Abstract
Despite an increased understanding of the pathophysiology of sickle cell disease (SCD), there remains a paucity of available agents for the prevention and treatment of specific SCD-related complications. Recently, there has been significant progress in the development of novel drugs for this disease. These agents, which increase the production of fetal hemoglobin, improve red blood cell hydration, increase the availability of nitric oxide and possess anti-inflammatory effects, are in varying stages of clinical development. With the complex pathophysiology of SCD, it is unlikely that a single agent will prevent or treat all the sequelae of this disease. As a result, patients may benefit from treatment with a combination of agents that possess different mechanisms of action. This overview discusses selected novel agents that appear promising in SCD.
A single point mutation in the beta;-globin gene results in the well known hemolytic and vaso-occlusive complications that characterize sickle cell disease (SCD). Although the polymerization of deoxygenated sickle hemoglobin (HbS) is the primary event in the molecular pathogenesis of this disease,1 the pathophysiology of SCD is quite complex. Adherence of red blood cells (RBC) and other cellular elements to vascular endothelium,2 pro-inflammatory events3 and quite possibly activation of the coagulation system4 contribute to the pathophysiology. More recently, the role of ongoing hemolysis, with the resultant scavenging of nitric oxide (NO) and the development of vascular instability as well as a chronic vasculopathy, has been implicated in the pathogenesis of several SCD-related complications.5
Medical advances in the management of SCD patients have led to significant increases in life expectancy. This improved longevity is likely a result of neonatal screening, patient and parental education, improved public health, advances in red blood cell transfusion medicine, penicillin prophylaxis for children, pneumococcal vaccinations, and hydroxyurea therapy. To date, allogeneic bone marrow transplantation remains the only available cure, although this form of therapy is limited by the availability of potential donors and by its toxicity. Despite our increased understanding of the pathophysiology of SCD, there has been a tremendous lag in its application to the development of safe and effective therapies. There has recently been an increase in the development of drugs based on the pathophysiology of SCD. With the recognition that the complications of SCD may fall into two partially overlapping sub-phenotypes, the hemolytic and viscosity-vaso-occlusive phenotypes, the concept of targeted therapies may become more realistic. This review discusses selected agents that appear promising in the treatment of SCD. These agents were identified based on a MEDLINE search and a review of published abstracts. Detailed reviews on other potential therapies in SCD have recently been published.6–8
Induction of Fetal Hemoglobin
Fetal hemoglobin (HbF) is a potent inhibitor of the polymerization of deoxyhemoglobin S.1 This is because neither HbF (α2γ2) nor the hybrid tetramer, α2γbeta;s, are incorporated into the polymer phase. Multiple epidemiological studies show that the level of HbF predicts clinical severity in patients with SCD. Furthermore, the Cooperative Study of Sickle Cell Disease (CSSCD), a natural history study of SCD in the United States, reported an inverse correlation between HbF concentration and the frequency of painful crises,9 acute chest syndrome10 and mortality.11 The goal of HbF-inducing treatments is to achieve levels of HbF in each sickle RBC that are sufficient to inhibit or retard HbS polymerization. HbF-inducing agents include hydroxyurea, DNA demethylating agents, short chain fatty acids and histone deacetylase inhibitors (Table 1 ). Hydroxyurea, a ribonucleotide reductase inhibitor, is the only drug approved by the US Food and Drug Administration specifically for treating SCD. While it’s exact mechanism of action remains uncertain, hydroxyurea has been shown to reduce the frequency of hospitalizations, acute painful episodes, acute chest syndrome, and blood transfusions in severe sickle cell anemia. For more details of the effects of hydroxyurea in SCD, please see the accompanying article by RE Ware and B Aygun, beginning on page 62.
Human γ-globin genes are methylated in adult erythroid cells and hypomethylated in fetal tissue. Hypomethylation of the γ-globin gene promoter triggers its expression and induces γ-globin synthesis.12 Hypomethylating agents also induce selective degradation of DNA methyltransferase (DNMT) 1, resulting in re-expression of γ-globin genes.13 When administered at low doses, the nucleoside analog, decitabine (5-aza-2′-deoxycytidine) hypomethylates cellular DNA without cytotoxicity.14 Upon incorporation into DNA, it forms covalent bonds with DNMT, resulting in depletion of the enzyme and subsequently in DNA hypomethylation.15 Decitabine has been shown to produce an increase in HbF levels in patients who did not respond to hydroxyurea.14,16 Low-dose subcutaneous injections of decitabine (0.2 mg/kg 1– 3 times per week) were administered to adult patients with SCD and produced marked increases in HbF, F-cell proportion and hemoglobin levels, with decreased reticulocyte and absolute neutrophil counts.14 A recently published case series of adult SCD patients with multiple complications who did not respond adequately to hydroxyurea treatment reported reduced vaso-occlusive events and increased hemoglobin levels following treatment with decitabine.16 Treatment of SCD patients with decitabine also produces a thrombocytosis,14,16 possibly due to a shift in patterns of cellular differentiation.
