Abstract
Pain is the most common cause for hospitalization and acute morbidity in sickle cell disease (SCD). The consequences of SCD-related pain are substantial, affecting both the individual and the health care system. The emergence of the patient-centered medical home (PCMH) provides new opportunities to align efforts to improve SCD management with innovative and potentially cost-effective models of patient-centered care. The Department of Health and Human Services has designated SCD as a priority area with emphasis on creating PCMHs for affected patients. The question for patients, clinicians, scientists, and policy-makers is how the PCMH can be designed to address pain, the hallmark feature of SCD. This article provides a framework of pain management within the PCMH model. We present an overview of pain and pain management in SCD, gaps in pain management, and current care models used by patients and discuss core PCMH concepts and multidisciplinary team–based PCMH care strategies for SCD pain management.
Introduction
Despite clinical innovations in medical care and improved survival among individuals with sickle cell disease (SCD),1,2 pain and its management continue to pose a substantial challenge for patients, families, clinicians, scientists, and policy makers. Pain is an unpredictable and hallmark feature of SCD, presenting in acute, chronic, neuropathic, or mixed forms.3 Its impact in SCD is enormous with respect to health care utilization,4-8 financial strain on the health care system,9 quality of life,10 and lifelong productivity. The estimated annual cost of medical care for the ∼ 70 000 individuals with SCD in the United States exceeds $1.1 billion.9 Although hydroxyurea may modulate underlying disease,11 it will not completely prevent SCD-related pain and carries its own set of considerations.
Adults and children with SCD may seek care for pain management in a variety of clinical care settings. Patients may be cared for by primary care providers with limited experience, ancillary support, and time to manage SCD-related pain.12 Other patients may predominantly seek care in hospitals, where providers may be emergency room (ER) physicians or hospitalists with varying expertise in managing SCD pain. Care delivery initiatives, such as the establishment of day hospitals for acute SCD pain,13-15 have provided adults and children with access to expert care and reduced hospitalizations and length of stay. However, the day hospital only improves the episodic nature of pain and does not address the chronic, multidisciplinary challenges of SCD-related pain. Comprehensive SCD centers provide specialist-led, multidisciplinary models of care. Such centers provide diverse services and ongoing chronic disease management, including patient education, pain control, and psychosocial services. However, the data on outcomes are mixed and only a minority of adults and children with SCD have access to these centers or hematologists in general.8
The patient-centered medical home (PCMH) is emerging as the cornerstone of efforts to reform chronic disease management in the US health care system and to transform primary care into a centerpiece for improving health care quality.16 The PCMH can be envisioned as a multidisciplinary team of providers focused on a patient's needs, with care functions and team processes coordinated through integrated HIT.17 Studies on PCMH have demonstrated trends toward improvements in quality, patient experience, and system efficiency for both adults and children.18,19 Every patient with SCD needs a PCMH with the understanding that the location of the PCMH may vary depending on patient preference, patient proximity to providers, and access to hematologists.20,21 Given the shortage in hematologists caring for adults, new care models must be explored. In 2011, the US Department of Health and Human Services designated SCD as a priority area, specifying that action was needed “to increase the availability of medical homes to improve access to quality routine care.”22 A central question on the implementation of PCMHs for individuals with SCD will be how this model of care can be effectively leveraged to improve pain management.
This article provides a framework of pain management within the PCMH model. First, we present an overview of pain and pain management in SCD, gaps in pain management, and current care models used by patients. Second, we present core PCMH concepts and discuss multidisciplinary team–based PCMH care strategies for SCD pain management.
