Abstract
The development of neutralizing antibodies against factor VIII (FVIII inhibitors) and factor IX (FIX inhibitors) is the major complication in hemophilia care today. The antibodies neutralize the biological activity of FVIII and FIX and render replacement therapies ineffective. Antibodies are generated as a result of a cascade of tightly regulated interactions between different cells of the innate and the adaptive immune system located in distinct compartments. Any event that modulates the repertoire of specific B or T cells, the activation state of the innate and adaptive immune system, or the migration pattern of immune cells will therefore potentially influence the risk for patients to develop inhibitors. This chapter reviews our current understanding of different pathways of antibody development that result in different qualities of antibodies. Potential differences in differentiation pathways leading to high-affinity neutralizing or low-affinity non-neutralizing antibodies and the potential influence of gene polymorphisms such as HLA haplotype, FVIII haplotype, and polymorphisms of immunoregulatory genes are discussed.
Learning Objectives
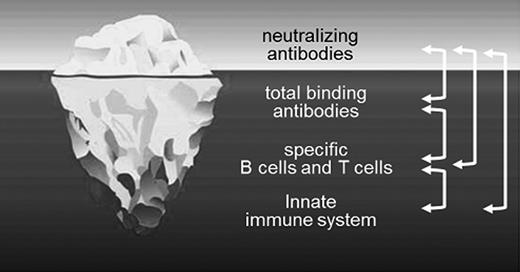
To understand that FVIII and FIX inhibitors are only the tip of the iceberg: antibodies are generated as a result of a cascade of tightly regulated interactions between different cells of the innate and the adaptive immune system located in distinct compartments
To understand that any event that affects the activation state of the innate or the adaptive immune system, the repertoire of specific B or T cells, or the migration pattern of immune cells potentially influences the risk for patients to develop FVIII or FIX inhibitors
Neutralizing antibodies against FVIII and FIX are the major challenge in replacement therapies for patients with hemophilia
The development of neutralizing antibodies against factor VIII (FVIII inhibitors) and factor IX (FIX inhibitors) is the major complication in hemophilia care today. The antibodies neutralize the biological activity of FVIII and FIX and render replacement therapies ineffective. FVIII inhibitors develop in ∼20%-32% of patients with severe hemophilia A (plasma FVIII activities <1%) and in ∼3%-13% of patients with moderate (plasma FVIII activity 1%–5%) and mild (plasma FVIII activity 5%–25%) hemophilia A.1,2 Recently, Eckardt et al3 reported that the risk for patients with mild and moderate hemophilia A to form inhibitors increases with an increasing number of days of exposure to FVIII products and might be higher than anticipated.
Most FVIII inhibitors bind to functionally important domains of FVIII and prevent its interaction with other coagulation factors such as factors IIa, IXa, and X and VWF or with phospholipids.4 Other FVIII inhibitors have catalytic activities and hydrolyze the protein.4
FIX inhibitors are seen less frequently than FVIII inhibitors. Their overall incidence is 1%–3% for all patients with hemophilia B treated with FIX products and 9%–23% for patients with severe hemophilia B who express plasma FIX activities <1%.5 The development of FIX inhibitors is frequently associated with anaphylactic reactions, a complication that is rarely seen with FVIII inhibitors in hemophilia A.5 The reason that FIX inhibitors are associated with anaphylactic reactions is unclear. Several potential root causes have been suggested, but have not been formally proven. One suggestion is that the smaller molecular weight of FIX (55 kD) might be important because it allows FIX to be distributed into the extravascular space, which may facilitate mast cell activation and IgE-mediated hypersensitivity triggered by binding of FIX to FIX-specific IgE.6 In contrast, FVIII bound to VWF stays in the intravascular space. Another potential root cause could be that patients with hemophilia B are exposed to much larger amounts of exogenous protein when treated with standard doses of FIX: 1 unit of FIX is ∼5 μg of FIX protein, whereas 1 unit of FVIII is only ∼100 ng of FVIII protein. Large amounts of FIX protein in the presence of FIX inhibitors could result in high concentrations of circulating immune complexes, which might trigger anaphylactic reactions. So far, however, immune complex formation has not been reported in patients with anaphylactic reactions to FIX.5
