Abstract
Treating Hodgkin lymphoma by using chemotherapy with or without radiotherapy is highly successful, with substantially fewer deaths from lymphoma than from other causes in recent studies of both early-stage and advanced-stage disease. Long-term toxicity is a major consideration in this context, and recent trials have used functional imaging with [18F]fluorodeoxyglucose (FDG) positron emission tomography early in the course of treatment (interim PET) to assess response and modulate subsequent therapy. In early-stage disease, this has allowed omission of consolidation radiotherapy after a good response to doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) chemotherapy, and trials have shown that this can be done without detriment to overall survival, despite a small increase in rates of recurrence of ∼5%. Conversely, escalation to more intensive chemotherapy with bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone (BEACOPP) for those with positive interim PET scans seems to be an effective strategy with improved disease control. In advanced-stage disease, several groups have elected to start treatment with ABVD and escalate to BEACOPP or myeloablative therapy for patients who remain PET positive after 2 cycles, which gives rates of disease control of ∼65%. De-escalation by omission of bleomycin and consolidation radiotherapy after a negative interim PET scan seems safe with no increase in recurrence rate, but the performance of interim PET after ABVD is suboptimal, especially for those with very advanced disease at presentation; recurrence rates after a negative scan are ∼15%. The negative predictive value of PET is higher after escalated BEACOPP chemotherapy, and the approach of initially treating with BEACOPP and de-escalating to ABVD for those with negative interim PET scans shows promising early results. Response-adapted therapy has yielded important results for patients with Hodgkin lymphoma and is becoming established as a standard approach.
Learning Objectives
Understand the application and limitations of FDG-PET imaging in the early assessment of response to treatment in Hodgkin lymphoma
Understand the results of recent trials of response-adapted therapy in Hodgkin lymphoma and how they will influence clinical practice.
Introduction
The treatment of Hodgkin lymphoma (HL), originally with radiotherapy and subsequently with combination chemotherapy, has transformed the outlook for patients with this illness over the last 50 years. Patients with early-stage disease can expect to be cured in more than 95% of the cases, and even for patients with advanced-stage disease, the potential cure rate is more than 90%. The progressive rise in the probability of cure in a group of patients who most frequently present in the second or third decade of life has changed the calculus of therapy from a predominant focus on the eradication of the malignancy to a more complex assessment of interdependent considerations of the chance of cure and the risk of long-term adverse effects. The results of recent large-scale studies in both early-stage1 and advanced-stage2 HL indicate that the risk of death from disease is exceeded by the risk of death from other causes, notable among which are the toxic effects of therapy.
Apart from the readily acknowledged short-term adverse effects of therapy, such as nausea, myelosuppression, mucositis, and fatigue, survivors are at risk of a range of longer-term toxicities. The most serious of these include epithelial malignancies induced by radiotherapy,3 myelodysplasia and acute leukemia from extensive treatment with alkylating agents,4 accelerated coronary and valvular heart disease induced by mediastinal radiotherapy and anthracyclines,5 infertility caused by high doses of alkylating agents, and pulmonary fibrosis caused by bleomycin.6 The risks of such late toxicities have been reduced by a variety of measures since they were recognized 3 to 4 decades ago, and some measures have been effected without apparent loss of disease control. For example, reduction of radiotherapy fields from extended field to involved field radiotherapy (IFRT) and involved node radiotherapy (INRT) techniques7 has lowered the exposure of normal tissues to radiation with an attendant decrease in second cancers but without an increase in the rates of recurrence.8 In some situations, it has been possible to omit consolidation radiotherapy altogether, for example, in patients with advanced-stage disease in whom a complete response was seen at the end of chemotherapy.9 However, not all trials have shown equivalent efficacy for less intensive treatment. As an example, the German Hodgkin Study Group (GHSG) H11 trial in unfavorable-risk early-stage disease showed that reducing the dose of IFRT from 30 Gy to 20 Gy could only be done without loss of disease control if it was preceded by more intensive chemotherapy, in this case, bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone (BEACOPP) rather than doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD).10 Similarly, in advanced-stage disease, the probability of failure-free survival (FFS) after escalated BEACOPP (BEACOPPescalated) is higher than that after ABVD by ∼10% to 15%, although none of the trials directly comparing the two showed an overall survival (OS) difference, mainly because of different rates of salvage with second-line therapy.11,12 The management of HL in patients older than age 60 years poses another set of challenges, because intensification with BEACOPP is attended by unacceptable rates of treatment-related morbidity and mortality,13 and even ABVD is difficult to deliver because of the high rates of pulmonary toxicity in this group attributable to bleomycin exposure.
