Abstract
The antiphospholipid syndrome (APS) is defined by venous or arterial thrombosis and/or pregnancy morbidity in patients with persistent presence of antiphospholipid antibodies (aPLs). Catastrophic APS is the most severe form of APS, which is associated with rapid development of microvascular thrombosis resulting in multiorgan failure in patients with aPLs. Patients with APS and catastrophic APS are recognized to have a high risk of recurrent thrombosis that can occur despite anticoagulant therapy. Although antithrombotic therapy remains the mainstay of treatment, bleeding manifestations can complicate management and contribute to increased morbidity. Patients with persistently elevated aPL levels, particularly those who exhibit positive testing for lupus anticoagulant, anticardiolipin antibodies, and anti-β2GPI antibodies (triple positivity), appear to be at increased risk for thrombosis and pregnancy complications, whereas isolated positivity for aPLs appears to be associated with low risk. Recognizing that patients with APS have different thrombotic risk profiles may assist clinicians in assessing the risks and benefits of anticoagulation. The optimal type, intensity, and duration of anticoagulation in the treatment of APS remain controversial, particularly for arterial thrombosis and recurrent thrombosis. Future studies that delineate thrombotic risk in APS and evaluate current and novel anticoagulants as well as nonanticoagulant therapies are required.
Introduction
The antiphospholipid syndrome (APS) is a prothrombotic condition characterized by venous or arterial thrombosis and/or pregnancy morbidity in the presence of persistent laboratory evidence of antiphospholipid antibodies (aPLs). aPLs are autoantibodies that target phospholipid-bound proteins, notably β2-glycoprotein I (β2GPI). Although the presence of these antibodies is the defining feature of this syndrome, the mechanism by which aPLs result in a hypercoagulable state remains incompletely understood. APS is recognized to be a syndrome prone to recurrent thrombosis when anticoagulants are discontinued, although some patients develop recurrent events despite standard anticoagulant therapy. A subset of patients with APS have a severe variant known as catastrophic antiphospholipid syndrome (CAPS), which is characterized by thrombosis affecting multiple organs in a short period of time and histopathologic evidence of small vessel occlusion. Management of the thrombotic complications in these patients can be extremely challenging due to competing risks of bleeding and thrombosis. Understanding the thrombotic risk in this heterogeneous condition can assist clinicians in determining the optimal antithrombotic treatment.
Recognizing APS
APS is one of the few clinical conditions in which patients can present with both venous and arterial thrombosis, with deep vein thrombosis of the lower extremity the most common presentation and stroke the most common arterial manifestation.1 Recurrent pregnancy loss is the most common pregnancy-related complication. Other clinical characteristics aside from thrombosis and pregnancy morbidity may be seen in patients with APS, including thrombocytopenia, hemolytic anemia, livedo reticularis, valvular heart disease, and neurologic findings such as cognitive deficits and white matter lesions.2 In patients presenting with thrombosis or pregnancy complications, these findings may alert clinicians to consider the diagnosis of APS. Despite these varied clinical manifestations, the defining feature of this syndrome is the persistent presence of aPLs. These heterogeneous autoantibodies bind to phospholipid-binding proteins, although binding to β2GPI appears to identify the pathologic subgroup of antibodies that result in thrombosis and pregnancy complications.3-5
Diagnosing APS
