Abstract
There is now clear clinical evidence that adoptive cellular immunotherapy can eradicate hematologic malignancy and cure otherwise lethal viral infections. With this knowledge comes the challenge of improving the effectiveness and safety of the approach and of simplifying the methodologies required whilst still meeting appropriate federal regulatory guidelines. This review provides an overview of the current status of cellular immunotherapies and addresses how they may be implemented and the future directions they are likely to take.
In Section I, Dr. Brenner with Drs. Rossig and Sili reviews the clinical experience to date with adoptive transfer of viral antigen-specific T cells for the successful treatment of Epstein-Barr virus-associated malignancies as well as viral infectious diseases. Genetic modification of the T cell receptor of the infused cells to potentiate such T cells as well as modifications to improve safety of the infusions are described.
In Section II, Dr. Young describes the hematopoietic lineages of human dendritic cells and some of their immunotherapeutic applications. The critical importance of dendritic cells to T cell immunity and the capacity to generate dendritic cells in large numbers has spawned enormous interest in the use of these specialized leukocytes to manipulate cellular immunity. Successful cytokine-driven differentiation of dendritic cells reveal two types, myeloid- and plasmacytoid or lymphoid-related dendritic cells. The effects of maturation on phenotype and function of the dendritic cells and their use as immune adjuvants in dendritic cell vaccines to elicit antitumor and antiviral immunity are reviewed.
In Section III, Professor Goulmy illustrates some current and future approaches towards tumor-specific cellular therapy of hematopoietic malignancy. Minor histocompatibility antigen (mHag) disparities between HLA-matched bone marrow donor and recipient can induce allo-responses that may participate in post bone marrow transplantation (BMT) graft-versus-leukemia (GVL) reactivities. A lack of such allo-reactivity may result in relapse of leukemia after BMT. In these patients, adoptive immunotherapy with cytotoxic T cells (CTLs) specific for hematopoietic system-restricted mHags may be used as an extension of current efforts using immunotherapy with donor lymphocyte infusions. Adoptive immunotherapy with CTLs specific for the hematopoietic system-restricted mHags, however, offers the prospect of greater and more predictable effectiveness in the absence of graft-versus-host disease.
I. Virus- and Tumor-Specific Cytotoxic T Cell Therapy
Malcolm Brenner, M.D., Ph.D.,*Claudia Rossig, M.D., and Uluhan Sili, M.D.
Center for Cell and Gene Therapy, Baylor College of Medicine, 6621 Fannin Street, #3-3320, Houston TX 77030-2303
Adoptive transfer of antigen-specific cytotoxic T lymphocytes (CTLs) has become an attractive strategy for the treatment of viral diseases and cancer. Major obstacles to this application include the need for identification of tumor antigens that can serve as targets for CTLs; the development of methods to activate and expand tumor-specific CTLs in vitro; and the discovery of means to protect the transferred cells from the anti-immune tactics employed by viruses and tumors and, with allogeneic T cells, from the host's immune response against the T cell itself. Recent successes in transferring genes into CTLs have significantly broadened the potential applications of adoptive immunotherapy. Thus, retroviral gene markers have helped to track tumor-specific T cells and validate their activity, while “suicide genes” have facilitated the removal of unwanted T cell-mediated activities. The introduction of single-chain antibodies coupled to T cell receptor (TCR) signal transduction elements may help to overcome the major histocompatibility complex (MHC) restriction of T cells that otherwise limits their activity.
Epstein-Barr Virus-Associated Infections and Tumors
Epstein-Barr virus (EBV) infection provides an excellent model system with which to study the safety and therapeutic efficacy of adoptively transferred CTLs. EBV is a latent herpesvirus that infects over 90% of the population. Primary infection occurs in the oropharynx in mucosal squamous epithelial cells. The viruses produced in these cells infect circulating B cells. Primary EBV infection is usually a self-limited process followed by a life-long latency in oral epithelial cells and in B cells; the virus is also associated with a range of malignant diseases, not only of B and epithelial cells, but also of T cells, natural killer (NK) cells, and muscle.1,2 All EBV-positive tumors reflect the latent life cycle of the virus. That is, with any given type of EBV-related malignancy, only a small proportion of the viral genome is expressed, and the differential regulation of these genes is one of many strategies the virus employs to evade the immune response.
Three types of latency have been described in EBV-positive tumors. Type 1, which involves only four EBV genes (EBNA1, RK-BARFO and the two EBERs), is common to Burkitt lymphoma and gastric carcinoma. Type 2 latency, as seen in Hodgkin lymphoma, nasopharyngeal carcinoma, NK and T cell lymphomas, and other mucosal carcinomas, involves two additional genes encoding the membrane proteins LMP1 and LMP2. The lack of an immune response to these antigens may occur because Reed-Sternberg cells secrete inhibitory cytokines such as TGF-β, IL-10 and the Th2 chemokine TARC.3,4 Type 3 latency involves genes encoding all EBV-associated proteins, some of which are highly immunogenic. CTL-specific epitopes in the EBNA3 proteins, for example, dominate the cellular immune response to EBV in almost all hosts. Since cells defined by type 3 latency do not evade the immune response, they can only cause lymphoproliferative disorders in persons severely immunocompromised by organ or stem cell transplantation, congenital immunodeficiency, or HIV infection.
Lymphoproliferative disease
Latent EBV infection can become active and induce lymphoproliferative disease (LPD) in recipients of solid organ or allogeneic stem cell transplants who are receiving immunosuppressive therapy or who lack an efficient CTL response. The reported incidence of EBV-LPD among persons undergoing solid organ transplantation ranges from 1% to 10%, with the highest risk in seronegative recipients and patients receiving higher doses of immunosuppressive agents. Risk factors for unsuccessful hematopoietic stem cell transplantation (SCT) include in vitro T cell depletion of donor marrow, use of a mismatched family donor or closely matched unrelated donor, and intensive immunosuppression.5
The onset of EBV-LPD is usually preceded by a large increase in viral load in recipients of either solid organ6 or stem cell transplants.7,8 The majority of these cases are B cell lymphomas or histologically high-grade non-Hodgkin lymphomas of the immunoblastic or undifferentiated large cell type,9 which respond poorly to cytotoxic therapy. The malignant cells express latent cycle virus-encoded antigens (EBNA1, 2, 3A, 3B, 3C and LMP1, 2a, 2b), most of which are targets for virus-specific immune activity.10 The immunogenicity of these antigens has been exploited to treat post-transplantation EBV-LPD with unmanipulated donor T cells. Sloan-Kettering investigators reported responses to donor T cells in 20 of 22 patients undergoing stem cell transplantation.11 Others have also had success with this strategy but have shown lower response rates and a significant risk of graft-vs-host disease (GVHD).12 EBV-specific CTLs5 can be used as either prophylaxis or treatment for this disease.
Prophylaxis with CTLs
Thirty-nine patients were treated with infusions of CTLs following transplantation of T cell- depleted stem cells. None developed LPD, compared with 11.5% of a comparable untreated historical control group.13 Gene-marked EBV-specific CTLs persisted in the patients for as long as 60 months, reconstituted immune responses to EBV, and reduced the high virus load seen in about 15% of patients.14 A study from Sweden recently confirmed the efficacy of EBV-specific CTLs in reducing the viral load in patients with high EBV-DNA levels post-transplantation.8
Treatment with CTLs
Immunotherapy with antigen-specific CTLs can also be used to treat patients who develop overt lymphoma.13 In one study, two of three patients with this complication responded well to CTL infusion. One had a biopsy-proven accumulation of gene-marked CTLs at the disease site,13 but there was a marked inflammatory reaction during the therapeutic response, underscoring the benefits of a prophylactic approach. The third patient did not respond and died of progressive disease 24 days after CTL therapy. This failure was traced to a deletion in the EBNA3B gene in tumor cells that removed immunodominant epitopes, thereby inducing resistance to killing by CTLs.15 Such escape mutants can compromise results even when polyclonal CTL lines are used and present a particular problem in patients with a large tumor load. Bonini et al16 attempted an alternative approach, transducing nonspecific T cells with a retroviral construct containing the thymidine kinase (TK) gene, which renders the cells sensitive to the cytotoxic effects of ganciclovir. When used to treat relapsed or EBV-associated lymphoma, the transduced cells provoked GVHD in three patients, which resolved in two after treatment with ganciclovir. Several other patients developed immune responses to the transgenes, which may have reduced the longevity of the transferred cells.
