Abstract
Most patients with myelodysplastic syndrome eventually become dependent on regular red cell transfusions. This dependency has a negative impact on clinical outcome, primarily because it may be associated with more severe marrow failure. In addition, however, transfusion dependency may involve clinical consequences of chronic anemia and iron overload. Although transfusion iron is primarily taken up by the reticuloendothelial cells, the metal is later redistributed to parenchymal cells. This redistribution is modulated by several factors, including the degree of ineffective erythropoiesis through its suppressive effect on hepcidin production. Body iron status is routinely assessed by serum ferritin and transferrin saturation, but there is a need of reliable tools for locating iron accumulation in patients. Magnetic resonance imaging T2* provides a non-invasive method for detecting and quantifying both liver and myocardial iron overload. Clinical consequences of parenchymal iron overload have been reported not only in thalassemia major, but also in patients with myelodysplastic syndrome. Transfusion-dependent patients with isolated erythroid dysplasia and low risk of leukemic evolution are more likely to develop parenchymal iron overload and its toxicity, and therefore may benefit from chelation therapy. There may also be a benefit of chelation therapy in patients with transfusion iron overload undergoing allogeneic stem cell transplantation. Deferoxamine and deferasirox are currently available for treatment of transfusion iron overload in patients with myelodysplastic syndrome.
Introduction
Due to our uniquely limited iron absorption and excretion, we are the only species that has difficulties in maintaining iron balance.1 More than 500 million persons throughout the world have iron deficiency,2 while hereditary hemochromatosis is the most common genetic disorder among Caucasians.3 The absence of an active iron excretion system represents a major problem in patients receiving regular red cell transfusions, since progressive iron loading inevitably occurs. Untreated iron overload from transfusions is responsible for morbidity and mortality in patients with thalassemia major,4,5 but clinical consequences have been reported also in nonthalassemic adults with anemias requiring regular transfusions.6 This article will examine the clinical relevance of anemia and transfusion iron overload in patients with myelodysplastic syndrome.7
Physiology of Iron Storage and Reticuloendothelial Iron Recycling: Reticuloendothelial Versus Parenchymal Iron Overload
Storage iron is deposited in the body as ferritin and hemosiderin. Cytoplasmic ferritin has ubiquitous distribution among living species and plays a key role in body iron metabolism through its dual functions of iron detoxification and iron reserve.8 Degradation of ferritin occurs within membrane-encapsulated lysosomes (siderosomes) and generates hemosiderin, which is an aggregated and partially denatured form of cytoplasmic ferritin.
Reticuloendothelial cells (macrophages in the bone marrow and spleen, Kupffer cells in the liver) and hepatocytes are two major areas of iron storage in humans. Macrophages receive their iron from the phagocytosis of non-viable or senescent red blood cells (Figure 1; see Color Figures, page 501). Heme is catabolized by heme oxygenase 1, and the processed iron is either rapidly recycled to the plasma through the iron exporter ferroportin, or is stored in cytoplasmic ferritin. Plasma ferritin is a byproduct of cytoplasmic ferritin, glycosylated and secreted through the Golgi apparatus.9 Within macrophages, ferroportin expression is induced by heme at the level of gene transcription, and by iron at the translational level.10 However, ferroportin expression, and therefore iron export, is mainly regulated on the macrophage surface (Figure 1; see Color Figures, page 501). Hepcidin, a small peptide produced in the liver,11 blocks cellular iron efflux by binding to and inducing the degradation via internalization of ferroportin.12 Hepcidin synthesis is regulated by iron stores through the bone morphogenetic protein (BMP) signaling pathway,13,14 being increased by iron loading and suppressed by iron deficiency. Additionally, hepcidin production is decreased by anemia and hypoxia.15,16 Recent studies have identified a novel physiological regulator of hepcidin production, matriptase-2, a transmembrane serine protease encoded by the gene TMPRSS6.17,18 Matriptase-2 appears to be a physiological inhibitor of hepcidin production, and mutations in TMPRSS6 are responsible for familial iron deficiency anemia.19,20