Why some patients develop neutralizing antibodies whereas others do not is far from clear. There is evidence that both genetic and nongenetic factors influence patients' susceptibility to developing FVIII or FIX inhibitors.6-9 The types of F8 or F9 gene mutations that cause the disease are a major risk factor for the development of inhibitors.6,7 Mutations that result in the absence or severe truncation of the FVIII or FIX protein are associated with the highest risk, whereas mutations causing the generation of a dysfunctional FVIII or FIX protein are associated with a lower risk. Other genetic risk factors include race/ethnicity, family history, polymorphisms in genes coding for the MHC, and polymorphisms of certain immunoregulatory genes. Nongenetic risk factors are still the subject of extensive studies, with intensity of treatment at first or at any exposure, surgical procedures, product-related factors, and treatment in association with major immune challenges gaining most attention. Conversely, prophylaxis has been intensively discussed as a potential protective factor in association with FVIII inhibitor development.8,9
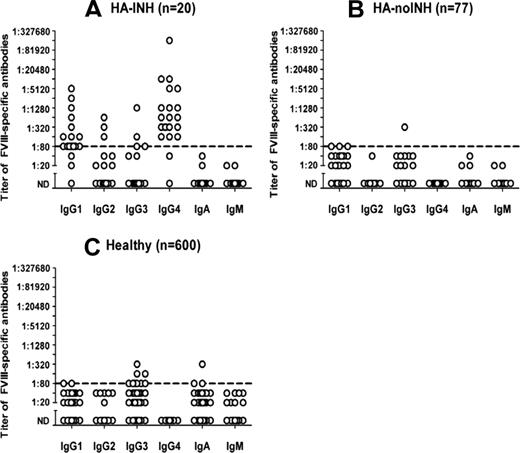
In clinical practice, unwanted immune responses against FVIII or FIX are commonly identified as FVIII or FIX inhibitors using Bethesda or Nijmegen-modified Bethesda assays that assess the neutralizing capacity of FVIII- or FIX-specific antibodies.10,11 Although this is vital information, testing solely for inhibitors is like uncovering the tip of the iceberg while the complexity of FVIII- or FIX-specific immune responses remains under the surface (Figure 1). Antibodies are produced as a result of a cascade of tightly regulated interactions between different cells of the innate and adaptive immune system located in distinct compartments. Any event that modulates the repertoire, activation state, or migration pattern of immune cells will therefore potentially influence the risk for patients to develop inhibitors. In the future, it will be important to monitor additional immunological variables to better understand the kinetics of inhibitors and how they evolve in patients with hemophilia who receive replacement therapies. Recently, we presented a comprehensive analysis of the prevalence of FVIII-specific antibodies found in different cohorts of patients with hemophilia A and in healthy individuals.12 We not only assessed FVIII inhibitors, but also analyzed the total FVIII-binding antibody response, including breaking down Ig isotypes and IgG subclasses. Our data indicate that FVIII inhibitors are only part of the overall antibody spectrum directed against FVIII. There are binding antibodies with specificity to FVIII that do not neutralize the protein and cannot be detected using Bethesda assays. In addition, circulating antibodies against FVIII are found in some patients without FVIII inhibitors and even in some healthy subjects. Moreover, we found considerable differences for IgG subclasses of FVIII-binding antibodies between the different study cohorts. IgG4 and IgG1 were the most abundant IgG subclasses in patients with FVIII inhibitors, whereas IgG1, IgG3, and IgA dominated the FVIII-specific antibody response in patients without inhibitors and in healthy individuals (Figure 2). Remarkably, IgG4 was completely absent in patients without inhibitors and in healthy subjects. The question remains as to which regulatory pathways give rise to the production of the various populations of FVIII-binding antibodies. Moreover, further investigations are required to find the relation, if any, between neutralizing and non-neutralizing antibodies and to explain the biological significance of non-neutralizing antibodies in patients and healthy subjects.