Treatment with donor-derived T cells is obviously not an option in recipients of solid organ transplants. Thus, unmanipulated allogeneic T cells from an HLA-matched sibling have been successfully used to treat LPD in the central nervous system (CNS) of a lung transplant recipient.17 Haploidentical EBV-specific CTLs afford another option, as most patients will have a haploidentical relative.18 When administered to a renal transplant recipient with EBV-LPD, EBV-specific CTLs derived from a haploidentical parent induced regression of the disease.11 However, this effect was only transient, suggesting that the CTLs were not surviving long term, possibly because they were being eliminated due to recognition of MHC antigens on the nonshared haplotype. Autologous EBV-specific CTLs have been used prophylactically in three solid organ transplant recipients,19 all of whom had decreases in EBV load and increased numbers of CTL precursors postinfusion, with these effects persisting for as long as 3 months.19 More recently, Khanna and colleagues20 generated an autologous EBV-specific CTL line from a renal transplant recipient with active LPD and showed significant regression of the disease post-infusion. New lymphoma lesions developed in this patient, suggesting that the transferred CTLs may not survive as well in immunosuppressed recipients of solid organ transplants as in those given stem cell transplants.20 At autopsy, this patient had evidence of necrosis and hemorrhage in a pulmonary vein, reinforcing observations of inflammatory reactions in stem cell recipients and arguing for caution when using adoptively transferred T cells to treat patients with bulky disease.
Hodgkin's disease
In North America, 50% of Hodgkin tumors are EBV positive, in a type 2 latency pattern. In one recent study, EBV-specific CTLs were prepared from eight patients with advanced relapsed disease, gene-marked, and reinfused as antitumor therapy.14 Follow-up analyses showed in vivo expansion and long-term persistence of CTLs capable of binding LMP2 tetramers. There was also a reduction of EBV load and evidence for penetration and selective accumulation/expansion of CTLs at tumor sites. Despite resolution of type B symptoms and stabilization of disease, none of the patients had a complete response and all subsequently progressed.21
We are investigating several possible means to improve outcome of CTL therapy for Hodgkin disease. In one strategy, based on the use of CTLs specific for the subdominant antigens expressed in this disease, dendritic cells are transduced with an adenoviral vector encoding a full-length LMP2 gene. The CTLs recovered after exposure to these gene-modified cells are highly biased toward recognition of the LMP2 antigen. Another approach centers on the mechanisms by which Hodgkin cells evade immune surveillance.3,4 Such cells secrete a number of Th2 cytokines and chemokines, such as TARC and IL-10, that can inhibit to CTL immune responses. TARC recruits Th2 cells, which secrete IL-4 and thus contribute to the pro-Th2 and anti-Th1 environment already induced by the secretion of IL10. To overcome this inhibition we plan to transduce CTLs with a Th1 cytokine, IL-12, and CCR4, the chemokine receptor for TARC. It is hoped that TARC-expressing CTLs will be recruited to tumor tissues, where expression of IL-12 will make them resistant to the inhibitory effects of IL-4 and IL-10. The production of IL-12 may also activate local professional antigen-presenting cells and facilitate cross priming with tumor antigens.
Cytomegalovirus infection
Deficiencies in class I HLA-restricted CD8+ cytotoxic response to cytomegalovirus (CMV) contribute importantly to the pathogenesis of CMV disease in immunocompromised patients.22 During the first 100 days after stem cell transplantation, about 50% of the recipients are deficient in a CD8+ CMV-specific response, placing them at risk for this disease, which can produce significant morbidity and mortality.22 CMV-specific CTLs also play an important role after renal transplantation in controlling viral load, as demonstrated by decreased levels of viral antigen and protection from CMV disease.22 Although ganciclovir reduces the incidence of CMV disease, it causes severe neutropenia in 30% of the cases and is associated with an increased incidence of CMV disease 100 days post-transplantation. CD8+ CMV-specific cytotoxic T cells, infused into 14 patients 30-40 days after stem cell transplantation,23 lacked discernible side effects and were active against CMV in the 11 patients who were deficient in such activity. Importantly, responses were maintained only in patients whose CD4-mediated CMV-specific responses had recovered. A follow-up study in which both CD4 and CD8 clones were transferred into patients has shown long-term persistence of transferred immunity.24 The importance of both a CD4- and a CD8-specific immune response in the maintenance of long-term immunity has been confirmed by several other groups.
Multispecific CTL lines
The above studies with EBV and CMV have proved the antiviral efficacy of CTL therapy, but each cell line was specific for only one of the many viruses that can cause morbidity in immunocompromised patients. To generate CTL specific for both CMV and EBV, Lucas et al25 transduced EBV-transformed B-lymphoblastoid cell lines with a retrovirus encoding CMV pp65, the immunodominant CMV polypeptide. The CTLs generated with these antigen-presenting cells showed specific cytotoxicity against EBV and CMV. A similar approach using dendritic cells to present antigen is being used to generate CTLs specific for EBV, adenovirus and CMV.
HIV Infection
The ability of CTLs to control viremia at initial stages of infection, with resultant recovery of CD4+ cell counts, led to a clinical trial in which in vitro-expanded autologous HIV envelope specific CTLs were infused into patients26 to determine if the cells would “home” to sites of viral replication and mediate antiviral activity. As a safety precaution, the cells were transduced with a fusion gene, Tk-Hyg, that encoded parts of herpes simplex thymidine kinase and hygromycin phosphotransferase. The intent was to select transduced cells by exposure to hygromycin ex vivo, and then kill them in vivo with ganciclovir should their infusion produce unwanted adverse events. Unfortunately, the Tk-Hyg gene product turned out to be exceedingly immunogenic, even in AIDS patients, and the cells were rapidly destroyed after infusion. In a second-generation study, patients received three infusions of unmodified autologous HIVGag-specific CD8+ CTL clones, followed by infusion of neomycin phosphotransferase-marked CTLs.27 The infused CTLs localized to areas of viral replication, producing decreases in the number of circulating HIV-infected cells, but they persisted only briefly, probably due to an inadequate Th response.24
Because CD4+ T cells are themselves targets for HIV infection, efforts have been made to render the CTLs independent of T-helper function, for example, by transducing them with an IL-2 gene carrying the promoter of a cytokine, such as GM-CSF, that is secreted by CTLs or with a gene incorporating the extracellular domain of a CTL-associated cytokine receptor and the intracellular domain of IL-2.28 An alternative strategy has been to transduce CD4+ helper T cells with HIV-resistance genes that act through several different mechanisms: sequestering Tat or Rev by expressing RNA decoys,29 cleaving HIV RNA by expressing antitat and anti-rev ribozymes,30 or expressing intracellular antibodies31 or chemokines32 that can bind and sequester HIV proteins or co-receptors, respectively. None of these modifications has proved effective in preliminary evaluations.