The hepcidinferroportin interaction that takes place both at the enterocyte and macrophage level is central to iron metabolism in humans, as regulatory molecules that control body iron homeostasis mainly act by modulating this interaction. The complexity of this pathway also explains the genetic and clinical heterogeneity of hereditary hemochromatosis.21,22
The hepatocyte takes up iron from transferrin in amounts that vary according to the saturation of the plasma carrier molecule.23 This relationship is explained in part by the greater iron donating capacity of diferric as compared with monoferric tranferrin.24
The distinction between reticuloendothelial and parenchymal iron overload is not merely academic but has considerable clinical impact. Selective accumulation of iron in reticuloendothelial cells is relatively safe, as best illustrated by patients with ferroportin disease showing isolated iron accumulation in the Kupffer cells on liver biopsy.25 By contrast, the iron deposited in parenchymal cells is extremely toxic. While the liver is the most reliable indicator of parenchymal iron overload, cardiac dysfunction is the most lethal effect of iron toxicity.1
Erythroid Activity, Hepcidin Production, Iron Absorption and Reticuloendothelial Iron Recycling in Anemic Patients
Under physiological conditions, most of the plasma iron turnover derives from macrophage iron recycling, which amounts to about 20 mg per day in the normal adult. As shown in Figure 1 (see Color Figures, page 501), the ferroportin/hepcidin interaction regulates reticuloendothelial iron efflux. Among several factors that modulate hepcidin production by the hepatocyte, an important role in anemic patients is likely played by the erythroid marrow itself, perhaps by the degree of ineffective erythropoiesis.
Erythroid marrow activity varies considerably in anemic patients, being almost undetectable in aplastic anemia and several times normal in patients with thalassemia.26 Expanded, but ineffective, erythropoiesis represents the major factor responsible for anemia in congenital and acquired conditions characterized by cytoplasmic or nuclear maturation defects27 that lead to the premature death via apoptosis of immature nucleated red cells in the bone marrow.28 However, the mechanisms driving ineffective erythropoiesis are insufficiently understood, as shown by a recent study in mouse models that mimic β-thalassemia intermedia.29
Congenital anemias due to ineffective erythropoiesis are frequently associated with a marked increase in dietary iron absorption and progressive iron loading, and are defined as “iron loading anemias.” Iron loading occurs particularly in patients with X-linked sideroblastic anemia, congenital dyserythropoietic anemia and thalassemia intermedia.30,31 The mechanism by which the erythroid marrow expansion, combined with ineffective erythropoiesis (and therefore with excessive apoptosis of immature red cells), induces a positive iron balance32 has been debated for years. Finch33 introduced the concept of the “erythroid regulator” of iron balance, defining it in physiologic terms at that time.
The identification of the ferroportin/hepcidin axis has facilitated studies of effects of erythroid activity on iron balance so erythroid regulator(s) can be better defined. Studies in mouse models of β-thalassemia intermedia have shown that ineffective erythropoiesis is characterized by increased iron absorption mediated by downregulation of hepcidin and upregulation of ferroportin.34 In this model, ineffective erythropoiesis was also able to override the expected increase in hepcidin expression due to high liver iron concentration.
Miller and coworkers35 performed studies to test the hypothesis that the release of the BMP/TGF-β superfamily members during the process of ineffective erythropoiesis might interfere with hepcidin production, at least in thalassemia. They found that GDF15 serum concentration was highly increased in patients with β-thalassemia syndromes, and that GDF15 serum levels were directly related to serum erythropoietin and soluble transferrin receptor levels. In addition, serum from thalassemia patients suppressed hepcidin mRNA expression in primary human hepatocytes, but this suppressive effect disappeared following depletion of GDF15.
