Abstract
This paper examines the evidence available to guide treatment decisions in three areas of Hodgkin's lymphoma management. In Section I Dr. Evert Noordijk describes evolving strategies for patients with early stage disease outlining the eras during which the focus has changed from initially accomplishing cure through refining and intensifying the treatment to one of maximizing cure rates and finally into a patient-oriented era in which the twin goals of maintaining high rates of cure and minimizing late toxicity are being achieved. In Section II Dr. Sandra Horning reviews the way in which the cooperative groups of North America and Europe have built upon initial observations from single centers to assemble the trials that have defined the treatment for advanced stage Hodgkin's lymphoma. Over a period of almost three decades, these well-constructed trials have defined a current standard of treatment, ABVD chemotherapy and are now investigating innovative approaches to move beyond this standard. She also indicates the need to appreciate diagnostic factors and the implications of prognostic factor models for the design and interpretation of clinical trials. In Section III Dr. Joseph Connors summarizes the evidence available to inform our choice of treatment for the uncommon but important entity of lymphocyte predominance Hodgkin's lymphoma. Once again, the guidance that can be derived from carefully conducted clinical investigation is used to address the issues surrounding choice of treatment, reasonable monitoring in long term follow-up and the clear-cut need to base diagnosis on objective immunohistochemical evidence.
I. Optimal Management of Early Stage Hodgkin's Lymphoma
Evert M. Noordijk, MD*
Dept. of Clinical Oncology, Div. of Radiation Oncology, Leiden University Medical Center, P.O. Box 9600, 2300 RC Leiden, The Netherlands
Although Peters reported cures in selected patients as early as 1950,1 before 1960 the treatment of Hodgkin's lymphoma was usually considered palliative. Since 1960, curative treatment of Hodgkin's lymphoma has developed rapidly. Three time periods can be distinguished:
1960-1985, the disease-oriented period, in which the main objective was the improvement of overall survival
1985-1995, the treatment-oriented period, in which disease free survival, relapses and salvage therapy also became important and the late effects of treatment became of major concern
1995-present, the patient-oriented period, in which minimal curative therapy and quality of life are the main issues.
1. 1960-1985
In the early sixties, four factors attributed to the growing possibilities for curative treatment:
improvement of approaches to staging, using systems based on understanding of the spread of disease and with methods such as lymphography and staging laparotomy
better radiation equipment (cobalt machines and linear accelerators), allowing the delivery of higher doses and the application of extended fields, such as mantle field and inverted Y field
development of effective chemotherapy-combinations
discovery and validation of prognostic factors for relapse and survival, leading to tailoring of the treatment to the burden and extent of the disease
a. Staging
In 1971, the Ann Arbor staging system came into use.2 It had developed from the three-stage system of Peters3 and the clinical four-stage Rye-system.4 It took into account the absence or presence of general symptoms (A or B), the presence of extranodal spread (E) and the findings of staging laparotomy (CS versus PS). Much later, in the Cotswolds-meeting,5 bulk was added as a prognostic factor (X).
Staging laparotomy was first reported by Glatstein et al6 and became almost a standard procedure in the seventies and early eighties, predominantly in the US, but not everywhere in Canada and Europe. It is remarkable that already in the H2-trial of the EORTC (1972-1976), the equivalence of spleen removal and spleen irradiation was shown.7 In the mean time, before these results had been reported, in the EORTC H5-F trial (1977-1982) staging laparotomy was mandatory.8 In the EORTC H6-F trial (1982-1988), the comparison of staging laparotomy and clinical staging became subject of study. Clinical staging appeared to be similar to laparotomy, considering relapse free survival as well as overall survival, while laparotomy and splenectomy proved to have some serious drawbacks.9 Since then, in the EORTC Lymphoma Group, staging laparotomy was no longer used. Others10– 12 have also reported adverse effects of staging laparotomy, such as an operative mortality of 0.5-1% and miscellaneous infectious, cardiac and pulmonary complications. At present, the procedure has been abandoned almost everywhere.
As will be argued later, this does not mean that spleen involvement is no longer of importance. Without surgical staging, treatment of the upper abdomen with either irradiation or combination chemotherapy will always be necessary.