Neutralizing antibodies are only the tip of the iceberg. Neutralizing antibody responses are induced as a result of a cascade of tightly regulated interactions between different cells of the innate and adaptive immune system located in distinct compartments. Any event that modulates the repertoire, activation state, or migration pattern of immune cells will therefore potentially influence the risk of patients developing inhibitors. (Figure adapted from license-free figure 5348288 from www.fotolia.de)
Neutralizing antibodies are only the tip of the iceberg. Neutralizing antibody responses are induced as a result of a cascade of tightly regulated interactions between different cells of the innate and adaptive immune system located in distinct compartments. Any event that modulates the repertoire, activation state, or migration pattern of immune cells will therefore potentially influence the risk of patients developing inhibitors. (Figure adapted from license-free figure 5348288 from www.fotolia.de)
Titers of FVIII-binding antibodies assessed for individual Ig isotypes and IgG subclasses. Shown are the detected titers of Ig isotypes and IgG subclasses of FVIII-binding antibodies for patients with hemophilia A and inhibitors (HA-INH; A), for patients with hemophilia A without inhibitors (HA-noINH; B), and for healthy individuals (C). Plasma samples were diluted at least 1:20. Samples that did not give a positive signal at this minimum dilution were considered as negative (not detectable, ND). The dotted line at a titer of 1:80 indicates the minimum titer required for proof of specificity. Titers of <1:80 were too low to be confirmed for specificity. (Figure and legend reprinted with permission from Whelan et al.12 )
Titers of FVIII-binding antibodies assessed for individual Ig isotypes and IgG subclasses. Shown are the detected titers of Ig isotypes and IgG subclasses of FVIII-binding antibodies for patients with hemophilia A and inhibitors (HA-INH; A), for patients with hemophilia A without inhibitors (HA-noINH; B), and for healthy individuals (C). Plasma samples were diluted at least 1:20. Samples that did not give a positive signal at this minimum dilution were considered as negative (not detectable, ND). The dotted line at a titer of 1:80 indicates the minimum titer required for proof of specificity. Titers of <1:80 were too low to be confirmed for specificity. (Figure and legend reprinted with permission from Whelan et al.12 )
Current understanding of the regulation of antibody responses against proteins: T-cell-dependent and T-cell-independent pathways
The initial event in any antibody response against proteins is the recognition of proteins by specific BCRs expressed on naive B cells. Most of these B cells reside in and circulate through the B-cell follicles of peripheral lymphoid organs such as spleen, lymph nodes, or mucosal lymphoid tissues. BCR binding of proteins initiates the activation of intracellular signal-transduction pathways, which can eventually lead to B-cell activation and clonal expansion and differentiation into antibody-producing plasma cells. Ligation of BCRs by a monovalent protein antigen such as FVIII or FIX is unlikely to be sufficient to initiate clonal expansion and differentiation of B cells. Additional activation signals, such as those provided by cognate interactions with activated CD4+ T cells or by cross-linking of BCRs, accompanied by a triggering of the innate immune system are probably required.13
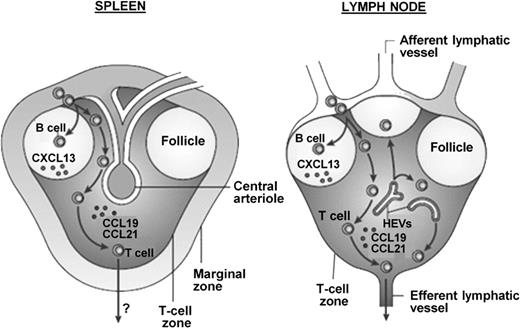
B-cell follicles are located in the white pulp of peripheral lymphoid organs, which are segregated into regions enriched with B cells (follicles) and regions enriched with T cells (T-cell zones) (Figure 3). This segregation is maintained by region-specific cytokine/chemokine secretion.14 B-cell follicles are positioned adjacent to T-cell zones, facilitating the interaction of activated B cells and activated T cells. The spleen contains an additional compartment, the marginal zone (Figure 3), which is an important transit area for cells leaving the bloodstream and entering the splenic white pulp.14 The marginal zone contains specific macrophage populations and nonrecirculating B cells, providing a compartment for both innate and adaptive immune responses.14 The unique position of marginal zone B cells allows them to play an important role in immune responses to antigens delivered via the blood. Given sufficient stimulatory signals, activated marginal zone B cells can rapidly differentiate into short-lived antibody-secreting plasma cells independently of T-cell help.15
