Abstract
Clinical experience with hydroxyurea for patients with sickle cell disease (SCD) has been accumulating for the past 25 years. The bulk of the current evidence suggests that hydroxyurea is well-tolerated, safe, and efficacious for most patients with SCD. Hydroxyurea has proven clinical efficacy for reducing acute vaso-occlusive events including pain episodes and acute chest syndrome. Salutary effects on hematological parameters include increases in fetal hemoglobin (HbF), hemoglobin, and MCV; also significant decreases occur in WBC, ANC, reticulocytes, LDH, and bilirubin. Treatment with hydroxyurea is usually considered for patients with recurrent vaso-occlusive events, but additional indications for treatment may include laboratory markers of disease severity and evidence of chronic organ dysfunction. Ten years ago, the US Food and Drug Administration approved hydroxyurea for adult patients with clinically severe SCD; however, its use in children remains off-label. Despite the large body of evidence regarding its efficacy and safety, hydroxyurea is currently prescribed only sparingly for patients with SCD and therefore has only limited effectiveness for this disorder; barriers to its use need to be identified and overcome.
Sickle cell disease (SCD) was first described almost exactly a century ago, and the molecular basis for the disorder was elucidated a half-century ago, yet therapeutic options have been very slow to develop. The pathophysiology of SCD is complex and involves erythrocyte sickling, acute vaso-occlusive events, hemolysis, endothelial vasculopathy, and chronic organ damage. Due in part to this multifaceted pathophysiology, effective treatment against the primary disease process has only recently been realized. Hydroxyurea is currently the only US Food and Drug Administration (FDA)–approved treatment for severely affected adults with sickle cell anemia in the United States (approved in 1998); equivalent approval by the European Medicines Agency (EMeA) for both adults and children with SCD in the European Union occurred in 2007.
Hydroxyurea is a simple chemical compound that has excellent oral bioavailability. Taken once a day, hydroxyurea has proven laboratory and clinical efficacy for persons with SCD, primarily by increasing levels of fetal hemoglobin (HbF). The %HbF has been shown to be a powerful predictor of clinical severity in SCD,1,2 and a potential threshold of 20% HbF has been suggested to prevent recurrent vaso-occlusive events.3 Pharmacological induction of HbF helps prevent intracellular sickling, which decreases vaso-occlusion and reduces hemolysis. Due to its ease of oral administration, wide therapeutic index, and relatively mild toxicity profile, hydroxyurea has many features of an ideal drug for SCD.4
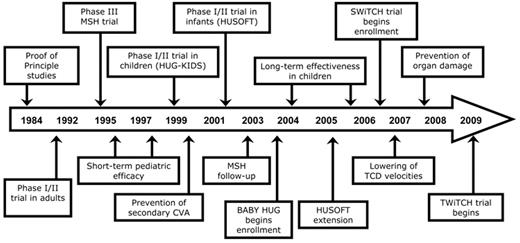
As illustrated in Figure 1 , the timeline of hydroxyurea use in SCD began 25 years ago with initial “proof of principle” studies, but then progressed to observational studies and a formal prospective phase I/II trial in adults,5 followed by a pivotal definitive phase III randomized clinical trial known as the Multicenter Study of Hydroxyurea (MSH).6 Pediatric studies have primarily been observational, beginning with small series in the mid-1990s, followed by a formal prospective phase I/II trial in children7 and then in infants.8 In the current decade, long-term studies have suggested the benefit of hydroxyurea in preventing many complications in children9–11 and even reducing mortality in adults.12,13 Current investigations are focusing on the ability of hydroxyurea to preserve organ function, primarily among young patients.
Although abundant evidence has accumulated for the use of hydroxyurea in patients with SCD of all ages, some questions about its long-term safety and toxicity profile remain unanswered. In addition, translation of efficacy (benefits identified in a controlled clinical trial) into effectiveness (benefits that occur in real-life clinical care situations) has been problematic due to a variety of barriers. In this review, the published evidence for hydroxyurea will be summarized, followed by a discussion of clinical indications for its use. Current NIH-funded clinical trials will then be described, as well as future research needs.
Hydroxyurea for SCD: What Is the Evidence?
An initial small clinical study involving adult patients with SCD was reported 25 years ago.14 Since that time, there have been many publications that address the efficacy and safety of hydroxyurea for patients with SCD. Sifting through these publications for relevant and definitive studies with high-quality evidence is an arduous task, but recently two groups were commissioned to assess and grade the published literature. Two evidence-based documents and subsequent publications provide thorough analyses of the efficacy and safety of hydroxyurea, and serve as up-to-date summaries for discussion.
