Abstract
Hematopoietic stem cell (HSC)–targeted gene transfer is an attractive approach for the treatment of a number of hematopoietic disorders caused by single gene defects. Indeed, in a series of gene transfer trials for two different primary immunodeficiencies beginning early in this decade, outstanding success has been achieved. Despite generally low levels of engrafted, genetically modified HSCs, these trials were successful because of the marked selective advantage of gene-corrected lymphoid precursors that allowed reconstitution of the immune system. Unlike the immunodeficiencies, this robust level of in vivo selection is not available to hematopoietic repopulating cells or early progenitor cells following gene transfer of a therapeutic globin gene in the setting of β-thalassemia and sickle cell disease. Both preclinical and clinical transplant studies involving bone marrow chimeras suggest that 20% or higher levels of engraftment of genetically modified HSCs will be needed for clinical success in the most severe of these disorders. Encouragingly, gene transfer levels in this range have recently been reported in a lentiviral vector gene transfer clinical trial for children with adrenoleukodystrophy. A clinical gene transfer trial for β-thalassemia has begun in France, and one patient with transfusion-dependent HbE/β-thalassemia has demonstrated a therapeutic effect after transplantation with autologous CD34+ cells genetically modified with a β-globin lentiviral vector. Here, the development and recent progress of gene therapy for the hemoglobin disorders is reviewed.
The hemoglobin disorders are highly prevalent, recessive genetic diseases in which co-inheritance of two defective globin alleles results in severe hematological disease. Patients with the β-globin disorders, sickle cell disease (SCD) and β-thalassemia suffer severe anemia and a myriad of other problems affecting numerous organ systems. In patients with SCD, the beta chain contains a substitution of valine for glutamic acid at position 6.1 This substitution results in a change in surface charge that predisposes deoxygenated HbS to polymerize, causing red cells to assume rigid sickled shapes, leading to severe anemia, vaso-occlusion, painful crises and organ damage. Although drug and transfusion therapies improve the quality and duration of life for many individuals, developing curative treatments for SCD remains the desired goal. The only curative therapy, hematopoietic stem cell (HSC) transplantation, has been performed on about 200 patients with SCD worldwide.2,3 Most patients have received bone marrow (BM) transplantation from HLA-matched siblings, with a highly successful outcome. However, this approach is available only for a minority of patients due to lack of available, matched donors. Unfortunately, a 5% to 10% mortality rate due to regimen-related mortality (infection) and graft-versus-host disease3,4 continues to be problematic.
Unlike SCD, in which there are normal levels of an abnormal β-globin protein that causes the pathophysiology, β-thalassemia results from deficient β-globin chain synthesis due to a variety of deletions and mutations in the β-globin gene or its upstream regulatory elements. Patients with markedly reduced or no β-globin expression rely on routine red cell transfusion therapy for survival and quality of life. Advances in chelation therapy, including the recent availability of oral chelators, have improved the quality of life and potential for longevity in these patients.5 However, iron overload, particularly in the heart, remains a significant issue, despite chelation that is adequate to unload the liver.6 In comparison with stem cell transplantation for SCD, almost 1600 stem cell transplants have been performed worldwide for β-thalassemia.7 Great success has been obtained with matched-sibling allogeneic transplants for patients with early stage disease. However, as for SCD patients, early mortality can occur in 5% to 10% of patients. For patients with later stage disease, the outcome is less favorable. Similarly, transplantation using matched, unrelated donors has been problematic.8 Thus, substantial efforts have been invested in the development of gene transfer into autologous HSC as an alternative therapy with curative intent.
