Abstract
Chronic lymphocytic leukemia (CLL) and lymphoplasmacytic lymphoma (LPL) are malignancies of mature B cells. In LPL, mutations of the adaptor protein MYD88 (L265P) in the Toll-like receptor pathway have been recognized recently as being a hallmark of the disease and indicate a dependence of the tumor on this pathway. In CLL, functional studies have implicated BCR activation in the tissue microenvironment as a pivotal pathway in the pathogenesis. Bruton's tyrosine kinase (BTK) and the PI3Kδ isoform are essential for BCR signaling and also seem to be required for signal transduction in LPL cells, even if the role of BCR signaling in this disease remains less well defined. Ibrutinib, a covalent inhibitor of BTK approved by the Food and Drug Administration as a second-line treatment for CLL, and idelalisib, a selective inhibitor of PI3Kδ, achieve excellent clinical responses in both diseases irrespective of classic markers indicating high-risk disease. Several additional inhibitors targeting BTK and PI3Kδ, as well as the spleen tyrosine kinase, have entered clinical trials. This review discusses the biologic basis for kinase inhibitors as targeted therapy for CLL and LPL and summarizes the clinical experience with these agents.
Learning Objectives
Gain an overview of the role of BCR signaling in the pathogenesis and treatment of CLL and LPL
Be able to identify kinases that can be targeted therapeutically in CLL and LPL
Understand differences in clinical response and side effect profiles between kinase inhibitors and standard chemoimmunotherapy
Be able to discuss the pros and cons of targeted treatment with kinase inhibitors
Introduction
Chronic lymphocytic leukemia (CLL) is characterized by the accumulation of mature monoclonal B cells in the blood, bone marrow (BM), lymph nodes, and spleen. The diagnosis of CLL requires the presence of ≥5000 tumor cells/μL of blood with a characteristic immunophenotype (CD19+, CD5+, CD23+, weak CD20 expression).1 Small lymphocytic lymphoma (SLL) shares the biological characteristics of CLL, but is distinguished by having <5000 tumor cells/μL of blood in the presence of pathologic lymphadenopathy, splenomegaly, or BM disease. The standard of care for CLL is watchful waiting of asymptomatic patients; treatment is reserved for patients having symptomatic disease or compromised BM function.2 This approach is guided by the absence of curative treatments (with the exception of allogeneic stem cell transplantation), clinical trials showing no benefit for early treatment in asymptomatic patients, and the relatively long and heterogeneous natural history of the disease. Although the median survival of all patients in a large referral center was 11 years,3 it can be much shorter for patients in high-risk disease groups; on the other hand, patients with indolent CLL can have a life expectancy comparable to age-matched controls.4,5
The combination of chemotherapy with anti-CD20 monoclonal antibody (mAb), referred to as chemoimmunotherapy, was shown to be superior to chemotherapy alone and has become the standard first-line treatment for CLL.6-8 However, the majority of patients will relapse within years of first treatment. Median progression-free survival (PFS) after first-line chemoimmunotherapy can be <2 years in patients with adverse cytogenetic markers, in particular in those with deletion of chromosome 17p (del17p) or in those carrying somatic mutations in TP53, NOTCH1, or SF3B1.9 Clonal evolution and the selective pressure exerted by treatment can promote the outgrowth of cells carrying additional genetic lesions that confer treatment resistance. For example, del17p is present in <10% of patients at the time of first-line therapy, but in up to 1/3 of patients with relapsed disease. Identifying treatment options for patients with relapsed/refractory disease and for those with del17p has been and remains a major need.
Lymphoplasmacytic lymphoma (LPL) is a malignancy of mature B cells residing in BM and lymph nodes that secrete immunoglobulin, mostly of the IgM type.10 Accumulation of large amounts of clonal IgM, referred to as Waldenstrom's macroglobulinemia, can lead to hyperviscosity syndrome and neuropathy. Other common disease manifestations include cytopenias and constitutional symptoms. In many regards, LPL is an intermediary between CLL and multiple myeloma and treatment often consists of drugs used in either of the other diseases, including nucleoside analogs, anti-CD20 mAb, and proteasome inhibitors.10
The BCR is a master regulator of B cells that promotes their development, survival, proliferation, functional differentiation, and migration. Expression of a functional BCR is required for the survival of all B cells past the earliest development stages. PI3Kδ, spleen tyrosine kinases (SYK), and Bruton's tyrosine kinase (BTK) are essential for BCR signal transduction, and their knockout in mouse models leads to impaired antigen-driven maturation and expansion of B cells. Over the years, an increasing number of B-cell malignancies were recognized to depend on BCR signaling for proliferation and/or survival.11,12 This concept, although in many cases shown or at least supported by genetic and biologic studies, is emphasized by the clinical success of kinase inhibitors that block BCR signaling in a variety of B-cell malignancies. Here, I briefly review the BCR signaling pathway and its role in CLL, summarize the clinical experience with these targeted agents, and provide an outlook on their possible future role in the therapeutic approach to CLL and LPL.