b. Better radiotherapy
The special clinical patterns of Hodgkin's lymphoma, with it's tendency to spread to adjacent lymph node areas, had been recognized for years13,14 and have been reconfirmed recently in an elegant study by Roth et al.15,16 The possibilities of giving prophylactic irradiation had already been postulated by Peters,3 but with the introduction of megavoltage radiotherapy the techniques to treat ‘extended fields’ really became available. With the development of mantle field irradiation, subtotal nodal irradiation, total nodal irradiation and total lymphoid irradiation, radiotherapy became the cornerstone of the treatment of Hodgkin's lymphoma.17 In 1962, the first randomized trial comparing involved field irradiation with extended field irradiation was begun at Stanford.18
Megavoltage equipment brought another advantage: the possibility of delivering a sufficient dose to deeper parts of the body. Based on a dose-effect relationship, the tumoricidal dose was considered 4000-4400 rads in Stanford.19 Peters in Toronto gave only 3500 rads to involved areas and 2500 rads to adjacent, apparently uninvolved lymph node areas.3 These doses were used throughout the first time period, but came under question in more recent years; high doses (40 Gy) only for bulky disease, lower doses (30-35 Gy) for non-bulky disease and even lower doses (25-30 Gy) for subclinical disease have been suggested.20– 25
c. Effective chemotherapy
In the years before 1960, just like radiotherapy, chemotherapeutic agents were used only for palliation in Hodgkin's lymphoma. Nitrogen mustard, cyclophosphamide, vinblastine and procarbazine were all used separately and mainly in advanced disease. In 1964, the first Hodgkin's trial of the EORTC, the H1-trial, investigated the role of vinblastine as an adjuvant treatment in stage I and II disease, testing it randomly against no further treatment after 40 Gy mantle field or inverted Y irradiation. The vinblastine, 10 mg given every week for two years, improved relapse free survival and also had some effect on overall survival.26
In 1964, the MOPP (nitrogen mustard, vincristine, procarbazine, prednisone) scheme was conceived, being the first scheme that cured patients with advanced disease.27 It was followed some years later by the Italian ABVD (doxorubicin, bleomycin, vinblastine, dacarbazine) scheme, first considered as a non-crossresistant salvage combination for MOPP, but later proving to be superior in first line.28
Both schemes were tested in this time period as treatments for patients with ‘unfavorable’ stages I and II Hodgkin's lymphoma. In the GELA (Groupe d'Etudes des Lymphomes de l'Adulte) study (1972-1979), patients were treated up-front with 3 or 6 courses of MOPP, followed by surgical restaging with splenectomy and extended field radiotherapy. Three MOPP courses proved to be as effective as 6 courses in sterilizing splenic disease and achieving high survival rates.29
In two EORTC trials, the H5U trial and the H6U trial, the MOPP and ABVD schemes were also tested in early stage Hodgkin's lymphoma patients. In the H5U trial (1977-1982), 6 courses of MOPP + mantle field irradiation (40 Gy) were randomly compared to a total nodal irradiation of 40 Gy. The combined modality therapy resulted in a superior relapse free survival, but not in a better overall survival.8 In the H6U trial (1982-1988), 6 courses of MOPP (+ mantle field) were randomly compared to 6 courses of ABVD (+ mantle field). Again, the ABVD arm was superior in relapse free survival but not in overall survival.9 Since then, MOPP alone has no longer been used in any EORTC trial. ABVD is being used as the standard-arm in the current H9U trial.
d. Prognostic factors
Prognostic factors are variables measured in individual patients, offering a partial explanation of the heterogeneity observed in the outcome of Hodgkin's lymphoma. The factors may be used to predict outcome (response, relapse free survival, overall survival) and therefore may be used to define risk groups that can be selected (stratified) for different treatments. There are tumor-related and patient-related factors.30–,32 In the EORTC, the H1 and H2 trials were used to find prognostic factors for relapse free and overall survival, which were used in all consecutive later trials to stratify patients with stage I and II into (very) favorable and unfavorable subgroups, requiring different intensities of treatment.30,32
The EORTC has been using the following six prognostic factors for stratification:
age
gender
B-symptoms + elevated ESR
number of involved areas
large mediastinal mass (MT-ratio > 0.35)
histologic subtype
According to Specht33 the last four factors are all related to total tumor burden, and peripheral bulk should have been added as an independent factor. These factors mainly predict outcome of relapse free survival. Age and gender are patient-related factors and predict outcome of overall survival.
2. 1985-1995
In the late 1970s and early 1980s it became clear that the increase in management aggressiveness, especially aiming at high relapse free survival rates, was inducing acute and late side effects, which were not balanced by an improvement in overall survival. The standardized mortality ratio after initial treatment remained increased as long as 20 years and by that time mortality from second cancers exceeded mortality from Hodgkin's lymphoma.36,37 It appeared that modern radiotherapy (extended fields, high doses) could induce late mortality because of lung damage,38,39 myocardial infarctions,36,40 and secondary solid tumors, especially lung cancer,41 breast cancer42 and gastrointestinal cancer.43 Combination chemotherapy (MOPP and MOPP/ABV44) was mainly responsible for acute leukemia45 and non-Hodgkin's lymphoma.41 In the EORTC, 320 of 1660 patients with stage I and II, died, 53% of Hodgkin's lymphoma, 8% of treatment related causes, 14% of second malignancy, 8% cardiac and 17% intercurrent or unspecified.46 After 15 years, the risk of dying from Hodgkin's lymphoma was gone, but the percentage of fatal second malignancies was still rising. The same crossing of the curves after 15-20 years has been observed for stages I and II by others.36,47,48 Although deaths from other causes accounted for 37% in early stage patients, it was only 19% in advanced stage patients, in whom the predominant cause of death still was Hodgkin's lymphoma progression.36 It thus became obvious that the treatment schemes had to be modified in such a way that overall survival rates of more than 90% would be maintained but at lower costs in terms of toxicity.
