Abstract
Long-term survivors of Hodgkin lymphoma (HL) are at an increased risk for a range of late complications, with subsequent malignant neoplasm and cardiovascular disease representing the 2 leading causes of death in these patients. Raising awareness, close follow-up, and adoption of selected early-detection and risk-reduction strategies may help to reduce the adverse impact of these late effects on patients. This chapter reviews known long-term complications of HL therapy, risk factors, and the timing of their occurrence. Where available, data on the efficacy of screening for selected late effects of HL are presented. Current evidence-based and consensus-based recommendations on follow-up of long-term HL survivors are also reviewed. As HL therapy evolves over time, late effects and implications on follow-up of patients treated in the contemporary era should be considered and opportunities for future research should be explored.
Learning Objectives
To review the risk of and risk factors for late effects after HL therapy
To discuss data on the efficacy of screening strategies for selected late effects of HL
To summarize current follow-up recommendations for long-term HL survivors
Introduction
Long-term Hodgkin lymphoma (HL) survivors are at risk of developing a range of therapy-related complications that may present years after treatment. These complications have resulted in an increased mortality among HL survivors. Early detection through screening and risk-reduction strategies may reduce the adverse impact of some of these late effects on patients. This chapter summarizes selected late effects in long-term HL survivors. In addition, treatment-related and patient-related risk factors are discussed. Finally, current recommendations on optimal follow-up of long-term survivors are summarized.
Late effects after HL
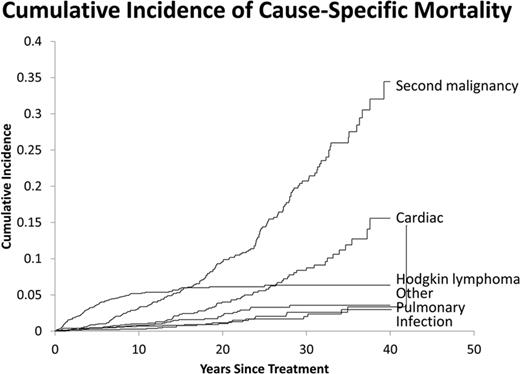
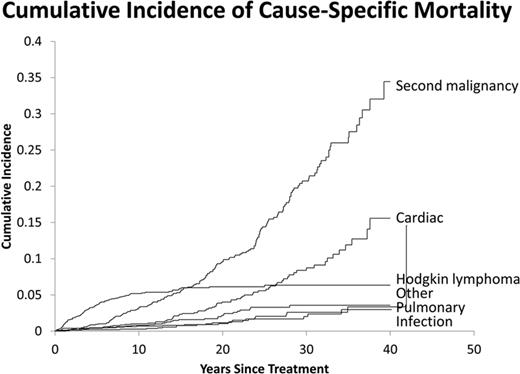
A diverse array of late effects of HL therapy have been documented. Several studies focusing on competing mortality after HL therapy have shown that, whereas deaths from HL level off after the first 10-15 years, deaths from other causes, most notably second malignancy and cardiac disease, continue to increase over time. Figure 1 shows the cumulative incidence of cause-specific mortality of 1542 stage I and II HL patients treated from 1967 to 2007 at the Dana-Farber/Harvard Cancer Center. Other late effects, including noncoronary vascular disease, pulmonary dysfunction, xerostomia resulting in increased risk of dental caries and periodontal disease, hypothyroidism, infertility, and musculoskeletal atrophy, and developmental hypoplasia have also been reported. Some of these late effects may not be life-threatening, but can negatively affect the quality of life of survivors. The following sections describe selected long-term complications and their associated risk factors.
Cumulative incidence of cause-specific mortality of long-term HL survivors.