Murine Leukemia Virus as a Vector to Transfer Genes into Blood Stem Cells: Success in Two Immunodeficiency Disorders
A critical element in developing gene therapy for blood disorders was the research focusing on identifying an effective vector system for gene transfer into hematopoietic cells. In the early 1980s, gene transfer vectors based on the murine leukemia retrovirus (MLV) were developed that could successfully and stably transfer a marker gene into the genome of HSCs in murine models.9,10 These MLV-based vectors utilize the powerful enhancer and promoter elements within the long-terminal repeat (LTR) at the 5′ end of the viral genome to drive transgene expression. Replication-incompetent, recombinant vectors were derived by replacing the viral genes with a marker gene or other gene of interest. Fibroblast cell lines, stably expressing both the recombinant vector genome and the required components of the viral particle, were used to produce the vector. Years later, these efforts culminated in the success of human clinical trials for two severe combined immunodeficiencies (SCID). To date, more than 30 patients with SCID secondary to deficiency of the common gamma chain (X-SCID1) or due to adenosine deaminase (ADA) deficiency have been successfully treated using MLV-based vectors encoding either the common gamma chain or the ADA enzyme, respectively.11,–14 Despite this success, vector-mediated insertional activation of nearby proto-oncogenes initiated the development of leukemia in five patients treated for common gamma chain deficiency, highlighting the importance of the role of vector design in the safety of gene therapy.11,15 These trials provided encouragement for continued effort to develop stem cell–targeted gene therapy for hemoglobin disorders, while at the same time focusing new attention to vector safety.
Lentiviral Vectors Emerge as an Effective System to Mediate Gene Transfer and High-Level Expression of Globin Genes
MLV-based globin gene vectors, as opposed to the relatively simple MLV vectors used in the X-SCID1 and ADA trials, proved challenging to design and produce due to the requirement to include specific endogenous regulatory elements from the β-globin locus that were obligatory to achieve adequate expression. Despite more than a decade of intensive efforts by several laboratories to develop MLV-based globin retroviral vectors, a potentially therapeutically useful vector design was never identified.16
In the mid-1990s, the development of lentiviral vectors based on the human immunodeficiency virus (HIV)17 is now recognized as a key milestone that made possible the subsequent development of globin lentiviral vectors. Indeed, a significant breakthrough in the globin gene therapy field occurred in 2000 when an HIV-based, globin lentiviral vector was used to cure a mouse model of β-thalassemia intermedia.18 The lentiviral vector backbone, coupled with the nuclear to cytoplasmic RNA export system utilized by HIV, made possible the transmission of a β-globin expression cassette containing a large constellation of regulatory elements. Unlike the MLV-based globin vectors, this lentiviral vector transmitted the globin regulatory and coding sequences without rearrangement and could be produced in sufficient titer. Since then, additional reports describing use of globin lentiviral vectors to correct murine β-thalassemia and SCD models have emerged (see below).
Recently, it has been reported that relatively high levels of lentiviral vector-mediated HSC gene transfer were obtained in a clinical trial for children with cerebral X-linked adrenoleukodystrophy (ALD), a demyelinating disease due to deficiency of an enzyme that breaks down very long chain fatty acids. Three children enrolled in this trial in France have been described.19 After pre-transplant conditioning with myeloablative doses of busulfan and cyclophosphamide, the patients received autologous, cytokine-mobilized peripheral blood CD34+ cells transduced with a lentiviral vector encoding the ALD enzyme. As reported by Dr. Natalie Cartier at the 2009 American Society of Gene Therapy Annual Meeting, 10% to 20% of the peripheral blood cells in these patients contain the vector, with follow-up ranging from 9 to 30 months. There may be some therapeutic effect as measured by the slowing or cessation of central nervous system disease. Notably, these results demonstrate that lentiviral vectors can mediate significant levels of gene transfer into human HSCs.