BCR and Toll-like receptor (TLR) signaling in CLL and LPL
Genetic evidence for a role of antigen selection
A role for antigen signaling in the pathogenesis of CLL is indicated by observations that many CLL cells use a restricted repertoire of immunoglobulin heavy chain variable (IGHV) region genes, which encode the antigen-binding domains of the BCR.13,14 Naive B cells acquire these IGHV mutations after antigen biding as part of a regulated maturation process in the germinal center of the lymph node. The presence or absence of somatic mutations in the clonal IGHV gene distinguishes 2 major CLL subtypes; IGHV mutated (M-CLL) and IGHV unmutated (U-CLL, which has >98% sequence homology to the germline IGHV).1 M-CLL cells appear to be “anergic,” that is, in a state of hyporesponsiveness to BCR activation that can result from frequent BCR stimulation.15 In contrast, many U-CLL clones have BCR structures found in polyreactive B cells that weakly bind many different antigens.16,17 Specific antigens may include microbial structures, molecules expressed on dying cells, or classic autoantigens.18 In addition, it was shown that the BCR of many CLL cells recognizes an epitope that is part of the CLL BCR itself, possibly contributing to autostimulation on a single-cell level.19 The observation that U-CLL is a more rapidly progressive disease with inferior survival compared with M-CLL indicates that the degree of BCR activation and/or the type of antigen may be important. LPL cells derive from a postgerminal center B cell and typically express mutated IGHV genes.
BCR signaling in CLL
Comparative analysis of CLL cells isolated from the blood and lymph nodes provided direct evidence for ongoing antigen-dependent signaling through the BCR in vivo and suggested that the lymph node may be the primary site of BCR activation.20 Therefore, active antigenic signaling continues throughout the disease course of CLL. This conclusion is also supported by the observations of a reversible down-modulation of surface IgM expression on CLL cells and the anergic state of some CLL cells.15,21 BCR signaling is likely a key driver of CLL proliferation; in vitro BCR activation supports CLL cell survival and proliferation22-26 and a strong cellular response to BCR activation correlates with a more aggressive disease course.20,27,28 Consistent with these in vitro data, the degree of BCR activation in CLL cells in vivo correlates with increased tumor proliferation and shorter time to progression.20
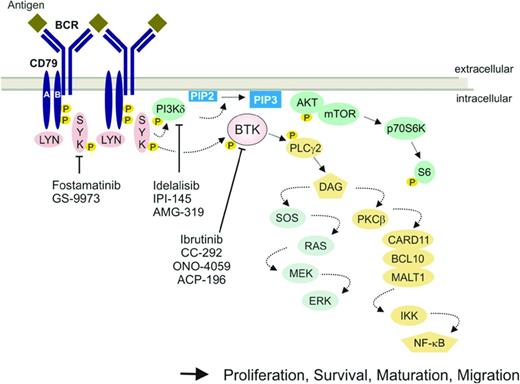
The transduction of signals from the BCR involves a network of kinases and adaptor molecules that connect antigen stimulation to intracellular responses (Figure 1).29 In vivo, additional elements present in the tissue microenvironment cooperate with the BCR and may influence the cellular response. The term “microenvironment” collectively describes cellular, structural, and soluble components of the anatomic compartment in which the CLL cells reside.30 In vitro, different types of stromal cells and monocyte-derived cells, designated “nurse-like-cells,” promote CLL cell survival.30-32 In addition, T cells aggregate with proliferating CLL cells in so-called proliferation centers in BM and lymphoid tissue and are required for CLL cell proliferation in mice engrafted with PBMCs from CLL patients.33 Extensive in vitro studies identified many pathways and factors that enhance CLL cell survival and promote limited proliferation, including TLRs, cytokines, chemokines, CD40, B-cell-activating factor of tumor necrosis factor family (BAFF), integrins, and components of the extracellular matrix.22,25,31,34-38 Many of these extrinsic factors signal through SYK, PI3Kδ, and BTK and activate similar intracellular pathways, most prominently the PI3K/AKT/mTOR, NF-κB, and MAPK pathways. It is therefore difficult to estimate to what degree any single factor or pathway may be necessary or sufficient for CLL pathogenesis.39 Many of the most powerful adverse prognostic markers in CLL relate to both BCR signaling and the ability of the tumor cells to interact with the microenvironment, including unmutated IGHV, expression of ZAP70, and CD49d.40 In addition, CCL3 and CCL4 serum levels, which may serve as biomarkers of BCR signaling strength, also confer prognostic information.41
BCR signaling and downstream pathways. The BCR consists of a surface transmembrane Ig receptor associated with the Ig alpha (Igα, CD79A) and Ig beta (Igβ, CD79B) chains. BCR signaling in response to antigen binding induces LYN- and SYK-dependent phosphorylation of tyrosine motifs (phosphorylation denoted by “P” in yellow circle) on CD79A and CD79B. Several protein tyrosine kinases (red symbols) and the lipid kinase PI3Kδ (green symbol) transmit survival and proliferation signals and regulate cell maturation and migration. Small-molecule inhibitors of select kinases in the BCR pathway that have demonstrated significant clinical activitgips2 indAR ed.