The first group of evidence-based reports derives from the National Institutes of Health Office of Medical Applications of Research (OMAR), which commissioned a systematic review of the available published evidence on the use of hydroxyurea in patients with SCD. This topic was selected by the Agency for Healthcare Research and Quality (AHRQ) for systematic review by an evidence-based practice center. Specific topics for summary included the efficacy, effectiveness, toxicities (short- and long-term harms), and barriers to its use in this patient population. The detailed evidence report15 describes fully the methodology used for the data sources search, as well as the process of study selection, data extraction, quality assessment, data synthesis, and grading of evidence. The results of these analyses were summarized in three articles published in 2008: efficacy and toxicity of hydroxyurea in adults with SCD,16 efficacy and toxicity of hydroxyurea in children with SCD,17 and barriers to the use of hydroxyurea in patients with SCD.18
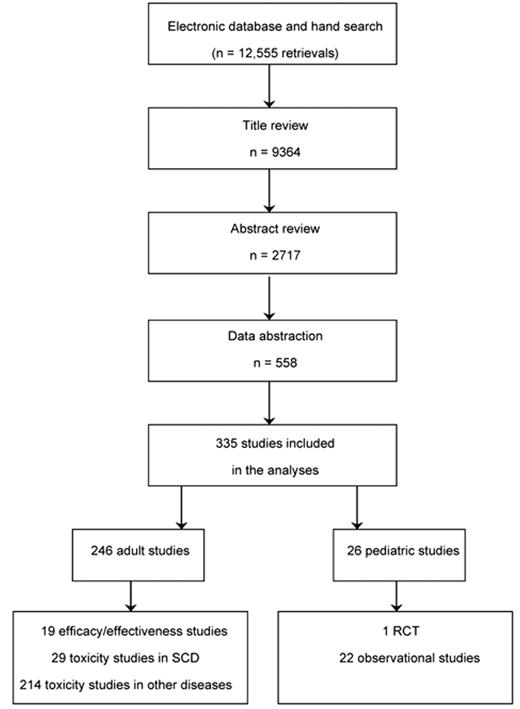
This AHRQ systematic review is notable for its thorough and rigorous review (Figure 2 ). Over 12,500 articles were identified from four large database searches, from which over 9000 titles were reviewed and over 2700 abstracts were reviewed. Most of these were later excluded for not being relevant to the key questions, lacking sufficient data to address the key questions, lacking original data, or reporting very small numbers of patients. A total of 558 studies underwent data abstraction. In the adult publication, a total of 335 studies were included in the full evidence report,15 but only 19 studies described efficacy or effectiveness of hydroxyurea in adults with SCD, while 29 addressed the issue of toxicity in SCD.16 In the pediatric report, only 26 studies were included in the final analyses.17
Efficacy of Hydroxyurea
Hematological effects of hydroxyurea treatment include increases in %HbF, hemoglobin concentration, and mean corpuscular volume (MCV), as well as significant decreases in white blood cell (WBC) count, absolute neutrophil count (ANC), absolute reticulocyte count, and lactate dehydrogenase (LDH). These changes, coupled with morphological changes that improve erythrocyte deformability and rheology, represent potentially beneficial effects for patients with SCD.
The AHRQ review identified only a single randomized clinical trial (MSH) that tested the efficacy of hydroxyurea,6 although six additional articles associated with this trial were later published. Together, these MSH data proved clinical efficacy for hydroxyurea, with statistically significant reductions in pain episodes (44% lower), longer time to first pain episode, fewer episodes of acute chest syndrome, and fewer patients who required transfusions or hospitalization. In long-term follow-up, mortality rates were 40% lower while patients were receiving hydroxyurea compared with no hydroxyurea (2.6 deaths per 3-month period, compared with 1.5 deaths per 3-month period).12 Among twelve observational efficacy studies involving adults with SCD, only one was high quality since most did not describe adherence or account for patients who were lost to follow-up. The %HbF was significantly increased during treatment, which was associated with a decrease in the number of pain episodes. Evidence for the efficacy of hydroxyurea among adults with SCD is summarized in Table 1 .