To summarize an extensive literature on the subject, it seems that for each risk group (early-stage favorable, early-stage unfavorable, advanced stage), there is a minimum threshold of treatment below which rates of durable remission begin to decrease, but it is not clear to what extent treatment intensification above this level is attended by further improvements in outcome, especially when the increased late toxicities of more treatment lead to increased mortality, thus offsetting the effect of better lymphoma control. The nonconcordance of FFS and OS is a feature of many studies in HL, partly owing to the successful use of second-line therapy, and partly owing to the long-term mortality increase after more intensive or extensive treatment, which benefits only a minority of the patients exposed to the risk if all are treated the same. One potential approach to this problem is the use of response-adapted therapy.
Principles of response-adapted therapy: choosing the test
The proposition behind response-adapted therapy is simple: measure the effect of treatment early in the course to distinguish those patients for whom the treatment is proving effective from those in whom it is failing and modify the treatment accordingly. Clearly this requires two elements: a test and the capacity to modify the treatment.
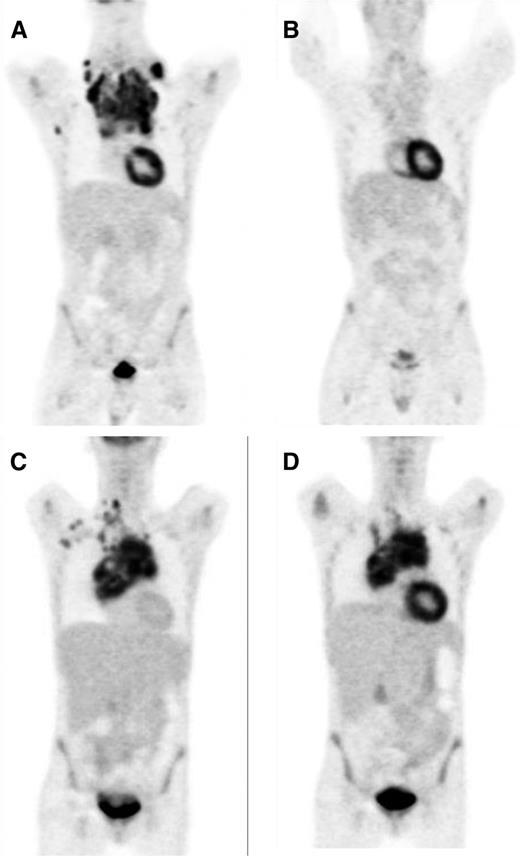
The test needs to be reliable, with a result that carries a strong correlation to the final outcome of treatment and with the ability to be performed relatively rapidly in order to guide decision making. Attempts to use conventional cross-sectional imaging or blood-based biomarkers have not yet proved to be effective in this context, but functional imaging, currently performed by using positron emission tomography (PET) with 2′-[18F]fluorodeoxyglucose (FDG) seems to meet the criteria, at least in part. The imaging is based upon the preferential uptake of labeled FDG by actively metabolizing tissues, among which are sites of involvement by active HL, although other tissues such as the myocardium, brain, kidney, liver, brown fat, regenerating bone marrow, and inflamed lung (or indeed any site of inflammation) also show significant FDG avidity (Figure 1). Uptake in brown fat is a particular problem among patients in their teenage and young adult years. Because of the numerous potential confounding factors and the need for a measure of interpretation in the assessment of FDG-PET scans, strict quality control is needed in acquiring the images, and a standardized method of reading the results has been developed.14 The 5-point Deauville scale (Table 1) uses comparison with normal physiologic uptake to grade abnormalities,15 and this has proved to be reproducible and broadly applicable in large series, with high concordance between local and central reviewers.16 The gradations of the scale allow the cutoff between positive and negative to be set differently according to the question being asked in a trial. Thus, if a high level of sensitivity is needed (eg, for de-escalation of therapy), the threshold can be set at the level of the mediastinal blood pool (score of 1 to 2 is negative), whereas for a study that requires the best positive predictive value for escalation of therapy, the threshold may be higher (eg, at the level of normal liver uptake) (score of 1 to 3 is negative). The 5-point scale is now incorporated into the standard response criteria for lymphoma.17
FDG-PET interim scans demonstrating negative and positive results. (A, C) Presentation scans showing uptake by HL. (B) Negative interim PET scan showing only physiological FDG uptake. (D) Positive interim PET scan showing residual uptake in the mediastinum.