Second malignancy
Second malignancy has been shown to be the leading cause of death among long-term HL survivors. The association between use of alkylating chemotherapy for HL therapy and leukemia risk was first recognized in the early 1970s. Over the years, the data on second malignancy after HL have accumulated, with solid tumors accounting for the majority of cases of second malignancy after HL. In addition, the relative risks remain significantly elevated at 25 years after initial HL diagnosis.1 Radiation therapy is a main contributor to solid tumors in HL survivors, although more recent data have linked alkylating chemotherapy to a variety of solid tumors, including lung cancer and gastrointestinal cancers.2-5 For selected second malignancies, sex, age at treatment, environmental exposures, and underlying genetic factors also contribute to the increased risks.6-8 Best et al showed 2 variants at chromosome 6q21 to be associated with subsequent malignant neoplasm in survivors of HL treated with radiation therapy as children but not as adults.6 Ma et al showed that genetic variation in FGFR2 influences breast cancer risk in HL patients treated with radiotherapy.8
Leukemia
Earlier studies showed an increased leukemia risk with the use of MOPP (mechlorethamine, vincristine, procarbazine, and prednisone) chemotherapy, and the use of large-field radiotherapy further contributes to the risk. The risk of leukemia from a combination of alkylating chemotherapy and radiation therapy was highlighted in the European Organisation for Research and Treatment of Cancer (EORTC) trial of MOPP/ABV (doxorubicin, bleomycin, vinblastine) with or without radiotherapy, in which the combined modality therapy arm had a significantly inferior survival outcome driven mostly by deaths due to leukemia.9
Modern chemotherapy with ABVD (doxorubicin, bleomycin, vinblastine and dacarbazine) does not appear to be leukemogenic. However, an increased leukemia risk is a concern with the more aggressive regimen of BEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, procarbazine, and prednisone)10 In the 10-year update of the German Hodgkin's Study Group (GHSG) H9 trial, the estimated 10-year cumulative incidence rate for acute myelogenous leukemia/myelodysplasia (AML/MDS) was lower for patients receiving COPP (cyclophosphamide, vincristine, procarbazine, prednisone)/ABVD (0.4%) compared with BEACOPP baseline (2.2%) and BEACOPP escalated (3.2%; P = .03). Both the alkylators and topoisomerase II inhibitors in some of these more modern regimens can contribute to the leukemia risk.11 Patients with treatment-related leukemia after HL have a poor prognosis. In a recent report from the GHSG on 106 patients diagnosed with AML/MDS after HL, the median overall survival for all AML/MDS patients was 7.2 months. However, for patients who received allogeneic stem cell transplantation, better outcomes were reported, with median overall survival not reached after 41 months of median follow-up (P < .01).10
Breast cancer
The majority of data on breast cancer after HL were in women treated with full mantle radiotherapy to doses of 40-44 Gy. The latency to breast cancer development is 10-15 years or longer. Multiple studies have shown that the significantly increased risk is seen mostly in women irradiated at a young age (30 or younger). Exposure to alkylating chemotherapy and/or pelvic radiotherapy have a protective effect against breast cancer in HL survivors, suggesting that hormonal milieu plays in important modifying effect on the breast cancer risk. Several case-control studies showed that estimated prior radiation doses to the specific area where the breast cancer developed, compared with doses to a similar area in the controls, showed a clear radiation dose-response relationship on breast cancer development. In the largest study that included 120 cases of breast cancer after HL and 266 controls, the relative risk of breast cancer increased significantly with increasing radiation dose, reaching 8-fold at the highest dose category (median dose 42 Gy) compared with the lowest dose group (<4 Gy; P < .001 for trend).12 Using the same dataset, Travis et al estimated the cumulative absolute breast cancer risk for young women treated for HL.13 For patients treated at age 25 years with a chest radiation dose of at least 40 Gy without alkylating agents, the estimated cumulative absolute risks of breast cancer by age 35, 45, and 55 years were 1.4%, 11.1%, and 29.0%, respectively. Several studies have demonstrated a direct correlation between breast cancer risk and radiation field size14-17 and also showed that smaller fields and treatment volume are associated with a significantly lower risk of breast cancer. In a population-based study comparing outcome of de novo breast cancer versus breast cancer after HL, women with localized breast cancer after HL had a significantly increased 2-fold risk of death from breast cancer compared with patients with de novo breast cancer.18 This finding could be explained by a greater prevalence of contralateral breast cancer in HL survivors, potential differences in the biology of breast cancers after HL, and limitations in treatment options for breast cancer after HL due to prior treatment exposures. The latter supports the importance of early breast cancer detection in women with history of chest irradiation for HL.
Lung cancer
Both radiotherapy and alkylating chemotherapy contribute to the risk of lung cancer after HL.5 The risk of lung cancer is directly related to radiation dose, as shown in a case-control study in which patients who received a dose of 30 Gy or higher had a 7- to 9-fold higher lung cancer risk compared with those who received <5 Gy to the area of the lung in which the cancer developed (P < .001 for trend).19 Similarly, a significant correlation between number of cycles of alkylating chemotherapy for HL and lung cancer risk has also been demonstrated.19,20 Tobacco use further contributes to the risk of lung cancer in a multiplicative manner.19 Prognosis of lung cancer after HL is dismal, with a median survival of <1 year. A population-based study found that lung cancer cases after HL are associated with a 30%–60% lower overall survival compared with de novo lung cancer.21 It is unclear whether this is due to more aggressive biology in treatment-related lung cancer and/or to more limited treatment options in HL survivors due to prior treatment exposures.