Comparison of murine lymphoid compartments and the migration pathways of lymphocytes into the splenic white pulp and the lymph nodes. Spleen: Lymphocytes enter the white pulp of the spleen from the marginal zone and entry is mediated by signaling through chemokine receptors. B cells are attracted to the B-cell follicles by CXC-chemokine ligand 13 (CXCL13), whereas T cells are directed to the T-cell zone by responding to CC-chemokine ligand 19 (CCL19) and CCL21. It is unclear how lymphocytes eventually leave the white pulp. Lymph node: Few lymphocytes enter the lymph node from the afferent lymphatic vessels. Most lymphocytes enter through specialized blood vessels that are known as high endothelial venules (HEVs) and then migrate to the B-cell follicles or the T-cell zone, which again is regulated by CXCL13, CCL19, and CCL21, respectively. Lymphocytes exit lymph nodes in efferent lymphatic vessels and then reenter the bloodstream from the lymph. (Figure and legend reprinted from Mebius and Kraal.14 )
Comparison of murine lymphoid compartments and the migration pathways of lymphocytes into the splenic white pulp and the lymph nodes. Spleen: Lymphocytes enter the white pulp of the spleen from the marginal zone and entry is mediated by signaling through chemokine receptors. B cells are attracted to the B-cell follicles by CXC-chemokine ligand 13 (CXCL13), whereas T cells are directed to the T-cell zone by responding to CC-chemokine ligand 19 (CCL19) and CCL21. It is unclear how lymphocytes eventually leave the white pulp. Lymph node: Few lymphocytes enter the lymph node from the afferent lymphatic vessels. Most lymphocytes enter through specialized blood vessels that are known as high endothelial venules (HEVs) and then migrate to the B-cell follicles or the T-cell zone, which again is regulated by CXCL13, CCL19, and CCL21, respectively. Lymphocytes exit lymph nodes in efferent lymphatic vessels and then reenter the bloodstream from the lymph. (Figure and legend reprinted from Mebius and Kraal.14 )
Follicular B cells can enter different pathways for differentiation into antibody-producing plasma cells: extrafollicular differentiation pathways (outside of B-cell follicles) and follicular differentiation pathways (inside of B-cell follicles in germinal centers). Which differentiation pathway an activated follicular B cell enters has substantial consequences for the survival and location of the resulting antibody-producing plasma cells and for the quality and quantity of the antibodies that they secrete. Plasma cells that arise from extrafollicular pathways are reported to be predominantly short-lived and nonmigratory. The antibodies that they secrete are of low or moderate affinity.13 Extrafollicular pathways of B-cell differentiation can be either T-cell dependent or T-cell independent.13 In contrast, plasma cells that develop from follicular pathways in germinal centers are predominantly long-lived. They migrate to the BM were they can survive in specific plasma cell niches. The antibodies that they produce are of high affinity.13 Germinal centers are specialized microenvironments that are established during a T-cell-dependent immune response. They are seeded by antigen-specific B cells and CD4+ T cells that were activated during the early phases of the immune response. The interaction of antigen-specific B cells and CD4+ T cells initiates the expansion and differentiation of B cells and also triggers isotype switching and affinity maturation of antibodies, which results in the switch from IgM to IgG, IgA, and IgE and, furthermore, in the generation of high-affinity antibodies.16
Clinical and experimental data demonstrate that the development of FVIII inhibitors depends on CD4+ T-cell help.17,18 This indicates that FVIII inhibitors are most likely the result of the follicular pathway of plasma cell development. In this case, plasma cells develop in germinal centers that provide the microenvironment required for close interactions of specific follicular B cells and CD4+ T cells. Plasma cells arising from this pathway are usually long-lived and produce high-affinity antibodies.