BCR signaling and downstream pathways. The BCR consists of a surface transmembrane Ig receptor associated with the Ig alpha (Igα, CD79A) and Ig beta (Igβ, CD79B) chains. BCR signaling in response to antigen binding induces LYN- and SYK-dependent phosphorylation of tyrosine motifs (phosphorylation denoted by “P” in yellow circle) on CD79A and CD79B. Several protein tyrosine kinases (red symbols) and the lipid kinase PI3Kδ (green symbol) transmit survival and proliferation signals and regulate cell maturation and migration. Small-molecule inhibitors of select kinases in the BCR pathway that have demonstrated significant clinical activitgips2 indAR ed.
MYD88 mutations and TLR signaling in LPL
Somatic mutations in MYD88 (L265P) are found in >90% of patients with WM and are also common in IgM monoclonal gammopathy of undetermined significance, suggesting that this mutation may play a role in the development of the disease.42,43 MYD88 is an adaptor in the TLR pathway and the L265P mutation may enhance or trigger signaling through BTK and PI3Kδ to the NF-κB and AKT/mTOR pathways.10,44 A more detailed discussion of the genetics of LPL is provided in the chapter by Dr. Davide Rossi in this publication.
Small-molecule inhibitors of BCR signaling
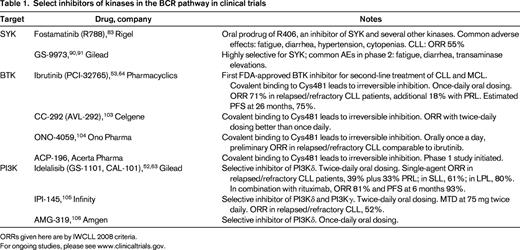
Several kinases in the BCR pathway can be targeted by small molecules. Most advanced in their clinical development are inhibitors of BTK, PI3K, and SYK (Table 1). Many of these inhibitors were initially developed for use in inflammatory diseases. Preclinical in vitro and in vivo studies identified these kinases as promising targets for the treatment of CLL and other B-cell malignancies (reviewed previously39 ), and their inhibition effectively interrupts BCR signaling, leading to reduced activation and proliferation of tumor cells.45-48 Because the same kinases also play important roles in pathways that regulate tumor-microenvironment interactions, the inhibitory effects of the small molecules extend beyond BCR signaling to such microenvironmental factors as chemokines, CD40 ligand, BAFF, fibronectin, and TLR ligands.48-50 Likewise, most inhibitors are not entirely specific to only one kinase, but may also inhibit additional (related) kinases to some degree.18,39 Furthermore, the kinases targeted by these small molecules also function in other immune cells. To what degree such tumor-extrinsic effects contribute to efficacy or to adverse events are becoming an important area of investigation.51
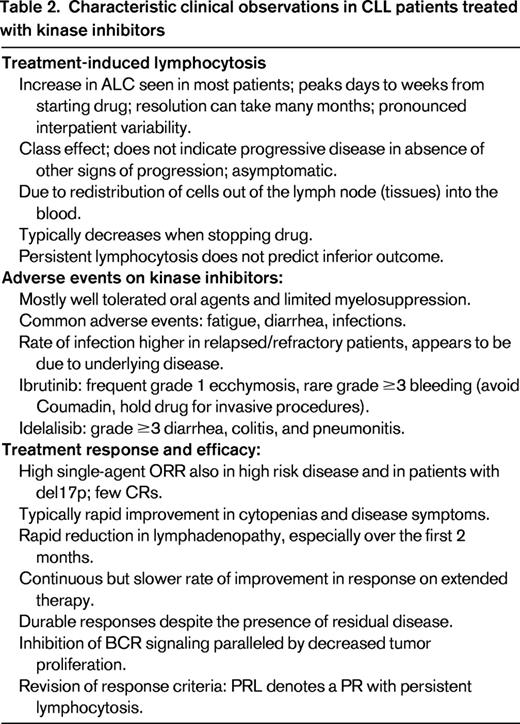
Patients treated with kinase inhibitors typically experience symptomatic improvement and rapid reduction in lymphadenopathy in parallel with a transient increase in absolute lymphocyte count (ALC; Table 2).52-54 In fact, in CLL, this treatment-induced lymphocytosis is a class effect of kinase inhibitors that target BCR signaling,39 with the caveat that it may be missed because the peak ALC can occur within the first days or even hours of starting the drug.54 There is consensus among experts that this treatment-induced lymphocytosis in the absence of signs of progression in other disease sites does not indicate disease progression and that patients can and should be maintained on drug.55 In addition, there is currently no evidence that the drug-induced increase in lymphocytosis in CLL patients is associated with morbidity.52-54 In most patients, the treatment-induced lymphocytosis peaks within the first 2 months before gradually resolving, but there is considerable interpatient variability. A subset of patients may show persistent lymphocytosis for many months to years on monotherapy and this does not appear to be a harbinger of treatment failure.47 Treatment-induced lymphocytosis is not limited to CLL; a 3-fold or greater increase in ALC was also recorded in patients with indolent non-Hodgkin's lymphoma (NHL) treated with idelalisib, mostly in SLL (64% of patients), and less commonly in follicular lymphoma (18%). Treatment-induced lymphocytosis was not seen in patients with LPL.56 In mantle cell lymphoma (MCL), ibrutinib transiently increased the ALC (≥50% increase and >5000 cells/μL) in 34% of patients.57