Gastrointestinal cancer
There are increasing data on gastrointestinal cancer, including esophageal cancer, pancreatic cancer, stomach cancer, and colorectal cancer, after HL therapy. Case-control studies have shown a significant radiation dose-response relationship for the development of stomach cancer in HL survivors.2,4 In a population-based study, it was found that HL patients who develop cancer of the transverse colon and stomach experience significantly reduced survival compared with patients with de novo cancers.22 In addition to radiotherapy, several chemotherapeutic agents, including procarbazine, platinum, and dacarbazine, are associated with an increased risk of gastrointestinal cancer in a dose-related manner.2-4
Cardiovascular disease
Mantle-field radiation therapy leads to an increased long-term risk of a wide range of cardiovascular complications, including coronary artery disease, valvular disease, pericardial disease, arrhythmia, and cardiomyopathy. The increased risk typically emerges after a latency of 10 years and remains persistently elevated over time. In addition, it is a key contributor to the excess mortality seen in long-term HL survivors. The risk of cardiac disease is directly related to radiation doses.23,24 In a study of 1132 pediatric HL survivors treated on 5 consecutive German-Austrian pediatric trials, the 25-year cumulative incidence of cardiac disease in the group with a mediastinal radiation dose of 36 Gy was 21% and the risk decreased significantly to 10%, 6%, 5%, and 3% in those with lower mediastinal radiation doses of 30, 25, 20, and 0 Gy, respectively (P < .001).23 On multivariable analysis, mediastinal radiation dose was the only significant factor predicting for cardiac disease-free survival (P = .0025).
The cardiotoxicity of anthracycline is well documented, with clinical manifestations of decreased systolic function, dilated cardiomyopathy, and congestive heart failure. The risk is related to the cumulative anthracycline dose, but a significantly increased risk of congestive heart failure is observed even after cumulative doses of <240 mg/m2.25 Specific to HL survivors, exposure to ABVD has been shown to contribute to increased cardiac mortality.26 In a study by Swerdlow et al on myocardial infarction mortality risk of HL survivors, among 385 patients treated with ABVD, the standardized mortality ratio of those treated with chest radiotherapy was 12.1 (P = .004). The risk was lower among those who were treated with ABVD without chest radiotherapy, but was still significantly elevated at 7.8-fold higher than that of the normal population (P = .01).
Several studies have demonstrated that traditional cardiac risk factors, including hypertension, hypercholesterolemia, and smoking further, contribute to the risk of cardiac disease in HL survivors.27-30 In a population-based study from Ontario, Canada, preexisting heart disease was the most significant predictor for post-HL therapy cardiac complications,29 with a hazard ratio of 3.98 (P < .001) on multivariable analysis.
An increased risk of noncoronary atherosclerotic vascular disease and a 2- to 5-fold increased risk of stroke have been demonstrated in survivors of HL after mantle irradiation.31,32 The absolute risk, however, appears to be low. In one study, the incidence of stroke after mantle irradiation for HL was estimated 109.8 per 100 000 person-years, or 0.1% per person per year.31 The risk was significantly associated with radiation dose27 and history of hypertension, diabetes mellitus, and hypercholesterolemia.27,32
Endocrinopathies
HL survivors can develop a variety of endocrinopathies after therapy. The risk of hypothyroidism is as high as 60% after neck irradiation.33 The risk appears to be higher among pediatric HL survivors. In a study evaluating the relationship between radiation doses to the thyroid gland and the risk of hypothyroidism, a significant dose-volume effect was found. The risk of developing hypothyroidism was 11.5% if the percentage of the thyroid gland receiving 30 Gy (V30) was 62.5% or lower, whereas the risk was 70.8% if the thyroid gland V30 was >62.5% (P = .0001).34
Several types of HL therapy can result in sterility, including pelvic radiotherapy and exposure to alkylating chemotherapy regimens such as MOPP (mechlorethamine, vincristine, procarbazine, and prednisone), the historical regimen for HL. Both escalated and baseline BEACOPP, regimens developed by the GHSG for patients with advanced HL, are associated with a risk of azoospermia in over 90% of male HL patients.35 Half of women who received escalated BEACOPP reported continuous amenorrhea in one study, and the risk is significantly associated with advanced-stage disease, age over 30 at treatment, and lack of oral contraceptive use during treatment. However, the risk of amenorrhea was lower with baseline BEACOPP.36 Although modern chemotherapy regimens for HL, including ABVD and Stanford V, do not appear to affect patient fertility,37,38 in patients with relapsed or refractory disease, salvage therapy will be associated with a significant risk for loss of fertility. Fertility preservation should therefore be discussed with all patients of child-bearing age and referral to reproductive endocrinology and semen or oocyte cryopreservation options should be offered to patients accordingly.