Low-titer, non-neutralizing FVIII-specific antibodies as found in healthy subjects and in patients without FVIII inhibitors could be the result of either the differentiation of marginal zone B cells into plasma cells or of the extrafollicular differentiation pathway of follicular B cells. Therefore, neutralizing high-affinity and non-neutralizing low-affinity FVIII-specific antibodies are most likely produced by different subsets of plasma cells that are generated by distinct pathways of B-cell differentiation.
HLA haplotypes and the risk of FVIII-inhibitor formation
The HLA-class II complex (the human version of the MHC-class II complex) is essential for shaping the CD4+ T-cell repertoire in the thymus and for selecting antigenic peptides that are presented to CD4+ T cells in peripheral lymphoid organs.19 Clinical and experimental data indicate that the development of FVIII inhibitors depends on CD4+ T-cell help. CD4+ T cells express TCRs that recognize antigen-derived peptides presented by HLA-class II molecules expressed on specialized APCs in the periphery. Structural features of both the HLA-class II molecule and the antigenic peptide determine the specificity of CD4+ T cells that can bind to the complex formed between HLA-class II molecules and peptides.20 Recently, Wroblewska et al21 summarized our current understanding of FVIII processing and the presentation of FVIII-derived peptides via HLA-class II molecules.
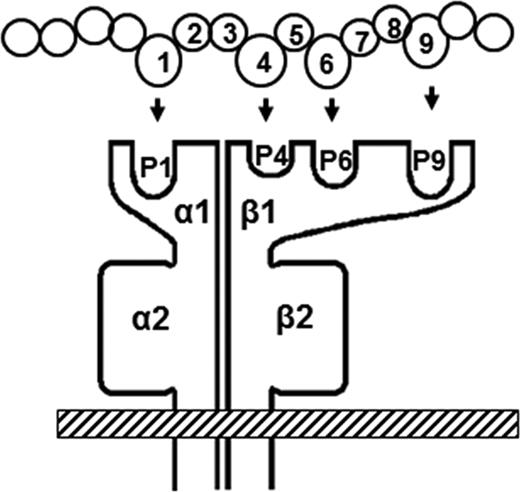
HLA-class II molecules are heterodimeric proteins. They consist of 2 noncovalently associated polypeptide chains, the alpha (α) chain and the beta (β) chain (Figure 4). Each α- and β chain has 2 domains: the highly conserved α2 and β2 domains and the highly polymorphic α1 and β1 domains. The α1 and β1 domains form an open binding groove that presents peptides to CD4+ T cells. The binding groove can accommodate peptides of ∼12-25 amino acids, depending on charge, stability, and affinity. The binding groove is mainly characterized by the properties of the so-called P1, P4, P6, and P9 pockets (Figure 4), which confer the specificity to the anchor residues of the peptides bound to the groove.22 The conformation of the peptide (residues 1-9; Figure 4) that is bound to the groove is determined by hydrogen bonding between HLA-class II residues and the peptide backbone. Therefore, the conformation adopted by the peptide is independent of its sequence and is different from the conformation of the peptide sequence in the context of its native protein.22 The HLA-class II region genes code for 3 major class II molecules: DP, DQ, and DR.