In patients with β-thalassemia intermedia, a strong inverse relationship was observed between urinary hepcidin levels and both serum erythropoietin and soluble transferrin receptor protein, markers of erythropoietic activity.36 Urinary hepcidin values were significantly higher in patients with β-thalassemia major, whose soluble transferrin receptor levels were significantly lower than those of patients with β-thalassemia intermedia, indicating lower erythroid activity and lower ineffective erythropoiesis. Liver biopsies from patients with thalassemia intermedia showed iron deposition mainly in the hepatocytes, with deposition in rare Kupffer cells.36 By contrast, liver biopsies from patients with thalassemia major showed massive iron deposition in the majority of Kupffer cells. These observations suggest that in thalassemia intermedia the expanded erythroid marrow and the high degree of ineffective erythropoiesis inhibit hepcidin production. This not only results in increased absorption of dietary iron, but also in accelerated macrophage iron recycling. Interestingly, serum ferritin was markedly lower in patients with β-thalassemia intermedia than in those with β-thalassemia major, indicating that the circulating ferritin mainly derives from reticuloendothelial cells and might more accurately reflect reticuloendothelial than parenchymal iron load.36
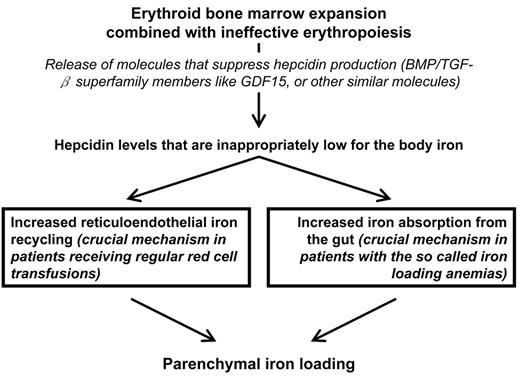
Although the molecular mechanisms still need to be defined, the above observations establish a link between ineffective erythropoiesis and suppression of hepcidin production, as illustrated in Figure 2 . According to this model, increased absorption of dietary iron plays a major role in the pathophysiology of iron loading anemias.31 By contrast, increased reticuloendothelial iron recycling is likely the major mechanism of parenchymal iron loading in anemic patients receiving regular blood transfusions.
Pathogenesis and Prognostic Significance of Anemia in Myelodysplastic Syndromes
Myelodysplastic syndromes show impressive clinical heterogeneity, ranging from indolent conditions spanning years to forms with a rapid evolution into acute myeloid leukemia.7 The vast majority of these patients present with anemia, and many of them become transfusion dependent in the long term.37
Variable pathogenetic mechanisms are responsible for anemia in myelodysplastic syndromes. Several years ago, we studied these mechanisms by means of ferrokinetics.38,39 Patients with refractory anemia with ringed sideroblasts had high erythropoietic activity, which was largely ineffective, while patients with multilineage dysplasia or with excess blasts showed relative erythroid marrow failure, i.e., an erythropoietic effort inadequate for the degree of anemia.26,40 Intermediate patterns were observed with patients with refractory anemia.