Developmental hypoplasia/musculoskeletal atrophy
Radiation therapy can have a long-term effect on musculoskeletal growth in children in an age- and dose-related manner, especially after radiation doses of >20 Gy. This led to the early adoption of lower doses of radiation therapy for pediatric HL. In addition to its effect on growth in children, radiation therapy can also cause cervicoscapular muscle atrophy and weakness, also known as dropped-head syndrome, in both children and young adults. It is a rare form of delayed complication, manifesting decades after exposure to high-dose mantle-field radiotherapy.39 It is characterized by weakness of neck extensor muscles resulting in an inability to extend the neck and a posture with the head flexed. The pathophysiology is unclear, but is thought to result from a combination of primary muscle damage and nerve damage. This debilitating rare late effect appears to be irreversible. Management is limited to supportive care including use of braces or cervical collar to maintain the patient's head in an upright position.
Evidence on screening and prevention strategies in HL survivors
Although much has been published outlining the risks and risk factors of late effects after HL, relatively limited data are available on the effectiveness of routine surveillance and/or prevention strategies. Most of the current screening recommendations on HL survivors are based on their increased risk pattern over time. The following summarizes available data on early intervention of selected late effects after HL.
Breast cancer
Prior studies have shown that implementation of mammography screening led to a stage shift, with more breast cancers diagnosed at earlier stages in female HL survivors. The addition of breast MRI as an adjunct to mammogram in these patients has been shown to improve the sensitivity of breast cancer detection. In a study on female HL survivors treated with chest radiotherapy at age 35 or younger who were at least 8 years out from treatment, the sensitivities for breast cancer detection with mammogram alone and breast MRI alone were 68% and 67%, respectively, but the 2 screening modalities together resulted in a sensitivity of 94%.40 Importantly, 94% of the screen-detected breast cancer cases were either pre-invasive or node-negative subcentimeter disease. In comparison, in a study based on the Surveillance, Epidemiology, and End Results (SEER) program on 298 HL survivors who developed breast cancer, only 63% were diagnosed at a localized stage.18
With the known increased risk of breast cancer in women who had received prior chest irradiation, risk-reduction strategies are being explored. An ongoing National Cancer Institute–sponsored prospective randomized trial is evaluating the use of low-dose tamoxifen as chemoprevention in these women, with mammographic density as a surrogate end point for breast cancer risk.
Lung cancer
The National Lung Screening Trial (NLST) demonstrated a survival benefit to low-dose computed tomography (CT) screening for patients aged 55-74 years with a ≥30 pack-year smoking history. However, this study did not specifically address cancer survivors at risk for developing lung cancer. A retrospective study analyzing lung cancer after HL showed that patients with lung cancers that were incidentally detected by imaging had a significantly higher median survival than patients with symptomatic disease at diagnosis.41 A cost-effectiveness analysis using Markov modeling, recently updated to include male and female survivors treated for HL at ages 25 and 35, found that low-dose CT screening is cost-effective only among survivors with a tobacco history.42 The optimal timing of initiating screening ranged from 6 to 15 years after treatment, depending on the age at treatment, sex, and radiation field and dose received.
Cardiovascular disease
Several prospective studies have evaluated the role of cardiac screening in HL survivors with history of mantle irradiation. The largest cardiac screening experience is from Stanford University on 294 asymptomatic HL survivors who had received mantle radiation therapy to a median dose of 44 Gy.43 Patients prospectively underwent resting ECG, stress echocardiogram, and radionuclide perfusion imaging. Coronary angiography was performed at the discretion of the physician based on ECG or stress echocardiogram findings. The prevalence of significant valve disease, coronary artery disease (CAD) with ≥50% stenosis, and CAD with ≥70% stenosis was 29%, 7.4%, and 5.5%, respectively. In addition, the prevalence of valvular disease, regional wall motion abnormality, and pericardial disease increased with increasing follow-up time.
