Learning Objectives
Understand the role of panel-based molecular testing at the time of diagnosis in AML
Consider the characteristics and limitations of serial panel-based molecular testing in AML
CLINICAL CASE
A 52-year-old woman is diagnosed with acute myeloid leukemia (AML). At diagnosis, pathology demonstrated myelomonocytic morphology with a normal karyotype. The patient underwent standard induction chemotherapy with cytarabine and daunorubicin, achieving a complete remission, and is currently having consolidation therapy with high-dose cytarabine without an initial plan for allogeneic hematopoietic stem cell transplantation. What is the utility of broad panel-based molecular testing at different time points during the management of this patient?
Introduction
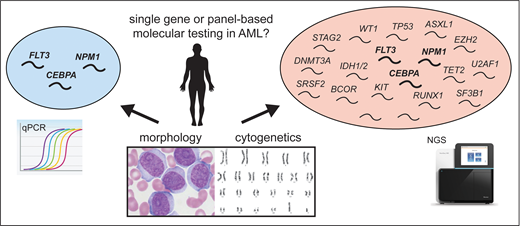
One of the great advances in understanding the pathobiology of AML has been through the discovery and characterization of recurrent somatic gene mutations. This is a rapidly evolving area where clinical decision-making may now capitalize on knowledge of a patient's mutational profile for diagnostic subtyping, prognostication, and choice of therapy, carried out in conjunction with standard histopathologic and cytogenetic studies at the time of diagnosis. Somatic mutations can be identified using several techniques, including targeted sequencing of a single gene, RNA- or DNA-based quantitative polymerase chain reaction (qPCR) assays, panel-based next-generation sequencing (NGS), and whole-exome or whole-genome sequencing, each of which exhibits varying sensitivity and specificity for the detection of gene mutations. Application of these technologies has revealed the genomic complexity of AML, with molecular heterogeneity between patients that may evolve over time and in response to treatment. A strong evidence base supports the testing of a small number of specific gene mutations in routine clinical practice, including NPM1, FLT3, and CEBPA, as they may influence diagnostic subtyping and provide clear prognostic information in patients with a normal karyotype on cytogenetic testing.1 Improved technology and declining cost for gene sequencing has provided more widely available panel-based gene testing for patients with AML, providing accessible testing for a larger number of genes. NGS-based gene panels used in AML have grown to incorporate an ever-expanding set of genes that typically include FLT3, NPM1, CEBPA, RUNX1, isocitrate dehydrogenase 1 and 2 (IDH1/2), TET2, TP53, KIT, WT1, and ASXL1, among other recurring gene mutations found in myeloid malignancy (Table 1). While NGS-based gene panels are able to detect a larger number of gene mutations and comutations in a single patient, it can be challenging to interpret and clinically use all of these data points. In this evidence-based minireview, we assess the decision to test a broad NGS panel, rather than individual genes, in AML and how this decision may affect the diagnosis, prognosis, and/or treatment selection for a patient.
What role does molecular testing play in establishing a diagnosis of AML?
AML diagnosis is primarily based on morphology and cytogenetics but increasingly takes molecular features into consideration. Some AML subtypes now incorporate specific gene mutations into the diagnostic criteria, including NPM1 and CEBPA.1-3 This is based on the observation that these mutations are associated with distinct clinicopathologic features that are reflected in patient outcomes. Notably, AML may now be diagnosed by the presence of NPM1 mutation irrespective of bone marrow myeloblast percentage, analogous to the finding of specific cytogenetic abnormalities, such as t(8;21) and inv(16). An emerging area is the understanding that comprehensive molecular profiles may better characterize the origin of a given AML subtype; for instance, the detection of gene mutations in SRSF2, SF3B1, U2AF1, ZRSR2, ASXL1, EZH2, BCOR, or STAG2 are associated with >95% specificity for secondary AML (sAML).4 However, to date, the formal diagnosis of sAML uses the correlation of such molecular features with the clinical history, morphology, and cytogenetic findings. In the investigational setting, detailed molecular profiling of patients with AML has been shown to effectively subclassify patients into diverse, clinically relevant subgroups and predicts the existence of leukemia subtypes not currently known within the existing classification system,5 suggesting the strong potential for future clinical use of in-depth molecular disease classification. At this time, it is important to recognize the expanding number of mutations necessary for a complete AML classification; although single-gene mutation testing can be done for a minimal set of genes, panel sequencing increasingly has an advantage in this domain.
What role does molecular testing play in predicting a patient's prognosis?
FLT3, NPM1, and CEBPA were identified early as having a role in risk stratification of patients with AML who have normal cytogenetics,6 effectively identifying patient risk of relapse and survival after chemotherapy.1,2 AML with an isolated NPM1 mutation predicts for more favorable-risk disease with good response to standard chemotherapy.7 Similarly, in-frame mutations within the basic leucine zipper region of the CEBPA gene identify patients with favorable-risk disease.8,9 In contrast, the presence of FLT3 gene internal tandem duplication predicts a higher risk of relapse. Recent data suggest that broader mutation profiles—often facilitated through panel-based gene testing approaches— can improve upon risk stratification and disease prognosis (Table 1). For example, TP53 mutations confer a distinctly poor prognosis, have a high risk for failure with standard chemotherapy, and may prompt alternative treatment approaches such as those with a hypomethylating agent backbone.10,11 RUNX1,12 ASXL1,13 and other secondary-like mutations may also indicate higher risk of patient relapse or therapy resistance. In addition, high mutational burden or the detection of certain mutations (Table 1) may suggest a diagnosis of sAML, which has clinical importance, in that these gene mutations identify a group of patients with very poor prognosis, and increasingly guides the choice of induction chemotherapy and consolidation strategy.
