Abstract
Transfusion-associated acute lung injury (TRALI) has emerged as a leading cause of transfusion-related morbidity and mortality. TRALI is characterized by acute non-cardiogenic pulmonary edema and respiratory compromise in the setting of transfusion. The study of TRALI has been hampered by inadequate case definitions and an incomplete understanding of the pathologic mechanisms. Recent consensus conferences took an important first step by providing a framework for case definition. Recent advances in the understanding of the pathogenesis of TRALI have also occurred. TRALI has been primarily attributed to donor leukocyte antibodies that are thought to interact with recipient neutrophils, resulting in activation and aggregation in pulmonary capillaries, release of local biologic response modifiers causing capillary leak, and lung injury. An alternate mechanism termed the “two hit” or “neutrophil priming” hypothesis postulates that a pathway to neutrophil activation and aggregation can occur without leukocyte antibodies. A first event such as sepsis or trauma can induce pulmonary endothelial activation, release of cytokines, and priming of neutrophils. A subsequent second event such as exposure to lipids, cytokines or antibodies in a blood component would then cause activation of adherent neutrophils and a release of bioreactive molecules leading to lung injury. There are limited clinical and animal studies to support the “two hit” model. These proposed mechanisms are not mutually exclusive in that donor leukocyte antibody can be pathogenic in both models and have implications for new strategies to prevent TRALI.
Advances in blood safety have greatly reduced the risk of transfusion-associated infectious disease transmission. As a result, noninfectious serious hazards of transfusion have come to the forefront as increasingly important blood safety issues. Transfusion-associated acute lung injury (TRALI) has emerged as a leading cause of transfusion related morbidity and mortality.1 This report will summarize recent consensus conferences that have provided practical clinical definitions of TRALI to aid the clinician in diagnosis and to facilitate its study. Recent advances in understanding of the pathogenesis of TRALI will be presented with a potential unifying hypothesis.
Definition
A lack of a standardized definition of TRALI has hindered accurate clinical diagnosis, epidemiology, and research investigation. A recent NHLBI working group convened to identify research needs addressed this critical issue by providing the following definition: “new acute lung injury (ALI) occurring during or within 6 hours after a transfusion, with a clear temporal relationship to transfusion, in patients without or with risk factors for ALI other than transfusion.”2 Limitations to the proposed NHLBI working group definition are the exclusion of patients with preexisting ALI, excluding cases with onset more than 6 hours after transfusion, lack of laboratory diagnostic criteria, and a required severity of hypoxia that would miss cases of mild TRALI. A subsequent Canadian consensus conference in April 2004 further modified the NHLBI working group criteria for TRALI2,3 (Table 1 ). The modified criteria broadened the definition of hypoxia from pulse oximetry to include clinical evidence (introducing some subjectivity) and created a category of “possible TRALI” to address cases in which patients have other risk factors for ALI temporally related to transfusion such as septic shock, sepsis syndrome without shock, aspiration, near drowning, disseminated intravascular coagulation, trauma, pneumonia, drug overdose, fracture, burns, and cardiopulmonary bypass.2 While the participants acknowledge that subtle cases may not meet the definition, the great majority of clinically significant cases should be captured. The Canadian consensus conference criteria represent an important advance that provides the framework from which evidence-based modifications will evolve.
Clinical and Laboratory Diagnosis
TRALI has a clinical presentation mirroring ARDS occurring in the setting of transfusion. Patients present with respiratory distress (dyspnea), hypoxia, pulmonary edema on exam, and bilateral fluffy infiltrates on chest x-ray during or within 6 hours of transfusion. The majority of cases occur during or within 1 to 2 hours of transfusion.4 Signs and symptoms include: tachypnea, frothy pulmonary secretions, hypotension (less commonly hypertension), fever, tachycardia and cyanosis. All patients require supplemental oxygen and the majority of patients require intubation with ventilatory support. Importantly, there is no evidence of circulatory overload with absence of jugular venous distension or an S3 gallop. Central venous pressure and pulmonary wedge pressure is normal. B-natriuretic peptide (BNP) may have some value in distinguishing transfusion-associated circulatory overload from TRALI.5 Circulatory overload is suggested by an absolute BNP level greater than 100 pg/dL and a posttransfusion-to-pretransfusion ratio greater than 1.5.5 In contrast to ARDS from other causes, patients typically recover with resolution of pulmonary infiltrates within 96 hours. The mortality rate has been reported to be between 5% and 10%.6 Laboratory findings in the acute setting are of limited value because they are suggestive but not diagnostic of TRALI. Such findings include: leukopenia, neutropenia, monocytopenia and hypocomplementemia.1,7 Laboratory tests that strongly support the clinical diagnosis of TRALI include the demonstration of HLA class I or class II, or neutrophil-specific antibodies in donor plasma and the presence of the cognate (corresponding) antigen on recipient neutrophils. (See section on Immune-Mediated TRALI.) Such testing typically takes days or weeks, thus making TRALI primarily a clinical diagnosis with confirmation based on subsequent test results. Tests for lipid-priming activity or neutrophil-activating factors are only available on a research basis.
