Abstract
Despite big advances in antimicrobial therapies and infection strategies, the emergence of antibiotic resistance represents an emergency situation, especially in immunocompromised hosts. Specifically, infections due to multidrug resistant, gram-negative pathogens are responsible for high mortality rates and may leave few effective antimicrobial options. Furthermore, although new compounds are available for severe methicillin-resistant staphylococcal infections, there is a paucity of novel classes of antimicrobials to target resistant gram-negatives. A careful assessment of the clinical conditions and underlying comorbidities, along with knowledge about the previous history of colonization or infections due to multidrug-resistant bacteria, represent key points in approaching the hematological patient with signs of infection. A de-escalation therapy with initial use of wide-spectrum antimicrobials followed by a reassessment after 72 hours of treatment may represent a good option in severe infections if a resistant pathogen is suspected. Prompt empiric or targeted therapy using combination regimens (ie, antipseudomonal beta-lactam plus an aminoglycoside or a quinolone) with the addition of colistin, along with increased dosage and therapeutic drug monitoring, represent options for these life-threatening infections. Continuous epidemiological surveillance of local bacteremias is necessary, along with stringent enforcement of antibiotic stewardship programs in cancer patients.
Introduction
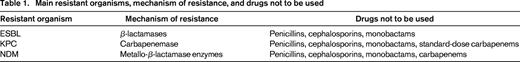
Reemergence of gram-negative infections and increased antimicrobial resistance due to overuse of antibiotics in cancer patients have changed the epidemiology of bacteremia in neutropenic patients in the past decade1-4 Classically, gram-positive organisms have been the predominant bacterial pathogens in this setting.5,6 Among gram-negatives, which are isolated in up to 80% of polymicrobial bacteremias, Escherichia coli, Klebsiella spp., and Pseudomonas aeruginosa remain the predominant species, although other Enterobacteriaceae, Stenotrophomonas maltophilia, and Acinetobacter spp. can also be isolated.7-9 Of particular challenge are the infections due to methicillin-resistant Staphylococcus aureus (MRSA), representing up to 50% of all staphylococcal infections; vancomycin-resistant enterococci (VRE), representing nearly 30% in the United States; extended-spectrum beta-lactamase (ESBL)–producing gram-negative bacteria; and other multidrug-resistant (MDR) organisms such as A. baumannii, Klebsiella pneumoniae carbapenem-resistant (KPC), P aeruginosa, and fluoroquinolone-resistant E coli10-12 (Table 1).
Although recent clinical practice guidelines recommend prophylaxis with ciprofloxacin or levofloxacin during profound neutropenia in acute leukemia and hematopoietic stem cell transplantation, their widespread use has been linked with a rising prevalence of MDR pathogens including gram-negatives, MRSA, and VRE.3,4
The use of inappropriate antibiotic regimens and, consequently, the delay in starting appropriate treatment account is considered the main cause for poor outcomes in severe infections, especially among human stem cell transplantation recipients during the early posttransplant period.13,14 The identification of risk factors associated with the development of MDR infection is important to guide the strategies that may decrease their adverse impact.15 Furthermore, different factors can affect in diverse ways the development of infections in hematological patients, including the duration and the severity of granulocytopenia, the mechanical defence damage (such as the presence of mucositis, use of central venous catheters [CVCs], tumor infiltration), and the reactivation of previous infections due to immunosuppression. Therefore, the initial approach to hematological patients with a suspected drug-resistant infection includes the evaluation of underlying disease, the severity and the duration of the immunodeficiency, the presence of additional predisposing factors to infections, and the severity of clinical presentation.
Bloodstream infections (BSIs, including CVC-related BSIs), pneumonia, and mucositis represent the majority of infectious sites. In this setting, prompt initiation of an appropriate empiric therapy, reassessment after the availability of susceptibility test, and the continuation of a targeted therapy taking into account the patient comorbidities, type and site of the infection, and pathogen resistances may contribute to a reduction of the mortality.
Below we discuss the different approaches and the antimicrobial strategies for empiric and targeted therapies in hematological patients presenting with severe infections.
How to treat resistant infections in hematological patients
1. Initial clinical assessment and risk factors for resistant infections
In the selection of an antimicrobial therapy to approach a patient with febrile neutropenia, of key importance is a knowledge of the epidemiology and resistance patterns at each single institution. Also of paramount importance is the obtainment of a detailed medical history of the patient's colonization and the documentation of previous infections caused by resistant pathogens.
A patient's age, comorbidities, duration of aplasia, and complications (eg, bleeding, dehydration, liver and kidney failure) should be assessed, along with the clinical parameters that are evocative of a severe infectious process (septic shock or hemodynamic instability, sensory loss) and a localized infection (pneumonia, enteritis, catheter-related infection).