Ideally, modifications to reduce late toxicity would imply either less extended radiotherapy49 or the use of combination therapy with fewer courses of non-toxic, non-leukemogenic chemotherapy, followed by smaller radiotherapy fields whenever possible, with lower doses.50 Several groups initiated clinical trials to compare standard treatment with schemes replacing MOPP by less toxic chemotherapy such as VBM,51 ABVD,9 TBV52 or EBVP53 or replacing extended field by involved field.53– 55 In the EORTC H7 trials (1988-1993), several changes were made at the same time:
Patients with ‘very favorable’ disease (with all 6 prognostic factors favorable) received ‘minimal’ radiotherapy: mantle field only, without any abdominal treatment.
Patients with ‘favorable’ disease were enrolled in trials in which standard treatment (subtotal nodal irradiation) was randomly compared to 6 courses of EBVP, a modification of ABVD, and involved field radiotherapy.
Patients with ‘unfavorable’ disease: MOPP/ABV44 was considered standard treatment and was randomly compared to the same, presumably less toxic, combination of EBVP and involved field.56
In the H8 trials (1993-1998), the general ideas were maintained: a ‘very favorable’ group as in the H7 trial; a ‘favorable’ group treated with STNI compared to only 3 courses of MOPP/ABV plus involved field radiotherapy; and an ‘unfavorable’ group treated with 4 or 6 courses of MOPP/ABV plus involved field radiotherapy or STNI.
In a large meta-analysis of 3888 patients in 23 randomized trials, Specht57 showed, that more extensive radiotherapy in comparison to less extensive radiotherapy resulted in a lower risk of recurrence (43% versus 31%), but 10-year survival rates were 77% for both groups. Increased mortality from recurrent Hodgkin's lymphoma in patients treated with smaller fields appeared to be balanced by increased mortality from treatment-related causes (cardiac, second tumors) in patients receiving more extensive radiation. Likewise, the addition of chemotherapy to radiotherapy gave a significantly lower disease-free survival rate (33% versus 16%) in the combined modality arms, but overall survival at 10 years was not different (80% versus 77%). It was concluded that salvage chemotherapy for relapse was effective and that again increased mortality from recurrence was offset by increased mortality from treatment-related causes after initial combination of radiotherapy and chemotherapy.
The criticism of Mauch and others has been that most patients in the meta-analysis received MOPP and extended field radiotherapy. The newer ABVD scheme and involved field radiotherapy could prove to be as efficacious and/or less toxic, thus rendering relapse free survival a more important issue.
3. 1995 to the Present
In recent years, Hodgkin's lymphoma patients have usually been grouped on the basis of prognostic or risk factors:
Favorable: stage I and II without risk factors
Unfavorable: stage I and II with risk factors, stage IIIA, with or without risk factors
Advanced: stage IIIB and IV, low risk, stage IIIB and IV, high risk
The goal of the treatment is for:
Favorable disease: cure with minimal side effects
Unfavorable disease: cure with some (acceptable) side effects
Advanced disease: cure without serious side effects.
The problem is to define ‘minimal’ treatment and to define what is ‘acceptable’ for the patient. A typical example is the outcome of the combined H7 VF and H8 VF EORTC-trials: 80 patients were treated with mantle field (36-40 Gy) only. Survival is excellent: only one patient has died. Event-free survival, however, was very disappointing, because almost one-third of the patients had relapse (predominantly abdominal) and needed salvage chemotherapy.58 MacKenzie et al49 found similar results in a retrospective series of 99 ‘low risk’ patients, treated with radiotherapy alone (35 Gy): a disease free survival of 75%, but an overall survival of 90%.
What proportion of relapse is acceptable? Is this for the doctor or the patient to decide?
How far do we want to go in diminishing radiotherapy dose? In the German Hodgkin Study Group (GHSG) HD4-study it was shown, that in PS IA to IIB patients, extended field radiotherapy (RT) to 30 Gy with an extra 10 Gy on involved areas was as effective as extended field RT to 40 Gy.20 In the GHSG HD3-study, patients with stage III and IV, reaching a complete remission after 6 COPP (cyclophosphamide, vincristine, procarbazine, prednisone) + ABVD courses, did as well with 20 Gy involved field RT as with further chemotherapy.59 In the current EORTC H9 F trial, after 6 courses of EBVP, favorable patients are randomized to involved field irradiation of 36 Gy, 20 Gy or no radiotherapy. Unfavorable patients, randomized to ABVD or BEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, prednisone), never receive more than 30 Gy involved field RT if in complete remission. We will have to wait for a long time before we know if those lower doses and smaller fields will result in fewer secondary solid tumors, and these must be balanced against a higher rate of relapses and salvage therapies.