Chimeric T Cell Receptors for the Targeting of Cancer Cells
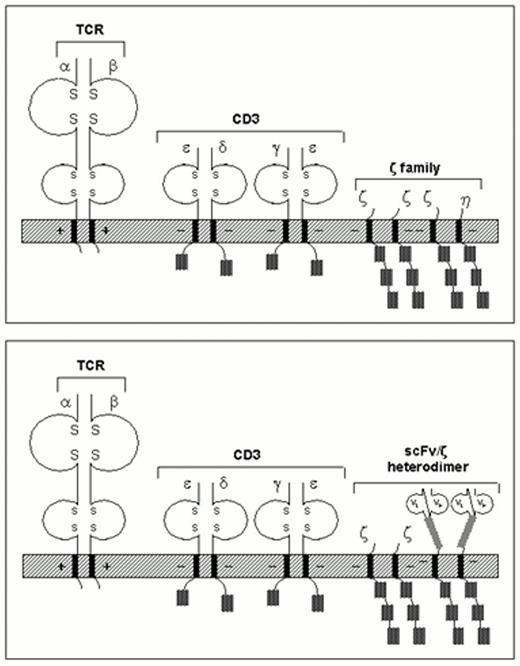
Large numbers of tumor-specific T lymphocytes can also be produced by genetically modifying human T cells to express tumor antigen-specific chimeric immune receptors (“T-bodies”). This tactic is based on the observation that engagement of a single T cell or Fc receptor chain suffices to induce cellular activation.33,34 One can generate chimeric receptors by joining the heavy- and light-chain variable regions of a monoclonal antibody, expressed as a single-chain Fv (scFv) molecule, to the TCR-ζ (Figure 1) or Fc-γ immune receptor domain. To promote functional recognition of its target antigen, the scFv is disengaged from the plasma membrane, usually by insertion of an immunoglobulin hinge-like domain. Antigen stimulation of the extracellular component of the chimeric receptor results in tyrosine phosphorylation of immune-receptor activation motifs present in the cytoplasmic domain, initiating T cell signaling to the nucleus. Human T lymphocytes genetically engineered to express the recombinant receptor genes were capable of specific lysis and cytokine secretion upon exposure to tumor cells expressing the relevant target antigens.35 Adoptively transferred chimeric receptor-transduced cells were protective in murine tumor models.36
Structure of the TCR complex (top), and chimeric receptor expressed as part of that complex. Details are given in the text.
Structure of the TCR complex (top), and chimeric receptor expressed as part of that complex. Details are given in the text.
T cells with chimeric receptors have numerous advantages over immunotherapies based on monoclonal antibodies or T lymphocytes alone. They can be directed toward any native tumor- or viral-associated antigen for which a monoclonal antibody exists, making this strategy applicable to a wide variety of malignancies and viral diseases. In contrast to the lengthy process of CTL selection by standard methods, characterization and expansion of lymphocytes with native specificity for target antigens allows one to generate large populations of antigen- redirected T lymphocytes in a matter of weeks. Since chimeric T cell receptors provide T cell activation in a non-MHC-restricted manner, they permit cells to evade the major mechanisms by which tumors avoid T cell recognition, such as downregulation of HLA class I molecules and defects in antigen processing. The absence of MHC restriction may also allow a “universal” cytotoxic T cell to be generated, although immune recognition of such foreign cells may reduce their clinical value. T body-mediated effector functions are more likely to eradicate tumor cells than humoral immune responses alone, in that cytokine secretion upon T cell activation recruits additional components of the immune system, amplifying the antitumor viral immune response. Finally, unlike intact antibodies, T cells can migrate through microvascular walls and penetrate the cores of solid tumors to exert their cytolytic activity.
Efficient tumor cell lysis
Ensuring long-term persistence of transferred T cells in the host is a major challenge in adoptive immunotherapy. Rapid clearance of modified T effector cells may be partly overcome by humanization of currently available hybridoma antibodies or by the generation of fully human single-chain antibodies by phage display technology. Coexpression of potentially immunogenic marker genes can be avoided by the use of highly efficient retroviral vector systems for T cell transduction, eliminating the need for selection of transduced cells. However, even in the absence of immunogenicity, T lymphocytes may be locally lysed by factors secreted by tumor cells, and the surviving modified T lymphocytes may lose their antitumor viral reactivity by returning to a resting state. Although T cell activation was not a prerequisite for efficient signaling through the chimeric receptor in vitro,37 the functional capabilities of T cells with chimeric in situations where costimulation is limiting remain to be determined. To avoid the functional inactivation of T lymphocytes expressing chimeric receptors in vivo, it may be necessary in future designs to engage relevant coreceptor molecules.
The dynamics of the interaction between chimeric receptors and target antigens in vivo is not well understood. In all published studies, the degree of specific tumor cell lysis by cells expressing chimeric TCRs has been highly variable, depending on the density of antigen as well as the number of receptors expressed on the T cell surface. Although minimal ζ chimeric receptor gene expression appears sufficient for the induction of effector functions in T cell hybridomas, the surface expression of such molecules on conventionally derived T cell lines may be too low to ensure effective responses.38
The specific properties of the antibody used for antigen recognition may also be crucial for effective receptor stimulation. Signaling through native TCRs requires low-affinity binding to allow for serial triggering of a large number of these receptors,39 yet the majority of antitumor antibodies used in the clinic bind with high affinity. Whether such binding is optimal for the efficient lysis of tumor cells by T bodies remains to be determined. Similarly, the target antigen for chimeric receptor-mediated immunotherapy needs to be carefully chosen, as receptor binding by shed tumor antigens or downregulation of the target antigen represent potential mechanisms of immune system evasion by tumor cells. Ideally, the targets of chimeric receptors constitute part of the tumor cell phenotyping.
Conclusion
Cytotoxic T cells have produced clear benefits in the treatment of EBV- and CMV-associated diseases. As our understanding of tumor cell biology and of T cell function increases, and as the technology for gene transfer improves, we can look forward to broader applications of adoptive immunotherapy with these cells.
II. Immunotherapeutic Applications of Dendritic Cells
James W. Young, M.D.*
Allogeneic Bone Marrow Transplantation and Clinical Immunology Services, Division of Hematologic Oncology, Memorial Sloan-Kettering Cancer Center, 1275 York Ave., Box 553, New York NY 10021
Immunologists have long exploited the immune system to combat human disease. Cancer and some infections have proven elusive, however. Among the many reasons that cancer has challenged immune interventions are that most tumor antigens (Ags) are self-differentiation Ags to which apparent anergy exists,1 tumor cells and virally infected cells can be poor initiators as well as poor targets of immune reactions, and the tumor microenvironment can be inhibitory. Dendritic cells (DCs), the most potent leukocytes for initiating cellular immunity, may provide a solution to these challenges. DCs were originally discovered in mice a little more than a quarter century ago,2,3,4 but only in the past decade has it become feasible to generate either animal or human DCs in sufficiently large numbers and purity for large scale experimental and clinical investigation. With increased access to DCs has come a more universal realization of their potent immunostimulatory properties and a keen interest in using DCs as immune adjuvants for the treatment of human disease.
Dendritic Cells Are Specialized Antigen-Presenting Cells for Stimulating Cell-Mediated Immunity
The onset of an immune response requires not only Ag and lymphocytes, but also a third-party cell to present antigens to the lymphocytes. Long recognized as a requirement for so-called accessory or feeder cells in vitro, the exact cell type remained elusive until DCs were first purified and distinguished from other antigen-presenting cells (APCs) in mice, such as B lymphocytes and macrophages.2,3,4
DCs are uniquely specialized among all leukocytes to couple the presentation of Ag, bound to MHC molecules, with all the adhesive and costimulatory signals, collectively termed accessory molecules, required to initiate cellular immune responses. Unlike B cells that recognize soluble or native antigen and transform into antibody (Ab)-secreting plasma cells, TCRs can only recognize peptide fragments of antigen bound to MHC molecules on APCs. MHC molecules are of two types, class I MHC and class II MHC. For the most part, class I MHC molecules bind intracellular or endogenous antigens that have been cut into peptides in the cytosol. Class II MHC molecules bind extracellular or exogenous antigens that have entered the endocytic pathway of the APC. DCs also have a unique capacity to capture exogenous antigens from dying cells, which then access the class I MHC pathway for Ag presentation.5,6,7 This contrasts with the sequestration and clearance of phagocytosed Ag accomplished by macrophages. With few exceptions class I and II MHC-peptide complexes stimulate CD8+ CTLs and CD4+ helper T cells, respectively.
While DCs express abundant MHC molecules of both types, they also constitutively express large numbers of accessory molecules. The inducible increase in expression of these adhesive and costimulatory molecules coordinates with maturation and activation stimuli in culture. This mimics the in vivo capture of Ag by DCs in the periphery, followed by their maturation and migration to secondary lymphoid organs, where DCs complete their activation while stimulating T cells.8,9,10,11,12 It is this pairing of Ag/MHC presentation with potent accessory function that enables DCs to stimulate T cell immunity without additional adjuvants. DCs have therefore often been termed “nature's adjuvants” or “professional APCs.”