Decreased cell adhesion and reduced homing and migration of CLL cells are the likely factors contributing to lymphocytosis in patients treated with kinase inhibitors.58-60 Changes in immunophenotypic markers indicate that the increase in circulating CLL cells, at least in the first days, is due to the egress of cells from tissue compartments into the peripheral blood.54 Clearly, this lymphocytosis is not due to clonal expansion, because several studies have reported reduced tumor proliferation within days of starting treatment.45,47,54 Importantly, these targeted agents do not just redistribute the disease, because the increase in ALC does not match the decrease in nodal disease and there is often a dramatic and rapid reduction in total tumor burden, especially within the first few months.54 We also found that, upon starting ibrutinib, the frequency of dead or dying cells in the circulation doubled from baseline. Accordingly, ibrutinib inhibits proliferation and increases the rate of cell death, resulting in a gradual attrition of the tumor burden over time that matches well with the observed clinical response.54 The same conclusion has been reached using mathematical modeling.61 Therefore, despite significant reductions in total tumor burden over just a few weeks, tumor lysis syndrome has not been a common concern.62-64
Because of the treatment-induced lymphocytosis, many patients do not meet response criteria defined in the 2008 International Workshop on Chronic Lymphocytic Leukemia (IWCLL) guidelines despite clear and substantial clinical benefit.52,53,64 Recently, the authors of the IWCLL guidelines have clarified that patients meeting criteria for partial response (PR) but who have persistent lymphocytosis may be considered responders.65
In the next sections, I discuss in more detail ibrutinib, which was approved by the Food and Drug Administration (FDA) in February 2014 as a second-line treatment for CLL, and idelalisib, on which a decision is expected by August 2014. This is followed by a brief discussion of other kinase inhibitors in clinical trials.
Ibrutinib
Ibrutinib (formerly PCI-32765) is an orally bioavailable BTK inhibitor that irreversibly inactivates the kinase by covalently binding to a cysteine residue (Cys481) near the active site.66,67 BTK is a cytoplasmic tyrosine kinase of the TEC family that is essential for BCR signaling and couples BCR-induced calcium release to activation of the NF-κB pathway and cellular proliferation.68 Loss-of-function mutations in BTK block B-cell maturation at the pre-B-cell stage and cause X-linked agammaglobulinemia (also known as Bruton's agammaglobulinemia), which is characterized by the virtual absence of mature B cells and immunoglobulins, resulting in recurrent bacterial infections.69 Although BTK is expressed in myeloid cells, it does not appear to have essential functions outside of the B-cell compartment.68
Ibrutinib was approved by the FDA in November 2013 for the treatment of relapsed MCL and in February 2014 for relapsed/refractory CLL. BCR activation in B cells is inhibited with an IC50 of ∼10 nM.66,67 Few other kinases have homologous cysteine residues that can be covalently bound by ibrutinib, thereby conferring selective target inhibition.70 However, one of the other kinases inhibited by ibrutinib is ITK, the inhibition of which has been shown to enhance Th1-type immune responses in murine models.51 Nevertheless, BTK is likely the key target, as indicated by genetic mouse models and emerging data on ibrutinb resistance (discussed below).
Due to its covalent binding to BTK, ibrutinib can be given once daily despite the short half-life of the drug. The phase 1 study that dosed ibrutinib up to 12.5 mg/kg once daily did not establish a maximum tolerated dose.71 Target site occupancy in BTK was measured using a fluorescently labeled derivative of ibrutinib. Full BTK occupancy, a surrogate of complete kinase inhibition, was observed at 4 hours after administration of doses of ≥2.5 mg/kg. Subsequent studies in CLL used fixed doses of 420 and 840 mg once daily.53 On day 8, the pre-dose occupancy of BTK at the 420 mg dose level ranged from ∼60% to 99%, with no correlation between the degree of inhibition and best objective response.53
Safety.