Schematic picture of an MHC-class II molecule and a pepide. Presented is an MHC-class II molecule with the peptide-binding groove containing the peptide-binding pockets P1, P4, P6, and P9. Each pocket binds an anchor residue of a peptide. The properties of the binding pockets define the peptides that can be bound and presented to CD4+ T cells. (Figure and legend reprinted from Reipert et al.41 )
Schematic picture of an MHC-class II molecule and a pepide. Presented is an MHC-class II molecule with the peptide-binding groove containing the peptide-binding pockets P1, P4, P6, and P9. Each pocket binds an anchor residue of a peptide. The properties of the binding pockets define the peptides that can be bound and presented to CD4+ T cells. (Figure and legend reprinted from Reipert et al.41 )
Despite the high degree of polymorphism of the HLA-class II region, 3 major HLA-class II haplotypes, DR2(DRB1*1501)/DQ6(DQB1*0602), DR3(DRB1*0301)/DQ2(DQB1*0201), and DR4(DRB1*0401)/DQ8(DQb1*0302), account for the association of HLA-class II with ∼90% of all human autoimmune diseases.23 What makes these 3 haplotypes so unique among the potentially thousands of HLA-class II haplotypes in the human population is unclear. Mangalam et al23 recently suggested that these haplotypes have survived bottlenecks of infectious episodes in human history because of their ability to efficiently present pathogenic peptides to activate CD4+ T cells that secrete cytokines to clear infections. Unfortunately, these haplotypes also efficiently present self-peptides to activate autoreactive CD4+ T cells that cause autoimmune diseases.23 Interestingly, 1 of these 3 HLA-class II haplotypes, DR2(DRB1*1501)/DQ6(DQB1*0602), has also been shown to be associated with an increased risk for patients with hemophilia to develop FVIII inhibitors.24-26 Although the increase in risk associated with the DRB1*15/DQB1*0602 haplotype was reported to be only modest and did not always reach statistical significance, the data could indicate that this haplotype is particularly efficient in presenting FVIII peptides to FVIII-specific CD4+ T cells in patients. In general, the association of distinct HLA haplotypes with the risk of patients developing FVIII inhibitors seems to be rather modest. This could be because FVIII is a large protein that can provide immunogenic peptides for many different HLA-class II haplotypes. Furthermore, at least some of the FVIII peptides generated and presented by human APCs seem to be promiscuous, meaning that they can bind to a range of different HLA-class II haplotypes.27,28 Identifying the peptides selected by HLA-class II molecules during the natural processing of FVIII or FIX will be of key importance in understanding the repertoire of FVIII- or FIX-specific CD4+ T cells and how these T cells modulate FVIII- and FIX-specific antibody responses in patients with hemophilia A or B. Moreover, it will be important to design methods to compare peptides selected during the processing of natural FVIII and FIX proteins with those selected during the processing of chemically or genetically modified FVIII or FIX proteins. This information will help us to understand whether and how chemical or genetic modifications of natural proteins influence the immunogenicity of FVIII and FIX. Recently, Sauna et al29 used a computational in silico approach to investigate whether new junctions resulting from protein engineering in the generation of B-domain deleted (BDD) FVIII products could give rise to neoepitopes for CD4+ T cells. That study identified several peptides generated from the new junctions in BDDFVIII products that could contain neoepitopes for CD4+ T cells if they were generated and selected during the natural processing of these modified FVIII proteins. The investigators cautioned that their approach was based on computational assessments and would need experimental confirmation. However, the data presented by Sauna et al29 indicate that any genetic modification of FVIII or FIX proteins and any artificial linker region requires careful evaluation for potential generation of neoepitopes for CD4+ T cells that might be associated with altered immunogenicity of the protein. Another interesting aspect is the question if the intracellular processing of different biological forms of FVIII, for example, FVIII bound to VWF as present in the circulation, thrombin-activated FVIII as present at the site of coagulation, and FVIII fragments as present after FVIII inactivation, will result in the selection of different peptides to be presented by the HLA-class II system. Any difference could contribute to potential treatment-related differences in the immunogenicity of FVIII products, depending on whether the product is given prophylactically or on demand. Modern technologies such as T-cell hybridoma libraries derived from humanized mouse models, as described by Steinitz et al,27 or mass spectrometry for the analysis of FVIII peptides eluted from HLA-class II expressed on APCs, as described by van Haren et al,28 will help to address these questions in the future.