SCD-related pain syndromes
Pain in SCD can be characterized as acute, chronic, neuropathic, or mixed. Acute pain may occur throughout the lifespan, presenting as unpredictable episodes of sharp and/or throbbing sensations with sudden or gradual onset.23 It is mediated by vasoocclusion, which leads to ischemia and end organ tissue damage. Chronic pain is characterized as deep, achy, and persistent in nature, typically lasting 3 or more months in duration.23 Chronic pain may occur secondary to clear pathophysiologic events, including avascular necrosis and leg ulcers, or may be the result of persistent or frequently occurring acute painful episodes that are inadequately treated over time. Investigators postulate that chronic pain may involve a process of central sensitization in which the pain threshold is decreased and hyperalgesia ensues. Neuropathic pain is also a recognized form of pain attributable to SCD. It is characterized by spontaneous and ongoing burning, shooting, or tingling sensations with amplified pain responses after noxious or non-noxious stimuli. It arises as a result of nerve injury or dysfunction.23
Principles of pain management
According to the biopsychosocial model of pain,24 the experience of pain may be modulated by biological response, basic demographics, psychological factors, religious beliefs, culture, family responsibilities, occupation, and perceptions of disease severity. Recognizing the important contribution of these factors enables clinicians to effectively tailor both pharmacologic and nonpharmacologic approaches to pain management. Nonpharmacologic management of pain consists of a broad spectrum of directly applied therapies and coping strategies, including heat or cold packs, self-hypnosis, cognitive behavioral therapy, and guided imagery.23 Because there is some support for the efficacy of these strategies, they offer patients proactive solutions to manage their pain.25,26 Pharmacologic management of SCD pain is composed of 3 major drug classes: non-opioids, opioids, and adjuvants. Non-opioids include acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), topical agents, and corticosteroids. Non-opioids are typically recommended for mild pain. NSAIDs in particular are effective at relieving the inflammatory component of bone pain related to vasoocclusive episodes. Opioid analgesics consist of μ-antagonists, mixed agonist/antagonists, and partial agonists. Opioids are typically used for moderate to severe pain or in situations where NSAIDs are contraindicated. In a subset of patients, opioid therapy can lead to dependence or addiction. However, the percentage of adults with SCD who demonstrate behavior consistent with substance abuse is similar to that seen in the general population.27 Although addiction is a problem for a small subset of the SCD population, a more pervasive concern is undermedication of those truly in pain.28 Adjuvants act on excitatory neurotransmitters, inhibitory neurotransmitters, or neurotransmitters that modulate the pain experience. Classes of psychotropic medications commonly used in pain management consist of antidepressants, antiepileptic drugs, antianxiety agents, stimulants, and tranquilizers.
Persistent gaps in pain management
Over the past several years, the National Heart, Lung and Blood Institute (NHLBI) has outlined a strategic plan to “… identify and understand the relationships of molecular events to pathophysiologic processes involved in vaso-occlusion.”29 NHLBI is collaborating with the National Institute for Neurological Diseases and Stroke (NINDS) to co-fund a request for application entitled “Exploratory Studies in the Neurobiology of Pain in Sickle Cell Disease.” This RFA will support molecular study of pain regulation and dysregulation. NHLBI is also collaborating with the Clinical and Translational Sciences Awards (CTSA) Pain Researchers Interest Group (CPRIG) to design and implement new clinical strategies to manage SCD-related pain. Lastly, the NHLBI will shortly release new evidence-based guidelines for the management of SCD with pain management being a major focus.
Although there is increasing prioritization of molecular and translational research to address SCD-related pain, strategies to improve health care delivery models for pain management are less well articulated. Current literature documents deficiencies in pain management and patient centeredness.30,31 In a recent qualitative study on patient perceptions of primary care, adults with SCD perceived poor pain management, lack of access to outpatient care services, poor communication between health care professionals, and inadequate follow-up as major concerns.31
Variable access to providers and shortages in hematologists in adult practice indicate that new models of care are needed to address the pain management of this now aging population. Currently, adults and children seek care in several settings, with variable comprehensive and coordinated care. A minority of patients with adequate access are seen in comprehensive SCD centers. Patients may have a primary care provider with periodic referral to a hematologist. Other individuals may receive episodic care primarily managed by a hematologist without a primary care provider. Individuals may also have no primary care provider or regular hematologist coordinating care.