The short chain fatty acid, butyrate, inhibits histone deacetylase (HDAC) and promotes elevated levels of core histone acetylation, affecting chromatin structure and transcription rates of γ-globin gene.17 It appears to modulate globin gene expression by binding to transcriptionally active elements in the 5′ flanking region of the γ-globin gene, and has an effect on the translational efficiency of γ-globin mRNA.18 In vitro studies, as well as studies in animal models, show that butyrate induces γ-globin production.19 Studies in SCD and beta;-thalassemia patients treated with butyrate showed increased HbF production, although this initial response was followed by a decline in HbF levels,20 an effect attributed to its cumulative erythroid anti-proliferative activity. Treatments with “pulse” doses of butyrate (250–500 mg/kg/day for a maximum of 6 days per month), however, resulted in sustained HbF production and higher hemoglobin levels.20,21 The magnitude of HbF response following butyrate therapy appears to be related to the baseline level of HbF.20 Other short chain fatty acids, such as 2,2 dimethylbutyric acid, also induce HbF expression and stimulate cell growth, but do not inhibit HDAC.22 A clinical study of sodium 2,2 dimethylbutyrate in SCD is currently underway (http://www.clinicaltrials.gov#NCT00842088).
The HDAC inhibitor, trichostatin A, has been tested in transgenic sickle mice.23 This drug, which is known to increase HbF, significantly inhibits pulmonary vein expression of vascular cell adhesion molecule (VCAM) and tissue factor (TF) in the severe transgenic sickle mouse, hBERK1, and in the mild sickle transgenic mouse, NYDD1, following hypoxia-reoxygenation.23 It also significantly inhibits vascular stasis, suggesting that it may possess multi-modality benefit. Further studies of HDAC inhibitors in SCD patients are warranted.
Pomalidomide is an immunomodulatory thalidomide derivative. It has been reported to stimulate erythropoiesis, F-cell production, total hemoglobin and HbF synthesis in human CD34+ cells.24 There appeared to be a synergistic upregulation of HbF expression when pomalidomide was combined with hydroxyurea. The treatment of transgenic sickle mice with pomalidomide augmented HbF expression comparable to that obtained with hydroxyurea, although HbF levels returned to control values when pomalidomide and hydroxyurea were combined.25 Following treatment with pomalidomide, the WBC count was unaffected and liver histology showed decreased tissue inflammation and focal necrosis in approximately 50% of treated animals.
Prevention of Red Blood Cell Dehydration
Polymerization of HbS is linked in an exponential manner to the intracellular hemoglobin concentration.26 As a result of this concentration dependence of HbS polymerization, the hydration status of sickle RBC is critical to the rate and degree of polymer formation. The dehydration of sickle RBC, which follows the loss of solutes and osmotically obliged water, is thought to result from increased ion flux via the potassium selective pathways, the calcium-activated potassium (K+) efflux (or Gardos) pathway and the K-Cl co-transport pathway,27 and the Na-K ATPase channel. A treatment approach that prevents ion and water loss from sickle RBC by inhibiting any of these pathways may ameliorate the clinical expression of SCD.