The pathogenesis of refractory anemia with ringed sideroblasts is therefore similar to that of the so-called iron loading anemias,30,41 as ineffective erythropoiesis plays a major role in its production. Mitochondrial iron overload may be related to the excessive apoptosis of immature red cells in this condition. The iron deposited in perinuclear mitochondria of ringed sideroblasts is present in the form of mitochondrial ferritin,42 and the aberrant mitochondrial ferritin expression occurs at a very early stage of erythroid differentiation and is paralleled by an upregulation of genes involved in this process.43 CD34+ cells from patients with refractory anemia with ringed sideroblasts have a peculiar gene expression profile characterized by upregulation of mitochondria-related genes and, in particular, of those of heme synthesis.44 By contrast, one downregulated gene is ABCB7, encoding a transporter that functions to enable transport of iron from the mitochondria to the cytoplasm.45 Germline mutations in ABCB7 are responsible for X-linked sideroblastic anemia and ataxia.46 Thus, refractory anemia with ringed sideroblasts is a clonal stem cell disorder characterized by mitochondrial iron accumulation, excessive apoptosis of immature red cells, and ineffective erythropoiesis.41
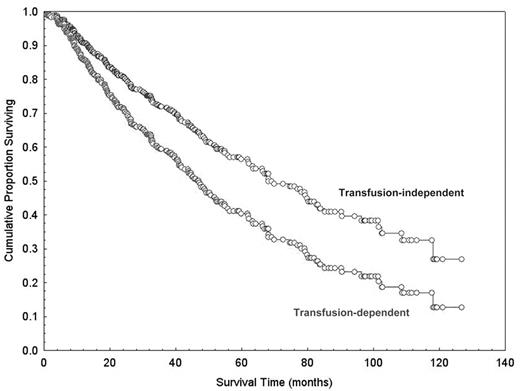
In patients with myelodysplastic syndrome, dependency on transfusions has an effect on the likelihood of survival.7 We examined 374 patients given a diagnosis of myelodysplastic syndrome at the Fondazione IRCCS Policlinico San Matteo, Pavia, Italy, between 1992 and 2002. As shown in Figure 3 , once a regular need for blood transfusion developed, patients had a significantly lower probability of survival. This observation has been recently confirmed by Kao and coworkers47 in a study performed using the original International MDS Risk Analysis Workshop (IMRAW) database that led to the definition of the International Prognostic Scoring System (IPSS).48 The aim of the study was to determine whether different degrees of anemia, thrombocytopenia, and neutropenia were of additional prospective prognostic value for the IPSS. Only anemia at diagnosis was of additive prognostic value to IPSS in terms of overall survival, and this independently stratified patients within the intermediate IPSS risk categories (Int-1 and Int-2 risk groups). Specifically, patients with hemoglobin levels ≤ 10 g/dL had a lower life expectancy than those with hemoglobin levels higher than 10 g/dL.
Several mechanisms may explain the negative impact of severe anemia on the clinical outcome of patients with myelodysplastic syndrome.49 First, the severity of anemia likely reflects inherently poorer marrow function and higher risk of leukemic evolution. Second, chronic anemia is known to be associated with increased mortality and morbidity per se in community-dwelling older adults and patients with chronic heart failure.50 Furthermore, cardiac dysfunction can result from transfusion iron overload developing in adulthood.6,51
Life Expectancy in Myelodysplastic Syndromes According to WHO Criteria and WHO Classification-Based Prognostic Scoring System
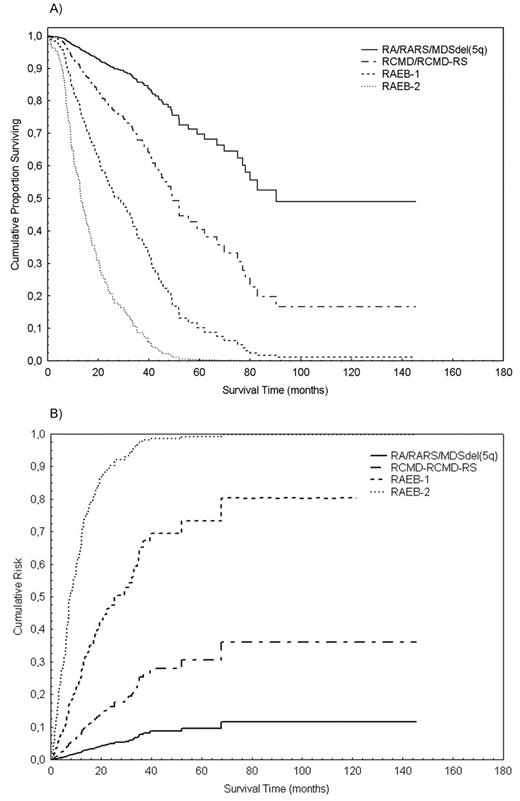
We have previously shown that the WHO classification of myelodysplastic syndromes has a relevant prognostic value.37,52 In particular, among patients without excess blasts, isolated involvement of the erythroid lineage (refractory anemia, refractory anemia with ringed sideroblasts) rather than bi- or tri-lineage marrow dysplasia (refractory cytopenia with multilineage dysplasia) is associated with a significantly better prognosis in terms of both overall survival and leukemia-free survival. A time-dependent analysis of overall survival and risk of leukemic evolution in patients with myelodysplastic syndrome classified according to WHO criteria is reported in Figure 4 .
