Abstract
Iron deficiency and iron deficiency anemia are common conditions worldwide affecting especially children and young women. In developing countries, iron deficiency is caused by poor iron intake and/or parasitic infection, whereas vegetarian dietary choices, poor iron absorption, and chronic blood loss are common causes in high-income countries. Erythropoiesis stimulating agents can result in functional iron deficiency for erythropoiesis even when stores are iron-replete. Diagnosis of iron deficiency is straightforward, except when it occurs in the context of inflammatory disorders. Oral iron salts correct absolute iron deficiency in most patients, because low hepcidin levels facilitate iron absorption. Unfortunately frequent side effects limit oral iron efficacy. Intravenous iron is increasingly utilized, because currently available preparations allow rapid normalization of total body iron even with a single infusion and are effective also in functional iron deficiency and in iron deficiency associated with inflammatory disorders. The evidence is accumulating that these preparations are safe and effective. However, long-term safety issues of high doses of iron need to be further explored.
Learning Objectives
To diagnose absolute iron deficiency, iron deficiency anemia, and functional iron deficiency in the light of recent advances in iron metabolism
To evaluate advantages and disadvantages of oral and intravenous iron therapy
Disorders of iron metabolism are common human pathologic conditions. Iron deficiency, defined as low body iron with or without anemia, is estimated to affect >2 billion people. Iron deficiency anemia is the most prevalent anemia worldwide roughly affecting 1 of 8 persons, with the highest prevalence in developing countries.1 Still iron deficiency anemia often remains undiagnosed and untreated.
Iron is tightly regulated at both the cellular and systemic level. Systemic iron homeostasis is under the control of hepcidin and is dominated by the erythropoietic needs for hemoglobin synthesis.2 Thus, individuals at increased risk of developing iron deficiency are young children and adolescents, because of expanding erythropoiesis during rapid growth, and postpartum women. Also regular blood donors may develop iron deficiency and anemia after multiple donations.3 Insufficient iron intake, diets containing poorly bioavailable sources of iron, and parasitic infections account for most cases in low-income countries.1 In high-income countries, iron deficiency anemia, usually with the exception of groups with increased iron needs, may point to pathologic conditions associated with poor iron absorption and/or chronic blood loss.
A vast literature primarily based on observational studies indicates that iron deficiency anemia may have a detrimental effect on cognitive development in children, on physical performance and work productivity in adults, and result in unfavorable pregnancy outcomes. In addition, the direct effect of iron deficiency on tissues other than erythropoiesis (as muscles, heart, and brain) even in the absence of anemia is a matter of a debate in view of the potential benefit of correcting tissue iron deficiency.
The laboratory diagnosis of iron deficiency anemia is well established, except when it occurs in patients with chronic infections/inflammation. In these cases, the increased cytokines and hepcidin levels cause body iron maldistribution that confounds the diagnostic parameters. The diagnostic approaches and the differential diagnosis of iron deficiency anemia, as well as the different strategies to supplement iron, are reviewed in light of our improved knowledge of the regulation of iron homeostasis.
Mechanism of adaptation to iron deficiency
Iron deficiency anemia usually develops slowly. As iron levels decline in the stores (iron deficiency) and in the circulation (iron restricted erythropoiesis) becoming insufficient for the full hemoglobinization of mature erythroblasts (iron deficiency anemia), the liver peptide hormone hepcidin is transcriptionally suppressed.4 Indeed serum hepcidin levels are significantly lower in young women with a negative iron balance compared with males and postmenopausal women, and are even undetectable in serum of individuals with iron deficiency anemia.5,6 The decrease of hepcidin enhances iron release into plasma through ferroportin from both enterocytes and macrophages in the attempt of maintaining normal transferrin.