Ibrutinib was very well tolerated and treatment discontinuation because of side effects rare. The most common side effects were grade 1-2, including diarrhea (47% of patients), upper respiratory tract infections (33%), fatigue (28%), cough (31%), arthralgia (27%), rash (27%), pyrexia (22%), and peripheral edema (21%).53 Grade 3 or 4 anemia, neutropenia, or thrombocytopenia were seen in ≤15% of patients. Bleeding events grade ≥3 occurred in 4 patients.53 Although BTK may play a role in glycoprotein signaling in platelets, the clinical significance of BTK inhibition is not clear and no consistent effect of ibrutinib on platelet aggregation was seen in routine testing.72 Grade ≥3 pneumonia and bacteremia was seen in 12% and 5% of patients with relapsed/refractory disease, respectively.53 However, this likely reflects the infection risk in this high-risk patient population because the frequency of infections decreased with time on study from 7.1 events per 100 patient-months during the first 6 months to 2.6 per 100 patient-months thereafter. In addition, grade ≥3 infections were less common in elderly, previously untreated patients.64 The majority of adverse events resolved without the need for suspension of treatment. Interestingly, ibrutinib did not significantly reduce immunoglobulin levels; on the contrary, both IgA and IgM have been found to increase on treatment.53,71,73
Single-agent efficacy.
The overall response rate (ORR) in the phase 1 study in patients with relapsed/refractory B-cell malignancies overall was 60%, with the highest rates in CLL (79%), MCL (78%), and LPL (75%). In this dose escalation trial, >1/3 of patients were treated at doses below the dose chosen for phase 2 studies. However, responses occurred at all dose levels.71
In the phase 1b/2 study in relapsed/refractory CLL, the ORR was 71% by 2008 IWCLL criteria,2 with complete response (CR) in 2 patients, and an additional 18% of patients achieved a PR with lymphocytosis (PRL). ORR was comparable across different risk groups, including del17p. At 26 months, the estimated PFS and overall survival (OS) were 75% and 83%, respectively. Disease progression occurred in 11 patients and, in 7, this appeared as a biologic transformation to diffuse large B-cell lymphoma (Richter's transformation). For patients with del17p (n = 28), the estimated rates of PFS and OS at 26 months were 57% and 70%, respectively.53 In our investigator-initiated, single-center, phase 2 trial (NCT01500733), PR at 6 months was recorded in 81% of patients with no del17p and in 53% of patients with del17p. However, including PRL, the ORR was 91% and 96%, respectively. The estimated event-free survival at 14 months was 93%.74
In an open label phase 3 study, 391 patients with relapsed or refractory CLL or SLL were randomly assigned to receive daily ibrutinib or the anti-CD20 mAb ofatumumab.62 The ORR for ibrutinib was 42.6% and for ofatumumab it was 4.1%. An additional 20% of ibrutinib-treated patients had PRL. At 6 months, the PFS with ibrutinib was 88% compared with 65% with ofatumumab (P < .001). Ibrutinib also significantly improved OS at 12 months to 90% compared with 81% in the ofatumumab arm.
Combination efficacy.
Burger at al reported on ibrutinib in combination with rituximab for 6 cycles, followed by ibrutinib until disease progression.75 The ORR was 95%, with CR in 8%. The redistribution lymphocytosis peaked earlier and resolved more rapidly than with single-agent ibrutinib. Brown et al reported results of a phase 1b/2 trial of 33 relapsed/refractory CLL patients (50% refractory to purine analogs, 53% bulky disease, 23% del17p) treated with ibrutinib in combination with bendamustine and rituximab.76 The ORR was 93% (13% CR) and at a median follow-up of 8.1 months the PFS was 90%. The response was compared with a historical ORR of 59% with bendamustine and rituximab alone.
Idelalisib
Idelalisib (formerly GS-1101 and CAL-101) is an orally bioavailable, selective, reversible inhibitor of the PI3Kδ isoform. The PI3K pathway is a key “hub” linking many signaling pathways to cellular growth, proliferation, and survival.77,78 PI3K isoforms α and β are expressed ubiquitously, whereas the PI3Kδ isoform is primarily expressed in leukocytes. PI3Kδ is essential for antigen-induced BCR signaling. In addition, PI3Kα can also participate in BCR signaling and promote cell survival (reviewed previously39 ). In a dose escalation phase 1 study of oral idelalisib in indolent NHL,56 MCL80 and CLL52 patients were treated at 6 dose levels ranging from 50 to 350 mg once or twice daily, and remained on continuous therapy while deriving clinical benefit. No maximum tolerated dose was established. Based on consistent reductions in lymphadenopathy, long PFS, and pharmacokinetic considerations, a dose of 150 mg twice daily was chosen for future studies.56
Safety.