As Mauch stated in 1996,60 the treatment of early stage Hodgkin's lymphoma has become more complicated over the past 10 years. Initial treatment decisions may have profound long-term effects on patients. It is debatable if ‘routine’ cases exist and it is still advisable to treat patients in controlled clinical trials.
Treatment recommendations for patients not enrolled on a clinical trial
The most desirable choice of treatment for a patient with early stage Hodgkin's lymphoma should be entry into a clinical trial. This will ensure both that the patient will receive the highest possible quality of care with appropriate monitoring and follow-up and that additional important lessons will be learned that will lead to further improvements in treatment for future patients. If enrollment in a clinical trial is not feasible, the following choices of treatment would be reasonable:
1. Early stage with favorable prognosis
Definition: clinical stage I or II without any of the following risk factors:
Age > 50 y
Erythrocyte sedimentation rate > 50 mm/h or > 30 mm/h in the presence of B symptoms
Four or more separate sites of nodal involvement
Mediastinal mass ratio > 0.35
Treatment: combined modality preferred
First choice: ABVD × 4 cycles + involved field radiotherapy 36-40 Gy
Alternative choices if first choice contra-indicated:
Sub-total nodal irradiation 36-40 Gy
EBVP x 6 cycles + involved field radiotherapy 36-40 Gy
2. Early stage with unfavorable prognosis
Definition: stage I or II with any of the following risk factors:
Age > 50 y
Erythrocyte sedimentation rate > 50 mm/h or > 30 mm/h in the presence of B symptoms
Four or more separate sites of nodal involvement
Mediastinal mass ratio > 0.35
In addition, patients with stage IIIA could also reasonably be included in this group
Treatment: combined modality treatment essential
First choice: ABVD × 6 cycles + involved field radiotherapy 36-40 Gy
Alternative choice if first choice contra-indicated:
MOPP/ABV × 6 cycles + involved field radiotherapy 30-40 Gy
II. Cooperative Group Studies in Advanced Hodgkin's Disease
Sandra J. Horning, MD*
Division of Oncology, Stanford University Medical Center, 1000 Welch Road, Suite 202, Palo Alto CA 94304-5756
Building on the successes seen at individual treatment centers, definitive phase III clinical trials conducted over the past three decades by cooperative groups in North America and Europe have come to determine the standard treatment for advanced Hodgkin's disease. In addition to the choice of combination chemotherapy as the major treatment variable, the trials described in Table 3 differ in the definition of advanced disease, inclusion of patients who had relapsed after radiotherapy alone, duration of chemotherapy and incorporation of radiotherapy. Patients with advanced Hodgkin's disease and their clinicians face the task of balancing the risk of progression or relapse, which is usually early, with toxicity, which is often delayed. The ability to eradicate Hodgkin's disease in a significant proportion of patients with second-line treatment adds complexity to the decision-making process. From these considerations, we appreciate the difficulty in establishing a survival advantage for a given treatment and the necessity for following patients for 10+ years for an accurate survival estimate.
Chemotherapy Alone in Advanced Hodgkin's Disease
Bonadonna and colleagues at the Milan Tumor Institute pioneered the ABVD regimen, establishing its efficacy in untreated patients and patients with recurrence after MOPP therapy and combining it with MOPP in an alternating schedule.1–,3 Following on these successes, the CALGB designed a trial for IIIA2, IIIB and IV patients comparing 6-8 cycles of MOPP to 6-8 cycles of ABVD or 12 cycles of alternating MOPP and ABVD.4 At 5 years, overall survivals (OS) were 66% for MOPP, 73% for ABVD and 75% for MOPP/ABVD (p = NS for doxorubicin-containing combinations versus MOPP). However, both ABVD and MOPP/ABVD yielded failure-free survivals (FFS) superior to MOPP at 5 years: 61% and 65% versus 50%, respectively (p = < 0.05). Notable factors in this trial comprise the inclusion of patients who had failed radiotherapy, the variable duration of chemotherapy in the treatment arms, and the greater dose-limiting, acute myelotoxicity in the MOPP arm. In this trial, as with others in this era, dose modification reflected the practice at a time when growth factors were not available and severe neutropenia was less well-tolerated by patients and physicians.