Based on the WHO classification and transfusion dependency, we defined a WHO classification-based prognostic scoring system (WPSS) (Table 1 ) that is able to classify patients into five risk groups.52 WPSS is a dynamic prognostic scoring system that provides an accurate prediction of survival and risk of leukemic evolution in patients with myelodysplastic syndrome at any time during the course of their disease, and can be used for clinical decision-making. For instance, WPSS predicts post-transplantation outcome in patients with myelodysplastic syndrome.53 It has been also found to predict the outcome of patients with myelodysplastic syndrome with deletion 5q more clearly than IPSS.54 As a time-dependent prognostic scoring system, WPSS can be used to define the risk of parenchymal iron loading in patients receiving regular blood transfusions, as discussed below.
Clinical Consequences of Transfusion Iron Overload in Patients with Myelodysplastic Syndrome
Clinical consequences of transfusion iron overload in nonthalassemic adults had been previously reported by Schafer and coworkers.6 These authors also reported that long-term deferoxamine iron chelation therapy was effective not only in retarding but even reversing organ damage caused by parenchymal iron overload.55
In a study of the natural history of refractory anemia with ringed sideroblasts,51 we found that mild iron overload was a common feature at presentation, but produced clinical manifestations of hemochromatosis only in those patients who subsequently had a regular need for blood transfusions. Complications of iron overload were the most common causes of death.51
More recently, we studied the effect of transfusion dependency and secondary iron overload on survival of patients with myelodysplastic syndrome classified according to WHO criteria.37,56,57 Overall, transfusion dependency was found to significantly worsen the probability of surviving and to increase the risk of progressing to leukemia in patients with myelodysplastic syndrome. An inverse relationship was observed between severity of transfusion requirement and probability of surviving. The negative impact of transfusion dependency was more pronounced in patients with refractory anemia, refractory anemia with ringed sideroblasts, and myelodysplastic syndrome with isolated deletion 5q. Overall, the most common non-leukemic cause of death was cardiac failure.
Transfusion iron overload, as assessed by serum ferritin, was associated with worse survival in patients receiving regular red cell transfusions.57 The effect of iron overload was mainly noticeable among patients with refractory anemia, who have a median survival of more than 5 years and are more prone to develop long-term toxicity of iron overload.
These observations indicate that the development of secondary iron overload per se worsens the survival of subgroups of transfusion-dependent patients with myelodysplastic syndrome. These subgroups include patients with myelodysplastic syndrome with isolated erythroid dysplasia, like refractory anemia or refractory anemia with ringed sideroblasts, and those with myelodysplastic syndrome with isolated 5q deletion, a condition that has a benign clinical course despite multilineage involvement.58
Iron overload in patients with myelodysplastic syndrome undergoing allogeneic stem cell transplantation may be associated with adverse outcome. Findings of a retrospective, single-institution study suggest that iron overload significantly contributes to treatment-related mortality.59 This was previously observed in patients with thalassemia major.60
Diagnostic Tools for Assessing Parenchymal Iron Overload in Patients with Myelodysplastic Syndrome
The diagnostic tools currently available for the evaluation of body iron status in patients with myelodysplastic syndrome receiving regular blood transfusions are reported in Table 2.
Serum ferritin is routinely employed for assessing levels of storage iron and effects of chelation therapy in subjects regularly transfused.61,62 In these patients, elevated serum ferritin is the result of the combined effects of increased ferritin synthesis in reticuloendothelial cells and the release of intracellular ferritin from damaged parenchymal cells, e.g., hepatocytes.63 The relative contributions of these sources of serum ferritin in transfusion iron overload may vary considerably.
Transferrin saturation represents the most practical test for defining the site of iron accumulation, in particular for distinguishing between reticuloendothelial and parenchymal iron overload.1 A high value for transferrin saturation suggests parenchymal iron loading.
