, co-morbid conditions, disease stage, non-transplant chemotherapy, type of donor, source of stem cells, and possibly other factors, all affect the decision regarding transplantation and impact on outcome. GVHD and post-HCT relapse remain problems. The availability of new non-transplant modalities may affect the timing of HCT. Conceivably, some of those agents could be incorporated into transplant conditioning regimens. Prospective randomized trials in regards to the importance of pre-transplant therapy and the type of transplant regimen are needed.
Impact of pre-transplant co-morbidity score on post-transplant survival in 42 patients with chronic myelomonocytic leukemia (CMML).33
Impact of pre-transplant co-morbidity score on post-transplant survival in 42 patients with chronic myelomonocytic leukemia (CMML).33
Fred Hutchinson Cancer Research Center and the University of Washington, Seattle, WA, USA
Supported by grants HL36444 and CA87948, National Institutes of Health, Bethesda, MD, USA
Acknowledgments: I would like to thank Bonnie Larson and Helen Crawford for help with manuscript preparation. Thanks to Michael Maris, MD, for his input to Table 1.