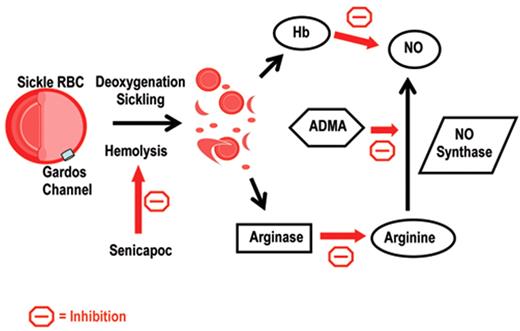
Senicapoc [bis(4-fluorophenyl)phenyl acetamide], previously known as ICA-17043, is a potent and selective blocker of the Gardos channel.28 Increasing concentrations of senicapoc produce a consistent and increasing block of rubidium (86Rb+) flux through the Gardos channel in washed RBC loaded with rubidium, with an IC50 (drug concentration that inhibits 50% of K+ efflux from RBC) of 11 ± 2 nM compared to an IC50 of 100 ± 12 nM for clotrimazole.28 Senicapoc produced a significant and sustained decrease in Gardos channel activity, increase in RBC K+ content, increase in hematocrit, and decrease in both MCHC and RBC densities when administered to transgenic sickle mice.28 A 12-week, multicenter, phase II study of senicapoc showed a dose-dependent increase in hemoglobin levels, with associated decreases in the number and percentage of dense RBC and reticulocytes, as well as levels of chemical markers of hemolysis.29 A subsequent phase III study was terminated early because of a failure of senicapoc to demonstrate a reduction in the rate of acute pain episodes. Despite this result, it remains possible that senicapoc may be beneficial in the prevention or treatment of hemolysis-associated complications in SCD (Figure 1 ).
Increased intracellular magnesium reduces the efflux of potassium from sickle RBC by inhibiting the K-Cl co-transporter. Studies in transgenic sickle mice show that magnesium supplementation can reduce K-Cl co-transport activity, with subsequent decreases in the MCHC, RBC density, and reticulocyte count.30 Treatment of adult SCD patients with magnesium supplements appears to be well tolerated, with diarrhea being the most common side effect.31 A phase I study of magnesium pidolate combined with hydroxyurea in HbSS children reported a significant reduction of K-Cl co-transport activity following introduction of oral magnesium pidolate, with the most common side effects being diarrhea and abdominal pain.32 A phase II study evaluating the role of magnesium pidolate in children and adults with HbSC disease is ongoing (http://www.clinicaltrials.gov#NCT00040456).
Nitric Oxide
There is increasing evidence that hemolysis may contribute to the pathogenesis of several complications in SCD.5 Intravascular hemolysis results in high rates of NO destruction and a state of resistance to NO activity. NO is a potent endogenous vasodilator. Cell-free plasma hemoglobin reacts with NO at a rate 1000-fold faster than intra-erythrocytic hemoglobin.33 As a result, soluble guanylate cyclase, which converts GTP to cyclic GMP, is not activated and vasodilation is inhibited. Arginase-1, an enzyme that converts the substrate for NO synthesis, arginine, to ornithine,34 is also released following hemolysis. Furthermore, the level of asymmetric dimethylarginine (ADMA) correlates with measures of hemolysis35 and may further contribute to limiting NO bioavailability in patients with SCD by competitively inhibiting NO synthase.
The beneficial use of inhaled NO was reported in cases of SCD patients with acute chest syndrome whose clinical courses were complicated by respiratory failure, hypoxia and pulmonary hypertension that failed to respond to standard treatments.36,37 More recently, 20 patients were treated in a prospective, double-blind, placebo-controlled randomized clinical trial with inhaled NO (80 ppm with 21% inspired oxygen) or placebo (21% inspired oxygen). Although there was no significant difference in pain scores assessed by visual analog scale, the use of morphine was significantly less in the inhaled NO group over 6 hours (0.29 mg/kg vs 0.44 mg/kg; P = .03). Other studies of inhaled NO are ongoing in pain crisis (http://www.clinicaltrials.gov#NCT00094887 and NCT00142051) and in acute chest syndrome (http://www.clinicaltrials.gov#NCT00748423).
L-arginine is converted by NO synthase (NOS) to citrulline and NO. L-arginine is low in HbSS adults in the steady state and appears to decrease to even lower levels during acute pain episodes.38,39 NO synthase is uncoupled under conditions of low arginine concentration, producing reactive oxygen species in lieu of NO,40 which may further reduce NO bioavailability in SCD and enhance oxidative stress. Arginase, an enzyme that converts L-arginine to ornithine and urea, is increased in SCD34 and can limit NO bioavailability through increased consumption of the substrate for NO synthase. Arginine also reduces the RBC density in transgenic sickle mice by inhibiting Gardos channel activity.41 Treatment of 10 patients with pulmonary hypertension with arginine for 5 days produced a 15% reduction in the mean estimated pulmonary artery systolic pressure (63.9 ± 13 to 54.2 ± 12 mm Hg, P = .002).34 However, preliminary results from a multicenter phase II study of arginine in children failed to show any change in arginine levels or other laboratory endpoints after 3 months of treatment.42 Despite decreased enthusiasm, a study to evaluate the efficacy of arginine in acute chest syndrome is ongoing (http://www.clinicaltrials.gov#NCT00029731).