The liver iron concentration (LIC) is a reliable indicator of total body iron stores in patients with thalassemia major,64 and liver iron biopsy with iron measurement by atomic absorption spectroscopy remains the gold standard for the assessment of liver iron concentration in these patients.65 However, liver biopsy is invasive and cannot be employed in many patients with myelodysplastic syndromes, especially for serial assessments.
Non-invasive techniques such as superconducting quantum interference device (SQUID)66 and magnetic resonance imaging (MRI) are now available for evaluation of liver iron. SQUID is available in only few centers in the world, while MRI is now accessible in many hospitals. Anderson et al67 have developed a reproducible MRI method for quantifying myocardial iron concentration using a relaxation parameter defined as T2*, which reflects local magnetic field inhomogeneities that are increased with iron deposition.
MRI T2* has been used to quantify both liver and myocardial iron loading in patients with myelodysplastic syndromes.68–70 Di Tucci et al69 studied 27 transfusion-dependent patients, most of whom did not receive iron chelation therapy. All patients who had received at least 24 RBC units showed MRI T2* detectable hepatic iron [liver T2* value ≤ 6.3 milliseconds (ms)]. Cardiac MRI T2* values ranged from 5.6 to 58.7 ms, and a pathological cardiac T2* value (< 20 ms) was found in 3 patients. Cardiac T2* correlated with transfusion burden, and only patients with severe hepatic iron overload (T2* < 1.4 ms) showed pathological cardiac T2* values. Serum ferritin was not significantly correlated with cardiac T2*. Two studies involving already chelated patients failed to demonstrate myocardial iron deposition.68,70
The available evidence indicates that MRI T2* provides a noninvasive reproducible method for detecting both liver and myocardial iron overload in patients with myelodysplastic syndrome and that it might be useful for guiding iron chelation therapy.
Plasma non–transferrin-bound iron (NTBI) has been detected in patients with thalassemia major71 and in individuals with low-risk myelodysplastic syndrome,72 but its clinical utility is unclear.
A few assays are now available for the determination of serum hepcidin.73,74 Although they represent research tools at present, clinical applications are likely in the future. In fact, inappropriately low hepcidin levels in patients receiving blood transfusions might indicate a high risk of parenchymal iron loading.75
Iron Chelation Therapy in Patients with Myelodysplastic Syndrome
Therapeutic strategies that may successfully restore effective erythropoiesis in patients with myelodysplastic syndromes have been reviewed recently.76 In particular, treatment of anemia with erythropoietin plus granulocyte colony-stimulating factor (G-CSF) has a positive impact on survival while not affecting the risk of leukemic transformation.77,78 However, only a portion of patients have a durable response to this treatment. In the long term, the vast majority of patients with myelodysplastic syndrome become dependent on regular red cell transfusions.
Only uncontrolled studies, reviewed by Alessandrino et al,79 have been published on the efficacy of iron chelation therapy on transfusion iron overload in patients with myelodysplastic syndrome. One study showed that subcutaneous bolus injection of deferoxamine is an acceptable alternative to slow, pump-driven infusion.80 Based on the limited available evidence, the Expert Panel of the Italian Society of Hematology79 agreed that iron chelation should be considered as a therapy for myelodysplastic syndrome. It was concluded that patients who have previously received more than 50 red blood cell units and for whom a life span longer than 6 months is expected should be treated and that deferoxamine should be employed.
The Expert Panel of the British Society of Hematology81 acknowledged that their recommendations for iron chelation treatment in myelodysplastic syndromes were based on limited data. The British experts concluded that iron chelation should be considered once a patient has received 5 g iron (approximately 25 units of red cells) but only in patients for whom long-term transfusion therapy is likely, such as those with pure sideroblastic anemia or the 5q- syndrome. According the British guidelines, deferoxamine 20 to 40 mg/kg should be administered by 12-hour subcutaneous infusion 5 to 7 days per week.