Nomenclature and Hematopoietic Lineages of Human Dendritic Cells
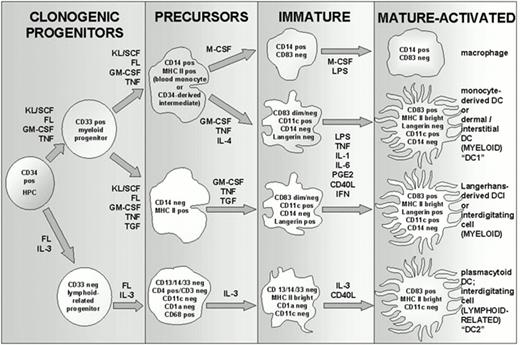
Successful cytokine-driven growth and differentiation of DCs from defined precursors has revealed that DCs comprise at least two types, myeloid-related and plasmacytoid or lymphoid-related, of which the myeloid-related DCs comprise at least two subsets (Figure 2). There is also a spectrum of differentiation within these divisions, from marrow-derived clonogenic progenitors, to circulating precursors in blood and lymphatics, to immature DCs resident in peripheral tissues, to mature or maturing forms in the thymus and secondary lymphoid organs.
Hematopoietic development of human dendritic cells.
All human DCs develop originally from CD34+ hematopoietic progenitor cells (HPCs) from either bone marrow, cord blood, or cytokine-elicited peripheral blood stem cells. Expansion is supported in vitro by factors like FLT-3-ligand (FL; c-fms-like tyrosine kinase ligand) and c-kit-ligand or stem cell factor (KL/SCF), with additional contributions from either granulocyte-macrophage colony stimulating factor (GM-CSF) or interleukin 3 (IL-3). GM-CSF supports myeloid DC expansion and differentiation, whereas IL-3 supports that of lymphoid-related DCs (also called plasmacytoid DCs, or IPCs, for natural interferon producing cells). Tumor necrosis factor-alpha (TNF) exerts pleiotropic effects, recruiting transferrin receptor positive CD34+ HPCs into cell cycle, at least partially suppressing G-CSF and M-CSF receptors early in CD34+ HPC differentiation, and later supporting terminal DC maturation. Additional cytokines like interleukin 4 (IL-4) and transforming growth factor-beta 1 (TGF) suppress CD14+ macrophage differentiation, and IL-4 is especially useful in this respect. TGF supports the differentiation of Langerhans cells (LCs), instead of dermal/interstitial DCs (DDC/IDCs). DDC/IDCs and monocyte-derived DCs (moDCs) are considered comparable progeny, with development of the former defined from CD34+ HPCs via a CD14+ bipotential intermediate and development of the latter defined from peripheral blood monocytes. Pertinent to approaches that require dividing cells for introducing antigen, like some forms of gene transfer, it should be noted that DC precursors as represented here are no longer in cell cycle. Note also that immature DCs require some form of terminal maturation and activation stimulus in order not to revert to an immature state or to an alternative differentiation pathway, usually supplied in vivo by bacterial products like lipopolysaccharide (LPS) or reactive T lymphocyte, but mimicked in vitro by certain cytokines as shown (including interleukin 1, IL-1; interleukin-6, IL-6; prostaglandin E2, PGE2; interferon-alpha and beta, IFN; CD40-ligand, CD40L). CD83 remains the best available marker of terminally matured DCs, and it is never expressed by committed macrophages. Additional maturation/activation epitopes are discussed in the text. Note that not all mature/activated LCs continue to express Langerin, but none of the DDC/IDCs or moDCs express this antigen. CD1a does not discriminate between LCs and DDC/IDC/moDCs, as it is expressed by all myeloid DC types.
Hematopoietic development of human dendritic cells.
All human DCs develop originally from CD34+ hematopoietic progenitor cells (HPCs) from either bone marrow, cord blood, or cytokine-elicited peripheral blood stem cells. Expansion is supported in vitro by factors like FLT-3-ligand (FL; c-fms-like tyrosine kinase ligand) and c-kit-ligand or stem cell factor (KL/SCF), with additional contributions from either granulocyte-macrophage colony stimulating factor (GM-CSF) or interleukin 3 (IL-3). GM-CSF supports myeloid DC expansion and differentiation, whereas IL-3 supports that of lymphoid-related DCs (also called plasmacytoid DCs, or IPCs, for natural interferon producing cells). Tumor necrosis factor-alpha (TNF) exerts pleiotropic effects, recruiting transferrin receptor positive CD34+ HPCs into cell cycle, at least partially suppressing G-CSF and M-CSF receptors early in CD34+ HPC differentiation, and later supporting terminal DC maturation. Additional cytokines like interleukin 4 (IL-4) and transforming growth factor-beta 1 (TGF) suppress CD14+ macrophage differentiation, and IL-4 is especially useful in this respect. TGF supports the differentiation of Langerhans cells (LCs), instead of dermal/interstitial DCs (DDC/IDCs). DDC/IDCs and monocyte-derived DCs (moDCs) are considered comparable progeny, with development of the former defined from CD34+ HPCs via a CD14+ bipotential intermediate and development of the latter defined from peripheral blood monocytes. Pertinent to approaches that require dividing cells for introducing antigen, like some forms of gene transfer, it should be noted that DC precursors as represented here are no longer in cell cycle. Note also that immature DCs require some form of terminal maturation and activation stimulus in order not to revert to an immature state or to an alternative differentiation pathway, usually supplied in vivo by bacterial products like lipopolysaccharide (LPS) or reactive T lymphocyte, but mimicked in vitro by certain cytokines as shown (including interleukin 1, IL-1; interleukin-6, IL-6; prostaglandin E2, PGE2; interferon-alpha and beta, IFN; CD40-ligand, CD40L). CD83 remains the best available marker of terminally matured DCs, and it is never expressed by committed macrophages. Additional maturation/activation epitopes are discussed in the text. Note that not all mature/activated LCs continue to express Langerin, but none of the DDC/IDCs or moDCs express this antigen. CD1a does not discriminate between LCs and DDC/IDC/moDCs, as it is expressed by all myeloid DC types.
The two types of myeloid-related DCs are Langerhans cells (LCs) in epithelial surfaces and dermal or interstitial DCs (DDC/IDCs) in the dermis of skin or interstitium of solid organs. DCs are most likely to encounter and capture Ag in the periphery, leading to their maturation and migration via afferent lymphatics into draining lymphoid organs. This culminates in the final activation of DCs as they stimulate incoming clones of Ag-specific naïve or resting memory T cells, which then exit to function as producers of helper cytokines or as CTLs in the periphery.
Evidence best supports the direct differentiation of LCs from CD34+ HPCs, whereas interstitial or dermal DCs develop from CD34+ HPCs via a CD14+ bipotential intermediate.13,14,15,16 This CD14+ intermediate is not clonogenic and is termed bipotential because it can alternatively develop into macrophages instead of DCs.14,15 The latter DC type is usually considered the homologue of the peripheral blood monocyte-derived DC (moDC), generated under the aegis of GM-CSF and IL-4 and the most readily DC type obtained by most investigators.
LCs move into the T cell-rich parafollicular areas where they are especially likely to encounter naïve T cells. In these sites they are termed interdigitating DCs, which can be nominally confused with interstitial DCs if the same IDC acronym is used. Although LCs have usually been thought of as immature DCs, a new specific marker, Langerin,17,18 still distinguishes some of the mature, activated LCs from the other myeloid-related interstitial or dermal dendritic cells.
Interstitial or dermal DCs migrate into germinal centers where they are termed germinal center DCs (GCDCs). GCDCs present processed antigen to memory T cells and additionally participate in humoral immunity by direct interaction with germinal center B cells and indirectly by stimulation of CD4+ T cells that provide cognate help for B cell differentiation.16,19
Recently, the terms DC1 and DC2 have been used to distinguish myeloid-related DC1 from lymphoid-related DC2, based on the propensity of each type to stimulate Th1 vs Th2 responses, respectively.20 The myeloid-related DC1 refers to the moDC or its counterpart in the CD34+-derived system, the dermal or interstitial DC. The term DC1 was not intended to encompass LCs, although LCs are also myeloid-related and meet many of the criteria for DC1. Most investigators are focusing on the myeloid-related DC and/or DC1 to stimulate acquired antiviral and antitumoral immunity, as these DCs stimulate Th1 responses that support CTL generation.