The phase 1 dose escalation study conducted across a wide range of hematologic malignancies enrolled 54 patients with relapsed/refractory CLL.52 Commonly observed grade ≥3 adverse events were pneumonia (20%), neutropenic fever (11%), and diarrhea (6%).52 Most pneumonias appeared to be bacterial and 2 patients developed Pneumocystis jiroveci pneumonia. The rate of pneumonia on idelalisib was comparable to the rate of ∼0.06 pneumonias/patient-month reported previously for a similar CLL population.52,81 Two cases of possibly drug-related organizing pneumonia and one case of interstitial pneumonitis responded to corticosteroids and 2 of the 3 patients continued idelalisib. Treatment-emergent grade ≥3 neutropenia (43%), anemia (11%), and thrombocytopenia (17%) were reported mostly in patients with preexisting cytopenias.52 Diarrhea was reported in 29.6% of patients (grade ≥3 in 5.6%) and colitis in 7.4%. Except for 1 case, transaminase elevations in 28% of CLL patients were grade <3.
On a phase 2 study, 125 patients with indolent NHL were treated with idelalisib 150 mg twice daily, until disease progression.83 Twenty percent of patients discontinued drug due to adverse events and 34% required a dose reduction. Grade ≥3 diarrhea, colitis, or both developed in 16% of patients. Transaminase elevations were more common in indolent NHL than in CLL and were grade ≥3 in 13% of patients.82 The transaminase elevations were not dose related and appeared to be idiosyncratic reactions.56
Single-agent efficacy.
Among CLL patients, the ORR according to the 2008 IWCLL criteria was 39%.52 An additional 33% of patients had PRL. The median time to response was 1 month. The median PFS for all CLL patients enrolled was 15.8 months and 32 months for those receiving continuous dosing with idelalisib ≥150 mg twice daily. Although patients with a del17p or TP53 mutation responded to treatment, the median PFS in these patients was only 5 months, compared with 41 months in patients without this abnormality.52 The ORR in patients with LPL was 80%.82
Combination efficacy.
Study 116 randomized 220 frail patients with relapsed CLL to either idelalisib with rituximab or rituximab with placebo.63 The data-safety-monitoring board recommended early stopping due to excess events in the placebo group. The ORR (all PRs) was 81% in the idelalisib group compared with 13% in the placebo group. At 24 weeks, the PFS was 93% in the idelalisib group and 46% in the placebo group. The benefit of idelalisib and rituximab was similar in groups stratified by status of del17p, TP53 mutation, and IGHV mutation. Consistent with the monotherapy experience, serious adverse events more often encountered with idelalisib were pneumonitis and diarrhea. In contrast, infusion reactions with rituximab appeared to be milder in the idelalisib group.63
Select additional kinase inhibitors in clinical trials
In the slightly more than 7 years since the first patient was treated with the SYK inhibitor fostamatinib,83 there has been a virtual explosion of small molecules that target kinases in the BCR pathway (reviewed previously39,84 ). In addition to ibrutinib, 3 other covalent BTK inhibitors have entered clinical trials (CC-292, ONO-4059, and ACP-196). In addition, several noncovalent BTK inhibitors are in preclinical or very early clinical development (reviewed previously84 ). Many different PI3K inhibitors are in clinical trials. In B-cell malignancies, the focus has been on PI3Kδ inhibitors including idelalisib, AMG-199, and IPI-145 (which also inhibits PI3Kγ). Isoform-selective targeting of the PI3K pathway is an attractive option to prevent adverse events seen with inhibitors targeting multiple PI3K isoforms. However, in transformed cells, the dominant role of a specific isoform may be lost and different isoforms can assume redundant functions.85 Whether this will give rise to treatment failure remains to be defined. Table 2 lists select inhibitors in clinical trials; some of these are discussed briefly below.
SYK inhibitors
SYK and ZAP70 are cytoplasmic tyrosine kinases that together form a unique family and are each essential for BCR and TCR signaling transduction, respectively. In CLL, ZAP70 expression is more common in U-CLL than M-CLL, correlates with a more progressive disease course, and enhances the cellular response to BCR activation and chemokines independently of its kinase activity.28,86 Upon antigen binding to the BCR, LYN phosphorylates SYK, which in turn amplifies the initial BCR signal and activates the downstream signaling cascade. In addition, SYK is involved in chemokine, integrin, and Fc-receptor signaling.87
The first clinical trial of a SYK inhibitor used fostamatinib in patients with relapsed/refractory NHL and CLL.83 The dose-limiting toxicity was a combination of diarrhea, neutropenia, and thrombocytopenia. The ORR in 11 patients with CLL was 55%. In tumor cells sampled on treatment, fostamatinib effectively inhibited BCR signaling and reduced tumor proliferation.88 The subsequent development of fostamatinib focused on rheumatoid arthritis, with mixed results.89 GS-9973 is a highly selective and orally efficacious SYK inhibitor.90 On a phase 2 study, patients with CLL or indolent NHL were treated at 800 mg twice daily. Grade ≥3 adverse events were fatigue, transaminase elevations, and nausea. Nodal responses were seen in patients with or without del17p.91
Considerations and outlook on the role of kinase inhibitors in CLL
Why do kinase inhibitors work (so well)?