A prospective Phase II trial evaluated the efficacy of deferasirox in regularly transfused patients with myelodysplastic syndromes or other anemias.82 In patients with baseline LIC = 7 mg Fe/g dry weight, deferasirox initiated at as dose of 20 or 30 mg/kg/d produced statistically significant decreases in LIC. Similar observations have been done in a recent smaller study.83
Deferasirox has been approved by the U.S. Food and Drug Administration (FDA) for “treatment of chronic iron overload caused by blood transfusions in patients 2 years of age and older.” The therapeutic indications approved by the European Medicines Agency (EMEA) are more detailed, and—with respect to myelodysplastic syndromes—the drug is “indicated for the treatment of chronic iron overload due to blood transfusions when deferoxamine therapy is contraindicated or inadequate.” Thus, deferasirox is now available for treatment of transfusion iron overload in patients with myelodysplastic syndrome, but data on its long-term safety and effectiveness are needed.
Table 3 summarizes the risks of parenchymal iron overload and its clinical consequences in patients with myelodysplastic syndrome receiving regular blood transfusions and stratified according to WPSS. Low-risk patients with refractory anemia, refractory anemia with ringed sideroblasts or 5q- syndromes who have a regular need for blood transfusion are more likely to develop clinical consequences of transfusion iron overload and are the best candidates for iron chelation therapy. Starting iron chelation once a patient has received 25 units of red cells appears to be a wise choice. Iron chelation should also be considered in iron-loaded patients who are candidates for allogeneic stem cell transplantation.
The choice between deferoxamine and deferasirox is controversial. Deferoxamine is definitely effective and safe, but requires subcutaneous administration and is therefore uncomfortable for patients. As an oral drug, deferasirox is clearly easier for patients, but its long-term effectiveness and safety have not been defined. Deferoxamine should be employed before allogeneic stem cell transplantation.
Whether or not prevention of severe parenchymal iron overload by chelation therapy will result in lower morbidity and mortality in regularly transfused patients with myelodysplastic syndrome remains to be established, and observational or registry studies are welcome.
Summary
Once anemia is symptomatic, red-cell transfusions are the mainstay of therapy patients with myelodysplastic syndrome. The redistribution of transfusion iron from reticuloendothelial cells to parenchymal cells is modulated by hepcidin. Ineffective erythropoiesis has a suppressive effect on hepcidin production, and therefore increases iron redistribution. Parenchymal iron overload may be located using magnetic resonance imaging T2*, which provides a non-invasive method for detecting and quantifying both liver and myocardial iron overload. Transfusion-dependent patients with isolated erythroid dysplasia and low risk of leukemic evolution are more likely to develop parenchymal iron overload and its toxicity, and therefore may benefit from chelation therapy. Deferoxamine and deferasirox are currently available for treatment of transfusion iron overload in patients with myelodysplastic syndrome.
Impact of ineffective erythropoiesis on intestinal iron absorption and reticuloendothelial iron recycling through its suppressive effect on hepcidin production.34–36
According to this model, increased absorption of dietary iron plays a major role in the pathophysiology of the so called iron loading anemias (X-linked sideroblastic anemia, congenital dyserythropoietic anemias, thalassemia intermedia),31 while increased reticuloendothelial iron recycling is likely the major mechanism of parenchymal iron loading in anemic patients receiving regular blood transfusions (e.g., refractory anemia with ringed sideroblasts).41,51
Impact of ineffective erythropoiesis on intestinal iron absorption and reticuloendothelial iron recycling through its suppressive effect on hepcidin production.34–36
According to this model, increased absorption of dietary iron plays a major role in the pathophysiology of the so called iron loading anemias (X-linked sideroblastic anemia, congenital dyserythropoietic anemias, thalassemia intermedia),31 while increased reticuloendothelial iron recycling is likely the major mechanism of parenchymal iron loading in anemic patients receiving regular blood transfusions (e.g., refractory anemia with ringed sideroblasts).41,51
Cumulative probability of survival among 374 patients given a diagnosis of myelodysplastic syndrome at the Fondazione IRCCS Policlinico San Matteo, Pavia, Italy, 1992–2002.