FDG-PET interim scans demonstrating negative and positive results. (A, C) Presentation scans showing uptake by HL. (B) Negative interim PET scan showing only physiological FDG uptake. (D) Positive interim PET scan showing residual uptake in the mediastinum.
A decade ago, several retrospective series examined the outcomes for patients treated with ABVD chemotherapy and were analyzed according to the result of an FDG-PET scan after the first 2 cycles of treatment. They showed that patients with negative interim PET scans had a significantly higher probability of durable remission (95% in the largest series) than those with positive interim PET scans (13%), and that this difference effectively negated the effect of baseline prognostic variables such as stage or the International Prognostic Score.18 The International Validation Study broadly confirmed these findings: patients with a PET score of 1 to 3 had a 95% 3-year FFS whereas those with score of 4 to 5 had an 18% FFS.19 However, it should be noted that subsequent prospective trials have generally not shown such a large difference in outcomes, with higher rates of recurrence among the PET-negative patients and better outcomes among the PET-positive patients than originally reported.20 A more recent analysis of the results seen when the 5-point scale was used suggested only marginally better outcomes, with 28% 3-year progression-free survival (PFS) for interim PET-positive patients continuing therapy with ABVD, 39% of whom had also received consolidation IFRT.21 There have been some attempts to improve the negative predictive value, for example, by performing the scan after 1 cycle rather than after 2 cycles,22 but this has not yet been evaluated prospectively. An alternative approach may be to use biological stratification with immunohistochemistry or gene expression analysis as an adjunct to PET, both of which have been proposed as predictive of treatment failure in pilot studies.23,24
Results of prospective trials: modifying the treatment
Having identified a test that might predict the outcome of treatment, several groups have undertaken prospective randomized trials to test the idea of modulating therapy according to the PET result.
Reducing treatment after a negative PET scan
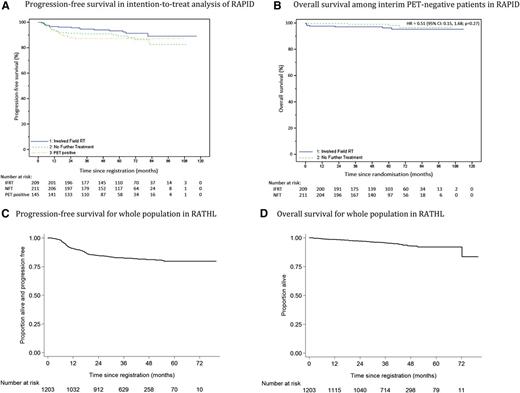
Two studies in early-stage disease have taken complementary approaches. The United Kingdom National Cancer Research Institute (NCRI) RAPID study randomly assigned patients with nonbulky stage IA to IIA disease who had a PET score of 1 to 2 after 3 cycles of ABVD to receive or not receive consolidation IFRT.1 The European Organisation for the Research and Treatment of Cancer (EORTC) HD10 study used an initial randomization between standard therapy and experimental PET-guided therapy. The latter arm was scheduled to omit consolidation INRT if the PET scan was judged negative (although the 5-point scale was not used) after 2 cycles of ABVD; patients with favorable-risk disease completed 4 cycles, and those with unfavorable-risk disease completed 6 cycles.25 In both trials, there was a small diminution of PFS with reduction of treatment. In the NCRI RAPID study, the PFS at 3 years was 94.6% in the group that received radiation therapy and 90.8% in the group that did not receive radiation therapy (Figure 2A-B), whereas in the EORTC H10 study, an early interim analysis established that the PET-guided therapy arm did not show equivalence to the standard treatment group, although the results were good in both risk strata: 1-year PFS rates were 100% and 94.9% in the favorable-risk group and 97.3% and 94.7% in the unfavorable-risk group. Neither study showed any indication that OS was compromised by the omission of radiotherapy, although the results of the EORTC HD10 study were reported after a relatively short follow-up. The absolute number of patient deaths in these studies was low; notably, the NCRI RAPID study reported 12 deaths among the 420 PET-negative patients at a median of 5 years of follow-up, of which only 1 death was attributed to HL. The conclusion from these trials is that omission of consolidation radiotherapy after a negative PET scan in early-stage HL is accompanied by a small increase in the risk of recurrence but no apparent worsening in OS, which allow patients and those treating them to make individual decisions based upon the relative risks from consolidation radiotherapy or the possible need for second-line treatment.