The impressive clinical activity of multiple different kinase inhibitors seems to be better than one would have predicted. Whether all of the therapeutic effects can be attributed to the inhibition of BCR signaling is not clear and the answer may differ among different B-cell malignancies. Functional studies with CLL cells in vitro, ongoing activation of CLL cells through the BCR in vivo, and evidence for antigen selection in cases with stereotyped BCRs are strong indicators that the BCR is a pivotal pathway in pathogenesis and disease progression (reviewed previously11,18,29,39,92 ). However, BCR activation seems to occur primarily in the lymph node microenvironment, where multiple additional factors may contribute or even be required for tumor proliferation.18,39,93 T cells may have an essential role, as shown by experiments demonstrating that reconstitution of a humanized microenvironment that can support CLL cell proliferation in NSG mice requires the cotransfer of human T cells.33,94 When T cells are eliminated, CLL cells do not proliferate.
In LPL, some observations also indicate a possible role for BCR activation. However, the MYD88 L265P mutation in the TLR pathway contributes to BTK activation, and both ibrutinib and idealisib may be clinically effective because they disrupt the aberrant TLR signaling in these tumors.43,95 It is possible that these kinase inhibitors are only efficacious because SYK, BTK, and PI3Kδ contribute to many different pathways with important roles in B-cell biology.39 However, this view begs the question of how inhibition of such central “hubs” that are active not only in B cells, but also in other lymphocytes and myeloid cells, can be as safe as these drugs appear to be.
What are the implications of residual disease on treatment with kinase inhibitors?
Most responses to monotherapy with kinase inhibitors are PRs and, even in combination with anti-CD20 mAbs, deep remissions are infrequent.63,75 Nevertheless, many responses are maintained for long periods of time despite the presence of residual disease.47,53 Although the depth of response often increases on continued treatment, there is a subset of patients who still have lymphocytosis at 12 or even 24 months.47,53 These persistent tumor cells are quiescent or “dormant” in that the activity of key signaling pathways is down-regulated, markers of cell activation are reduced, and tumor proliferation is undetectable.46,47 Therefore, these cells should not be considered resistant to drug and are not a harbinger of imminent relapse. An important landmark analysis showed that CLL patients who had PRL at the end of the first year on ibrutinib continued to maintain their response, whereas some patients having achieved a traditional PR or even CR relapsed over the next 12 months.47
What are the effects of kinase inhibitors on the normal immune system?
Inhibitors of the kinases SYK, BTK, and PI3K can affect normal immune function in 2 ways. First, the targeted kinase also functions in cells other than B cells. For example, PI3Kδ promotes the maturation and expansion of CD4 T-cell subsets and of T-regulatory cells.78 Second, the kinase inhibitor is not specific for only one kinase. For example, ibrutinib can covalently bind and thereby irreversibly inactivate a limited number of other kinases.66,70 One such kinase is ITK in T cells. Dubrovsky et al showed that ITK is inhibited in T cells of CLL patients treated with ibrutinib and, in a mouse model, they demonstrated that ibrutinib enhanced a Th1-type immune response that allowed the mice to better clear parasitic or intracellular bacterial infections.51 Further, in natural killer cells and macrophages, ibrutinib can inhibit Fc-receptor signaling, probably through combined effects on BTK, ITK, and TEC. A practical consequence may be that inhibition of these kinases could interfere with effector mechanisms contributing to the clinical efficacy of therapeutic antibodies.96 Whether these effects on other cell types are relevant for treatment responses in B-cell malignancies and/or for the side effect profile of different small molecules will be important to define. In the case of ibrutinib, inhibition of BTK appears to be the mainstay of therapeutic activity, as suggested by the selection of BTK mutations in resistant disease and mouse models of CLL that, when crossed with BTK-knockout mice, have substantially delayed disease onset.97,98
Resistance to kinase inhibitors
Resistance mechanisms to kinase inhibitors are being identified. Interestingly, they are not the usual suspects. Patients with adverse cytogenetic features, including those with del17p and del11q, bulky disease, or unmutated IGHV respond, at least initially, as well as patients without these characteristics.53,63 Mechanisms of resistance likely will differ depending on which kinase is targeted. Recently, acquired mutations in BTK and in phospholipase C gamma 2 (PLCγ2), a direct downstream target of BTK, were identified in 6 CLL patients who developed resistance to ibrutinib.99,100 Five patients showed a cysteine-to-serine mutation in BTK (C481S) at the binding site of ibrutinib that disrupts the covalent binding between the drug and the kinase and thereby dramatically decreases the potency of ibrutinib. Two patients, including one with a C481S mutation, had gain-of-function mutations in PLCγ2 that led to autonomous BCR signaling.99 In addition, patients with Richter's transformation appear not to (durably) respond to ibrutinib,53 suggesting that some of the biologic changes occurring during transformation lead to BTK independent tumors. Although any resistance is a clinical disappointment, the frequency so far is quite low, and the specific mutations in BTK are a powerful validation of the target and its importance in tumor biology. In MCL, high expression of PI3Kα has been associated with resistance to idelalisib.79 Whether PI3Kα could play a similar role in CLL is not clear.