Correction of Murine and Human Models of β-thalassemia and SCD
Sadelain and colleagues were the first to demonstrate that a lentiviral vector encoding human β-globin could be used to cure a murine model severe β-thalassemia.18 In this and a follow-up study, they showed significant long-term hematologic and pathologic correction using a β-globin vector containing a somewhat large constellation of regulatory elements from the β-globin locus control region (LCR) totaling 3.2 kb in size.20 Approximately 80% of the HSCs were genetically modified, resulting in chimeric hemoglobin molecules incorporating human β-globin comprising about 21% of total hemoglobin. In another study, at least one copy of a lentiviral β-globin vector in every stem cell was required to correct severe murine β-thalassemia.21 The fact that correction in these experiments required most or all of the HSCs to be modified suggested that inconsistent globin expression could be occurring, as it was well known that location in the genome could affect expression of transgenes. In a different study and further supporting this possibility, only 1 of 6 animals in a model of thalassemia major demonstrated a relatively high level of hemoglobin following the gene transfer procedure despite nearly all the HSCs being genetically modified. The remaining animals remained severely anemic with a thalassemia intermedia phenotype.22
Leboulch and colleagues were the first to demonstrate hematologic correction and diminished end organ damage in murine SCD using lentiviral-mediated HSC gene transfer of an anti-sickling variant of the human β-globin chain.23 An average vector copy number of 3 in the HSCs was observed with dependence of globin transgene expression on genomic position. Subsequently, others confirmed this result by using a different SCD model and a slightly different anti-sickling β-globin variant. Phenotypic improvement with an average vector copy of 2.2 resulted in hemoglobin tetramers incorporating the transgene globin chain at a level of 20% of the total hemoglobin.24
Because increased fetal hemoglobin (HbF; α2γ2) levels naturally ameliorate the clinical severity of both β-thalassemia and sickle cell anemia, γ-globin MLV-based and lentiviral vectors have been developed and tested as an alternative to β-globin vectors.25,–27 HbF acts as a natural anti-sickling hemoglobin in part because of formation of mixed tetramers, α2γβS, which do not participate in polymer formation.28 A γ-globin lentiviral vector containing 1.7 kb of LCR elements to drive expression of the human Aγ-globin gene showed therapeutic efficacy in a murine model of severe β-thalassemia, with significant disease correction achieved with a copy number of 2 to 2.5 in the HSCs.27 Position-dependent expression of the globin vector was also observed and was a significant factor that affected efficacy. Hanawa et al subsequently developed a second generation γ-globin lentiviral vector, having more extensive LCR-derived regulatory sequences.29 This vector, shown to be less susceptible to position effects, was able to produce higher and more consistent levels of HbF, and one vector copy per cell was curative.29
Globin lentiviral vectors have also been used to transfer a β-globin gene into normal human hematopoietic cells capable of establishing hematopoiesis in immunodeficient mice.30 Correction of the β-thalassemia phenotype in patient cells was demonstrated by the establishment of effective erythropoiesis in erythroid cultures, both in marrow cells from patients cultured in vitro and in cells obtained from immunodeficient mice several months after transplant with the patients’ genetically modified primitive cells.31
Preclinical Studies of Globin Lentiviral Vectors: What We Have Learned
From the above studies, we can conclude that therapeutically adequate levels of globin protein expression can be obtained following HSC gene transfer by using lentiviral vectors containing a relative large and complex set of endogenous β-globin regulatory elements. However, the genomic site of integration can affect the level of globin expression. One potential solution to this problem has been to use DNA elements called “insulators,” which are DNA elements in the genome that can function both as barrier elements to dampen position effects and enhancer blockers to prevent nearby genes from interacting with one another32. Inclusion of such elements in globin vectors may reduce, but not eliminate, the problem of variable expression due to position of the vector in the genome.33 However, addition of insulator elements to the vector design can hamper vector production and may prevent successful scale up for clinical trials.34,35 Thus, many laboratories are now focusing on identifying functional “insulator” elements that will not dramatically affect vector titer.34,36
Highly efficient transduction of HSCs has been obtained with globin lentiviral vectors in mice (almost every HSC can be transduced) and this facilitated the ability to “cure” the various globin disease models. High concentrations of vector particles are required during the ex vivo transduction process. Thus, it has remained unclear whether significant levels of lentiviral vector-mediated gene transfer could be obtained for human HSCs. Encouragingly, the lentiviral vector trials described above and below suggest that HSC gene transfer rates of 10% or higher can be obtained in humans. However, these rates remain much lower than those obtained in mice and suggest that further research aimed at improving lentiviral vector gene transfer into human HSCs is worthwhile.