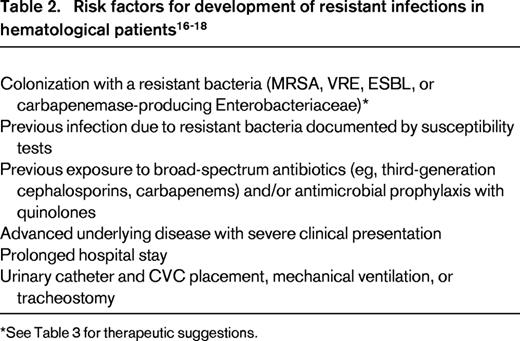
Risk factors including known colonization with resistant bacteria, previous infections, or exposure to broad-spectrum antibiotics (ie, beta-lactams and quinolones), advanced underlying disease with severe clinical presentation, prolonged hospital stay, and catheter placement (ie, urinary catheters for ESBL-associated infections and CVCs for MRSA) should be taken into consideration during the initial approach to high-risk hematological patients (Table 2).
2. Choice of empiric therapy regimens
A classic approach is represented by escalation therapy consisting of an initial empiric monotherapy using a beta-lactam (eg, ceftazidime, cefepime, or piperacillin-tazobactam) targeting Enterobacteriaceae and P aeruginosa infections without ESBL or carbapenemase-producing gram-negative coverage. If clinical deterioration or isolation of a resistant pathogen occurs, then therapy is escalated using an antibiotic with a broader spectrum or a combination of antimicrobials.
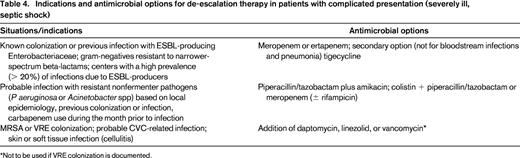
This approach may be inappropriate in the following instances: compromised patients with severe presentation; a hospital setting in which a high prevalence of ESBL-producing bacteria (> 20%) is reported; and patients with previous history of colonization or infection due to resistant pathogens (Table 3) or presenting with risk factors for resistances. In these cases, the escalation approach may lead to an initial inadequate antimicrobial treatment with a potentially negative impact on the outcome. In these cases, another approach is represented by de-escalation therapy starting from a very broad initial regimen possibly covering highly resistant pathogens and followed (after a reassessment at 48-72 hours) by a step-down therapy upon availability of susceptibility tests. Antimicrobials used in these regimens include monotherapy with a carbapenem or antimicrobial associations targeting gram-negative pathogens (eg, colistin with a beta-lactam or an aminoglycoside plus a beta-lactam) and gram-positive resistant bacteria, if specific risk factors are identified. Fluoroquinolones are recommended as a possible part of a combination therapy only in patients who were not receiving fluoroquinolone-based prophylactic regimens. Early coverage of resistant gram-positives using a glycopeptide or newer agents (eg, linezolid or daptomycin) should be used if risk factors for gram-positive infections, such as CVC placement, mucositis, or soft tissue involvement are present.
Although characterized by high efficacy as an empiric first-line treatment of febrile neutropenia, carbapenems should be avoided in uncomplicated patients lacking risk factors for resistant bacteria to preserve their activity for seriously ill patients. Nevertheless, centers with reported high rates of resistance due to ESBL production (> 20%) or carbapenemase-producing organisms should undergo a prompt infection control review.
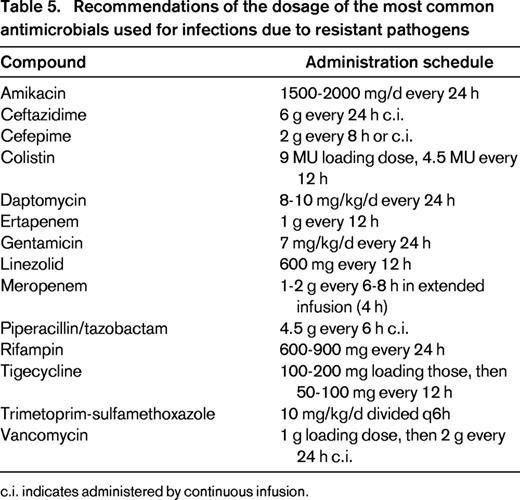
Details regarding the indications, the antimicrobial options for a de-escalation approach, and the suggested dosages are summarized in Tables 4 and 5. In general, a case-by-case adjustment of the initial regimen should be considered after 24 to 72 hours according to the clinical course and the microbiological results.
After the start of an escalation therapy, there may be no availability of microbiological documentation. In this case, the antimicrobial therapy should be changed if the patient presents persistent fever in association with deteriorating clinical conditions. Furthermore, investigation of the infectious source through repeated microbiological cultures, imaging (CT scan, MRI), and nonculture tests (eg, galactomannan, beta-glucan) is warranted. The new empiric regimen should include resistant gram-negative pathogens and should be based on the documentation of previous infections, prior use of wide-spectrum antimicrobials, and patient risk factors. Combination therapies including colistin and/or carbapenems may represent valid options.