The PCMH
The PCMH is a widely endorsed delivery system innovation that aims to redesign primary care as a centerpiece for integrated health care delivery, reduce care fragmentation, and decrease system inefficiencies associated with chronic disease management in the United States. The PCMH model proposes care that is accessible, continuous, patient centered, team based, and comprehensive, all in alignment with the patient's family and community.17 PCMH Joint Principles were approved in 2007 by major primary care professional organizations.32 The model has subsequently gained endorsement by specialty societies, all major national health plans, large employers, and consumer groups. The Sickle Cell Disease Treatment Demonstration Program (SCDTDP), which was created to improve SCD management, also embraces many concepts of the PCMH.33 Although most studies assessing the impact of the PCMH on health outcomes have focused on heterogeneous populations, several have focused on specific chronic conditions.19 Among adults with diabetes, the PCMH has been shown to improve HgbA1C, blood pressure, and lipid control while lowering hospitalizations. Among adults with depression, implementation of a PCMH model has been associated with increased use of antidepressants and psychotherapy, decreased depressive symptoms, and improved quality of life.
Multiple actions at the federal level have increased the potential for application of the PCMH model to individuals with SCD. The Affordable Care Act of 2010 set forth multiple provisions to increase access to primary care services. In 2011, the US Department of Health and Human Services established a Sickle Cell Disease Initiative designating increased access to PCMHs as a priority action item.22 Despite the potential of the PCMH to improve chronic disease management, little is known about the extent to which adults and children with SCD have PCMHs or whether PCMHs can improve SCD-related pain.34 A recent single-institution study assessed experience with PCMH care among children with SCD.35 In this study, only 11% of children met the standards for receiving care in a PCMH. Although > 90% of children had a regular provider, they experienced deficiencies in multiple aspects of care: comprehensive care (67%), family-centered care (59%), and coordinated care (20%). A related study demonstrated that children with SCD who experienced comprehensive care had lower rates of ER encounters and hospitalizations compared with those who did not experience comprehensive care.36
PCMH model for pain management
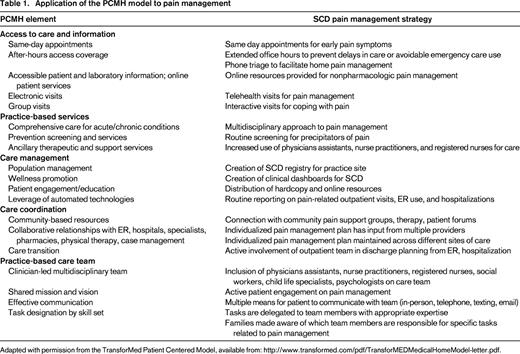
The core elements of integrated health care delivery represented by the PCMH can be modeled to create a system of care to improve pain management among individuals with SCD. Such a system may foster a proactive and preventive approach to pain management rather than one that is episodic and reactive. The PCMH resource organization, TransforMED,37 has developed a detailed model of PCMH implementation.38,39 In Table 1, we have adapted the framework to model SCD pain management. Because multiple models of PCMH implementation exist, the TransforMED framework represents one example of how to integrate care.
Access to care and information
To prevent unnecessary delays in care and avoidable high-acuity health care utilization, patients must have appropriate access to outpatient care. Patient-centered strategies to improve access to care must include same-day appointments and extended office hours. Same-day appointments may expand the options for care when a pain episode begins or decrease the time a patient must manage symptoms without the input of a medical provider. Extended clinical hours offer patients the opportunity to minimize the disruption to work and family schedules for uncomplicated pain episodes. New models of telecommunication are increasingly being incorporated into clinical care to increase access and convenience. These enhanced modes of communication may facilitate real-time management of pain episodes at home and may obviate the need to seek care in primary care or hematology practice or ER. Modes of communication may include 2-way video, e-mail, and text messaging. Preliminary studies show that such modes of communication have the potential to prevent delays in seeking treatment for SCD-related pain among children with SCD.40,41 Group visits may also offer news ways to share information among patients with chronic pain, but little is known about how such models would work with SCD.