In advanced-stage disease, two different approaches have been taken in which some groups tested initial therapy with ABVD and others used the BEACOPPescalated regimen before assessment with a PET scan. The international RATHL study2 randomly assigned patients with a negative PET scan after 2 cycles of ABVD to continue to 6 cycles of ABVD or to omit bleomycin from the last 4 cycles, with the recommendation that patients should not receive consolidation radiotherapy. The Italian Gruppo Italiano Terapie Innovative nei Linfomi (GITIL) group randomly assigned patients with a negative PET scan after 2 cycles of ABVD to receive or omit consolidation IFRT to sites of initial bulky disease at the completion of 6 cycles of ABVD.26 A number of other prospective trials have examined the outcomes for patients with negative PET scans after 2 cycles of ABVD who continue to 6 cycles without randomization (summarized in Table 2). From these studies, it is apparent that the negative predictive value of interim PET scans after 2 cycles of ABVD is lower than that reported in the retrospective series, with the precise figure varying according to the baseline prognostic features of the group being studied. Thus, patients with more advanced-stage disease are not only less likely to become interim PET negative, but those that do become PET negative have a higher risk of recurrence. In the RATHL study, the 3-year PFS was 79.6% for those with stage IV disease but 90.0% for those with stage II disease, a finding reflected in the results of other series in which the negative predictive value of the interim PET scan was lower the worse the risk factors used for inclusion. It is important to note that this observation does not relate to the presence of initial bulky disease: in the RATHL study, the presence of bulk was not associated with a higher rate of recurrence after a negative interim PET scan, with a 3-year PFS of 87.6%.
The RATHL study—the only randomized study of treatment de-escalation in advanced-stage disease to have reported results so far—has shown that the omission of bleomycin after a negative interim PET scan is not accompanied by a significant increase in the risk of recurrence in any subgroup, including those with advanced-stage, high-prognostic-score, or bulky disease, which suggests that although the test is imperfect, it may still be used to modulate therapy. Importantly, the RATHL study also confirmed that the omission of bleomycin from the last 4 cycles of treatment resulted in fewer severe respiratory adverse events and better preservation of lung diffusion capacity, which demonstrates the potential to reduce morbidity over both the short and long term (Figure 2C-D).
The groups that have used the BEACOPPescalated regimen before PET scanning have reported a higher negative predictive value. In the GHSG HD15 study, patients with PET-negative residual masses 2.5 cm in diameter or more at the end of BEACOPPescalated chemotherapy did not receive consolidation IFRT, and this group had a PFS of 92.6% at 4 years, very similar to that of the patients in whom conventional imaging showed a complete response (92.1%).27 Performing the PET scan earlier, after only 2 cycles of BEACOPPescalated also seems to identify a group with a greater chance of continued remission. In the LYSA AHL2011 study of patients with advanced-stage disease, patients with negative interim scans showed a 2-year PFS of 94% for the standard treatment arm, which received 6 cycles of BEACOPPescalated, and 92% for the experimental arm, which received 2 cycles of BEACOPPescalated followed by de-escalation to 4 cycles of ABVD.28
Taken overall, these results suggest that a negative interim PET scan is most reliable in patients with less extensive disease at presentation and in those treated with the most intensive chemotherapy. Despite this variation, the results of de-escalating therapy after a negative interim PET scan seem to be favorable across the randomized studies to date: in early-stage disease, the small increase in recurrence rate following the omission of radiotherapy after ABVD treatment does not seem to reduce OS, whereas in advanced-stage disease, neither omitting bleomycin after ABVD treatment nor reducing treatment from BEACOPPescalated to ABVD seem to result in increased recurrences, although there has been relatively limited follow-up.
Increasing treatment after a positive PET scan
If interim PET is an effective way to identify patients who were poorly served by their initial therapy, the escalation of subsequent treatment may be one way to improve their outcomes, assuming that the disease remains sensitive to intensified chemotherapy or other modalities such as radiotherapy. The success of second-line therapy for HL in the form of salvage regimens and myeloablative consolidation suggests that this should be the case, and the hope is that by identifying treatment failure early, the degree of intensification required may be less. Several studies have tested this idea in large prospective series, but so far, only 1 randomized trial has reported initial results in early-stage disease. In the EORTC H10 study already mentioned, patients on the PET-directed arm with a positive PET scan after 2 cycles of ABVD switched to 2 cycles of BEACOPPescalated. Among the 19% of patients with a positive scan overall, the estimated 5-year PFS was increased from 77% with continued ABVD and INRT on the standard treatment arm to 91% with BEACOPPescalated and INRT in the PET-directed group (hazard ratio, 0.42; P = .002), with a trend toward improved OS.29
A number of studies in advanced-stage HL have tested the strategy of escalating from ABVD to BEACOPP after a positive interim PET scan. None of them had a randomized design because of the reported poor outlook for patients with a positive scan after 2 cycles of ABVD in the retrospective series originally analyzed; the PFS was approximately 15%, which made recruitment to a control arm of continued ABVD difficult for both patients and clinicians.