In cases requiring a de-escalation approach without microbiological tests available, the antimicrobial regimen should be reassessed after 48 to 72 hours and changed as follows. In cases of clinical stability, a narrower-spectrum agent is preferred. To avoid renal toxicity and selection of resistances, aminoglycosides and quinolones should be discontinued. In cases of persistent fever or clinical deterioration, the presence of a resistant organism [eg, carbapenem-resistant P aeruginosa, KPC, New-Delhi metallo-beta-lactamase (NDM-1) E coli] or the occurrence of an infection due to MRSE, VRE, or a fungal infection should be suspected. Addition of colistin to a carbapenem monotherapy and anti-gram-positive agents may be performed, along with adequate imaging and nonculture tests to detect possible fungal infections.
3. Targeted therapy for severe infections in hematological patients
If a bacterial infection is documented, the results of the in vitro susceptibility tests, including minimum inhibitory concentration (MIC) when possible, should be used to guide the appropriate antibiotic regimen. Nevertheless, depending on the clinical indication and the site of the infection, agents with the less broad spectrum should be used when the same in vitro susceptibility is detected for more than one compound to prevent resistances. If MDR pathogens are detected, consultation with an infectious disease expert or clinical microbiologist is always recommended.
Furthermore, because hematological patients often present specific pathophysiological conditions that may alter the pharmacokinetic behavior of antimicrobials, different administration schedule and antimicrobial dosing regimens from the standard ones may be required. Specifically, increased dose (eg, aminoglycosides, fluoroquinolones, daptomycin), prolonged infusion (eg, beta-lactams), and therapeutic drug monitoring are important to optimize the antimicrobial therapy. A summary of the suggested antimicrobial schedule doses for severe infections in hematological patients is provided in Table 4.
Among MDR infections, particularly challenging are the infections due to difficult-to-treat MDR gram-negatives such as P aeruginosa and K pneumoniae (including KPC) because of the limited antimicrobial options available, along with reported high mortality rates.19 In this context, the role of combination therapy has been advocated to provide broader coverage, prevent emergence of reduced susceptibility, and achieve bacterial synergy.20-22 In pseudomonal infections, an initial combination therapy significantly reduced the likelihood of inappropriate therapy, although similar outcomes are reached using a targeted therapy once the susceptibility is documented.23 Conversely, association of at least 2 active compounds (eg, colistin and high doses of meropenem, 6 g/d, with tigecycline or gentamycin) has been linked to increased survival rates in severe KPC-related infections.21,24
Involvement of gram-positive pathogens is common in CVC-related infections and pneumonia. In these instances, antistaphylococcal drugs should include those with activities toward MRSA. Nevertheless, the widespread use of vancomycin has been related to the emergence of strains of MRSA with increased MIC to vancomycin (> 1 mg/L) causing severe infections.25 Particularly, low eradication rates and increased mortality have been documented in MRSA-related BSIs and pneumonia when high MIC values to vancomycin were reported.26-28 Daptomycin is highly active against MRSA BSIs and has shown to affect outcomes in cancer patients with BSIs, causing a faster resolution of symptoms compared with vancomycin.29 In cases of MRSA nosocomial pneumonia, linezolid has exhibited a better performance than vancomycin with regard to clinical efficacy and pathogen eradication and can be a valid choice for an empiric choice, although limitations can be posed due to its BM suppression in hematological patients.30
Conclusions
MDR infections pose a real threat to immunocompromised patients, causing severe infections with poor outcomes. The increase in infections caused by gram-negative and gram-positive resistant bacteria is concerning for the success of empiric treatment of febrile neutropenia. Immediate evaluation, risk assessment, and treatment with empiric broad-spectrum antibiotics are warranted when a resistant infection is suspected in hematological patients with severe immune impairment. Reassessment after 48 to 72 hours from the beginning of an empiric treatment should always be done to avoid an unnecessary use of wide-spectrum antibiotics that are not required or to choose an appropriate targeted therapy in case of documented multiple resistances. Nevertheless, efforts to reduce the risk of febrile neutropenia should be based on appropriate antimicrobial stewardship and infection control policies.
Disclosures
Conflict-of-interest disclosure: M.B. has received research funding from MSD, Novartis, and Astellas; has consulted for Vifor, Trius, Bayer, MSD, Novartis, Astellas, Pfizer, Roche, and Basilea; has received honoraria from Gilead, Bayer, MSD, Novartis, Astellas, AstrazZeneca, and Pfizer; and has been affiliated with the speakers' bureau for Vifor, Gilead, Bayer, MSD, Novartis, Astellas, AstraZeneca, and Pfizer. E.R. declares no competing financial interests. Off-label drug use: None disclosed.
Correspondence
Matteo Bassetti, MD, PhD, Clinica Malattie Infettive, Azienda Ospedaliera Universitaria Santa Maria della Misericordia, Piazzale Santa Maria della Misericordia 15, 33100 Udine, Italy; Phone: 39-0432-559355; Fax: 39-0432-559360; e-mail: mattba@tin.it.