Incidence of TRALI and Implicated Blood Components
The true incidence of TRALI is unknown because a standardized definition has not previously been available. Early reports quoted an incidence of 1:5,000 blood components4 with subsequent reports ranging from 1:432 whole blood platelets to 1:557,000 red cells.1 Such wide discrepancies illustrate the importance of having a consensus definition in defining the incidence of TRALI. It has clearly emerged as a leading cause of transfusion-related morbidity and mortality representing the leading cause reported to the FDA in 2003.1 TRALI has been reported from all types of blood components including whole blood, red cells, apheresis platelets, whole blood platelets, fresh frozen plasma, cryoprecipitate, granulocytes, stem cell products and even intravenous immunoglobulin preparations.8 FFP has been implicated most frequently in TRALI cases and TRALI-related deaths reported to the FDA9 and UK.10 Most implicated blood products contain more than 50 mL of plasma.1
Pathophysiology of TRALI
The exact mechanism of TRALI is not fully understood but is likely to be multifactorial. An immune antibody-mediated mechanism has been implicated in most cases of TRALI. In a minority of reported cases, however, an antibody is not identified and a nonimmune mechanism has been postulated. Data from animal models of TRALI and more recent clinical data have suggested that both mechanisms occur and that TRALI may represent the final common pathway of neutrophil activation and capillary leak, which can be triggered by antibodies and/or other biologic response modifiers.
Immune (Antibody)-mediated TRALI
In 65–90% of reported clinical cases of TRALI, leukocyte antibodies have been identified in the implicated donor.4,10–13 The cognate antigen can be identified on the recipient’s neutrophils in most of these cases.4,13 Antibodies that have been implicated in TRALI include donor HLA class I, HLA class II, and/or neutrophil-specific antibodies.1,4,11–14 Although a number of neutrophil-specific antibodies have been reported, the most common is directed at the 5b (HNA-3a) antigen.6,15 In a small percent of cases, the leuko-agglutinating antibody appears to be from the recipient and is directed at the transfused neutrophils.16–18 Most of the donors implicated in TRALI have been multiparous women who became alloimmunized during pregnancy. The frequency of sensitization to HLA class I and class II correlates with parity, with 2–8%, 10–15%, and 17–26% identified in women with zero, 1–2, or ≥ 3 pregnancies, respectively.19,20 Alloimmunization to neutrophil-specific antigens is much less frequent (0.1–1.8%).20,21 These studies, however, probably underestimate the frequency of HLA and neutrophil antibodies due to use of less sensitive testing methodology, e.g., lymphocytotoxicity vs flow cytometry.14,22 Passive transfer of these leukoagglutinating anti-bodies via transfusion of plasma containing blood components results in binding to recipient neutrophils. Antibody-bound neutrophils are activated and sequestered in the lungs where complement activation and release of neutrophil bioactive products results in endothelial damage, capillary leak and ALI. HLA class II antigens are also expressed on monocytes and may contribute to TRALI.12 The immune model is supported by both clinical data and animal models. Seeger et al23 developed a rabbit ex-vivo lung model for TRALI. Lung injury was observed when isolated lungs were perfused with human HNA-3a(5b) positive neutrophils followed by anti-5b and a source of complement but not in the absence of anti-5b, use of 5b negative neutrophils or with control rabbit plasma. A recently published ex-vivo rat model found that lung injury occurred in rats perfused with human neutrophils followed by administration of the neutrophil antibody with HNA-2a specificity independent of the presence of complement.24 When neutrophils with < 30% expression of anti-HNA-2a were used, the injury was greatly attenuated. Similar results were found in a recent in-vivo mouse model that demonstrated acute lung injury and increased mortality when a monoclonal MHC-I antibody was infused into mice with the cognate antigen.25 The lung injury was dependent on neutrophil expression of Fcγ receptors and was prevented in mice depleted of neutrophils by using antigranulocyte antibodies.25 These animal models demonstrate that HLA or HNA antibodies can induce neutrophil-mediated acute lung injury when the cognate antigen is present and that complement is not a requirement.