In 1999, international experts developed consensus criteria on the clinical and laboratory criteria for “definite APS” that became known as the Sapporo Criteria. These criteria were subsequently updated in 2006 at a meeting in Sydney, Australia and are now referred to as the updated Sapporo or Sydney Criteria (Table 1).2 The clinical criteria include objectively confirmed venous, arterial or small vessel thrombosis, or pregnancy complications that may be attributed to placental insufficiency, including pregnancy loss or premature birth. The laboratory criteria require that a positive laboratory test for aPLs be found on 2 or more occasions at least 12 weeks apart. The aPLs recognized in the international criteria include lupus anticoagulant (LA) detected according to guidelines published by the International Society on Thrombosis and Haemostasis (ISTH),6 anticardiolipin (aCL) antibody (IgG or IgM) exceeding 40 IgG or IgM phospholipid units, or anti-β2GPI antibody (IgG or IgM) at titers exceeding the 99th percentile. Although the laboratory criteria for measuring aPL is beyond the scope of this article, it is notable that false positive LA results can occur if testing is performed while patients are receiving anticoagulants or possibly in the setting of a factor deficiency. Infections and medications can also induce transient aPL but these generally disappear on repeat testing or drug discontinuation, emphasizing the importance of repeated aPL measurements in the diagnosis. These 3 laboratory tests are currently the key diagnostic tests used in the assessment of APS. These assays measure antibodies that are heterogeneous, may have different antigenic targets, and may be associated with different clinical phenotypes. Nonetheless, these criteria have been used to standardize patients entered into clinical studies evaluating aPLs and APS. Patients who have aPLs not currently recognized in the diagnostic criteria (eg, antiprothrombin antibodies, IgA aCL or anti-β2GPI antibodies) or who have clinical manifestations other than thrombosis or pregnancy morbidity are not formally recognized as having APS at present, but diagnostic criteria continue to evolve. Testing for these non-criteria aPL is not currently recommended in routine clinical practice because of a lack of standardization of the assays and the need for prospective studies to assess whether these antibodies provide additional information to the current testing.
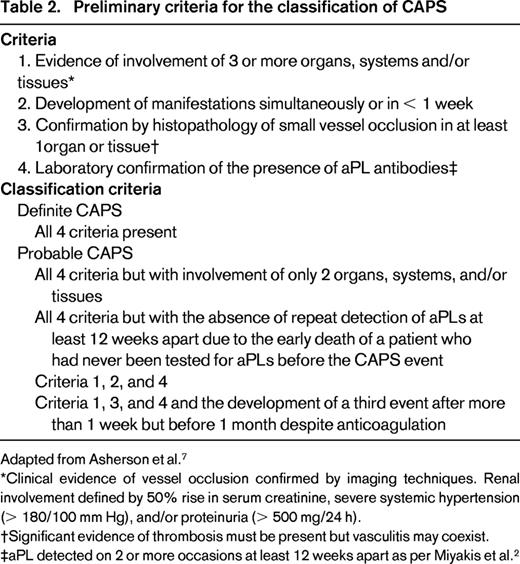
Diagnosing CAPS
The term “CAPS” was proposed in 1992 following reports of patients with an accelerated form of APS who presented with coagulopathy, ischemic necrosis of the extremities, and presence of aPLs. Proposed diagnostic and classification criteria for CAPS were published in 2003 (Table 2)7 and subsequently validated. Definite CAPS is classified with evidence of multisystem (3 or more) organ involvement over 7 days with histopathologic evidence of small vessel occlusion and laboratory evidence of aPLs. CAPS develops in < 1% of patients with APS,1 but is associated with a 30% mortality rate in the absence of treatment. Almost half of the patients with CAPS do not have a prior diagnosis of APS or underlying rheumatologic condition.8 An international registry of patients with CAPS known as the CAPS Registry was initiated in 2000 by the European Forum on Antiphospholipid Antibodies and contains clinical, laboratory, and treatment data on > 350 patients (http://www.med.ub.es/MIMMUN/FORUM/CAPS.HTM).9
The diagnosis of CAPS can be complicated by the rapidity with which patients develop organ failure, the inability to rule out other conditions that may present with similar findings, and difficulties in interpreting aPL testing. Positive aCL testing can result from infections that frequently coexist or precipitate CAPS and LA testing can be affected by anticoagulant therapy that is empirically initiated in these patients. This issue was addressed by a Catastrophic APS Task Force, which proposed updated diagnostic algorithms to assist clinicians manage patients with suspected CAPS.10 The main considerations in these algorithms include a prior history of APS or persistent aPL positivity, the number of organ thromboses developing in < 1 week, histopathologic findings of microthrombosis on biopsy, and alternate diagnoses for the thrombotic findings.