The Eastern Cooperative Oncology Group (ECOG) led an intergroup study of 737 patients with stage IIIA2, IIIB, IV HD or in first relapse after radiotherapy.5 Randomization to sequential MOPP followed by ABVD or MOPP/ABV hybrid was performed in 691 eligible patients. With a median follow-up time of 7.3 years, the 8-year FFS rates were 64% for hybrid and 54% for sequential treatment (p = 0.01). MOPP/ABV hybrid had significantly more life-threatening or fatal neutropenia and pulmonary toxicity. Nine cases of leukemia or myelodysplasia were reported on the sequential regimen as compared with only one on the hybrid (p = .01) (Table 4 ).
The CALGB led a North American Intergroup study in which 856 patients with stage III-IV Hodgkin's disease received 8-10 cycles of ABVD or the MOPP/ABV hybrid regimen developed by the Vancouver group.6 Patients with disease recurrent after radiotherapy were also eligible. At 3 years, the estimated FFS was 65% for ABVD and 67% for MOPP/ABV (p = NS). Similarly, no difference in overall survival (OS) was observed. The study was stopped prematurely, however, due to a greater number of treatment-related deaths in the hybrid arm (n = 16) compared with ABVD (n = 9). At the time of preliminary reporting, there were 2 second malignancies after ABVD compared with 12 after hybrid, including 6 cases of myelodysplasia/leukemia (Table 4).
Combined Chemotherapy and Radiotherapy in Advanced Hodgkin's Disease
The efficacy and safety of alternating MOPP and ABVD or hybrid regimens was studied in two comparative phase III trials. In the Milan study, stage IB, IIA bulky, IIB, III A and B and IV patients received MOPP/ABVD or hybrid MOPP and ABVD, each for a minimum of 6 cycles followed by 30 Gy to initial sites of bulky disease.7 At 10 years, the freedom-from-progression (FFP) rate was 67% versus 69% (p = NS) and the OS rate was 74% versus 72% for the alternating and hybrid regimens, respectively (p = NS). A total of 23 second malignancies were documented among 427 patients including 11 secondary leukemias (Table 4).
The National Cancer Institute of Canada reported the results of a study of similar design conducted in IIIB and IV patients or those who had failed prior radiotherapy.8 All patients received 8 cycles of chemotherapy either with MOPP alternating with ABVD or the Vancouver MOPP/ABV hybrid; those with residual disease in a local region after 6 cycles received radiotherapy. At 5 years, OS rates were 81% and 83% for MOPP/ABV hybrid and alternating MOPP/ ABVD, respectively. There was no difference in FFS: 71% and 67% for hybrid and alternating therapy, respectively. Of note, FFS was superior with alternating MOPP/ABVD for patients with prior irradiation (5-year FFS 94% versus 73%; p = .017). Although the cure rate was not different in the two arms in this study, there was significantly more febrile neutropenia and stomatitis with the hybrid regimen.
The GHSG fitted a model to the data of 706 patients treated with COPP alternating with ABVD and hypothesized that shortening the treatment interval would lead to modest benefit.9 On this basis they developed the BEACOPP regimen that is administered every 21 days. Their model further suggested that escalation of dose intensity by 30% might yield a 10-15% benefit in tumor control. On that basis, the escalated BEACOPP regimen was designed with granulocyte colony stimulating factor (G-CSF) support. Following phase II multi-center trials, the HD9 trial tested BEACOPP, escalated BEACOPP and COPP/ABVD in IIB and IIIA patients with risk factors and stage IIIB and IV patients. After 8 chemotherapy cycles, initial bulky sites received 30 Gy and residual disease sites received 40 Gy. On this basis, the majority of patients received consolidative radiotherapy. The interim results of this large study have been published in multiple manuscripts and abstracts, most recently in December 2000.10
With a median follow-up of 40 months, data on 1180 of 1212 patients were available. At 3 years, FFS was 70% for COPP/ABVD, 79% for BEACOPP and 89% for escalated BEACOPP (each p < 0.05). Early progression accounted for a significant proportion of these differences. In subgroup analysis, the benefit of escalated BEACOPP was limited to patients aged 60 years or younger. In fact, patients aged 65-75 experienced no benefit from BEACOPP compared with COPP/ABVD and there were fewer toxic deaths with the latter. OS at 3 years were 91% for BEACOPP and 92% for escalated BEACOPP compared with 86% for COPP/ABVD. At the time of this reporting, myelodysplasia or secondary leukemia occurred in 0 of 263 patients on COPP/ABVD, 2 of 457 patients on BEACOPP and 8 of 460 patients on escalated BEACOPP. These early leukemias were characterized by balanced translocations of chromosome 11, presumably related to the escalation of etoposide interacting with doxorubicin and cyclophosphamide. Leukemias related to alkylating agents characteristically occur 4 to 5 years after treatment. Longer follow-up is needed to determine the impact of dose intensity on mature OS data, especially given the competing effects of higher cure rates and second cancers. As anticipated on the basis of cumulative doses of drugs, sterility complicated the BEACOPP regimen.