DC2 precursors (pDC2) are critical effectors of the innate immune system as they rapidly produce large amounts of IFN-α (type I IFN) in response to enveloped viruses, bacteria, and tumor cells, and upon terminal differentiation become professional antigen-presenting type 2 DCs for stimulation of Th2 responses.21,22,23 The tolerizing role that DC2 may play, either directly or indirectly, is of considerable interest, but is more pertinent to transplantation and autoimmunity than to the generation of CTL against viruses and tumors.24,25,26
Cytokine-Supported Development of Human Dendritic Cells for Immunotherapy
Most investigators use CD14+ blood monocytes to generate moDCs in vitro, as these nondividing precursors are more accessible than CD34+ HPCs. CD14+ monocytes also yield a higher percentage of DCs in vitro with fewer enrichment steps compared to CD3+-derived DCs, as CD14+ monocytes are only bipotent rather than multipotent like CD34+ HPCs. CD14+ blood monocyte cultures require IL-4 in addition to GM-CSF in order to suppress macrophage differentiation27 and develop into moDCs. IL-4 is similarly useful to suppress macrophage differentiation from the post-clonogenic CD14+ intermediate cells derived from CD34+ HPCs, and together with GM-CSF and TNFα supports DC development. Generally all DCs, but especially those sharing a common proximate precursor with macrophages, require a maturation stimulus (see below) in order not to revert to immature forms or even to macrophages, upon removal of primary cytokines.
Hematopoiesis is stochastic, even for DCs. CD34+ HPCs can therefore develop through the CD14+ bipotential intermediate into dermal/interstitial DCs (counterparts of the moDCs) or directly into LCs, the other myeloid-related type of DC.13,14,15 In the presence of cytokines that support myeloid differentiation in general and DC differentiation in particular, both pathways are operative in bulk cultures (Figure 2). Macrophages, granulocytic cells, and their precursors also develop from CD34+ HPCs among the myeloid progeny that include both types of DCs, which require further enrichment for higher purity.
Two main requirements for immunotherapeutic uses of human DCs in vivo are the avoidance of xenogeneic Ags derived from fetal calf serum (FCS)-supplemented cultures and the generation of higher percentages of DCs in vitro. A variety of serum-free media are commercially available as alternatives to FCS for ex vivo culture. Most if not all components are treated as proprietary information by the manufacturers and are unfortunately not disclosed to investigators. Selection of a particular product is therefore entirely empiric, as is the use of human serum or plasma by some investigators. One should not underestimate the challenges to corroborating comparable phenotypic and functional maturation and activation of the final DC product, to what one obtains in FCS-supplemented media. Compared to FCS-supplemented media,28 CD34+ HPC expansion is always lower in serum-free media. However, investigators can better control the cytokine content of the medium when using serum-free products.
Two cytokines help enrich the percentage of DCs in the final products. IL-4 has proven useful in suppressing macrophage differentiation from the CD14+ bipotential intermediates that arise from CD34+ HPCs, just as it exerts a comparable effect on CD14+ blood monocyte.27,29,30 IL-4 therefore increases the purity of blood monocyte-derived DCs as well as that of the CD34+-derived counterparts, the dermal/interstitial DCs. TGF-β, first identified in mice as a critical cytokine for LCs,31 enriches LC differentiation of human CD34+ HPCs in serum-free culture conditions in vitro.32,33,34,35
Proceeding from original studies in mice, FLT-3L (c-fms-like tyrosine kinase ligand 3) also mobilizes both myeloid-related and lymphoid-related DCs in vivo in humans.36,37 FLT-3L can increase circulating human myeloid-related DCs by a mean 44-fold and lymphoid-related DCs by a mean 12-fold, with little toxicity.37 Physical methods can then enrich the DCs from leukopheresis products.38,39,40,41 FLT-3L by itself does not have this effect on CD34+ HPC expansion in vitro, so other factors not yet identified must contribute to its effect in vivo.
Maturation and Activation of Myeloid-Related DCs
Antigen capture and processing versus antigen presentation and T cell stimulation are processes that are dynamically related to the maturation state of DCs.42,43 Mature DCs are more stimulatory of Ag-specific T cells than are immature DCs. This distinction sometimes blurs in vitro, as DC maturation is asynchronous, and sufficient numbers of mature DCs are usually available among a stimulator population to begin activating T cells, which in turn mature the remaining immature DCs.10,11,12
An apparent paradox also involves the migratory capacity of DCs, even after maturation, as migration has always been considered a property of immature DCs/LCs. However, early clinical trials have shown that mature DCs injected peripherally are effective in inducing immunity, indicating that migration toward secondary lymphoid organs is not lost with maturation.44,45 Recent mouse studies have further corroborated this and demonstrated the importance of maturation in the formation of immunogenic MHC-peptide complexes when DCs are pulsed ex vivo.46 Chemokine receptors are also regulated in relation to maturation and support trafficking to secondary lymphoid organs.47,48,49,50
Additional stimuli in vitro ensure that differentiated DCs maintain phenotype and function rather than revert to immature forms or follow alternative differentiation pathways upon cytokine withdrawal (Figure 2). These stimuli can be in the form of bacterial products such as lipopolysaccharide (LPS) or inflammatory cytokines (e.g., IL-1, IL-6, TNFα, PGE2, type I IFN α/β).30 ,51,52,53,54 Cytokines secreted by activated macrophages can also support terminal and irreversible differentiation of monocyte-derived DCs.55 However, standardization between donors can be difficult, leading some investigators to prefer a recombinant cytokine cocktail that reproduces the effects of macrophage-conditioned medium.54
CD40-ligand (CD40L or CD154) is also a powerful stimulus for DCs, as evidenced by an activated phenotype, increased T cell stimulatory capacity, and secretion of IL-12.8,9,56 Soluble CD40L binding to CD40, which is upregulated on mature DCs, mimics the full activation of DCs accomplished by their initial interactions and crosstalk with CD4+ T cells at the onset of an immune response.10,11,12 Accordingly, while most investigators now accept that mature DCs are optimal for clinical immunotherapeutic applications, DCs already fully activated ex vivo may or may not be. Final activation might best be completed in vivo after administration of an Ag-loaded, mature DC vaccine. It is therefore important not to consider maturation and activation as necessarily synonymous or interchangeable in designing DC immunization trials.
It is also worth noting factors that inhibit the maturation and activation of DCs. Immature DCs are particularly susceptible to inhibitory factors like IL-10 and vascular endothelial growth factor (VEGF), whereas terminal maturation of DCs renders them insensitive to this inhibition.57,58 These inhibitory factors are abundant in the tumor microenvironment and may account in large part for the inefficacy of local DCs to stimulate antitumor immune responses, as well as the apparent inability of inflammatory mediators released by necrotic tumor tissue to mature DCs into potent immunogens. This also underlies the immunologic thinking that the controlled application of mature, tumor Ag-loaded DCs generated ex vivo may circumvent these limitations.
Finally, upon successful maturation of myeloid-related DCs, there are important properties that are always useful to distinguish them from their less mature precursors and from other leukocytes. The circumferential cytoplasmic veils or lamellipodia become more prominent with maturation in vitro. Mature myeloid-related DCs lack any significant expression of epitopes specific to macrophages (CD14, c-fms/CD115) or lymphocytes (CD3, CD4, CD8, CD19, CD20, CD16, CD56). Mature DCs increase expression of CD83,59 which is still the best available marker of maturation shared by LCs and DDC/IDC/moDCs alike. CD83 can also be detected intracellularly as evidence of commitment to the DC lineage, even before surface expression develops. Mature, myeloid-related DCs also express p55/fascin, which is an actin bundling protein,60,61 abundant class II MHC, B7-2/CD86 more so than B7-1/CD80,62 and DC-lysosome-associated membrane glycoprotein (DC-LAMP).63 CD45RO, nominally a marker of memory T cells, is also a marker of activated LCs and DDC/IDC/moDCs. IL-2R/CD25 is also expressed by certain activated DCs.