Side Effects of Retroviral Gene Transfer: Insertional Gene Activation
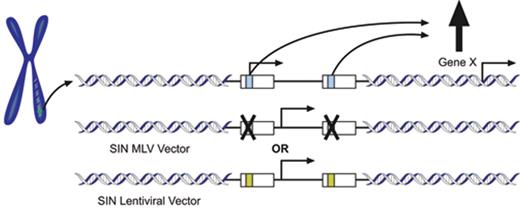
Despite the enormous success of the X-SCID1 gene therapy trials, with many patients demonstrating substantial improvements in their clinical and immunological status, four patients in the trial in France and one in the United Kingdom subsequently developed lymphoid leukemia due, in part, to vector-mediated insertional mutagenesis.15,37,–39 In another trial for chronic granulomatous disease (CGD), insertional gene dysregulation resulted in the outgrowth of myeloid clones.40 In these cases, the aberrant gene expression caused by the vector integration was due to the effects of the enhancer elements present in the LTR of the vector (Figure 1 ). This information is detailed elsewhere in this volume. These results prompted investigators to develop new in vitro and in vivo assays to measure vector genotoxicity.41 –44
Subsequent studies using these new assays indicated that lentiviral vectors may be a safer alternative to the LTR-containing, MLV-based vectors used in the X-SCID1 and CGD trials.42,43 Similarly, MLV-based vectors that have been modified to delete the enhancer and promoter elements within the LTR also show less genotoxicity in these assays.45 In both the lentiviral and modified MLV vectors, an internal promoter is used to direct transgene expression. Less powerful cellular promoters seem to be the best choice for driving transgene expression while minimizing potential effects on genes surrounding the insertion site.45 For this approach to be successful, such weaker promoters by necessity must be capable of directing therapeutic expression levels of the particular transgene in the appropriate cellular context. An effective vector design for a particular disorder will need to be identified empirically through studies in mice and human cells.
Globin Gene Transfer Clinical Trials
One clinical gene transfer trial for patients with β-thalassemia and SCD using globin lentiviral vectors is underway in France,46 while other groups, including our own, are planning to begin trials in the United States in the near future.47 As reported at the American Society of Gene Therapy Annual Meeting (May 2009) and detailed by the French Medicine Agency48 and the NIH Office of Biological Activities,49 Leboulch and colleagues, in a clinical trial sponsored by Genetix France, have treated two patients with β-thalassemia in Paris. The patients underwent bone marrow harvest and enriched CD34+ cells were transduced with a lentiviral vector containing β-globin locus regulatory elements driving expression of a β-globin protein with a mutation at amino acid 87. Initially developed as an anti-sickling β-globin variant,23 the use of the variant in this setting allowed vector-encoded β-globin to be distinguished from low levels of endogenous β-globin.
The first patient, with transfusion-dependent β-thalassemia major, received ex vivo transduced autologous CD34+ cells following myeloablative pre-transplant conditioning with high-dose busulfan. Unfortunately, the patient had prolonged post-transplant cytopenia and eventually received frozen, backup CD34+ cells for hematopoietic rescue. The second patient, a 19-year-old male with HbE/β-thalassemia, also received autologous, vector-transduced CD34+ cells (~4 × 106 cells per kg) following a myeloablative dose of busulfan in June 2007. The patient had hematologic reconstitution about five weeks post-transplant. In mid-2008, the patient became transfusion independent with a stable hemoglobin level above 9 g/dL. DNA analysis showed that about 10% of peripheral blood myeloid cells were genetically modified with the vector. Interestingly, of the ~9 g/dL of hemoglobin, one third was found to be composed of endogenous HbE, one third composed of vector-encoded β-globin, and, somewhat surprisingly, one third composed of HbF. Regarding this last observation, it is notable that several β-thalassemic and sickle cell patients who underwent allogeneic transplantation but subsequently rejected the donor grafts have been reported to have therapeutic levels of HbF following reconstitution with endogenous HSCs.50,51 Thus, it appears that the vector-encoded β-globin and “reactivation” of HbF expression both contributed to the therapeutic efficacy in this case.