Animal models have clarified the compensatory mechanisms used to supply iron to erythropoiesis. In the initial phases of iron deficiency erythropoietin is reduced by the IRP1–mediated repression of hypoxia inducible factor-2 (HIF-2α) translation, to balance erythropoiesis with the limited iron availability.7,8 Decreased di-ferric transferrin, the ligand of both transferrin receptors (TFR1 and TFR2) not only impairs cell iron uptake by erythroid TFR1,2 but also destabilizes the iron sensor TFR2 on both the hepatocyte2 and erythroid cell surface.9 Whereas this contributes to hepcidin suppression in hepatocytes, it disrupts the TFR2-erythropoietin receptor interaction in erythroid cells with the resulting increased erythropoietin sensitivity.9 This translates into decreased apoptosis and an increased number of erythroblasts, optimizing the use of the available iron to produce microcytic red cells.9 This moderate erythropoiesis expansion increases the hepcidin inhibitor erythroferrone.9,10 At the same time, the transmembrane protease TMPRSS6 is stimulated in iron deficiency in order to attenuate the BMP-SMAD signaling and to repress hepcidin synthesis.11 These mechanisms cooperate to sustain iron concentrations ensuring effective erythropoiesis, while at the same time avoiding excessive restriction of iron to other cells. Degradation of the storage protein ferritin occurs through “ferritinophagy”, an autophagy process carried out in starvation through NCOA4, a newly identified cargo protein, which targets ferritin to lysosomes for degradation.12 Whether this is important to recycle iron when cell iron is limited is an issue of great interest. Once iron deficiency has led to overt anemia, HIF-2α increases erythropoietin production in the kidney and enhances the expression of the iron importer DMT1, the iron reductase DCYT-B, and the iron exporter ferroportin in duodenal enterocytes.13
Traditional and emerging causes of iron deficiency
Groups of individuals at risk and traditional causes of iron deficiency and iron deficiency anemia are well known, summarized in Table 1 and will not be extensively discussed here. For thorough coverage the readers are referred to a recent review.14
Impaired iron absorption may result from surgical and medical conditions. Bariatric surgery, increasingly performed to control caloric intake or diabetes, is emerging as a potential cause of iron deficiency.15 Post-operative iron deficiency is influenced by preoperative iron status, which is often low in obese patients, and is found more commonly in females. Medical disorders affecting the gastrointestinal tract (eg, rarely autoimmune atrophic gastritis, more frequently Helicobacter pylori gastritis and celiac sprue) impair iron absorption and lead to resistance to oral iron treatment.16,17 In inflammatory bowel diseases iron deficiency may be due to both poor absorption and blood loss. A functional reduction of iron absorption secondary to high hepcidin and ferroportin degradation may occur in these disorders, as well as in any other chronic inflammatory conditions. Iron deficiency is increasingly reported in the inflammatory setting, a combination that is challenging for diagnosis and relevant for treatment. This problem is exemplified by anemia of chronic kidney disease, which is due to blood loss, especially at dialysis, enhanced hepcidin levels (because of increased production and reduced excretion) and treatment with erythropoiesis stimulating agents (ESAs).18 These agents may induce an imbalance between increased iron requirement and insufficient iron mobilization from stores, especially when hepcidin levels are elevated, leading to functional iron deficiency. Iron deficiency is increasingly reported in patients with heart failure,19 and may be a component of anemia in cancer patients and in the elderly, when associated with inflammation, low erythropoietin, and often multiple medications. Mild iron deficiency anemia is present in severely obese subjects, because of low-grade inflammation, increased hepcidin levels, and reduced iron absorption.14
Genetics and iron deficiency
Genetic forms of iron deficiency anemia are extremely rare. Iron-refractory-iron-deficiency anemia (IRIDA) is a recessive anemia caused by mutations in the transmembrane protease serine member 6 (TMPRSS6) gene, which encodes the liver protease that inhibits hepcidin transcription by cleaving the coreceptor of the BMP-SMAD pathway hemojuvelin.11 High hepcidin levels in IRIDA patients limit iron release to plasma from absorption sites and stores, leading to a microcytic hypochromic anemia that is unresponsive to oral iron.20 Such a disorder is usually suspected in children or young patients whose anemia is persistent and refractory to oral iron treatment, in the absence of gastrointestinal conditions that limit iron absorption.17 IRIDA has raised interest in the identification of genetic susceptibility to iron deficiency. Genome Wide Association Studies, including a recent meta-analysis, indicate that TMPRSS6 genetic variants associate with red cell and iron traits in Caucasian and Asian populations.21-23 The most common associated TMPRSS6 variant (rs855791, A736V) influences serum hepcidin levels.24
The genetic susceptibility to iron deficiency is of special interest for transfusion medicine because it has implications for blood donation. Blood donors, especially females, carriers of the allele (736A) of the TMPRSS6 variant rs855791 associated with low hepcidin levels,24 seem more resistant to the development of iron deficiency after blood donation as compared to blood donors with the high-hepcidin associated variant.25 Male donor carriers of a common polymorphism (P582S) in HIF-1α, which influences protein stabilization and thus the response to hypoxia, were found to have higher hemoglobin and ferritin levels and were protected from iron deficiency following blood donations compared with donors homozygous for the wild-type allele.25 These pilot studies indicate the need for further investigation with the aim of improving blood donor health, controlling iron deficiency, and personalizing blood donations.