Practice-based services
Comprehensive care necessitates a multidisciplinary approach with inputs from a variety of medical providers, including physicians, physician assistants, nurse practitioners, and registered nurses. Nonphysician providers may serve as the first line of proactive pain management through outpatient visits and telephone communication. They may encourage and teach self-management skills, including nonpharmacologic methods of pain reduction, stress management, and coping. They may also aid patients in identifying precipitators of pain. In the PCMH model, nonphysicians in consultation with the physician may take the responsibility for managing the majority of patients with uncomplicated pain, whereas physicians may provide more specialized care for patients with more severe or refractory pain.
Care management
Population management may require more formalization of how patients with SCD are identified and tracked within a practice. Patient registries at the practice level may offer an opportunity to assess pain management practices, track patients' self-management goals, determine the most effective therapies for treatment, and identify areas for practice improvement.42 They may also serve as central repositories for patient pain plans that can be modified by the care team. Clinical dashboards are computerized visual tools that allow practitioners to monitor real-time, clinically relevant information at the group or individual provider level. Dashboards provide a mechanism to develop internal reports and analyze day-to-day quality of care and patient adherence to care.43 A provider may query what percentage of their panel of patients with SCD have active prescriptions for pain medications, a formal pain management plan, or indications for hydroxyurea therapy. Population management may also involve more active distribution of educational materials on pain management to assist patients and family members.
Care coordination
Connection with community-based resources represents a key aspect of care coordination. With case managers, patient navigators, or social workers, patients can be connected with resources in the community, such as pain support groups, online patient forums, and alternative therapies for pain management. More collaborative relationships between the patient's PCMH, ER, and hospitals may facilitate more consistent pain management strategies across sites and proactive discharge planning for pain episodes with adequate and timely follow-up. Such collaborative efforts may prevent rehospitalization.4 Coordination may also involve proactive referrals to other specialists involved in care. Prior work has demonstrated that low-income African-American adults with SCD may be at increased risk for dental caries, which may be a precursor to oral pain episodes.44
Practice-based care team
As already described, a clinician-led multidisciplinary team will be essential to practice management. Team members may include physician assistants, nurse practitioners, and registered nurses, social workers, health educators, child life specialists, and psychologists who take on different responsibilities with respect to pain management. For example, social workers may take the leading role in connecting patients to community resources, whereas psychologists may engage patients regarding stress management and coping strategies. Many patients have nonmedical issues (eg, inadequate insurance, food insecurity, poor housing) that impede their ability to effectively self-manage their pain. Social workers and patient navigators may help patients overcome challenges that directly affect pain management. Such divisions of labor may increase the efficiency of the PCMH. Team members may communicate with patients through in-person visits, telephone, texting, and e-mail. However, clear delineations of roles and responsibilities are needed so that patients/families know who is responsible for different aspects of care. Patients and family members may take active roles in developing and modifying pain management plans in direct consultation with their care team.
Quality and safety
To provide evidence-based best practices for SCD pain management, a PCMH may use several strategies. Electronic prompts and clinical decision aids may help ensure that providers manage pain in a manner consistent with practice guidelines.45 Electronic prescribing can effectively monitor medication use, adherence, drug interactions, and side effects, in addition to meeting a key requirement of meaningful use of electronic health records as part of the American Recovery and Reinvestment Act of 2009.46 Patient satisfaction with pain management may be measured through periodic surveys in various care settings.
Health information technology
Health information technology (HIT) is increasingly used to improve efficiency and quality in diverse medical settings. Patient kiosks are interactive computer stations designed for self-service tasks typically located in practice waiting rooms.47 They can be used for patient data entry that will go directly into the medical record, for dissemination of health information, for assessment of patient satisfaction after visits, or for interventions. Interactive web-based technologies are currently being tested in pediatric SCD care to assess medication adherence, clinic attendance, and clinical outcomes.41 In addition to the use of HIT by patients and families, hospital systems and care teams are increasingly using HIT to document clinical care and to communicate across care settings. Strategies will need to be developed to ensure that care providers and others involved with the patient's care have the information they need at the time they need it. A priority for PCMH will be integrating electronic medical records across clinical settings so that pain management can be more consistent.