Despite the clinical improvement of the patient, it was reported on May 27, 2009 by the French Medicine Agency that the patient was found to have a “relative clonal dominance.” Of the 10% or so of genetically modified cells, one clone, identified as having integration in the HMGA2 gene, was present in excessive proportion relative to the contributions of other clones, as identified by their genomic vector integration sites. The potential clinical relevance of alteration of HMGA2 expression by the vector integration is highlighted by the fact that this gene has been implicated as a potential oncogene in a variety of settings.52 –54 It is known to be a chromatin-binding protein that interacts with transcription factors to regulate gene expression. One noteworthy observation is that in some tumors, HMGA2 is translocated with the breakpoint in intron 3, which leads to production of a truncated protein. Interestingly, the vector integration in this case occurred in intron 3, potentially leading to generation of a similarly truncated protein. Thus, the potential for growth perturbation is raised by this vector insertion. However, as pointed out by the OBA in their announcement, the amount of this particular clonal population has been stable for five months and the patient is doing well.
As presented by Dr. Leboulch at the American Society of Gene Therapy Annual Meeting in 2009, it remains unclear whether the vector insertion into this gene was contributory to the relatively high contribution of this clone to hematopoiesis. Ongoing laboratory studies and continued intensive clinical and molecular monitoring of this patient should eventually resolve whether this particular integration by the globin vector caused a growth perturbation. At this point, it seems plausible that these observations may alternatively reflect the consequences of engraftment from a small number of transduced HSCs. Both patients treated thus far in the trial demonstrated delayed hematopoietic reconstitution, consistent with this interpretation. In the context of a small dose of transplanted cells, clonal dominance can occur by chance without the requirement for increased fitness or proliferative capacity.55
Conclusions
Significant progress has been made in the last decade in advancing HSC gene transfer for the treatment of blood disorders. Remarkable success has been obtained in several trials for X-SCID1 and ADA deficiency. However, the X-SCID1 trials highlighted the problem of vector insertional gene dysregulation associated with the use of MLV-based vectors containing strong enhancer elements. Two current strategies that have been proposed to address this problem are (1) the use of MLV-based vectors lacking the powerful LTR enhancer elements and instead using internal cellular promoters and (2) the use of an “insulated” lentiviral vector also exploiting a cellular promoter to drive gene expression. Two new trials for X-SCID1 using these approaches have been reviewed by the Recombinant DNA Advisory Committee within the last year.56
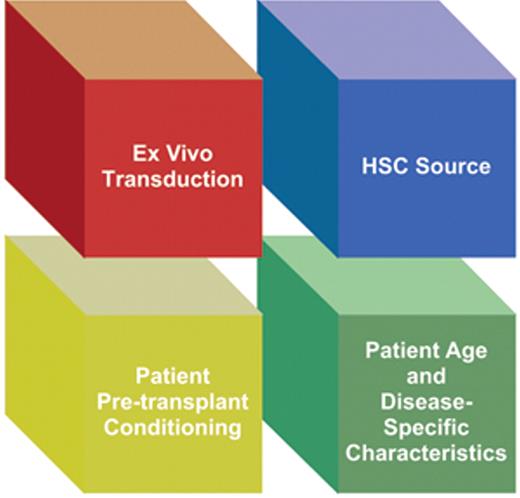
Compared with the immunodeficiency and ALD trials, clinical gene transfer trials for the hemoglobin disorders may face a unique set of challenges (Figure 2 ). First, in the initial trials for hemoglobin disorders, the patient population for enrollment will likely be older than for the other trials, which have enrolled young children. There is some evidence suggesting that the primitive repopulating cells of young patients may be more amenable to gene transfer than those of adults.19,57,58 Therefore, determining the most optimal HSC source for gene transfer and transplantation in the context of hemoglobin disorders will likely be important in achieving success. Although steady state bone marrow CD34+ cells were used as the source of HSCs for gene transfer in the first globin gene transfer trial, others are evaluating whether cytokine mobilization of peripheral blood CD34+ cells in patients with β-thalassemia might be safe and effective as an alternative way to collect HSCs (http://clinicaltrials.gov/ct2/show/NCT00336362).
