Abstract
This article reviews 3 products: pathogen-inactivated platelets, cold-stored platelets, and cryoplatelets. These are all coming to a transfusion service near you in the next few years. The article reviews the limitations of these new products and highlights the gaps in our understanding of their place in patient treatment.
Learning Objectives
Describe novel platelet therapies that are coming to transfusion medicine
Explain the limitations of these new products
CLINICAL CASE
A patient has received cold platelets in the context of cardiac surgery. A patient with bleeding at the end of cardiac surgery receives a transfusion of 1 adult dose of cold-stored platelets. This has helped to control the bleeding, because these platelets are activated and readily support coagulation activation through enhanced expression of phosphatidyl serine on their surface. Following transfusion, bleeding appears to have decreased. Cold-stored platelets express increased levels of phosphatidyl serine (PS) on their surface. Increased PS expression is associated with platelet activation, and in vitro studies suggest that this is one mechanism by which cold-stored platelets may contribute to hemostasis.
Introduction
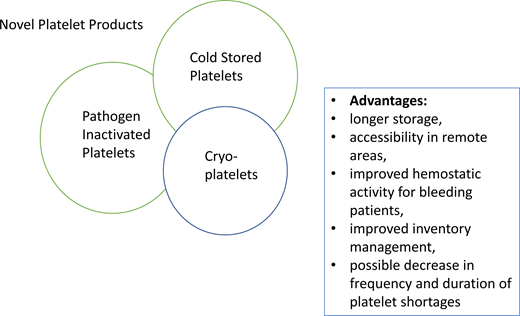
Several novel platelet products are becoming available. These include the increasing use of pathogen-inactivated platelets in the United States; the increasing use of cold-stored platelets for bleeding patients, in part in response to platelet shortages; and the potential future use of cryopreserved platelets as a means to ensure against platelet shortages. This article takes each one of these novel products in turn. Each of these new forms of platelet products is in different stages of evaluation and application in North America, Europe, the United Kingdom, Australia, and Japan.
Pathogen-inactivated platelets
Pathogen-inactivated platelets have become widely available in the United States. The American Red Cross has made a commitment to subjecting most of their platelet stock to pathogen inactivation. The only licensed technology in the United States is the Intercept technology (Cerus Corporation). This process involves numerous steps, including first removing plasma from an apheresis platelet collection, then adding a psoralen-derived compound (amotosalen) in platelet additive solution to the product, exposing to UV light. There are multiple steps involved and while plasma depletion may be of benefit to patients with allergic reactions to plasma proteins, there are many manipulations with their attendant downsides. The exposure of platelets to UV causes mild platelet activation, which worsens upon storage. This is true for all platelet inactivation technologies. They disrupt the function of mitochondria, which may shorten the circulation residency time of the platelets.
Both the EuroSPRITE and the SPRINT trials showed a shortening of the intertransfusion interval.1,2 This is probably because platelets subjected to pathogen inactivation technologies are somewhat more activated than untreated platelets (Table 1). This leads to the question of whether, with the use of pathogen inactivation, we will see increased demand on the platelet supply. Also, following treatment, the platelet count in blood products is lower owing to the various manipulations that are carried out.3 This may also influence the intertransfusion interval.
Canada along with Norway and the Netherlands conducted the PRePARES trial of Mirasol-treated platelets. This trial showed similar findings to the EuroSPRITE and SPRINT trials supported by Cerus.4 In addition, the use of pathogen-inactivated platelets did not prevent alloimmunization in patients4 on a per protocol analysis.
An alternative to Intercept is the riboflavin technology of TerumoBCT. This technology also activates platelets.3,5 Platelet activation is an inherent feature of pathogen inactivation technologies, and this is why some clinical trials have seen an increase in platelet utilization associated with pathogen inactivation technologies applied to platelets. The PREPAReS trial showed an increased use of platelets in hematology/oncology patients receiving prophylactic platelet transfusions on a per protocol basis.6 Furthermore, a Cochrane review has indicated that pathogen-inactivated platelets may have a greater propensity for an increased risk of platelet refractoriness.6 Additionally, concern over reduced quality of psoralen-treated platelets coupled with their greater cost may influence their acceptance in clinical practice.