Another prospective cardiac screening study was conducted at the Dana-Farber Cancer Institute on 182 asymptomatic HL survivors treated to a median mantle dose of 39.6 Gy.30 Resting and stress echocardiogram were performed at the time of screening, with further cardiac workup as indicated. Moderate valvular disease was detected in 8.8% of patients. The prevalence of >70% stenosis CAD was 4.4%. Moreover, prospectively measured blood pressure and high-sensitivity C-reactive protein at the time of screening were significantly associated with screen-detected CAD or valve disease. Every 5-mm Hg decrease in systolic or diastolic blood pressure was associated with a respective 22% or 26% decrease in the likelihood of CAD or valve disease, highlighting the importance of tight blood pressure monitoring and control in HL survivors.
In addition to blood pressure management, HL survivors may also benefit from screening for other traditional cardiac risk factors, including lipid screening. Guidelines for frequency of screening vary (discussed in the sections below) because of limited available data specific to cancer survivors at risk for cardiovascular disease due to treatment history. In a cost-effectiveness analysis on lipid screening for survivors of HL, lipid screening at 1-, 3-, 5- and 7-year intervals were cost-effective relative to a strategy of no screening.44 However, comparing screening intervals, a 3-year interval was the most cost-effective.
Modern treatment and implications on late effects
It is important to recognize that many of the reported late effects in HL survivors are based on patients treated with chemotherapy regimens and radiotherapy fields and doses that are no longer used in the present day. With increasing recognition of late effects of HL, the focus in recent years in the management of HL has been treatment reduction and modification to reduce the use of treatments that have been identified as culprit of late effects. Changes include replacement of MOPP by ABVD; elimination of radiation therapy (with more recent trials exploring omitting radiation therapy based on early positron emission tomography response45 ); and reduction of radiation volume from the historical extended field that included a full mantle field encompassing the submandibular, cervical, supraclavicular, infraclavicular, axillary, mediastinal, subcarinal, and hilar lymph nodes matched to an abdominal and splenic field to involved-field and, most recently, to involved-node/involved-site radiotherapy.46 Radiotherapy technique has evolved from rudimentary 2D planning to 3D planning with modern image guidance, techniques, and maneuvers to spare doses to lungs, heart, and breasts in a mediastinal field, including deep-inspiration breath hold techniques, inclined board, and intensity-modulated radiotherapy with “butterfly” technique. Radiobiological modeling studies have been conducted to estimate the reduction in risk of second malignancy and cardiovascular disease using involved-node radiotherapy and lower doses of radiation therapy,47 showing a several-fold reduction in the risks with modern radiotherapy volume and doses. Some of the follow-up recommendations summarized in the next section may not apply to HL patients treated in the contemporary era because of the anticipated lower risk of complications. However, because of the inherent uncertainties associated with modeling studies, long-term follow-up studies of modern treatments are needed to ascertain their true long-term risks.
Current follow-up recommendations
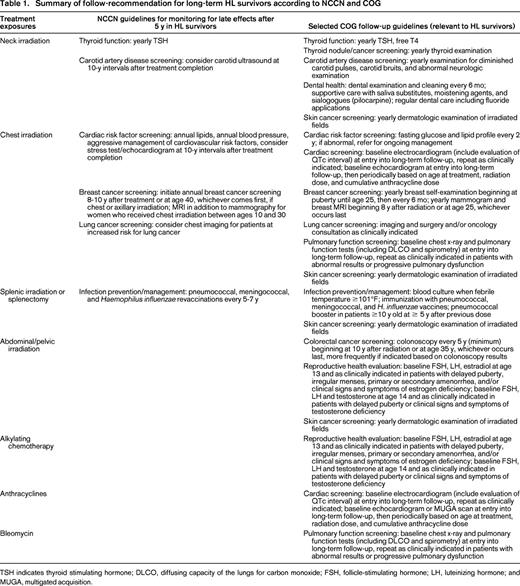
Multiple cancer survivorship guidelines exist, with several focusing on HL survivors. The National Comprehensive Network (NCCN)48 and Childhood Oncology Group (COG)49 provide key follow-up guidelines for adult and pediatric cancer survivors, respectively. The NCCN provides guidelines for monitoring for late effects specifically for HL survivors 5 years after initial treatment. Conversely, the COG provides recommendations according to specific treatment exposures and potential impact to body sites, rather than according to initial cancer type. Many of the COG follow-up guidelines, however, could be pertinent to HL survivors. Table 1 summarizes the NCCN guidelines for monitoring for late effects for HL survivors after 5 years and selected recommendations from the COG follow-up guidelines that may be of particular relevance to HL survivors based on typical HL treatment exposures.