All of these mature DCs, be they LCs or DDC/IDC/moDCs, are potent stimulators of T cells. Comparable T cell proliferation in vitro, used as a measure of the stimulatory activity of an APC population, requires at least 10- to 100-fold more APCs such as B cells, macrophages, or bulk peripheral blood mononuclear cells, than is required of mature DC stimulators.42,43
Challenges and Potentials for Using Human Dendritic Cells as Immunologic Vaccines In Vivo
Initial clinical trials of human DC vaccines are generating encouraging preliminary results both in patients with cancer and in normal volunteers.41,44,45,64 Important considerations in the design of such human trials include antigen selection, methods for introducing the antigen into MHC class I and II processing pathways, methods for isolating and activating dendritic cells, and route of administration. To date there is no clear consensus on these points, although the trials that carefully control and monitor these parameters are most likely to yield evaluable results that will guide future therapy.
Many investigators are focusing on malignant melanoma to validate DC immunotherapy because immunologic responses associated with disease activity have been previously documented in this malignancy. There are also defined immunodominant peptides derived from melanoma or melanocyte differentiation Ags, for which there are known HLA restrictions for peptide Ag presentation. Heteroclitic peptides and/or xenogeneic peptides with substantial homology to human melanoma peptides are also proving useful to generating tumor immunity.65,66,67
Other means of loading Ag apart from peptide pulsing are being explored in both animal and human models. These include peptide-pulsed, DC-secreted or -shed exosomes that carry class I and II MHC-Ag complexes and T cell costimulatory ligands.68 Gene transfer by a variety of methods is also being studied.66,69,70,71,72,73 DC and breast cancer cell heterokaryons have generated class I MHC-restricted CTL against autologous breast tumors.74 Another approach involves cross-priming or cross-presentation by DCs, whereby DCs immunize autologous T cells to Ag derived from a third-party or even MHC-incompatible cell. This pathway by which dying cells can access the class I MHC compartment for Ag presentation seems unique to dendritic cells. Macrophages in contrast phagocytose and sequester similar Ag from dying cells for the purpose of Ag clearance. Cross-priming and cross-presentation have been carefully studied in vitro with human moDCs5,6 and are operative in inducing CTL responses against tissue-restricted Ags at least in naturally occurring breast and ovarian cancer.7 Heat shock proteins may be critical in moving Ag from dying cells into the class I MHC Ag presentation pathway of DCs, and they have been shown to enhance immune responses against MHC-presented peptides.75,76
Gene transfer, DC-tumor heterokaryons, and the uptake of dying cells are all examples of loading DCs with tumor Ags where the specific Ag, immunodominant peptide, and/or HLA restricting allele(s) may be unknown. This allows the DC to tailor antigenic peptides for presentation on its own MHC molecules. These methods also facilitate the coupled presentation of class I and II MHC-restricted Ags that elicit CD4+ T cell help, which is important to the augmentation of CD8+ cytolytic T cell activity and to the generation and maintenance of immune memory.10,11,12,72
The route of DC immunization in current and planned DC vaccine trials varies between intradermal, subcutaneous, intravenous, or a combination. To date the choice reflects investigator bias or extrapolation from mouse studies. A recently published DC vaccine trial in melanoma, however, found that melanoma-specific immune responses documented after initial cutaneous immunizations declined after subsequent intravenous immunizations in the same patients.44 It is therefore important that the route of immunization be held constant in the design of clinical trials where other variables like type of DC, dose, and/or type of antigen are being evaluated. Specific evaluation of the optimal immunization route would conversely require holding some of these other variables constant.
Careful documentation of immune responses to DC tumor vaccines requires more than assessing clinical outcomes. Sensitive measurements to detect increases in T cell reactivity after DC vaccination are now available. These include ELISpot assays, which are ELISA-based assays for the detection of cytokine secretion by T cells. ELISpot assays have proven most reliable so far in detecting IFN-γ secretion by human T cells, the specificity and relevance of which to CTL activity is increased by evaluating purified CD8+ T lymphocytes rather than bulk T cell populations.
Another assay that is less laborious and probably more sensitive than limiting dilution analyses is tetramer staining to detect changes in the precursor frequency of antigen-specific lymphocytes.77 Here the Ag and restricting MHC allele must be known, as these components form a fluorochrome-tagged, tetrameric complex that binds Ag-MHC-specific, reactive T cells. Changes in the frequency of reactive T cells before and after DC immunization can thus be quantified cytofluorographically based on T cell binding to the tetramers. However, one may detect tetramer-positive T cells solely because they express the corresponding T cell receptor, while these T cells may or may not execute effector cytolytic functions.78 In some respects, though perhaps less sensitive, the standard 51 Cr-release assay therefore remains the gold standard to measure actual target cell killing.
Conclusion
Investigators now have the tools to generate DCs for the control and manipulation of immune responses against human disease. With increased access to these cells has come an explosion in the understanding of their unique properties at both cellular and subcellular levels. The DC system is far more complex than originally expected. However, this complexity provides a variability and adaptability that meets the demands of the various immunologic functions required of these uniquely potent antigen-presenting cells in initiating and controlling T cell-mediated immunity. There is great promise in the application of DCs as immune adjuvants for treating cancer in early clinical trials. There are still many challenging unknowns, however. These will only be resolved by carefully controlled protocols that account for the types of DCs, their maturation and activation states, doses and routes of immunization, the nature of the Ag and its presentation by class I and/or II MHC, and well-documented assessments of immunologic responses to the DC vaccine interventions.
III. Alloimmune T Cells for Adoptive Therapy of Hematological Malignancies
Prof. Els Goulmy*
Leiden University Medical Center, Dept. of Immunohematology and Blood Transfusion, Building 1, E3-Q, PO Box 9600, 2300 RC Leiden, The Netherlands
Allogeneic stem cell transplantation (SCT) not only restores patients' hematopoiesis but also possesses a curative graft-versus-leukemia (GVL) effect. Several clinical studies have indicated that the eradication of leukemia could be related to the presence of alloreactive T cells in the grafted bone marrow. The involvement of donor-derived alloreactive T cells in the GVL effect is clearly demonstrated by the higher relapse rates in patients who receive T cell-depleted SCT compared to those receiving non-T cell-depleted SCT. The lowest GVL effect is observed in SCT between identical twins, in whom donor/recipient alloreactivity is absent. Another indication of the involvement of donor-derived allogeneic T cells in the GVL effect is the successful use of donor lymphocyte infusions (DLI) as adoptive immunotherapy for chronic myeloid leukemia (CML) relapsing after SCT. Clinical response rates exceeding 80% have been achieved in several studies. The outcome of the DLI treatment is strongly associated with the development of GVHD.
Thus, one may conclude that alloreactive donor T cells are involved in anti-leukemia activities. The effector mechanisms may involve leukemia-specific T cells, NK cells or T cells recognizing HLA and non-HLA antigenic disparities, e.g. minor histocompatibility antigens (mHags) between SC donor and recipient. The supposition that donor T cells are involved in the GVL effects and that mHag disparities between HLA-matched donor and recipient facilitate this effect is plausible, since the GVL-associated alloimmune response is often not restricted to the leukemia cells. This paper focuses on the donor anti-recipient alloantigen-specific T cell responses in relation to their putative clinical application in adoptive immunotherapy of hematological malignancies.
Targets for Adoptive Immunotherapy of Hematologic Malignancies
Target antigens to be used in adoptive immunotherapy should fulfill at least three prerequisites for successful hematological tumor reactivity. The target antigens must be: 1) hematopoietic system specific; 2) functionally membrane expressed; and 3) immunogenic. In view of the relatively high leukemia relapse rate following autologous SCT1 and after syngeneic (between identical twins) SCT,2 the targets of choice for adoptive T cell therapy are allo (i.e. non-self) target molecules with relative specificity for the leukemic cells. Three types of potential allo target antigens for adoptive immunotherapy are discussed below.