Although APS and CAPS share similar features, the CAPS registry has highlighted unique aspects to the latter condition.9 In > 50% of patients with CAPS, a precipitating factor can be identified, with infection and surgery being the most common. The thrombotic manifestations of CAPS differ in their distribution compared with patients with APS. In contrast to APS, in which involvement of the deep veins of the extremities and pulmonary embolism predominate, patients with CAPS manifest with small vessel occlusion and most commonly present with abdominal pain and intraabdominal thrombosis (kidneys, adrenal glands, spleen, pancreas, and mesentery). The multiorgan involvement of CAPS typically manifests with renal failure (present in 71% of patients), respiratory failure (64%), and central nervous system involvement (62%). Another important feature of CAPS is the systemic inflammatory response syndrome, which is triggered in response to the tissue necrosis from underlying small vessel occlusion. The treatment of CAPS is therefore based on addressing thrombosis as well as the inflammatory response.
aPL profile and thrombotic risk
In contrast to the original Sapporo Criteria, the Sydney Criteria strongly advised that patients with APS be classified into those with positivity for one aPL (LA only, aCL only, or anti-β2GPI only) and those with > 1 laboratory criterion present in any combination.2 This was based on the concept that positivity for one aPL carries a lower risk of thrombosis or pregnancy complications compared with multiple (particularly triple) positivity.11 Evaluation of patients using the aPL profile of LA, aCL, and anti-β2GPI, rather than an individual test, may consequently be useful in assessing thrombotic risk. An understanding of the antigenic target of pathologic aPLs may explain these laboratory findings. Autoantibodies directed against β2GPI were identified in 1990 as an important subgroup of antibodies in patients with APS.3-5 Subsequently, it was elucidated that aCLs associated with thrombosis appear to be autoantibodies recognizing β2GPI, which has a high affinity for cardiolipin. There appear to be 2 types of aCL: anti-β2GPI–dependent aCLs, which are associated with thrombosis and pregnancy complications, and anti-β2GPI–independent aCL antibodies, which appear to be associated with infection. The latter antibodies are generally transient and are not associated with thrombosis.12 Many aCL kits include a source of β2GPI. Similarly, autoantibodies against β2GPI were subsequently identified to have LA activity.13,14 LA can be classified into LA that binds β2GPI and is associated with thrombosis15 and LA that binds prothrombin, but these are currently not available outside of a research setting.16 Distinguishing anti-β2GPI–dependent and anti-β2GPI–independent aCLs and LA may have important clinical implications, allowing clinicians to distinguish pathologic antibodies associated with thrombosis from nonpathologic antibodies.
The laboratory assays measuring LA, aCLs, and anti-β2GPI antibodies thus appear to detect overlapping, but different, populations of autoantibodies, which may account for the varied clinical manifestations of APS. Assays for LA appear to detect the pathologic aPLs better than aCL or anti-β2GPI assays.17,18 In addition to distinguishing if aPLs bind β2GPI, there appear to be different subpopulations of anti-β2GPI antibodies that recognize different epitopes on β2GPI. Antibodies that bind domain I of β2GPI appear to correlate with thrombosis and pregnancy complications compared with antibodies that bind other domains.19-21 Autoantibodies that bind domain I appear to result in triple positivity in the laboratory assays, identifying patients who are at highest risk of thrombotic complications. Other factors that predict thrombosis appear to be persistence of aPLs and a high aPL titer, which resulted in the inclusion of these criteria in the Sydney Criteria.2
Risk of thrombosis with positive testing for 1 aPL