Can gene panel testing affect treatment selection for AML differently than testing for single mutations?
Several mutation profiles affect the initial treatment strategy. The presence of FLT3 internal tandem duplication or FLT3 mutations in the tyrosine kinase domain, for instance, informs the use of drug therapies that target the FLT3 kinase. Incorporating FLT3 inhibitors with standard chemotherapy provides a survival advantage for patients with this AML subtype.14 More challenging perhaps is the entity of sAML, which may be more variably defined but for which CPX-351 (Vyxeos; Jazz Pharmaceuticals) may be advantageous to standard induction therapy.15 A growing number of available targeted therapies may be better suited to other genetic alterations. In patients with IDH1/2 mutations, small-molecule inhibitors of IDH1 or IDH2, combined with azacitidine, can improve outcomes in select patients,16 although these patients also have high response rates to other regimens such as azacitidine in combination with venetoclax.17 There is also evidence that TP53-mutated AML—and perhaps other secondary-like mutations—may be equally if not more responsive to alternative therapies to induction, such as hypomethylating agent-based therapies. With the expanding availability of targeted drug therapies, the value of panel-based gene testing is likely to expand.
Where is molecular testing likely to play an impact after initial AML diagnosis?
Molecular testing has a growing role following a patient's initial diagnosis during treatment. There is a strong interest and active research to optimize molecular monitoring of measurable residual disease to guide postremission treatment strategies for AML.18 In the setting of NPM1-mutant AML, specific detection of the mutant NPM1 transcript by qPCR is a powerful indicator of relapse risk that can be used to risk-adapt patient treatment.19 A limitation to the universal application of such techniques is the genetic heterogeneity of AML; NGS-based gene panel assays are being evaluated as a way to monitor disease over time and are better able to track clonal heterogeneity compared with gene-specific qPCR assays. This is relevant as most patients with AML will not have a mutation as easy to track as NPM1. If such tracking is validated, NGS panels have an advantage compared with qPCR assays because they assess a larger selection of genes, and most patients will have at least 1 genetic alteration detected by the panel assay that can be monitored over time.5 Furthermore, broad NGS-based gene panel testing enables detection of the emergence of additional molecular abnormalities over time that may not have been present at the time of diagnosis. NGS-based measurable residual disease monitoring faces several limitations, including relatively lower sensitivity compared with dedicated qPCR assays, including a lack of standardization, and significant challenges related to distinguishing what represents residual leukemia from what may be background clonal hematopoiesis (clonal hematopoiesis of indeterminate potential or clonal cytopenias of unknown significance).20 At this time, interval NGS testing in remission remains under investigation but may be most valuable at the time of clear treatment decisions where estimation of patient risk is clinically important, such as with allogeneic transplant.21
What is the role of molecular testing in patients with AML after relapse?
Finally, AML relapse after chemotherapy, like at diagnosis, represents a time point to reassess disease in order to develop a salvage strategy. In contrast to monitoring in remission, at relapse, there is more emphasis on immediately actionable mutations. These include mutations in FLT3, IDH1, and IDH2. Whether a broad NGS-based panel offers significant advantage over targeted sequencing at relapse is less clear, however. Particularly for late relapses, NGS can help to clarify the relation of the relapsed leukemia to the initial diagnosis. Since most disease at relapse has a universal poor prognosis, risk assessment has less immediate utility. It is nonetheless important to assess for FLT3 mutations, which can emerge during treatment and for which several targeted therapies are available. Mutations in IDH1 or IDH2 appear more stable over time but can be subject to subclonal evolution that may evade detection at low levels early in the disease course. An increasing number of targeted therapies in clinical development also require the presence of a mutated gene target; given the importance of clinical trials as an option for patients with relapsed or refractory AML, such testing can be informative.
Conclusions
Gene panel testing, now commonly performed by NGS-based technology, is an increasingly available tool for patients with AML. We recommend all patients with AML have broad gene panel testing at diagnosis, which includes the most common recurrently mutated genes in this disease where testing may influence diagnosis, prognosis, and treatment selection. At this time, there is an evolving evidence base for serial NGS-based broad gene panel testing during treatment in routine clinical practice. We await robust evidence to support the routine use of this outside of a clinical trial, although it may be valuable in specific clinical scenarios such as prior to allogeneic transplant. Many open questions remain, including optimal timing for serial panel mutation assessment, thresholds for detection in NGS-based methods that balance sensitivity and specificity, and better defining which gene mutations, and combinations thereof, are most predictive of patient outcomes. Finally, a major barrier remains regarding the accessibility, cost, and standardization of these techniques to make them more accessible in routine clinical practice.
Recommendations for NGS-based broad molecular testing in AML
Broad NGS-based gene panel testing should be performed at the time of AML diagnosis. (Strong recommendation, moderate certainty of the evidence)
At AML relapse, patients should have molecular testing repeated, although it is less clear whether NGS-based panel testing has an advantage over testing single actionable genes at this time. (Strong recommendation for testing in general, low certainty of evidence between testing modalities)
At this time, routine serial NGS-based gene panel testing for patients with AML in remission remains investigational, although may have value in specific scenarios. (Low certainty of evidence)
Conflict-of-interest disclosure
Brandon J. Aubrey is a former employee of the Walter and Eliza Hall Institute, Melbourne, Australia, and has received payments relating to royalties and milestone payments for the BCL-2 antagonist venetoclax/ABT-199.
Andrew Brunner is a consultant for Acceleron, Agios, BMS/Celgene, CTI Biopharma, Gilead, Keros Therapeutics, Novartis, Taiho, and Takeda.
Off-label drug use
Brandon J. Aubrey: nothing to disclose.
Andrew Brunner: nothing to disclose.