Investigators at Stanford took a different approach to unfavorable Hodgkin's disease. They hypothesized that the duration of chemotherapy could be shortened, through a combination of dose intensification and the judicious use of radiotherapy, without compromising efficacy. Major goals of this treatment approach were preserving fertility and minimizing secondary leukemia. The cumulative doses of doxorubicin and bleomycin are reduced in the Stanford V regimen compared with ABVD. Mustard is given on 3 occasions (total dose 18 mg/m2) and there is no procarbazine. After 12 weeks of chemotherapy, patients receive 36 Gy consolidative radiotherapy to initial disease sites ≥ 5 cm or macroscopic splenic disease. A group of 142 patients with bulky stage II, III or IV Hodgkin's disease were treated with Stanford V and followed a median of 6 years.11 Six-year FFS was 89% and OS was 96%. No secondary leukemia or myelodysplasia occurred. Fertility was preserved in a significant proportion of both men and women as evidenced by a total of 43 conceptions post-treatment.
Although the Stanford V data are compelling, they represent single institution data and must be confirmed in a larger population-based study. E2496 is a North American Intergroup study in which Stanford V and ABVD are being compared in bulky and advanced Hodgkin's disease. In addition to disease control and survival, pulmonary function and reproductive capacity are being assessed in this study.
The Role of Radiotherapy in Advanced Hodgkin's Disease
Through the years, multicenter groups have addressed the added benefit of RT in advanced Hodgkin's disease. Variables of potential importance in these studies include the chemotherapy combination, duration of chemotherapy, dose of RT, delivery of RT to selected bulky or residual disease sites or all initially involved sites, and quality control issues regarding RT. A number of these studies were underpowered to demonstrate a significant clinical difference. The SWOG (Southwestern Oncology Group) study of low-dose involved field RT after the MOP/BAP combination demonstrated no advantage to consolidative RT in the intent-to-treat analysis, although significantly better outcomes were seen in subsets of patients who actually received RT and those with nodular sclerosis histology.12 The GHSG conducted a study in which patients were treated with 6 cycles of COPP/ABVD and those in complete response (CR) were randomized to 2 further cycles or consolidative RT to initial sites, with a dose determined according to response.13 In this study, a significant proportion of patients were not randomized. Among the 100 patients who were randomized, there was no difference in disease-free survival for those treated with additional chemotherapy or RT. Of interest, there was a suggestion in this study that the addition of 2 cycles of chemotherapy was of benefit based on the experience among patients who were not randomized.
The GELA recently published data on a complex trial evaluating 6 cycles of 2 different chemotherapy regimens, MOPP/ABV or ABVPP (doxorubicin, bleomycin, vinblastine, procarbazine, prednisone). The study had a secondary randomization to 2 additional cycles of chemotherapy or subtotal or total nodal RT for IIIB and IV patients who achieved a CR or a good PR (75% tumor reduction). The dose of RT included 30 Gy to all volumes plus 5 Gy to involved areas and an additional 5 Gy to residual masses. After induction treatment, 418 patients were randomized to the consolidation phase. With a median follow-up of 48 months, the 5-year disease-free survival estimates were 80% for 8 cycles of MOPP/ABV, 82% for 6 cycles of MOPP/ABV plus RT, p = NS; and 68% for 8 cycles of ABVPP, and 75% for 6 cycles of ABVPP plus RTx (p = .01). The 5-year DFS estimates did not differ significantly between chemotherapy and RT, 74% and 79%, respectively (p = .07). FFS were 66% for MOPP/ABV and 56% for ABVPP (p = .10) and the differences in FFS among the 4 treatment arms did not achieve statistical significance (p = 0.07). At 5 years, 79% of study participants were alive. After MOPP/ABV, the 5-year OS estimates did not differ among patients randomized to chemotherapy or RT whereas, after ABVPP, the 5-year OS estimates were 94% for chemotherapy and 78% for RT (p = .002). Although there was a suggestion that RT partially compensated for the inferiority of ABVPP, the inability to salvage patients after wide-field RT paired with toxicity led to reduced OS. This is a complex study involving unusual chemotherapy and RT that is more extensive than most modern trials. Thus, it is difficult to factor the contribution of this study to the debate. Of note, 23% of deaths in this study were due to treatment-related complications during initial or salvage therapy.
EORTC investigators observed a superior FFP with a unique sequence of MOPP alternating with ABVD compared to MOPP in a comparative trial of stage IIIB and IV patients.14 RT was given similarly in both arms. In the follow-on trial, patients were treated with MOPP/ABVD × 6, and those achieving CR received 2 additional cycles of therapy prior to random assignment to observation or 24 Gy to all involved sites. All PR patients received RT in this study design.15 This study will assess the advantage of low dose RT in complete remission and complement the existing data.