A large body of circumstantial clinical evidence links TRALI to leukocyte antibodies by virtue of their presence in the great majority of reported cases. Other supportive clinical data include a prospective randomized crossover study of two units of plasma from multiparous donors (≥ 3 live births) versus control plasma in 105 intensive care patients.26 This study found that patients who received study plasma had impaired lung function as evidenced by a decrease in PaO2:FiO2 ratio versus controls. Dykes et al27 reported TRALI in a single lung transplant recipient after a red cell transfusion containing HLA-B44 antibodies. Lung injury was found only in the B44-positive transplanted lung but not in the B44-negative native lung. Lastly Kao and Wood22 performed immunohistochemical staining of lung tissue from a fatal TRALI case attributed to HLA class II antibody. Immunostaining revealed immunoreactive neutrophils lining alveolar capillaries in the study patient but not in controls. Endothelial activation in areas of neutrophil aggregation was also found as evidenced by high expression of the adhesion molecules CD31 and CD34.22 Thus clinical data and animal data support an immune mechanism mediated by leukocyte antibodies as etiologic events in TRALI.
Non-immune Mechanism for TRALI
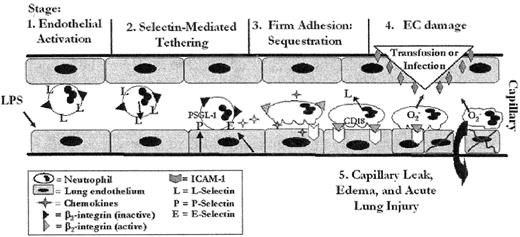
Despite the strong experimental and clinical evidence supporting an immune mechanism for TRALI, there are inconsistencies. First, antibodies have not been found in 15% or more of cases of TRALI.6 The use of more sensitive assays for HLA or neutrophil antibodies or identification of antibodies to other cell types such as monocytes12 or lymphocytes13 may explain some of these cases. Second, although HLA antibodies are commonly found in female donors, only a very small proportion of these donors are implicated in TRALI. Third, donors with known HLA antibodies transfused to patients with the cognate antigen caused lung injury in some patients but not others.28,29 Fourth, patients who have experienced TRALI reactions do not always have the cognate antigen to leukocyte antibodies found in the implicated donor.12 A non-immune mechanism for TRALI has been proposed to explain these limitations. A “two hit” model has been proposed by Silliman et al,30,31 which postulates that an initial insult to vascular endothelium results in endothelial activation, release of cytokines, and expression of adhesion molecules. Cytokines attract and prime neutrophils, which firmly adhere to the endothelium. Events that could cause the initial pro-inflammatory endothelial activation include severe infection, surgery, trauma, or massive transfusion. A second “hit” activates sequestered adherent neutrophils to release oxidases and proteases, which damage the endothelium causing capillary leak and acute lung injury (Figure 1 ). The second “hit” may be mediated by transfusion of biologic response modifiers such as leukocyte antibodies, lipid priming molecules,32,33 cytokines, CD40 ligand34 or endotoxin. Animal studies have provided support for this hypothesis. An ex-vivo rat model demonstrated ALI when rats were infused with endotoxin (first hit) and then followed with plasma from stored but not fresh platelet33 or red cells.32 Silliman showed that infusion of lipids (lysophosphatidylcholines) extracted from the plasma supernatant of stored but not fresh platelets also caused ALI, demonstrating lipid-priming activity as an important causative agent in stored blood components. Sachs et al24 used a similar ex-vivo rat model to show that rats infused with human HNA-3a (5b)+ neutrophils and then stimulated with formyl-Met-Leu-Phe (fMLP) as a first “hit,” develop ALI when infused with anti-5b antibodies. Clinical studies also provide support for a nonimmune mechanism. A nested case controlled study of 46 TRALI cases due to whole blood platelet concentrates found the same incidence of leukocyte antibodies in control donor components versus those implicated in TRALI.35 Furthermore, components implicated in TRALI had greater plasma-priming activity compared to components not implicated in TRALI. A smaller retrospective study of 10 consecutive patients with TRALI found HLA or granulocyte antibodies in donors in only 50% of cases and a predisposing event in all 10 patients.36 In this study greater lipid-priming activity was found in the plasma of patients with TRALI compared to controls or the patient’s pretransfusion samples. One limitation of the “two-hit model” is the appearance of TRALI in patients who were apparently healthy prior to transfusion such as in the setting of coumadin reversal for elective surgery.29 It is possible that such patients have subclinical evidence or unrecognized risk factors for endothelial activation. Alternatively, a transfused component may be able to provide both the mediators of endothelial activation and the second hit bioactive molecules that activate neutrophils triggering ALI.