Patients were grouped according to whether or not a transfusion requirement developed during their clinical course. The two groups were compared by means of a Cox proportional-hazards regression model with time-dependent covariates. Each patient was considered as part of the transfusion-independent group as long as he or she had no need for blood transfusion and was recategorized in the transfusion-dependent group when a transfusion requirement developed. Once a regular need for blood transfusion developed, patients had a significantly lower probability of survival (hazard ratio for death, 1.58; P = 0.005). Reproduced with permission and minor changes from: Cazzola M, Malcovati L. Myelodysplastic syndromes—coping with ineffective hematopoiesis. N Engl J Med. 2005;352:536–538.
Cumulative probability of survival among 374 patients given a diagnosis of myelodysplastic syndrome at the Fondazione IRCCS Policlinico San Matteo, Pavia, Italy, 1992–2002.
Patients were grouped according to whether or not a transfusion requirement developed during their clinical course. The two groups were compared by means of a Cox proportional-hazards regression model with time-dependent covariates. Each patient was considered as part of the transfusion-independent group as long as he or she had no need for blood transfusion and was recategorized in the transfusion-dependent group when a transfusion requirement developed. Once a regular need for blood transfusion developed, patients had a significantly lower probability of survival (hazard ratio for death, 1.58; P = 0.005). Reproduced with permission and minor changes from: Cazzola M, Malcovati L. Myelodysplastic syndromes—coping with ineffective hematopoiesis. N Engl J Med. 2005;352:536–538.
Overall survival (plot A) and risk of leukemic evolution (plot B) in patients with myelodysplastic syndrome classified according WHO categories.
These survival curves were obtained by applying a Cox proportional hazard regression model with time-dependent covariates on 271 patients followed at the University of Pavia, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy, between 1992 and 2004. These patients were evaluable for repeated measures of the variables of interest during their follow-up. According to the model adopted, a patient is classified into a WHO subgroup at the time of diagnosis, and remains in the same group as long as the disease remains stable. As a WHO diagnostic parameter changes, the patient will move from the old to a new WHO category, and will subsequently be followed-up in the latter one. Abbreviations: RA, refractory anemia; RARS, refractory anemia with ringed sideroblasts; MDSdel(5q), myelodysplastic syndrome with deletion 5q; RCMD, refractory cytopenia with multilineage dysplasia; RCMD-RS, refractory cytopenia with multilineage dysplasia and ringed sideroblasts; RAEB-1, refractory anemia with excess blasts, type 1; RAEB-2, refractory anemia with excess blasts, type 2.
Overall survival (plot A) and risk of leukemic evolution (plot B) in patients with myelodysplastic syndrome classified according WHO categories.
These survival curves were obtained by applying a Cox proportional hazard regression model with time-dependent covariates on 271 patients followed at the University of Pavia, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy, between 1992 and 2004. These patients were evaluable for repeated measures of the variables of interest during their follow-up. According to the model adopted, a patient is classified into a WHO subgroup at the time of diagnosis, and remains in the same group as long as the disease remains stable. As a WHO diagnostic parameter changes, the patient will move from the old to a new WHO category, and will subsequently be followed-up in the latter one. Abbreviations: RA, refractory anemia; RARS, refractory anemia with ringed sideroblasts; MDSdel(5q), myelodysplastic syndrome with deletion 5q; RCMD, refractory cytopenia with multilineage dysplasia; RCMD-RS, refractory cytopenia with multilineage dysplasia and ringed sideroblasts; RAEB-1, refractory anemia with excess blasts, type 1; RAEB-2, refractory anemia with excess blasts, type 2.
Disclosures Conflict-of-interest disclosure: The authors declare no competing financial interests. Off-label drug use: None disclosed.
References
Author notes
Department of Hematology Oncology, University of Pavia & Fondazione IRCCS Policlinico San Matteo, Pavia, Italy