Similarly, the AHRQ review identified only a single randomized clinical trial19 that tested the efficacy of hydroxyurea in the pediatric age group: 22 children with HbSS received hydroxyurea or placebo in a cross-over design that was scored as having only moderate quality. Their median age at enrollment was 8 years and each treatment was 6 months in duration, starting hydroxyurea at 20 mg/kg/day with a maximum dose of 25 mg/kg/day. Hemoglobin concentration increased only slightly but %HbF significantly increased (+10.7%, P < .001); hospitalizations and number of hospital days were significantly decreased during hydroxyurea treatment.19 An additional 22 observational studies in the pediatric age group were identified, involving 4 different clusters of young patients with SCD who received hydroxyurea therapy: as described in the AHRQ review,15 8 of these were viewed as primarily efficacy studies, 9 were primarily effectiveness studies, and 5 were primarily toxicity studies. Most of these studies included hydroxyurea titration to maximum tolerated dose (MTD) or clinical response, but occasionally provided hydroxyurea at a fixed and relatively low dose (15 or 20 mg/kg/day) without any titration.
The efficacy and effectiveness of hydroxyurea in these observational studies on children with SCD are summarized in Table 2 . Together, these studies provide high-grade evidence for significant increases in %HbF, from starting values of 5% to 10% to treatment values averaging 15% to 20%. Hemoglobin concentration also increased significantly, usually +1 g/dL. Although the number of supporting studies was lower, moderate- to high-grade evidence was also found for reduction in pain episodes and hospitalizations. Insufficient or low evidence was found for decreased transfusions, reduced neurological events (stroke or abnormal Transcranial Doppler flow velocities), and improved splenic function (Table 2 ).
A common question about hydroxyurea treatment for sickle cell disease relates to the need for dose escalation to MTD. If hematological parameters and clinical well-being improve at lower doses of hydroxyurea (eg, 15–20 mg/kg/day), why risk toxicity and push the dose higher? As illustrated in Table 3 , several studies provide hematological results with hydroxyurea escalated to MTD, compared to others using a lower “clinically therapeutic” dose. Although there is some variability and most of the studies include only children, hydroxyurea escalated to MTD typically has yielded a higher HbF value that is around the theoretical threshold of 20%. Not every patient with SCD responds equally to hydroxyurea, however, and reduced responses have been observed in patients with lower baseline neutrophil and reticulocyte counts, lower medication adherence, and decreased bone marrow reserve.5,20,21 For patients with renal impairment, responses to hydroxyurea can be improved using supplemental erythropoietin.22 Genetic factors also may play an important role in the individual response rate to hydroxyurea.23
Recently, several published articles have provided an accumulated low-grade evidence for the ability of hydroxyurea to protect against or even reverse chronic organ damage in SCD. Tested primarily in the pediatric population, hydroxyurea may have efficacy for reducing proteinuria24,25 or glomerular hyperfiltration26; normalizing low pulse oximetry readings27; reversing splenic dysfunction8,28,29; lowering pulmonary hypertension30 and TCD velocities31; and preventing primary stroke32 or secondary stroke.33,34 Based on these limited observational studies and encouraging results, further prospective investigations are warranted with larger numbers of patients, ideally in NIH-sponsored multicenter randomized clinical trials.
Toxicities of Hydroxyurea
Toxicities associated with the use of hydroxyurea by adults and children with SCD were also evaluated in the AHRQ report (Table 1 ). Data from two prospective US adult studies5,6 and pediatric studies7,8 indicate that myelosuppression is a predictable side effect of hydroxyurea therapy, particularly of the granulocyte series. In addition to mild neutropenia, occasional worsening anemia or thrombocytopenia was also identified among children and adolescents on hydroxyurea therapy7; however, the myelosuppression was temporary and reversible with a short discontinuation of treatment. Skin and nail changes have been reported in association with hydroxyurea therapy, particularly hyperpigmentation including melanonychia,35 but these changes were not more common in the hydroxyurea arm of the MSH trial than in the placebo group.6 High-grade evidence supports that hydroxyurea is not associated with the development of leg ulcers in patients with SCD (Table 1 ). Perhaps the most critical potential toxicity is the issue of malignancy associated with hydroxyurea use in SCD. It is important to note that malignancy can occur naturally in patients with SCD, as documented in a retrospective report with patients predominantly in the pre-hydroxyurea era.36 Based on a thorough review of the literature for patients with SCD as well as other medical disorders, the AHRQ review concluded that “…limited evidence suggests that hydroxyurea treatment in adults with sickle cell disease does not increase the risk for leukemia.”15
Toxicities associated with the use of hydroxyurea also were described in the second evidence-based report, which focused exclusively on this topic. The National Toxicology Program and National Institute of Environmental Health Sciences Center for the Evaluation of Risks to Human Reproduction (CERHR) issued a report, after a thorough literature search and expert panel discussion, on the effects of hydroxyurea on growth and development, reproduction, teratogenicity, and pregnancy.37,38 Among children with SCD receiving hydroxyurea treatment, there was no evidence for growth delay but insufficient data to evaluate any effects on puberty. No data were found on the effects of hydroxyurea on female reproductive processes in humans or animals, or following germ cell exposure. However, reproductive toxicity was found in male mice, with decreased testis weight and sperm count, which led to concerns about possible adverse effects of hydroxyurea on spermatogenesis among men. Currently there are limited data on human spermatogenesis, but possible deleterious effects among adult males with SCD have recently been reported39,40 and warrant further prospective investigation. The CERHR report also reviewed studies describing hydroxyurea use during pregnancy and concluded that hydroxyurea is not commonly associated with adverse perinatal outcomes. However, the expert panel expressed concerns about possible congenital anomalies or abnormal fetal growth.38 Further information from the MSH extension trial may be useful in this context; pregnancies and birth outcomes were monitored in this cohort for up to 10 years, with results expected in the near future.