Allo Targets for Adoptive Immunotherapy Hematological Malignancies
Chronic myeloid leukemia-specific BCR-ABL oncoprotein target antigens.
One of the most elegant examples in applied immunology is the clinical success of DLI for CML relapse after BMT.3,4 These observations provide a strong basis for in vivo donor allogeneic T cell reactivity against the leukemia. Moreover, infusion of lower numbers of donor leukocytes results in GVL without high incidence of GVHD.5 Therefore, the BCR/ABL CML-specific gene products would serve as the ideal target antigen for adoptive immunotherapy. Several efforts have been made to analyze the putative immunogenic BCR/ABL fusion protein peptides for their HLA class I and II binding capacities and their in vitro induction of allogeneic BCR/ABL peptide-specific T cells. Indeed, in selected cases both MHC class I and II restricted BCR/ABL peptide-specific T cell responses could be obtained. Disappointingly however, as yet only limited evidence has been presented that processed fusion protein peptides are recognized on the membrane of CML cells.6,7,8,9,10
Leukemia-associated target antigens
Occurrence of GVL without any sign of GVHD in some CML patients indicates that, clinically, GVHD can be separable from GVL. Thus, in principle it must be possible to generate leukemia-reactive T cells in vitro with relative specificity for the leukemic cells. Leukemia cell-reactive T cells have been generated ex vivo from normal donors and from patients after allogeneic BMT.14,15,16,17,18,19 Whether the leukemia cell reactivity in these studies is due to tissue-restricted mHag remains to be investigated. Another point of consideration in these studies is that the selective leukemia reactivity observed in the primary cell cultures may be transient or not genuinely leukemia specific. In several studies, T cells initially observed to selectively recognize leukemic cells appeared also to recognize normal target cells. It is unclear whether leukemic cells express unique antigens that can induce a leukemia cell-specific T cell response. Addressing this issue has been difficult because leukemic cells rarely induce a significant T cell response in vitro. This may be caused by the absence of costimulatory molecules such as CD80. Recent studies suggest that the T cell stimulatory properties of leukemic cells can be upregulated. For instance, upon activation via CD40, B cell lymphoma or leukemia cells express high levels of HLA and CD80/CD86 molecules and become efficient APCs for alloreactive T cells.20,21 Moreover, CD40-stimulating pre-B leukemia cells have been successfully used for the in vitro induction of leukemia-reactive autologous CTL from several pre-B leukemia patients.22 In an attempt to potentiate antigen presentation by AML cells, we generated leukemia-reactive CD4+ T cells from the HLA-identical sibling donor of an AML patient using CD80-transfected leukemic cells as stimulator cells.23 While some T cells preferentially recognized leukemic cells, the majority of the leukemia-reactive T cell clones did not discriminate between leukemic and non-leukemic cells, indicating that the target antigens are patient-specific mHags present on both leukemic and non-leukemic cells.23 Ostankovitch and co-workers generated T cell clones against a pool of peptides eluted from leukemia blasts from an AML patient. These donor-derived T cell clones showed HLA class I-restricted AML peptides and AML blast cell specificity.24 The antigen specificity of the effector T cells in the studies summarized above is unknown. Nonetheless, it is possible to generate ex vivo leukemia-reactive CTLs from the HLA-identical SC donor and to successfully use them to treat accelerated phase CML after SCT.25 Naturally, identification of the leukemia-associated target antigens that are recognized by these donor allogeneic T cells is crucial.
Hematopoietic system-specific target antigens
Relapse after HLA-matched SCT: The treatment of patients with recurrent leukemia is still difficult. DLI for relapsed ALL and AML patients has low rates of success.26,27 The use of hematopoietic system-specific target antigens may serve as a potential source for immunotherapy of these types of hematological tumors. As mentioned earlier, the three prerequisites for successful immunotherapy of hematological malignancies are hematopoietic system specificity; functional membrane expression; a target antigen capable of inducing an allo immune T cell response.
Typical examples that meet the criteria mentioned above are mHags. This proposition is based on the knowledge that mHag disparities between HLA-matched SC donor and recipient are capable of inducing alloresponses that participate in GVL reactivity post SCT.28 Absence of these mHag-induced alloreactivities may result in relapse of leukemia after SCT.29
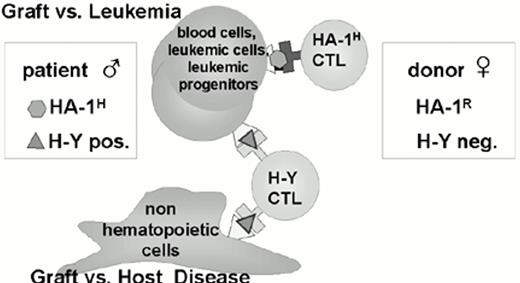
mHags are peptides from intracellular proteins that are of limited polymorphism and may be encoded by genes on the Y-chromosome or by autosomal genes. Proteins that differ in their amino acid sequence can give rise to antigenic differences, which can be recognized by alloreactive MHC-restricted T cells.28 mHags show either ubiquitous or restricted tissue expression.30 We investigated the functional HLA-mHag ligand membrane expression of a limited number of mHags using our mHag-specific cytotoxic T cell clones. These studies revealed that all the mHags we investigated (H-Y and HA-1 to HA-5) are expressed on hematopoietic progenitor cells,31 on clonogenic leukemic precursor cells32 and on circulating leukemic cells of lymphocytic and myeloid origin.33 In summary, the tissue expression of some mHags (HA-1 and HA-2) is limited to the hematopoietic system only, whereas other mHags (H-Y and HA-3) are ubiquitously expressed.30 Evidently, the mHags with tissue distribution restricted to the hematopoietic system are candidates for adoptive immunotherapy of hematological malignancies. Our local candidates to date for immunotherapy are mHags HA-1 and HA-2 since their restricted expression to the hematopoietic system has been functionally demonstrated. Moreover, the immunogenic polymorphism of HA-1 and HA-2 beyond HLA has been clearly demonstrated.28 The chemical characterization of HA-1 and HA-2 peptides34,35 is crucial for the ex vivo induction of CTLs with defined hematopoietic and patient specific activity.36
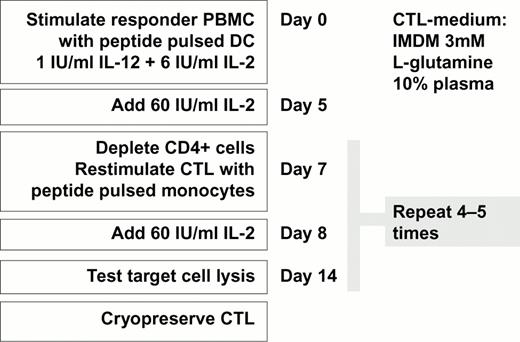
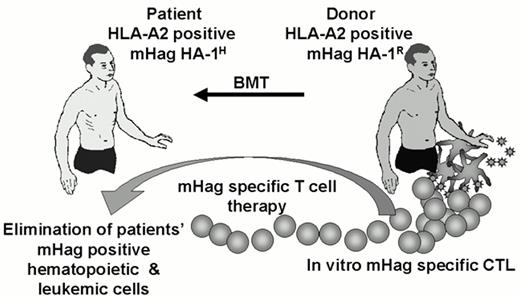
As demonstrated in the flow chart (Figure 3), we developed in vitro good manufacturing practice (GMP) grade protocols of HA-1- and HA-2-specific CTLs for adoptive immunotherapy of relapsed leukemia after HLA-matched, but HA-1- and/or HA-2-mismatched SCT.36 A phase I/II study has been initiated at our academic center, in which BM donor-derived mHag-specific CTLs will be infused into relapsed patients if donor engraftment has reached 50% or more. It is expected that most recipient hematopoietic APCs capable of initiating GVHD will then be replaced by donor APCs. This chimeric status of the patient is crucial, since we have previously demonstrated that HA-1 disparity between patients and donors is associated with the development of GVHD in adults.37 It is expected that most recipient hematopoietic cells will be replaced by donor type cells by day 50 to 60 post SCT. Since host-derived APCs are responsible for the initiation of GVHD,38 adoptive transfer of donor-derived HA-1- and/or HA-2-specific CTLs to a host already reconstituted with donor APCs should have a low risk of GVHD. Alternatively, one may transduce the HA-1- and HA-2-specific CTLs with a suicide gene that will make the in vivo elimination of cells possible if adverse events occur.39 As outlined in Figure 4, upon transfusion, of for example HA-1H-specific donor-derived CTLs, these CTLs will eliminate HA-1H-positive patients' hematopoietic and leukemic cells, while the mHag HA-1R-mismatched marrow of the BM donor will be spared. The advantage of adoptive immunotherapy with CTLs specific for hematopoietic system restricted mHags, as opposed to ubiquitously expressed mHags such as H-Y, is the hematopoietic system-restricted specificity (see Figure 5). Naturally, the applicability of HA-1- and HA-2-specific CTLs is rather limited because of the requirement for patient/donor pairs that are HLA-A2 and HA-1 or HA-2 mismatched. The first series of clinical results will function as the proof of principle and will determine whether there is a need to search for more hematopoietic system-specific mHags.