Prognostic Factors and Other Considerations in Bulky and Advanced Hodgkin's Disease
Current clinical trials in unfavorable Hodgkin's disease often include patients with bulky or symptomatic limited stage disease and all IIIA patients, in contrast to earlier studies where eligibility was restricted to those in stages IIIA2, IIIB and IV. These differences may have important interactions with therapies that, in turn, influence the results and interpretation of clinical trials. For instance, the use of RT is more likely to favorably impact bulky mediastinal or limited stage rather than disseminated disease involving one or more extranodal sites.16 The overall impact of the inclusion of more limited stage patients is to improve FFS and OS rates.
Older age, often defined as above 45 years in Hodgkin's disease, is a consistent adverse prognostic factor across all studies. Studies with MOPP/ABV hybrid and BEACOPP demonstrate that these therapies should not be given to patients over 60 years of age. Older patients were not included in the Stanford V series. The cumulative doses of doxorubicin and bleomycin in ABVD can also pose problems for senior patients. Older patients are more likely to have advanced symptomatic disease and less likely to have bulky mediastinal disease; these facts should influence the use of RT and duration of CT in this population.
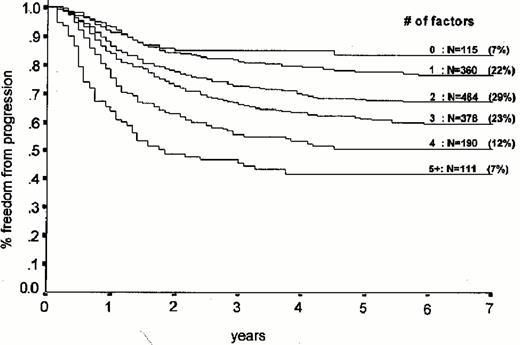
An international group supplied data on more than 5000 HD patients for an analysis of prognostic features headed by Hasenclever and Diehl. Seven prognostic factors (Table 5 ) were identified. Each factor contributed about a 7% decrement in FFP at 5 years, according to an analysis in 1618 patients (Figure 1 ). Only the group with 4-7 factors, representing fewer than 20% of patients, fell below 50% FFP at 5 years. Although the international prognostic score is an imperfect system, it does allow comparisons of populations across studies and can be used in the evaluations of outcome. For instance, BEACOPP was superior to COPP/ABVD in each of three prognostic groups (international prognostic score 0-1, 2-3, 4+) but the most striking difference was among patients in the highest risk group (p = 0.028). Evaluation of the international prognostic score and other time-honored prognostic variables (performance status, systemic symptoms) can be useful in considering the risks and benefits of different treatment strategies.
Balancing the Risks of Treatment Failure with Treatment-Related Toxicity
ABVD is currently the standard treatment for advanced stage Hodgkin's disease, with about 2/3 of patients alive and disease-free 3 years after treatment. Although ABVD enjoys a favorable toxicity profile relative to MOPP-containing chemotherapy (Table 4), it is not without adverse effects. Pulmonary toxicity can be serious or even fatal, and secondary leukemias and cancers have been reported in all large series, albeit with less frequency than alkylating-agent based treatment, and often in combination with RT. Selection of a favored first-line treatment for Hodgkin's disease must also consider the chance for secondary curative therapy. Current data indicate that continuous remissions may be achieved in as many as half of patients with recurrent Hodgkin's disease who receive high dose therapy and transplantation, less frequently among those who fail induction or prove to have poorly responsive disease at relapse.
BEACOPP is the only regimen broadly tested in a large phase III trial that appears to be superior to ABVD-containing treatment, although it must be remembered that the majority of patients in the GHSG study received combined modality therapy. Because BEACOPP sterilizes men and women and has a worrisome secondary leukemia risk (Table 4), it may be best reserved for higher risk patients, such as those with international prognostic score 5+. Although the OS at this time is slightly higher with either standard or escalated BEACOPP compared to COPP/ABVD, this endpoint must be evaluated with mature data that reflect the competing risks of Hodgkin's disease and treatment-related deaths. The current study of the GHSG addresses the issues of dose intensity with BEACOPP and the role of RT; these data will contribute significantly to the evidence base for advanced Hodgkin's disease.
Despite numerous studies, there continues to be controversy in the use of RT in bulky and advanced Hodgkin's disease. The effective control of irradiated disease must be balanced with the risk for late effects, particularly second cancers and heart disease. At this time, use of RT for advanced stage patients in a non-study setting is controversial but best accepted for bulky mediastinal disease. Of note, the Stanford V regimen is a combined modality treatment in which chemotherapy was abbreviated and consolidated with RT to bulky disease. This approach appears promising in the single institution setting as well as a pilot study conducted by ECOG and, together, these data support the comparison of ABVD and Stanford V in the ongoing phase III intergroup study (E2496) involving all North American cooperative groups.