Is combination therapy the way to go?
The absence of deep remissions, possible resistance to monotherapy, and the unproven tolerability and high cost of chronic treatment with these novel agents are all good reasons to pursue combination therapy. Current data on combinations in relapsed/refractory CLL patients are limited and response rates are not that different from monotherapy. In general, there is more rapid control of the treatment-induced lymphocytosis. Whether this is a valid goal to justify the possible toxicity of the additional agent is not evident. In particular, the more important end points such as PFS and rate of resistance await longer follow-up. Whether combining kinase inhibitors with current best first-line therapy can achieve deeper responses and cure the disease will be addressed in large studies. The answer to this question is obviously many years in the future.
We may also have to learn new rules of how to best combine drugs. Combination with chemotherapy seems to be “old fashioned,” but may work well because the mechanism of action is so different and there is a great deal of experience with chemotherapeutic agents. Dual kinase inhibitor therapy to hit 2 nodes in the pathway simultaneously could be more powerful, but likewise could also be more disruptive for normal cells. Combinations with other investigational agents may be mechanistically attractive, but combine 2 unknowns. Finally, a combination of immunotherapeutic approaches and kinase inhibitors could deliver an elegant “one-two punch” approach, but kinase inhibitors appear to change the immune system and these changes are still ill defined.
Rarely in CLL have there been so many good reasons to explore very different strategies. Therefore, it is particularly important to encourage all patients to participate in clinical trials to define the pros and cons of different approaches, which can then serve as the basis for individualized therapy. Clinical trials ongoing in the United States are registered at www.clinicaltrials.gov.
Should kinase inhibitors become the preferred treatment for everybody?
The greatest benefit of kinase inhibitors is seen in patients who have exhausted other treatment options and now suddenly have access to new and powerful medications that can turn dire situations around. Durability of response remains to be better defined, and, at least for younger patients having high-risk disease and an available well-matched donor, treatment with a kinase inhibitor followed by allogeneic transplantation may provide better long-term disease control than drug therapy alone.
Randomized clinical trials investigating kinase inhibitors as first-line therapy for CLL are ongoing.101 At this time, limited data suggest that patients who are unable to tolerate standard chemoimmunotherapy or who have del17p may benefit from starting kinase inhibitors in first-line.63,64,74 Conversely, maturing data with FCR (fludarabine + cyclophosphamide + rituximab) suggest that a subset of patients can have long-lasting deep remissions, raising the possibility that a proportion of patients are “cured” with FCR.9,102 In the M.D. Anderson experience, 35% of the patients in the initial cohort were alive and relapse-free 10 years from starting FCR. Further, a subset of these patients, tested with flow cytometry, was found to have no residual disease! Although many of these patients had lower-risk disease at the initiation of treatment (M-CLL, Rai stage <3, serum β2-microglobulin <4 mg/dL), these results suggest that up to 1/3 of patients may be cured.102 Therefore, for this group of patients, the relative benefit of novel agents would have to be demonstrated with regard to safety and tolerability.
Outlook
One thing is clear: patients with CLL and LPL have novel effective treatment options that are improving overall survival and quality of life. For once, patients in greatest need may actually reap the greatest benefit. For many among them, these novel agents can be life savers. Other patients already have excellent treatment options available and the tradeoff between different approaches remains to be defined. Increasingly, individual preferences and choices may become important factors in decision making. Unfortunately, the many options may create some anguish about choosing the “best” treatment. On the other hand, it is reassuring that if one treatment fails, there are other good options that can save the day.
Acknowledgments
The author is supported by the intramural research program of the National Heart, Lung, and Blood Institute of the National Institutes of Health.
Disclosures
Conflict-of-interest disclosure: The author has received research funding from and has consulted for Pharmacyclics. Off-label drug use: Ibrutinib as first-line treatment of CLL.
Correspondence
Adrian Wiestner, Hematology Branch, NHLBI, NIH, Bldg. 10, CRC 3-5140, 10 Center Drive, 20892-1202 Bethesda, MD; Phone: 301-496-5093; Fax: 301-496-8396; e-mail: wiestnea@nhlbi.nih.gov.