Sildenafil, an oral phosphodiesterase-5 (PDE5) inhibitor, can amplify the effect of endogenous NO by inhibiting the breakdown of cyclic GMP. Possibly due to the effect of cyclic GMP, treatment with sildenafil reduces platelet activation43 and may increase HbF levels.44 An open label study of sildenafil in 12 patients with pulmonary hypertension treated for a mean duration of 6 ± 1 months reported a decrease in the estimated PASP (50 ± 4 mm Hg to 41 ± 3 mm Hg, 95% CI: 0.3 – 17, P = .04) and improved cardiopulmonary functioning, with increases in 6-minute walk distances (383 ± 30 m to 462 ± 28 m, 95% CI: 40 – 117, P =.001).45 Sildenafil is currently being tested in a multicenter study to evaluate its efficacy in SCD-associated pulmonary hypertension (http://www.clinicaltrials.gov#NCT00492531). Despite concerns of an increased risk of priapism, current evidence suggests that chronic PDE5 inhibitor administration in the context of priapism could effectively recondition PDE5 regulatory function in the penis.46 Priapism may result from disturbances involving the reduced expression of PDE5 in the penis.47 Indeed, several case series suggest that PDE5 inhibitor therapy with sildenafil and tadalafil are successful in alleviating or resolving priapism in SCD.46,48 Further studies are required to assess the safety and efficacy of PDE5 inhibitors in SCD-associated priapism. Rolipram, a PDE4 inhibitor, has also been shown to prevent the hypoxia-induced development of pulmonary arterial hypertension in transgenic sickle mice, possibly by the modulation of both vascular tone and inflammatory factors.49
Tetrahydrobiopterin (BH4) is an essential cofactor during the formation of NO. In the absence of sufficient levels of BH4, endothelial NOS catalyzes a partial reaction in which oxygen is transformed into superoxide and NO is not generated. BH4 deficiency has been implicated as a cause of endothelial dysfunction in SCD patients.50 Preliminary results from a phase IIa, open label study in SCD showed that 6R-BH4 was well tolerated and resulted in significant dose-dependent improvement in endothelial function, assessed using a non-invasive, operator-independent technique of peripheral arterial tonometry.51
Anti-inflammatory Agents
Statins are a class of drugs that have pleitropic effects. They exert potent antiproliferative and proapoptotic effects on vascular smooth-muscle cells52; stabilize endothelial barrier function in response to injury53; have anti-inflammatory effects54; and enhance endothelial production of NO.55 In a study involving transgenic SCD mice, pretreatment with lovastatin eliminated excessive expression of endothelial TF in the lung of the mild sickle mouse following hypoxia-reoxygenation and in the more severe mouse at ambient air.56 A study evaluating the safety of simvastatin and its effect on vasoreactivity, endothelial adhesion and inflammation in SCD patients is ongoing (http://www.clinicaltrials.gov#NCT00508027).
Steroids have been reported to reduce the duration of severe pain episodes, as well as the severity of acute chest syndrome in children and adolescents, although there appears to be a substantial risk for readmission due to pain.57–59 Treatment with corticosteroids may also be associated with an increased risk of hemorrhagic stroke in children with SCD.60 More studies are required to define the benefits and risks of steroids in SCD. Unfortunately, a phase III study of dexamethasone in acute chest syndrome was recently terminated due to slow subject accrual.