No association was found between thrombosis and aCL in a systematic review,17 and this was subsequently confirmed in prospective studies.18 Even when assessed at moderate to high titer (aCL > 40 IgG or IgM phospholipid units), the presence of aCL alone was not associated with thrombosis,22 although pregnancy morbidity was observed.23 Similarly, there appears to be no association between thrombosis or pregnancy loss in patients only positive for anti-β2GPI.24 In contrast, LA appears to be more strongly associated with thrombosis and pregnancy complications,17 although there are conflicting data that suggest isolated LA may not be associated with elevated thrombotic risk.22,25 The ELISA assays for aCLs and anti-β2GPI have been plagued by poor standardization and unreliable results.26 In contrast, assays for LA have better standardization and good correlation with the clinical manifestations of APS.17
Risk of thrombosis with positive testing for 2 or more aPLs
Analysis of patient samples drawn at enrollment from the Warfarin in Antiphospholipid syndrome (WAPS) study found that patients with positive LA testing and positive anti-β2GPI were at increased risk for total thrombosis (odds ratio [OR] = 4.1, 95% confidence interval [CI], 1.3-13.5) and arterial thrombosis (OR = 2.5, 95% CI, 1.0-6.0).27 Patients with 3 positive aPL tests have been shown in retrospective and prospective studies to be at increased risk of thrombosis or pregnancy morbidity, with ORs for thrombosis ranging from ∼ 5 to 33.11,22,28,29 In a retrospective analysis of 160 patients with triple-positive aPL testing, a cumulative incidence of thrombosis of 12.2%, 26.1%, and 44.2% was observed after 1, 5, and 10 years of follow-up, respectively.11 In a prospective study of 194 patients with persistent LA and/or aCL, the highest incidence of thrombosis was found in patients with persistent LA who were also positive for anti-β2GPI and anti-prothrombin antibodies measured at 8.4% per patient-year.29 Further study is required to determine whether aPL profiles will affect APS classification and influence clinical decision making. aPL profiles and their effect on thrombotic risk have not been specifically studied in patients with CAPS or in the CAPS registry.
Additional considerations
In addition to the aPL profile of patients, other considerations that influence thrombotic risk include the presence of other thrombotic risk factors (eg, inherited thrombophilia, pregnancy, immobilization, surgery) and the presence of systemic lupus erythematosus (SLE). Patients with SLE have an increased risk of thrombosis compared with the general population, and those who also have isolated but persistently positive aPL appear to be at further risk.30
Antithrombotic treatment of APS
The high incidence of recurrent thromboembolism that characterizes this condition has resulted in antithrombotic therapy being the mainstay of treatment for patients with APS. However, the optimal antithrombotic agent, intensity of anticoagulation, and duration of treatment remain controversial, particularly for nonvenous thrombotic events. Further complicating treatment in patients with APS is the balance between thrombosis and hemorrhage, because many of these patients have thrombocytopenia, coagulopathy, and other comorbidities that contribute to increased bleeding risks.31
A systematic review of major bleeding rates in patients with APS estimated the frequency to be between 0.57% and 10% per year.32 In an analysis of 66 patients with APS receiving oral anticoagulation with a target international normalized ratio (INR) of 3.5, major bleeding occurred in 6 cases per 100 patient-years (95% CI, 1.6-15.0) and intracranial hemorrhage was 1.5 per 100 patient-years (95% CI, 0.04-8.4).33
Patients with aPLs and first venous thrombosis
There have been 2 randomized trials comparing standard-intensity (INR 2.0-3.0) versus high-intensity (INR 3.1-4.0) warfarin in patients with APS meeting the current criteria.34,35 The majority of the patients in these studies had a first episode venous thrombosis, and the study results have since been interpreted as being applicable to this specific subset of patients with APS. These studies found no difference in the rates of recurrent thrombosis or major bleeding, supporting the use of standard-intensity anticoagulation.