Prevention of TRALI
In the US, measures to prevent TRALI are currently limited to deferral of donors implicated in a TRALI case. Typically, implicated donors with a history of pregnancy or transfusion are screened for HLA or neutrophil antibodies. The AABB recently issued a standard in the 24th edition of Standards for Blood Banks and Transfusion Services requiring that donors implicated in a TRALI case be evaluated for eligibility to donate.37 In practice, donors found to have leukocyte antibodies corresponding to an antigen on patient leukocytes or exhibiting a positive crossmatch between donor serum and patient leukocytes are deferred from donating plasma containing blood components. The use of fresher platelets or red cells with reduced lipid priming activity1 or washed components has also been considered. One strategy that is gaining favor is to use plasma exclusively or primarily from male donors and divert plasma from female donors to recovered plasma that is only used for fractionation and production of plasma derivatives. The UK adopted this strategy in October 2003 with full implementation in January 2004. The UK Serious Hazards of Transfusion (SHOT) 2004 data showed that TRALI cases due to plasma dropped from 14 cases in 2003 to 6 cases, with no cases from plasma after January 2004.10 American Red Cross data from 2003 to 2006 show that 76% of all reported TRALI-related fatalities from plasma involved antibody-positive female donors (Anne Eder, MD, personal communication). These data suggest that diversion of female plasma may substantially reduce the number of TRALI cases. A similar strategy for platelets would be very difficult to implement due to supply limitations and has recently been addressed in the UK by resuspending platelet pools in male plasma. Variations of this strategy would be to divert plasma only from donors with a history of pregnancy or transfusion or to test female donors for leukocyte antibodies. The Retrovirus Epidemiology in Donors II (REDS II) NHLBI funded research network is about to launch a large study of HLA and leukocyte antibody prevalence in blood donors (LAPS) with a history of pregnancy or transfusion to provide a basis for rational decisions regarding donor management. The use of platelet additive solutions may be another practical way to reduce the plasma content and risk of TRALI from platelet components.
Summary
TRALI has emerged as leading cause of transfusion-related morbidity and mortality. Recently developed consensus clinical definitions will help provide consistency in identifying TRALI cases, facilitate establishing the true incidence of TRALI, and provide a framework from which laboratory and clinical studies can be performed. Such data will contribute to the development of rational strategies to reduce the risk of TRALI.
The two-event model of acute lung injury (ALI).
The stimulus (endotoxin = LPS) for proinflammatory endothelial activation comes from the intravascular space resulting in firm adherence of PMNs through: (1) slowing of vascular flow and L-selectin–mediated loose attachment and P- and E-selectin–induced tethering and (2) chemokine-induced firm adhesion and sequestration of PMNs. These firmly adherent, sequestered PMNs may be activated by a second agonist (3), the infusion of specific antibodies directed against granulocyte antigens or biologic response modifiers resulting in activation of PMNs endothelial damage (4), capillary leak, and ALI (5).
Reprinted with permission from Silliman CC, Kelher M. Transfusion. 2005 (suppl);45:109S-16S.
The two-event model of acute lung injury (ALI).
The stimulus (endotoxin = LPS) for proinflammatory endothelial activation comes from the intravascular space resulting in firm adherence of PMNs through: (1) slowing of vascular flow and L-selectin–mediated loose attachment and P- and E-selectin–induced tethering and (2) chemokine-induced firm adhesion and sequestration of PMNs. These firmly adherent, sequestered PMNs may be activated by a second agonist (3), the infusion of specific antibodies directed against granulocyte antigens or biologic response modifiers resulting in activation of PMNs endothelial damage (4), capillary leak, and ALI (5).
Reprinted with permission from Silliman CC, Kelher M. Transfusion. 2005 (suppl);45:109S-16S.
Director, Division of Transfusion Medicine; Department of Pathology, University of Pittsburgh Medical Center