The nuclear factor-kappa B inhibitor sulfasalazine significantly reduced the expression of VCAM, intercellular adhesion molecule (ICAM), and E-selectin, but not the expression of TF in circulating endothelial cells (CEC) in 3 patients with SCD.61 In companion studies performed in transgenic sickle mice, sulfasalazine significantly reduced CEC expression of VCAM, ICAM, and E-selectin, and it correspondingly reduced expression of these molecules in some blood vessels. In addition, sulfasalazine attenuates the effects of reperfusion injury by decreasing leukocyte adhesion and improving microvascular blood flow in transgenic sickle mice.62
Anticoagulants and Antiplatelet Agents
Multiple studies of anticoagulants and antiplatelet agents have been conducted in SCD patients with varying results.4 Unfractionated heparin decreases sickle cell adhesion to endothelium under static conditions, as well as P-selectin–mediated flow adherence of sickle cells to thrombin-treated human vascular endothelial cells.63 In a randomized, double-blind, placebo-controlled study of SCD patients during acute pain episodes, treatment with the low molecular weight heparin, tinzaparin, resulted in a significant reduction in the overall duration of painful crisis, number of days with the most severe pain scores, and duration of hospitalization compared with placebo.64 The glycoprotein IIb/IIIa inhibitor, eptifibatide, was reported to be safe in a pilot study of HbSS patients, with decreases in platelet aggregation and levels of the inflammatory mediator, soluble CD40 ligand.65 A phase I/II study of eptifibatide in acute pain episodes is presently ongoing (http://www.clinicaltrials.gov#NCT00834899).
Other Novel Agents
Nix-0699 (Niprisan®, Nicosan®, Hemoxin®) is a phytomedicine that contains extracts from four different plants. Although the active ingredient is unknown and its mechanism of action remains unclear, in vitro studies show that it inhibits RBC sickling and produces a left shift of the oxygen-dissociation curve of HbS.66,67 A placebo-controlled, double blind, cross-over trial in 82 patients with SCD showed that Nix-0699 appears to be safe. In addition, it significantly reduced the frequency of crisis associated with severe pain.68 Although available for treatment of patients with SCD in Nigeria, more studies of Nix-0699 are required to elucidate its mechanism of action, as well as its safety and efficacy.
Intravenous immunoglobulin (IVIG) has been reported to decrease the number of leukocytes adherent to endothelium, decrease the number of red cells interacting with white blood cells, and improve microcirculatory blood flow when administered to transgenic sickle mice that were pretreated to mimic a painful crisis.69 Treatment with IVIG also resulted in an improved survival compared with treatments using phosphate-buffered saline or albumin. A study to evaluate the safety and efficacy of IVIG in patients with SCD, admitted for uncomplicated acute pain episodes, is ongoing (http://www.clinicaltrials.gov#NCT00644865).
The endothelin receptor antagonist, bosentan, has been shown to prevent renal and pulmonary microvascular congestion, systemic inflammation, dense RBC formation, and infiltration of activated neutrophils into tissues in transgenic sickle mice following hypoxia-reoxygenation. Furthermore, bosentan prevented the death of transgenic sickle mice following exposure to a severe hypoxic challenge.70
Conclusion
Despite our increased understanding of the pathophysiology of SCD, treatments for this disease remain quite limited. The availability of several novel agents in various stages of development is encouraging. These agents may be used alone or in combination with hydroxyurea for the treatment of specific complications. However, with the complex pathophysiology of SCD, it is unlikely that a single drug will prevent or reverse all of its sequelae. Patients may benefit from treatment with agents that possess multimodality effect or a combination of agents that may exert additive or synergistic effects, akin to treatment paradigms in cancer.
Hemolysis contributes to the pathophysiology of sickle cell disease by reducing nitric oxide bioavailability. Modified from Ataga KI, Stocker J. Senicapoc (ICA-17043): a potential therapy for the prevention and treatment of hemolysis-associated complications in sickle cell anemia. Expert Opin Investig. Drugs 2009;18:231–239. ADMA indicates asymmetric dimethylarginine; Hb, hemoglobin; HbS, sickle hemoglobin; RBC, red blood cell.
Hemolysis contributes to the pathophysiology of sickle cell disease by reducing nitric oxide bioavailability. Modified from Ataga KI, Stocker J. Senicapoc (ICA-17043): a potential therapy for the prevention and treatment of hemolysis-associated complications in sickle cell anemia. Expert Opin Investig. Drugs 2009;18:231–239. ADMA indicates asymmetric dimethylarginine; Hb, hemoglobin; HbS, sickle hemoglobin; RBC, red blood cell.
Disclosures Conflict-of-interest disclosure: The author has received funding from Biomarin Pharmaceuticals, Icagen, and TRF Pharma. Off-label drug use: None disclosed.
Acknowledgments
This work was supported in part by NIH grants UL1RR025747, HL091265 and HL079915. Support for this work was also provided by an award from the North Carolina State Sickle Cell Program.
References
Author notes
Comprehensive Sickle Cell Program, Division of Hematology/Oncology, University of North Carolina, Chapel Hill, NC