Polymorphisms of immunoregulatory genes and FVIII haplotypes
Antibodies are generated as a result of a cascade of tightly regulated interactions between different cells of the innate and the adaptive immune system located in distinct compartments. There is evidence that FVIII-inhibitor development depends on CD4+ T-cell help. CD4+ T cells recognize FVIII-derived peptides presented by HLA-class II molecules expressed on specialized APCs. The microenvironment in which CD4+ T cells interact with APCs determines the outcome of the immune response. A microenvironment that favors stimulation of the innate immune system will facilitate the induction of effector CD4+ T cells that are able to promote clonal expansion and differentiation of B cells into antibody-producing plasma cells. A microenvironment that does not provide any stimulus for the innate immune system will facilitate nonresponsiveness or the induction of immune tolerance associated with the active suppression of antibody responses.23,30 Therefore, polymorphisms in promoter regions of immunoregulatory genes that lead to modifications in the activation status of innate immune cells or to changes in the expression levels of costimulatory or inhibitory molecules expressed by B cells, T cells, or innate immune cells will likely influence the outcome of immune responses against FVIII or FIX.
Polymorphisms of immunoregulatory genes
Previously, Dimitrov et al31 demonstrated that the induction of heme oxygenase-1, a stress-inducible enzyme with potent anti-inflammatory activity, significantly reduced the development of FVIII inhibitors in hemophilic mice that received treatment with human FVIII. More recently, Repesse et al32 presented data showing that patients with FVIII inhibitors have a higher frequency of gene polymorphisms in the promoter region of the heme oxygenase-1-encoding gene (HMOXI-1) and that they are associated with reduced expression levels of the HMOXI-1 gene. Both sets of data support the importance of the activation state of the innate immune system for the outcome of the immune response to FVIII.
Astermark et al33,34 reported that certain polymorphisms in the promoter regions of the IL10 gene and the TNF-α gene are associated with an increased risk of patients with hemophilia developing FVIII inhibitors. In an independent study, Pavlova et al26 confirmed the importance of these polymorphisms, which were shown to be associated with an increased expression of the respective genes. IL10 is known to be a growth and differentiation factor for activated human B cells and to induce activated B cells to secrete large amounts of antibodies. TNF-α is a well-characterized proinflammatory cytokine with multiple functions in inflammatory diseases. Astermark et al35 also identified a protective association between a polymorphism in the promoter region of the cytotoxic T-lymphocyte associated protein-4 (CTLA-4) gene and the risk of patients developing FVIII inhibitors. CTLA-4 is a regulatory molecule expressed on activated T cells. It binds to the accessory molecule B7 and down-regulates T-cell-dependent immune responses. CTLA-4–Ig constructs, which suppress the interaction between B7 expressed on APCs and CD28 expressed on T lymphocytes, were shown to prevent the development of anti-FVIII antibody responses in hemophilic mice; this supports the protective function of CTLA-4 against the development of FVIII inhibitors.36
FVIII haplotypes
Based on current knowledge, the available repertoire of FVIII- or FIX-specific CD4+ T cells is shaped in the thymus during embryonic development and involves positive and negative selection processes. Positive selection ensures that only T cells that recognize antigens in association with self-HLA molecules are selected. T cells that survive positive selection undergo negative selection, which results in clonal deletion of T cells with strong reactivity to self-antigens.19 Antigens that are not present in this process cannot cause clonal deletion of reactive T cells. Therefore, patients with large deletions in their F8 or F9 genes cannot be expected to efficiently delete wild-type FVIII- or wild-type FIX-specific CD4+ T cells during negative selection. These patients are likely to have higher frequencies of FVIII- or FIX-specific CD4+ T cells in the periphery, which could be a root cause for their susceptibility to developing inhibitors. Likewise, patients with small deletions or single point mutations that cause differences in the amino acid sequence between their endogenous FVIII or FIX proteins and the wild-type FVIII or FIX present in replacement products might not be able to sufficiently delete all the CD4+ T cells that recognize peptides derived from the wild-type proteins. However, this depends entirely on the individual HLA-class II haplotype of the patient and on the ability of his or her APCs to generate and present those FVIII peptides that cover the region of difference.