Clinical Indications for Hydroxyurea
Hydroxyurea treatment is currently FDA approved only for severely affected adults with sickle cell anemia. Typical clinical indications for initiating hydroxyurea include recurrent painful events, acute chest syndrome, and frequent hospitalizations. Because the drug is not FDA approved for pediatric patients, all hydroxyurea use for children in the United States is off-label. However, since the pathophysiology of acute vaso-occlusion is similar for children and adults, the use of hydroxyurea in young patients is warranted for similar clinical indications.
When carefully considered, however, there are additional potential laboratory and clinical indications for hydroxyurea treatment for patients with SCD, beyond treatment of acute vaso-occlusive events (Table 4 ). Laboratory values that are predictive of clinical severity, including low HbF and low hemoglobin concentration, or elevated WBC and LDH, are usually improved on hydroxyurea therapy. Initiating treatment on the basis of these abnormal laboratory values can be considered. Furthermore, although the benefits of hydroxyurea for the prevention of organ damage (or preservation of organ function) are supported by only small series of patients and relatively low-grade evidence, hydroxyurea should be considered for children with early organ dysfunction such as proteinuria, hypoxemia, or elevated transcranial Doppler flow velocities (Table 4 ). The spectrum of clinical and laboratory indications for hydroxyurea use is changing rapidly, and at this time there is no consensus based on high-grade evidence, so individual patients should be considered on a case-by-case basis. Several National Heart Lung and Blood Institute (NHLBI)–sponsored prospective clinical trials currently underway should provide additional data on which to base these clinical decisions.
Barriers to Using Hydroxyurea
Given the large accumulated body of evidence for laboratory and clinical efficacy of hydroxyurea in adults and children with SCD, it is perhaps surprising that hydroxyurea treatment appears to be prescribed sparingly in actual medical practice. Most patients receive hydroxyurea only in specialty clinics at academic centers, and only a fraction of patients who might benefit from hydroxyurea actually receive treatment.41,42 To assess and address this issue, the NHLBI and OMAR convened a Consensus Development Conference to discuss several important topics including the barriers to hydroxyurea treatment and potential solutions. The expert panel concluded that barriers to hydroxyurea treatment arise at many levels, ranging from the level of the patient, to the parent or family caregiver, and to the healthcare provider.18 Examples of these types of barriers include lack of knowledge about hydroxyurea as a therapeutic option; need for frequent monitoring; lack of adherence to the treatment regimen; provider bias and negative attitudes toward this patient population; and fears or concerns about cancer, birth defects, infertility, and other long-term risks. These types of barriers are often due to lack of education and familiarity by the parties involved, especially the healthcare providers, and possibly exaggerated concerns about toxicity and side effects. However, system-level barriers also exist that reflect financial, geographical, and cultural challenges. Examples of these barriers include lack of access to physicians with expertise using hydroxyurea; relative geographic isolation; lack of coordination between academic centers and community-based clinicians; inadequate financial support for persons with SCD; and lack of visible and helpful lay advocacy groups. Finally, access to medical care and knowledgeable providers within a medical home was considered to be a formidable challenge for many patients with SCD; solutions to these problems are articulated in the expert panel report but would require major restructuring of current models of medical care and approach to SCD.18
NIH-funded Clinical Trials with Hydroxyurea
Several NHLBI-funded clinical trials involving hydroxyurea treatment for patients with SCD are summarized below. Additional details can be obtained by review of each study at the NIH website http://clinicaltrials.gov.