Practice management
Practice management in the PCMH will be based on comprehensive and coordinated care for pain. This may require practice transformation and redesign with changes in personnel management. Given such a multidisciplinary approach, coding and billing should be prioritized to ensure that the practice is adequately reimbursed for services rendered. Practices must explore PCMH payment structures that reimburse for care coordination and registry-related tasks associated with pain management. Such payment structures may justify practice investment in PCMH care for SCD pain. Practices may also experiment with incentives for performance to improve the quality of pain management.
Options for the SCD pain management PCMH
High-quality pain management for individuals with SCD necessitates that they receive both comprehensive primary care and specialized services. However, only a minority of adults and children with SCD receive specialist care due to issues of access or inadequate coverage of services. Therefore, the PCMH model for SCD pain management may require flexibility in how the model is applied and who provides the medical home.
PCMH within hematology
It is possible that hematologists may take on the role of providing a PCMH. First, a patient may be cared for by a hematologist over a long period of time who understands all aspects of their pain management. Second, the available literature suggests that specialty physicians already address the primary care needs of patients, including care coordination.48 Third, it may not be feasible to reallocate the clinical duties of a hematologist to primary care. One study demonstrated that reallocating half of specialty return care to PCMHs would require every adult primary care physician to work an additional 3 weeks each year, “a time commitment that is equivalent to expanding the current primary care workforce by over 300 physicians.”49
Realignment of hematology care in the medical neighborhood
Given the focus on enhanced primary care in the PCMH model, the role of hematology specialty care in pain management may change. Policy makers increasingly advocate that primary care providers and specialists collaborate to create “medical neighborhoods” based on shared information systems for care coordination, improved measures of performance, and collective accountability for improving quality and reducing costs.17,49 In this new model of collaboration, clinical responsibilities may shift so that routine follow-up typically conducted by hematologists may be reallocated to primary care providers within a PCMH practice. Hematologists and pain specialists may provide care to patients who require more complex or specialized management.
There are several potential advantages to creating PCMH models for SCD pain located in primary care. First, the primary care provider is more likely to be located within the patient's community and therefore will be able to more effectively coordinate with school systems, community organizations, and local government agencies. Second, the primary care physician is more likely to be familiar with the patient's family and the competing needs of other family members. With more specific knowledge of family stressors and priorities, the primary care physician can effectively incorporate this information into pain management. Third, there is evidence that primary care physicians can provide more coordinated and less expensive care relative to specialists for adults with chronic disease.49 For this to be a successful model, primary care physicians will require additional training in SCD pain management.
Collaborative PCMH between hematology and primary care
Lastly, it may be that the PCMH for SCD pain management is achieved through active collaboration between the hematologist and other providers. In this model, continuous communication and information sharing between the hematologist and other clinicians is key. The hematologist takes primary responsibility for pain management, but works collaboratively with the primary care provider to ensure that the plan of care for pain is well communicated and implemented across sites. The resources of hematology and primary care may be combined to create a PCMH for pain management. For this model to work, patients and families must have clear understanding of the responsibilities for which specific providers are accountable.
Conclusion
Given the current landscape of national health care priorities, further efforts are warranted to improve care models for SCD pain management so that patient-centered, cost-effective structures are developed and sustained over time. The PCMH comprises several elements that have the potential to improve pain management for individuals with SCD. The challenge to implementation of a PCMH for SCD pain management will be applying this model to a small population of affected individuals relative to the general population. Future research should assess the potential benefits of the PCMH for SCD pain management and determine whether large-scale implementation is warranted.
Acknowledgments
This work was supported by the National Institutes of Health (grant 1K23 HL105568 to J.L.R.).
Disclosures
Conflict-of-interest disclosure: The authors declare no competing financial interests. Off-label drug use: None disclosed.
Correspondence
Jean L. Raphael, MD, MPH, Texas Children's Hospital, 6701 Fannin Street, Suite 1540.00, Houston, TX 77030; Phone: 832-822-1791; Fax: 832-825-3435; e-mail: raphael@bcm.edu.