Additionally, the ex vivo transduction process might be improved by methods to minimize the potential toxicity of the vector preparation. This is particularly relevant for globin lentiviral vectors, which are often significantly concentrated for use in gene transfer studies. One avenue being pursued is the use of lentiviral vector producer cells to produce large quantities of clinical grade vector that can subsequently be purified through downstream processing.59 On the patient side, the degree and type of myeloablation for patients with β-thalassemia and SCD that will allow sufficient engraftment of genetically modified HSCs remains undefined. The ALD and the β-thalassemia trials used full myeloablation with busulfan to achieve engraftment with 10% to 20% gene modified HSCs. Higher-efficiency HSC gene transfer would perhaps allow the degree of myeloablation to be reduced. Finally, it is not yet known whether any disease-specific factors of the hemoglobin disorders will affect the many aspects of the treatment process negatively. Despite these uncertainties, researchers in the field remain optimistic that, with continued efforts, HSC gene transfer to treat β-thalassemia and SCD is likely to become a useful therapeutic option for patients with these diseases.
Mechanism of vector insertional gene activation. A genomic integration site of a MLV-based retroviral vector in a target cell is depicted. With this MLV vector design, the enhancer and promoter within the U3 region (blue rectangle) of the long terminal repeat (LTR; white rectangles) drive transcription of the transgene (indicated by the parallel arrow arising from the blue rectangle). At top is shown a vector integration near Gene X. The enhancer elements located in the U3 region (blue rectangle) of the vector can interact with the regulatory elements upstream of Gene X to increase the basal level of transcription to inappropriately high levels, potentially altering the growth of the cell. Two alternatives to eliminate the use of the powerful enhancer in the U3 include 1) middle panel: use of a self-inactivating (SIN) MLV-based vector in which the U3 region has been deleted (noted by X) and which utilizes an internal cellular promoter to drive transgene expression (parallel arrow) and 2) bottom panel: use of a SIN lentiviral vector in which the U3 (yellow rectangle) has also been eliminated and, like the SIN MLV vector, uses an internal cellular promoter to drive transgene expression.
Mechanism of vector insertional gene activation. A genomic integration site of a MLV-based retroviral vector in a target cell is depicted. With this MLV vector design, the enhancer and promoter within the U3 region (blue rectangle) of the long terminal repeat (LTR; white rectangles) drive transcription of the transgene (indicated by the parallel arrow arising from the blue rectangle). At top is shown a vector integration near Gene X. The enhancer elements located in the U3 region (blue rectangle) of the vector can interact with the regulatory elements upstream of Gene X to increase the basal level of transcription to inappropriately high levels, potentially altering the growth of the cell. Two alternatives to eliminate the use of the powerful enhancer in the U3 include 1) middle panel: use of a self-inactivating (SIN) MLV-based vector in which the U3 region has been deleted (noted by X) and which utilizes an internal cellular promoter to drive transgene expression (parallel arrow) and 2) bottom panel: use of a SIN lentiviral vector in which the U3 (yellow rectangle) has also been eliminated and, like the SIN MLV vector, uses an internal cellular promoter to drive transgene expression.
Factors that are likely to influence the outcome of a gene transfer trial for the hemoglobin disorders. Knowledge regarding each component will likely facilitate successful gene therapy of hemoglobin disorders. HSC source, ex vivo cell manipulation and transduction conditions will be important components in determining efficient HSC gene transfer and subsequent engraftment. Patient age and disease-specific factors may influence these parameters. Finally, engraftment will be influenced by the type and amount of pre-transplant conditioning.
Factors that are likely to influence the outcome of a gene transfer trial for the hemoglobin disorders. Knowledge regarding each component will likely facilitate successful gene therapy of hemoglobin disorders. HSC source, ex vivo cell manipulation and transduction conditions will be important components in determining efficient HSC gene transfer and subsequent engraftment. Patient age and disease-specific factors may influence these parameters. Finally, engraftment will be influenced by the type and amount of pre-transplant conditioning.
Disclosures Conflict-of-interest: The author declares no competing financial interests. Off-label drug use: None disclosed.
References
Author notes
Division of Experimental Hematology, Department of Hematology, St. Jude Children’s Research Hospital, Memphis, TN