The optimal duration of anticoagulation in these patients is somewhat controversial, but based on observational studies demonstrating that patients with aPLs and a first episode of venous thrombosis have a high risk of recurrence if anticoagulants are discontinued,36 expert recommendations suggest consideration of long-term therapy.37 However, this recommendation must consider an individual patient's risk factors and preferences. Patients who are poor candidates for anticoagulation due to recurrent bleeding complications or noncompliance with therapy may not benefit from long-term anticoagulation. Further, patients whose initial event occurred in the context of a reversible risk factor and in whom subsequent aPL testing becomes negative may have a low risk of recurrence and may be considered candidates for anticoagulant discontinuation.37
Patients with aPLs and arterial thromboembolism
Recurrent arterial thrombosis appears to be more common than venous recurrence in patients with APS.31 The optimal antithrombotic regimen in these patients is controversial. The Warfarin versus Aspirin Recurrent Stroke Study (WARSS) compared warfarin (target INR 1.4-2.8) with aspirin 325 mg daily for secondary prevention of ischemic stroke. A subgroup analysis of this study, the Antiphospholipid Antibodies and Stroke Study (APASS)38 found that aPL positivity at presentation was not predictive of recurrent stroke and no difference between warfarin and aspirin for secondary stroke prevention was observed. Patients in this study did not meet the current definition of APS, because only one measurement of LA or aCL was measured at baseline and low-titer aCL patients were included. Many of these patients were older with cardiovascular risk factors and may be viewed as a different patient population compared with APS patients, who are typically younger with few cardiovascular risk factors. This study is interpreted by many experts as having enrolled patients with stroke who had an aPL, but many patients likely did not have APS. This has resulted in uncertainty as to whether the results can be generalized to patients with APS and ischemic stroke.
A systematic review of mainly retrospective studies found that patients with definite APS and arterial events had higher rates of recurrence despite anticoagulation compared with patients with venous events, although a minority of events (3.8%) occurred at INR levels > 3.0.32 These investigators recommended high-intensity warfarin (INR > 3.0) for patients with APS and arterial thrombosis, although this has never been specifically evaluated in a randomized trial. Patients with arterial events comprised almost 25% of the patients in the aforementioned trials, which enrolled mainly patients with venous events34,35 and supported standard-intensity anticoagulation (INR 2.0-3.0). However, definitive conclusions cannot be drawn due to the limited numbers. A small randomized trial compared aspirin versus aspirin and warfarin in patients with APS for secondary stroke prevention and found lower rates of recurrent stroke in patients receiving combination therapy.39 An international panel of experts convened at the 13th International Congress on Antiphospholipid Antibodies recommended that patients with definite APS and arterial thrombosis receive warfarin (INR > 3.0) or combination aspirin (100 mg daily) and warfarin (INR 2.0-3.0), but there was a lack of consensus on this recommendation.37 In general, patients with arterial thrombosis and aPLs receive indefinite duration therapy.
Patients with recurrent thrombosis while receiving anticoagulation
There have been no studies evaluating patients with APS who have recurrent arterial or venous thrombosis despite antithrombotic therapy. Recurrence must be carefully established, and patients with a subtherapeutic INR, recurrence in the setting of other thrombotic risk factors and postphlebitic syndrome must be excluded before changing therapy. Treatment options range from increasing the therapeutic INR range to a higher intensity (eg, from target INR of 2.0-3.0 to 2.5-3.5 up to 4.0) to the addition of antiplatelet therapy or changing the type of anticoagulation (eg, from warfarin to heparin). Oral factor Xa inhibitors and direct thrombin inhibitors have not been specifically studied in these patients to date.