Cold platelets
When component therapy was first developed, all blood products were stored in the refrigerator, including the platelet products. This caused platelet activation, which resulted in accelerated clearance when used in prophylactic platelet transfusion7 but not when used in bleeding patients.8 In bleeding patients, the fact that the platelets are partially activated supports the coagulation factor cascade. It is important to set the historical context around why we currently store platelets at room temperature. The fact that whole blood required refrigeration led us to refrigerate all blood products in the 1960s when component therapy was first developed. This proved not to be the right thing to do for platelets used in prophylactic platelet transfusions.
Even though cold platelets would result in more challenging inventory management for hospital transfusion services, there are benefits to using them. During the pandemic, the Mayo Clinic used cold platelet storage to manage inventory.9 Other blood operators globally have seen demand for cold platelets, and this may well be a way to improve inventory management during the pandemic. From preliminary modeling that we have done, we believe that it will help to reduce global wastage rates.
The issue with cold platelets is that although they seem to be better for bleeding patients than room temperature–stored platelets, they cannot be used for prophylactic platelet transfusions. Chilled platelets are rapidly cleared by Ashwell-Morrell receptors in the liver with the exposed β-N-acetylglucosamine moieties on cold platelets.10 This means the management of 2 platelet inventories in the hospital blood bank, but it will mean more focus on inventory management and moving products from room temperature into the cold. Clinical trials have shown improved bleeding cessation with cold platelets.11 Studies from our group have shown that you can transfer platelets into the cold after 3 or 4 days without an obvious impact on the platelets.8
Together with Angelo D'Alessandro, we have examined the metabolomic profile of cold platelets.12 As expected, platelets do not show much active metabolism in the cold. The use of cold platelets has distinct advantages. It is a more efficacious product for bleeding patients; however, more clinical studies are needed. The US Food and Drug Administration has approved a clinical trial in the United States that is led by Dr Philip Spinella; details can be found at https://www.clinicaltrials.gov/ct2/show/NCT04834414. The end point is reduction in acute bleeding. This trial should provide much useful data on cold platelets. It is focused on apheresis platelets as they form over 90% of the inventory in the United States. There is a markedly reduced risk of bacterial contamination and a reduced rate of development of the platelet storage lesion. The extension of shelf life to 14 days reduces wastage and improves platelet inventory management. Storage of cold platelets is simpler in that agitation is not required. That said, there are still many things we do not yet understand about cold platelets.13
Frozen platelets
Frozen platelets have been used by various military organizations, including the Australian Defense Force and the Dutch military blood bank. They were first developed by Robert Valeri at the Naval Blood Research Laboratory in Boston, Massachusetts.14 Valeri developed a protocol that avoids washing platelets as there is too much loss of platelets with washing. The protocol incubates platelets with dimethyl sulfoxide, spins them down, and removes the plasma with the residual dimethyl sulfoxide. The platelets are frozen as a pellet and subsequently thawed and suspended in a compatible plasma.
Platelets prepared in this manner are good for bleeding patients, but like cold storage, they cannot be used for prophylactic transfusions owing to their relatively rapid clearance from the circulation.
For countries with vast geographies, like Australia, the implementation of frozen platelets offers an opportunity to improve platelet management. The storage expiration date of cryopreserved platelets is 12 months, in contrast to an expiration date of 5 to 7 days for room temperature–stored liquid platelets. The Australians have begun to do clinical studies with frozen platelets. The CLIP trial has provided a first glimpse at the utility of frozen platelets.15 The Australians have now moved on from a pilot trial to a full trial. This trial involves comparison of cryopreserved platelets to liquid platelets in cardiac surgery patients.
Conflict-of-interest disclosure
Dana V. Devine is the chair of the Scientific Advisory Board of Macopharma, a French company working in the transfusion medicine space; an employee of Canadian Blood Services; chair of the medical advisory committee of the American Red Cross; on the board of directors of STRM.Bio, a Boston-based gene therapy company; and currently the president of the AABB.
Off-label drug use
Dana V. Devine: nothing to disclose.