Adoptive immunotherapy of relapsed leukemia with CTLs specific for hematopoietic system-restricted mHags.
Adoptive immunotherapy of relapsed leukemia with CTLs specific for hematopoietic system-restricted mHags.
HA-1 is hematopoietic system-restricted; H-Y is ubiquitously expressed.
Recently, Dolstra et al described anti-host mHag-specific CTL responses that show leukemia-associated recognition.40 The CTL isolated after HLA-identical BMT recognized a mHag expressed solely on B-acute lymphoblastic (B-ALL) cells and EBV-LCL.40 The HB-1 peptide has been identified,41 providing the possibility of generating in vitro HB-1 peptide-specific CTLs. Warren et al also described mHag-specific CTLs that lyse hematopoietic cells but not fibroblasts.42 Similarly, Yazaki et al43 reported on a novel mHag with apparent hematopoietic system-restricted specificity. Once additional information on the peptides of these mHags become available, in vitro mHag peptide-specific CTL induction protocols, as described for HA-1 and HA-2, can be executed.
Theoretically, any polymorphic hematopoietic system-restricted protein can give rise to mH peptides and thus create potential targets for alloimmune responses. A good example is the myeloid tissue-restricted proteinase 3 protein. Polymorphic regions have been identified in which peptides are present that bind to HLA-A2.44 It is not yet know whether these proteinase 3 polymorphic peptides are capable of inducing alloimmune T cells.
Relapse after HLA-mismatched SCT
So far, mHag incompatibilities have been discussed as the allo targets in the HLA-matched SCT setting. Because the numbers of HLA-mismatched SCT are steadily increasing, our current focus is the use of hematopoietic system-specific mHags in the context of HLA partially mismatched SCT for the treatment of leukemia relapse. Here, the patients' mismatched HLA molecules, which are absent in the SCT donor, will be used as allo targets and as antigen-presenting molecules for hematopoietic system-specific mHags. This proposal is based on recent work from other laboratories and ourselves and will be briefly outlined below.
It is known that alloreactive T cells can show specificity to tissue-specific peptides presented by mismatched allo-HLA antigens. Sadovnikova and Stauss have generated allo-MHC-restricted T cells that specifically recognize tumor-cell associated antigens mdm-2 and cyclin-D1 using peptide-loaded antigen-processing defective cells as stimulator cells for MHC-incompatible T cells.45, 46 Similarly, Munz et al stimulated PBMC from HLA-A2- and HLA A3-negative individuals with synthetic peptide libraries fitting HLA-A2 or HLA-A3 motifs presented on HLA-A2- or HLA-A3-positive TAP-deficient cells. They have demonstrated that peptide-specific allo-restricted CTLs comprised up to 50% of the total alloreactive CTLs.47 By stimulating the T cells of an HLA-DRw25-positive healthy individual with AML cells of an HLA class II-mismatched (i.e. HLA-DRw26) patient, we generated an HLA-DRw26-restricted CD4+ T cell clone that exclusively recognizes leukemic cells and CD34+ progenitor cells but not peripheral blood cells or non-hematopoietic cells.48 This allo-HLA-restricted T cell clone recognizes an hematopoietic system restricted, developmentally regulated antigen. Thus, alloreactive CTLs with specificity for hematopoietic system-specific antigens exist and can be generated in vitro. Concordantly, Gao et al demonstrated the in vitro generation of “allo-HLA/Wilm's transcription (WT1) factor peptide” specific CTLs. The allo HLA/WT1 peptide-specific CTLs show restricted leukemic cell lysis.50
We have also generated HA-1 peptide-specific CTLs from HLA-A2-negative individuals, using HA-1 peptide pulsed HLA-A2-positive T2 cells as stimulator cells. Because of the class I HLA-A2 difference between responder and stimulator cells, one can expect broad anti HLA-A2 T cell responses. Therefore, antigen-specific stimulation and subsequent selection by limiting dilution or by HLA-A2/HA-1 specific tetramers is required. The feasibility of specific staining of mHag specific CTLs with HLA class I/mHag peptides tetrameric complexes was demonstrated in our laboratory.49 In addition, we recently observed that HLA class I/mHag peptide tetrameric complexes facilitate monitoring of in vitro T cell cultures and select high avidity HA-1 and HA-2 specific CTLs for adoptive immunotherapy (manuscript submitted for publication). Based on the latter successful application of HLA class I/mHag tetrameric complexes, we sorted tetramer staining CD8-positive cells from the alloreactive T cell line. After expansion, the tetramer sorted cells showed significant lysis of both HLA-A2/HA-1 peptide pulsed target cells and target cells that express that natural HLA-A2/HA-1 membrane complex, whereas no lysis was detected against HLA-A2/HA-1-negative target cells. These preliminary results illustrate the feasibility of generating allo-HLA-A2-restricted HA-1 specific CTL clones by stimulating HLA-A2-negative responder cells with HLA-A2-positive/HA-1 peptide pulsed stimulated cells (The Hematology Journal; in press).
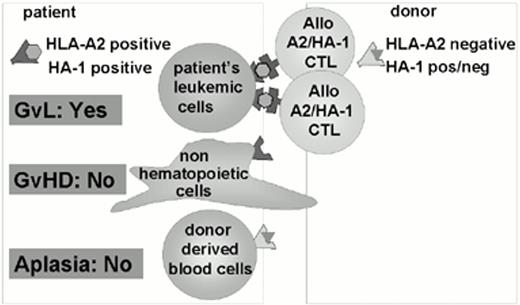
Immunotherapy with CTLs directed at patient's HLA-mismatched hematopoietic system-specific antigens should basically have identical in vivo results as described above for the HLA-matched mHags-mismatched protocol. Adoptive immunotherapy with CTLs specific for “allo-HLA-HA-1 specific ligand” in HLA-mismatched SCT will result in the GVL effect directed at the allo HLA-A2/HA-1 complex on the patient's leukemic cells (Figure 6). There will be a low risk of GVHD because of the absence of the hematopoietic system-specific HA-1 peptide on non-hematopoietic tissues. Moreover, no marrow aplasia should occur because the donor-derived hematopoietic cells do not express the patient's allo HLA-A2 target molecule.
Adoptive immunotherpay with CTLs specific for “allo HLA/HA-1-specific ligand” in HLA-mismatched SCT.
Adoptive immunotherpay with CTLs specific for “allo HLA/HA-1-specific ligand” in HLA-mismatched SCT.
Thus, hematopoietic system mHags can serve as components for adoptive immunotherapy of relapsed hematologic malignancies in both HLA-matched and HLA-mismatched SCT. In the former setting, the mHag mismatch is used as a target molecule; in the latter setting the HLA mismatch combined with hematopoietic mHags is used as a target molecule for hematopoietic tumor-specific cellular immunotherapy. The latter strategy may allow a variety of peptides to be derived from hematopoietic system specific proteins. The successful induction of the “allo HLA/WT1” specific CTLs50 together with our results on the generation of “allo HLA/HA-1” specific CTLs clearly underlines the feasibility of this approach for adoptive immunotherapy of hematological malignancies after HLA mismatched SCT.