Non-anticoagulant treatment of APS
Although anticoagulation is the mainstay of APS treatment, non-anticoagulant treatments have been evaluated. In patients with SLE, hydroxychloroquine has been shown to reduce the risk of an initial thrombotic event in patients with or without aPL40 and is frequently used in combination with anticoagulant therapy in these patients. The use of hydroxychloroquine in patients without SLE is uncertain, although hydroxychloroquine has been shown to protect the annexin A5 anticoagulant shield from aPL disruption.41
Statins have anti-inflammatory, anticoagulant, and immunoregulatory effects and may potentially have a role as a novel treatment option for patients with APS. In a small study of 41 aPL-positive patients who had inflammatory and prothrombotic markers measured at baseline and after treatment with fluvastatin 40 mg daily for 3 months, 50% of the measured biomarkers were significantly reduced compared with control subjects.42 Rituximab has been used in patients with APS who have refractory disease, but is not currently approved for this indication. Rituximab was found in a small phase 2 pilot study of 19 patients to reduce some of the non-criteria manifestations of APS.43
Treatment of CAPS
Early recognition and aggressive initiation of anticoagulant therapy is critically important in the treatment of CAPS. A treatment algorithm has been proposed by the CAPS Registry Project Group.7 The quality of evidence supporting these therapies is weak, because these recommendations have largely been based on observational data from the CAPS registry. However, since the introduction of combination therapy with anticoagulants, corticosteroids, and plasma exchange, the mortality rate for patients with CAPS has decreased from 53% to 33% in patients diagnosed before 2000 compared with those diagnosed between 2001 and 2005.44
The mainstay of CAPS treatment is anticoagulant therapy, most commonly with heparin. Decreased mortality was observed in patients who received anticoagulation compared with patients who were not anticoagulated (37% vs 78%, P < .0001).45 There was no difference between unfractionated and low-molecular-weight heparin and most patients in the registry were subsequently anticoagulated with vitamin K antagonists. Corticosteroids are also used as a first-line therapy in CAPS. Expert recommendations suggest methylprednisolone 1000 mg daily for 3 days, but longer duration of treatment may be required based on patient response.46 Use of corticosteroid therapy alone did not improve mortality in the CAPS registry, but is empirically used based on the presumed pathophysiology of CAPS. Plasma exchange (PLEX) using fresh frozen plasma has been shown in observational studies and in the CAPS registry to improve mortality.43 Expert recommendations suggest initiating PLEX in patients with CAPS who do not demonstrate a response to anticoagulation and corticosteroids using plasma volumes of 2 to 3 L exchanged daily for 3 to 5 days.46 IVIg administered alone did not appear to improve mortality, but may be of benefit in patients with immune-mediated thrombocytopenia when used in combination with PLEX. In these situations, IVIg is administered after completion of PLEX. The dose of IVIg typically used has been 0.4 g/kg/d for 4 to 5 days.46 Off-label treatments, including rituximab, defibrotide, and eculizumab, have all been reportedly used for CAPS, but discussion of these agents is beyond the scope of this article.47
Conclusions
APS is a prothrombotic disorder with various manifestations, most commonly venous and arterial thromboembolism and recurrent pregnancy loss. The varying clinical phenotype and heterogeneity in the antibodies that are central to the diagnosis of APS have resulted in challenges in studying this disease and controversy in optimal treatments. Patients with persistently positive aPL, particularly those who exhibit triple positivity, are at higher risk for thrombosis, as are patients with arterial thrombosis and those with recurrent thrombosis despite antithrombotic therapy. Understanding the thrombotic risk profile in patients with APS can assist in determining the optimal type and duration of antithrombotic therapy. Patients with CAPS have an extremely prothrombotic phenotype and require antithrombotic therapy and immunosuppression to address the inflammatory response that characterizes this condition. Future studies that refine our understanding of this condition, better characterize thrombotic risk, and evaluate current and novel anticoagulant and non-anticoagulant therapies are required and will need to be individualized in the context of patient-specific risk factors and preferences.
Disclosures
Conflict-of-interest disclosure: The author has received research funding from Leo Pharma, has consulted for Pfizer, and has received honoraria from Pfizer and Leo Pharma. Off-label drug use: None disclosed.
Correspondence
Wendy Lim, MD, MSc, FRCPC, St Joseph's Healthcare Hamilton, 50 Charlton Avenue East, Room L208, Hamilton, Ontario L8N 4A6, Canada; Phone: 905-521-6024; Fax: 905-540-6568; e-mail: limwp@mcmaster.ca.