There are some differences between the recommendations of the 2 guidelines, in part reflecting the different late effect concerns in patients treated as a child versus as an adult. There are also some variation in specifics of screening recommendation, which may be due to the lack of data on the efficacy of types and timing of screening tests. For example, for lipid screening, the NCCN recommends annual testing, whereas the COG recommends testing every 2 years. Colorectal cancer screening was addressed in the COG but not the NCCN guidelines, likely due to the lack of data on the efficacy of colorectal cancer screening in the HL population.
The NCCN recommends initiating annual breast cancer screening 8-10 years after treatment or at age 40, whichever comes first, if there is a history of chest or axillary irradiation, and the addition of breast MRI to mammography for women who were irradiated between ages 10 and 30. In the recent report from the International Late Effects of Childhood Cancer Guideline Harmonization Group, which graded the recommendations according to the strength of the underlying evidence, a strong recommendation was made for annual mammography, breast MRI, or both in women who had received chest irradiation to doses of 20 Gy or higher, starting at age 25 or 8 years after treatment, whichever occurs last.50
Both the NCCN and COG guidelines discussed consideration of chest imaging for lung cancer screening in high-risk patients or as clinically indicated. The type of chest imaging, timing, and frequency were not detailed, again likely due to the paucity of data on the efficacy of lung cancer screening in the HL population. In the previously discussed cost-effectiveness analysis on low-dose chest CT screening in HL survivors, the model assumed yearly screening.42
Other important follow-up recommendations, including dermatologic examination for skin cancer screening in irradiated patients and reproductive health evaluation including as-needed follicle-stimulating hormone, luteinizing hormone, and estradiol or testosterone testing in patients exposed to pelvic irradiation or alkylating chemotherapy, were addressed in the COG guidelines. Annual dermatologic examination may be especially important in the HL population due to the known increased skin cancer risk after radiation exposure. In a recent Dutch report on 889 HL patients treated between 1965 and 2005,51 318 skin cancers were diagnosed in 86 patients, with 93% of the skin cancers being basal cell cancer. The basal cell cancer risk was significantly increased at 5.2-fold in the HL survivors compared with the normal population, with 57% of the skin cancers developing within the prior radiation field.
The NCCN addressed these issues in more general terms, including “counseling on reproduction, health habits, psychosocial, cardiovascular, breast self-examination, and skin cancer risk.” In addition, regardless of treatment exposure, the NCCN recommends annual interim history and physical examination, annual complete blood counts, platelets, chemistry profile, and annual influenza vaccine in HL survivors.
Future directions
The management approach to HL has evolved considerably over the last 5 decades. Although patients with newly diagnosed HL will receive modern chemotherapy and radiotherapy that are likely to be associated with reduced late effects, there are still a large number of HL patients who were cured years ago and are in need of follow-up guidance. More data are needed to confirm the efficacy of screening and prevention strategies, including types of screening tests, timing, frequency, and target survivor population. Further work on genetic susceptibility to developing late effects of treatment can help to guide initial treatment decision and allow targeted and tailored follow-up of survivors.6,8 Additional research efforts on correlating radiation dosimetric parameters of specific organs with late effects would improve our understanding of the relationship between radiation dose-volume and long-term risks and guide future radiation treatment planning.24,34 There are emerging data on an association between anthracyclines and, not just cardiac risk, but also solid tumors, and further follow-up is needed to confirm the findings.52 Finally, as new targeted agents are adopted for HL, their long-term risks need to be fully assessed.
This article was selected by the Blood and Hematology 2014 American Society of Hematology Education Program editors for concurrent submission to Blood and Hematology 2014. It is reprinted with permission from Blood 2014, Volume 124.
Disclosures
Conflict-of-interest disclosure: The author declares no competing financial interests. Off-label drug use: None disclosed.
Correspondence
Andrea K. Ng, Department of Radiation Oncology, Brigham and Women's Hospital, 75 Francis St, Mailstop ASB1-L2, Boston, MA 02115; Phone: (617) 732-6310; Fax: (617) 732-7347; e-mail: ang@lroc.harvard.edu.