Hydroxyurea to Prevent Organ Damage in Children with Sickle Cell Anemia (BABY HUG, NCT00006400). BABY HUG is a double-blinded, placebo-controlled, multicenter randomized clinical trial that tests the hypothesis that hydroxyurea can prevent organ damage in infants with SCA. The primary endpoints are spleen and kidney function after 24 months of either hydroxyurea (20 mg/kg/day) or placebo. Study results are expected in 2010.
Stroke With Transfusions Changing to Hydroxyurea (SWiTCH, NCT00122980). SWiTCH is a multicenter randomized clinical trial for pediatric patients with previous stroke as well as transfusional iron overload. Alternative treatment (hydroxyurea and phlebotomy) will be compared with standard treatment (transfusions and chelation) for the prevention of recurrent stroke and the management of iron overload. SWiTCH enrollment is completed and study results are expected in late 2011.
Long Term Effects of Hydroxyurea Therapy in Children with Sickle Cell Disease (HUSTLE, NCT00305175). HUSTLE is a longitudinal observational single-institutional study from St. Jude Children’s Research Hospital that prospectively studies the pharmacokinetics, genotoxicity, and long-term effects of hydroxyurea on organ function. Both safety and efficacy endpoints are included in the trial design.
Evaluating the Safety and Effectiveness of Hydroxyurea and Magnesium Pidolate to Treat People with Hemoglobin SC Disease (CHAMPS, NCT00532883). CHAMPS is a multicenter trial investigating the combination of hydroxyurea with magnesium pidolate for children and adults with HbSC; CHAMPS was terminated recently due to inadequate enrollment, but some study results are expected in 2010.
TCD With Transfusions Changing to Hydroxyurea (TWiTCH) is a phase III multicenter randomized clinical trial for children with abnormal TCD velocities. TWiTCH will compare hydroxyurea to transfusions for maintaining TCD velocities and preventing primary stroke; enrollment is scheduled to begin in 2010.
The Future of Hydroxyurea in SCD
Until additional therapies become available, including those that target specific parts of the pathophysiology of intracellular sickling, acute vaso-occlusion, or hemolysis, the use of hydroxyurea should be considered for many more patients with SCD. Prospective studies are needed to determine the efficacy of hydroxyurea for preventing chronic organ damage in SCD. Unanswered questions remain about the efficacy of hydroxyurea in patients with variant genotypes, especially HbSC, and formal investigation in this population is warranted. Long-term risks have not been fully determined, particularly with regard to fertility and teratogenicity, although current evidence is reassuring in most cases. Inter-individual differences in response to hydroxyurea are well recognized but remain poorly understood; recent evidence suggests pharmacokinetic and possibly pharmacogenetic influences may be important.43 Outcomes research is needed to improve hydroxyurea utilization and adherence rates among patients who would benefit from treatment. Investigation of effectiveness is also needed to help bring a therapeutic option with proven efficacy into the mainstream of patient care and treatment.
Finally, the medical community should acknowledge and begin to address the barriers that prevent hydroxyurea from being offered to more patients who might benefit from treatment. Perhaps the greatest barriers must be overcome at the level of the medical community: healthcare providers should consider SCD a hematological disorder worthy of treatment, before patients develop acute events and chronic organ damage. SCD is a chronic hematological condition that warrants treatment even in the absence of obvious, clinically overt complications. Patients with SCD at steady-state are not necessarily “doing well”; instead, they have a serious medical condition that should be treated in an early and aggressive manner. Only more data will determine whether hydroxyurea treatment stands the test of time for SCD, but until another and better therapeutic option comes along, we should make this powerful and effective agent available to more children, adolescents, and adult patients with SCD.
Summary of the NIH OMAR-commissioned systematic review of literature for efficacy, effectiveness, toxicity, and barriers to use of hydroxyurea among adults and children with sickle cell disease (SCD). Adapted from Lanzkron et al16 and Strouse et al.17
Disclosures Conflict-of-interest disclosures: The authors declare no competing financial interests. Off-label drug use: Hydroxyurea for children with sickle cell anemia.
References
Author notes
Department of Hematology, St. Jude Children’s Research Hospital, Memphis TN