Laboratory diagnosis of iron deficiency and iron deficiency anemia: iron parameters
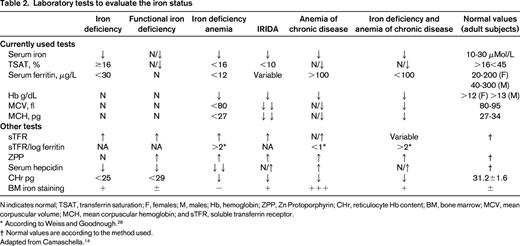
Serum ferritin <30ng/mL is the most sensitive and specific test to identify isolated iron deficiency,26 as it reflects low stores (Table 2). In the progression of the deficiency, because of low iron and increased transferrin synthesis, transferrin saturation (or the saturated iron binding capacity) drops <16%, di-ferric transferrin, the ligand of transferrin receptor, is reduced and iron supply to the bone marrow becomes insufficient. At this point serum ferritin is usually <12 ng/mL.4 In parallel, soluble transferrin receptor is shed in the circulation by the proprotein convertase subtilisin/kexin 7 (PCSK7), which cleaves the receptor when unbound to its ligand.27
Both transferrin saturation and serum ferritin are consensually decreased in iron deficiency anemia. Transferrin saturation may also be decreased in the anemia of chronic inflammation, but ferritin levels are increased, reflecting macrophage iron sequestration. In addition, transferrin and soluble transferrin receptor are not increased in inflammation. Although the distinction of iron deficiency anemia from anemia of chronic disease is straightforward, there is no clear-cut test that diagnoses iron deficiency anemia in the setting of inflammation (Table 2). Low transferrin saturation is one criterion with ferritin levels empirically set at <100 ng/mL28 or higher (<300 ng/mL) as in chronic kidney disease or in heart failure.14 Other proposed tests, such as the levels of serum soluble transferrin receptor (increased in iron deficiency and normal/low in inflammation) or the ratio between soluble transferrin receptor and log ferritin levels,28 are uncommonly used in clinical practice.
Perl's iron staining of bone marrow smears allows visualization of the absence of iron in both macrophages and erythroblasts in iron deficiency; the presence of iron in macrophages but not in erythroblasts occurs in anemia of chronic inflammation. Once the gold standard for the diagnosis of iron deficiency, Perl's staining is rarely assessed because it is qualitative and requires performance of an invasive procedure.4 In general the combination of tests rather than a single test helps to ascertain the correct diagnosis (Table 2).
In IRIDA, a discrepancy is often observed with extremely low transferrin saturation levels and normal/borderline low serum ferritin levels. Iron parameters differentiate IRIDA from other microcytic anemias,29 and a normal C-reactive protein level from anemia of inflammation. Measuring serum hepcidin might be useful in IRIDA, because levels are abnormally high (or normal but inappropriately high)30 considering the iron deficiency. At present, hepcidin assays are used for research but are not widely available for diagnostic purposes.
Laboratory tests: erythrocyte traits
Low mean corpuscular volume and mean corpuscular hemoglobin are typical of iron deficiency anemia. Red cell distribution width (RDW), a measure of variation of red cell volume is increased, especially in the initial phases of iron deficiency when newly produced small hypochromic red cells coexist with normal ones. The RDW is also increased after iron therapy that induces the production of better hemoglobinized cells in the context of the array of hypochromic microcytic ones. RDWs, as well as erythrocyte indexes, are not affected in anemia of chronic inflammation. The differential diagnosis of microcytic anemia has been recently reviewed.29
Decreased reticulocyte hemoglobin content, a parameter that measures the functional iron available for erythropoiesis over the previous 3-4 days, is an early sign of iron-restricted erythropoiesis, (eg, after treatment with ESA). On the other side its increase is a measure of an early (2-4 days after treatment start) response following intravenous iron therapy. The percentage of hypochromic red cells is less useful because it is not as early a sign as the reticulocyte hemoglobin content.26
Lack of iron affects the last step of heme synthesis leading to accumulation of protoporphyin IX and incorporation of zinc instead of iron in the protoporphyin ring. Increased red cell zinc protoporphyrins may be used as a screening test for iron deficiency. However, protoporphyrins may increase also in the rare sideroblastic anemias due to defects of enzymes in the heme synthetic pathway.