Howard et al37 identified 4 nonsynonymous single-nucleotide polymorphisms with F8 haplotypes (allelic combinations) that encode 6 distinct FVIII proteins. The investigators designated these H1, H2, H3, H4, H5, and H6. They found H1 and H2 proteins, which are present in currently available recombinant full-length FVIII products, in all racial groups and H3, H4 and H5 proteins only in black subjects. Viel et al38 recently speculated that the mismatch between the H1/H2 FVIII proteins present in FVIII products and the endogenous H3/H4 FVIII proteins present in many black subjects might contribute to the risk of H3/H4 carriers developing FVIII inhibitors. The investigators sequenced the F8 genes of 78 black patients with hemophilia A and found that patients with the haplotypes H3 and H4 had a higher risk of developing FVIII inhibitors than patients with the haplotypes H1 or H2. However, they did not provide evidence that peptides arising from the mismatch between the endogenous FVIII proteins and the FVIII proteins present in FVIII products are indeed generated and presented by the APCs of patients with H3 and H4 who developed FVIII inhibitors. Furthermore, the investigators did not take into account potential differences in polymorphisms of the HLA complex or in immunoregulatory genes between patients with H1/H2 and patients with H3/H4. Therefore, it is still not clear whether such mismatches do indeed contribute to the risk of patients developing FVIII inhibitors. Indeed, Schwarz et al39 could not confirm this association when they analyzed their data from 49 patients of African ancestry.
In conclusion, genetic polymorphisms that result in a modulation of the activation state of the innate or adaptive immune system or in changes of the frequencies of specific B or T cells can substantially alter the risk of patients with hemophilia developing antibodies against FVIII or FIX. Recently, the results of a genome-wide association study were reported. The investigators evaluated 13 331 single nucleotide polymorphisms from 1081 genes for the association with inhibitor development in patients with hemophilia A. The study group included 833 patients from 3 independent hemophilia A cohorts. The investigators identified 53 single nucleotide polymorphisms that showed a significant association with the risk of patients developing FVIII inhibitors. This study highlighted the complexity of the genetic polymorphisms that might modulate antibody responses against FVIII and FIX.40
Summary and conclusion
Neutralizing antibodies against FVIII or FIX are generated as a result of a cascade of tightly regulated interactions between different cells of the innate and the adaptive immune system located in distinct compartments. HLA-haplotype, race/ethnicity, polymorphisms in immunoregulatory genes, and FVIII/FIX mutations were shown to influence the susceptibility of patients to develop these antibodies. However, the immunoregulatory pathways that give rise to the generation of the different populations of neutralizing and non-neutralizing antibodies remain elusive.
Disclosures
Conflict-of-interest disclosure: The author is employed by Baxter Innovation GmbH. Off-label drug use: None disclosed.
Correspondence
Birgit M. Reipert, Baxter Innovation GmbH, Industriestrasse 72, A-1220 Vienna, Austria; Phone: 43-1-20100-2471285; Fax: 43-1-20100-5049; e-mail: birgit_reipert@baxter.com.