Several large-scale studies with strikingly similar results have now reported the results of treating patients with a positive PET scan with BEACOPPescalated after 2 cycles of ABVD (Table 3). In the RATHL study, which included unfavorable-risk stage II disease as well as stages III to IV, 16% of patients had a positive interim PET scan, and among 182 patients who went on to receive either 4 cycles of BEACOPPescalated or 6 dose-dense cycles of BEACOPP-14, there was a subsequent complete metabolic response in 74% of cases, with a 3-year PFS of 68% and OS of 87%.2 Similar results were seen in the Italian GITIL/FIL 0607 trial, in which treatment was increased to 4 cycles of BEACOPPescalated plus 4 cycles of BEACOPPbaseline with random assignment to the addition of rituximab or not; the 2-year FFS among 98 assessable patients was 66%.26 In the Southwest Oncology Group (SWOG) S0816 study, which gave 6 cycles of BEACOPPescalated, the 2-year PFS in 62 patients was 64%.30
Overall PFS and OS results in early- and advanced-stage HL in response-adapted NCRI RAPID1 and RATHL2 trials. (A) PFS in intention-to-treat analysis and (B) OS among interim PET-negative patients in the NCRI RAPID trial. (C) PFS and (D) OS for the whole population in the RATHL trial.
A more intensive approach was taken in the Italian Lymphoma Group HD0801 study, in which patients who were PET positive after 2 cycles of ABVD were judged against the FDG uptake of the mediastinal blood pool (score of 3 to 5 on the 5-point scale).31 They went on to receive the ifosfamide, gemcitabine, and vinorelbine (IGEV) salvage regimen for 4 cycles followed by myeloablative therapy and autologous stem cell rescue. This resulted in a 2-year PFS of 76%, although only 81 of the 102 PET-positive patients received the planned treatment.
The comparison of these series to historical control studies in which the proportion of durable responses after a positive PET scan was only 15% to 30% suggests that the escalation of therapy is an effective way to improve the outcomes for this group, although a PFS of 65% to 70% still leaves significant room for improvement.
Conclusions
The drive to maximize cures while minimizing late effects in HL remains an important challenge, and the studies required to demonstrate progress will require larger sample sizes and longer follow-up than has been the norm. The data on response-adapted therapy have led to its becoming increasingly accepted as the standard of care in that it supports both de-escalation of therapy for patients with a good early response and intensification of treatment for those with persistent FDG-avid disease early in the course. The findings in early-stage disease highlight the utility of interim PET in providing information to patients about the option of omitting consolidation radiotherapy or the advisability of escalating chemotherapy. In advanced-stage disease, it is clearly important to appreciate the interaction of the accuracy of the test with the baseline prognostic features and the intensity of treatment. A risk-adapted approach combined with a response-adapted approach may be optimal in using more intensive initial therapy for those with the worst disease but performing interim PET scans to assess the response in all and adjusting subsequent therapy accordingly. The data so far suggest that modulating treatment of advanced-stage HL both upward and downward after interim PET is an effective approach, which may improve the results and reduce morbidity and mortality in the long term, although we await longer follow-up to confirm this.
While we are investigating the role of response-adapted therapy, the therapy options themselves are changing, and in the near future, we will have more information about the possible contribution of the antibody-drug conjugate brentuximab vedotin32,33 and antibodies that target the PD-1/PDL-1 interaction,34 both of which seem to offer new opportunities for more effectively tailoring therapy to the patient. These will feed into the response-adapted approach that has been developed, which offers important opportunities to test the new treatments efficiently in the subpopulations of patients most likely to derive benefit from them.
Correspondence
Peter W. M. Johnson, Somers Cancer Research Building, Southampton General Hospital, Southampton SO16 6YD, United Kingdom; e-mail: johnsonp@soton.ac.uk.
References
Competing Interests
Conflict-of-interest disclosure: The author has received research funding from Janssen-Cilag and Eisai; has consulted for Janssen-Cilag, Boehringer Ingelheim, Bristol-Myers Squibb, Takeda Pharmaceuticals, and Celgene; and has received honoraria from Janssen-Cilag, Boehringer Ingelheim, Bristol-Myers Squibb, Takeda Pharmaceuticals, and Celgene.
Author notes
Off-label drug use: None disclosed.