Searching for the etiology of iron deficiency
Except when iron deficiency is clearly related to increased requirements, patients should be evaluated for the cause(s) of iron deficiency, usually gastrointestinal blood loss, or poor iron absorption. A gastrointestinal work-up should be undertaken to identify a source of blood loss and video capsule endoscopy may be useful in cases with negative conventional endoscopy to explore the small bowel as a source of occult bleeding. Aggressive work up is recommended in iron deficient men and postmenopausal women. Gynecologic evaluation is mandatory in females with heavy uterine bleeding.
Non-invasive tests such as the urea breath test or antibodies for Helicobacter pylori and anti-transglutaminase antibodies for celiac sprue are indicated after failure of oral iron treatment, even in young patients.17 C-reactive protein and a search for inflammatory/neoplastic conditions are especially relevant in the elderly, because, besides dietary deficiency, multiple causes are possible including clonal hematopoiesis. In rare instances paroxysmal nocturnal hemoglobinuria, as well as other causes of chronic intravascular hemolysis, should be searched for in unexplained cases of iron deficiency.
Sequencing of the TMPRSS6 gene is essential when suspecting IRIDA.30
Therapeutic options
Oral iron supplementation
Oral iron supplementation is the first line of treatment of iron deficiency anemia. Protocols for dosing and duration of treatment are well defined. Anemic adult patients are ideally treated with iron salts containing 100-200 mg elemental iron administered in divided doses fasting. Lower doses may be used with fewer side effects in individual patients. Children require liquid preparations (3-6 mg/Kg). The gold standard of oral iron treatment is ferrous sulfate; other effective compounds are iron fumarate, gluconate, carbonyl iron, and polysaccharide-iron complex. Slow release iron preparations should be avoided, because iron release occurs beyond the duodenum, which is the site of maximal absorption. However, oral iron is not easily tolerated. Dyspepsia, nausea, vomiting, abdominal pain, constipation, or diarrhea, likely due to the oxidative properties of iron on the gastrointestinal mucosa, occur frequently, especially when iron is taken fasting. A recent meta-analysis of randomized controlled trials has shown that gastrointestinal side effects are more common with oral iron compared with placebo or intravenous iron.31 For this reason, few patients fully adhere to the prescribed dose for the entire duration of treatment that should last 3-6 months in order to replenish iron stores. Iron administration with meals or dose reduction may increase tolerance. Interference by diet and drugs of common use (eg, antacids, H2 blockers, and proton pump inhibitors) may also reduce pharmacologic iron absorption.
Oral iron is effective in correcting anemia; however, results of the same treatment on the reversal of iron deficiency in other tissues are controversial. Few studies suggest that fatigue and quality-of-life improve in iron-deficient non-anemic females treated with oral iron. However, the studies are small, heterogeneous in design, and not always unbiased.32 Iron supplementation in very young preschool children living in low-income areas may correct anemia, but a large meta-analysis of randomized trials failed to find evidence of improved cognitive performance or positive effect on growth and development.33 In endemic malarial areas iron supplementation raises the concern of increasing parasitemia or even clinical malaria.34 Additional well-designed studies are needed to define the benefits/risks of iron supplementation in low-income countries.
Low-dose (37.5 mg) oral iron supplementation used to prevent iron deficiency in blood donors with normal hemoglobin levels, compared with no supplementation, showed a reduced time to recover the post-donation decrease in Hb concentration irrespective of basal ferritin levels.35
Anemic patients with malabsorption, Helicobacter pylori infection, atrophic gastritis, previous gastric or duodenal surgery, genetic IRIDA, as well as patients with elevated hepcidin levels driven by inflammation, do not respond or only partially respond to oral iron treatment. The use of oral iron is controversial in active inflammatory bowel disease. Eradication of Helicobacter pylori in infected patients or a gluten-free diet in asymptomatic celiac disease may normalize iron absorption.17
Intravenous iron: indications and controversies
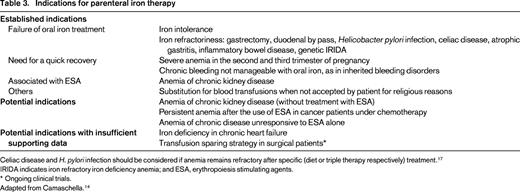
The only alternative to oral iron route is intravenous treatment. The intramuscular route has been abandoned because of the inconvenience of painful injection, dark discoloration of the skin, and development of sarcoma in the site of injection in treated animals. Intravenous iron is indicated when intestinal absorption is presumably poor, when rapid Hb increase is needed, as in severe anemia in the second to third trimester of pregnancy, or in chronic bleeding due to inherited defects, as in hereditary hemorrhagic telangiectasia (Table 3). With the intravenous route of administration, the exact dose of iron needed to normalize Hb levels and to replenish the stores can be calculated. Thus, it is not unexpected that hemoglobin response is better to intravenous than to oral iron, as documented in several studies.36
One drawback of intravenous iron has been the need for multiple infusions. However, some preparations on the market may replace the total dose needed to correct iron deficiency anemia (up to 1000 mg) in a single or a couple of infusions (Table 4).37 This approach reduces the number of clinic visits and may be quite useful in selected patients.
Intravenous iron is more effective than oral iron when combined with ESA in chronic kidney disease and may decrease the needs of these agents in dialysis patients18 ; uncertainty remains on the use of ESAs in the anemia of cancer patients undergoing chemotherapy.38
In rare cases of severe anemia of various etiologies, intravenous iron was used in combination with ESA in lieu of blood transfusions in Jehovah's witnesses, who refuse allogeneic human blood. Few studies have explored the use of parenteral iron in the preoperative setting.39 Although iron parameters in heart failure suggest iron maldistribution rather than iron deficiency, intravenous iron administration even in the absence of anemia has been shown to improve physical performances (6 minute walking test) and New York Heart Association functional class and quality-of-life, compared with placebo.40 The hypothesis that intravenous iron may correct cardiomyocyte iron deficiency is intriguing and needs to be further explored.
Intravenous iron is contraindicated in the course of infections, in the first trimester of pregnancy, and in patients with a history of iron or of other drug allergy.41
Immediate side effects of intravenous iron infusion may be nausea, vomiting, headache, flushing, myalgia, pruritus, arthralgia, and back and chest pain. Hypophosphatemia is usually transient and asymptomatic.
Hypersensitivity reactions, even anaphylactic shock, were reported with the use of high-molecular-weight iron dextran, whose use is now abandoned. Severe hypersensitivity reactions with the other preparations (Table 4) are exceptional. Simple recommendations to minimize the risk include slow administration with careful patient monitoring during and after treatment, an adequate clinical environment with trained staff and the avoidance of antihistamine premedication.41 Taking into account the ability of iron to generate oxidative stress and to increase susceptibility to infections36 the long-term side effects of large amounts of iron administered when iron stores are not depleted (eg, in inflammation) remain to be verified.
Conclusion
Oral iron remains the mainstay of therapy for most patients with iron deficiency. However, the optimal mode of iron supplementation depends on several factors related to both the patient and the type of drug. Factors to be considered include the underlying pathologic condition, the degree of anemia, the need for a rapid Hb increase, tolerability or refractoriness to previous treatments, history of allergy, drug cost, and side effects. When planning to administer a large iron dose in a single infusion the risk–benefit ratio should be evaluated, considering that the long-term effects of large iron doses remain uncertain with respect to iron overload, oxidative stress, and susceptibility to infections.
Correspondence
Clara Camaschella, Vita Salute University, San Raffaele Scientific Institute, Via Olgettina 58, 20132 Milano, Italy; Phone: +39-0226437782; Fax: +39-0226434723; e-mail: camaschella.clara@hsr.it.
References
Competing Interests
Conflict-of-interest disclosure: The author declares no competing financial interests.
Author notes
Off-label drug use: None disclosed.