Challenges Remain
Although ABVD is an effective treatment for Hodgkin's disease, at least 30% of patients will progress or relapse and less than half of these will be effectively treated secondarily. Pulmonary toxicity can be a serious problem, compounded by the use of chest radiotherapy. We have a poor understanding of the biologic underpinnings for treatment failure that could direct further treatment refinements. Genomic studies of single Reed-Sternberg cells and the application of a variety of new antibodies to elements of key signaling pathways in tissue micro-array studies may lead to rational therapeutics and an improved ability to select patients destined to fail conventional treatment who may be candidates for stem cell transplantation as primary treatment.
Practitioners may become complacent about treatment for Hodgkin's disease, an uncommon lymphoma for which the therapy is better than that for most neoplasms. But that is a disservice to young Hodgkin's disease patients, whose premature deaths are particularly tragic. Survivors have a long life expectancy subsequent to treatment, a long time to experience the toxicities of treatment. The need to further increase efficacy, the need to refine treatment according to risk, the need for predictors of late effects, and the need for mature follow-up for detection of late effects are compelling reasons for practitioners to enter patients with Hodgkin's disease, a rare but important disorder, on prospective clinical trials.
III. Lymphocyte Predominance Hodgkin's Lymphoma
Joseph M. Connors, MD*
B.C. Cancer Agency, Vancouver Clinic, 600 West 10th Ave., Vancouver BC V5Z 4E6
Dr. Connors is a member of the scientific board of Corixa, Inc.
Efforts to subdivide types of neoplasms are driven by the scientific desire to understand human biology in greater and greater detail and the clinical desire to identify subtypes that differ in natural history or response to treatment. The wide availability of reliable, reproducible immunohistochemical tests that detect the presence of individual cell surface antigens has been transforming the field of histopathology for the past two decades since the development of monoclonal antibody-based technology allowed the production and wide availability of standardized antigen-specific reagents. The classification of the lymphoproliferative diseases is a prime example of this transformation. The accurate identification of many of the entities listed in the Revised European-American Lymphoma (REAL)1 and World Health Organization (WHO)2 classification schemes can only be accomplished with the aid of these sophisticated new tools.3 In the special area of Hodgkin's lymphoma, understanding the entity of lymphocyte predominance Hodgkin's lymphoma has been particularly helped by application of these new immunohistochemical techniques. Thus, we have arrived at an appropriate time to reassess our understanding of this indolent and uncommon but highly treatable subtype.
Lymphocyte predominance Hodgkin's lymphoma (LPHL) was initially recognized, under other names, more than 50 years ago. In the 1960s the separate entity of lymphocytic and histiocytic Hodgkin's lymphoma was divided into nodular and diffuse subtypes. This name was used to identify a subtype of Hodgkin's lymphoma with an extensive lymphocytic background infiltration and peculiar scattered larger cells often later referred to as “L & H” or “popcorn” cells4 without classical Reed-Sternberg cells. In the widely used Rye classification5 the nodular and diffuse types were collapsed into one entity, LPHL. Results from individual centers and multi-institutional clinical trials established that LPHL often differed in presenting findings and staging and followed a more indolent course than the other types of Hodgkin's lymphoma (reviewed in 6). Attempts to better understand these differences by subdividing LPHL into separate entities focused on variations in histologic appearance, distinguishing nodular and diffuse subtypes.7–,11 However, inconsistent results precluded clear conclusions as to whether the natural history genuinely differed between the nodular and diffuse subtypes. Some authors found a different long-term outcome7,11 while others did not8– 10 leading some to assert that diffuse LPHL had a better, more Hodgkin's lymphoma-like behavior and nodular LPHL had a worse, more follicular lymphoma-like natural history, while others could not find this difference. Fortunately, the recent improvement in reproducibility of classification brought about by improved immunohistochemical testing should allow us to proceed beyond this impasse.
Diagnosis
The pioneering work of the International Lymphoma Study Group, which proposed the (REAL) classification,1 included an attempt to address the problem of LPHL. This group proposed that Hodgkin's lymphoma be subdivided into a classical variety including the familiar nodular sclerosing, mixed cellularity and lymphocyte depleted subtypes and, in addition, a new entity, lymphocyte rich classical Hodgkin's lymphoma and that a form of Hodgkin's lymphoma separate from the classical types be recognized, nodular lymphocyte predominance type. Most importantly, specific phenotypic and immunohistochemical criteria for the diagnosis of this new entity, nodular LPHL, were developed. The neoplastic cells exhibit characteristic folded, lobulated nuclei (“popcorn” cells) and inconspicuous nucleoli and are usually positive for CD20, negative for CD30, which is commonly positive in classical Hodgkin's lymphoma, and negative for CD15.12 Thus, this type of Hodgkin's lymphoma can be reliably identified by its typical immunophenotypic pattern (CD20 positive, CD15 negative, CD30 negative), which clearly distinguishes it from classical forms of Hodgkin's lymphoma (CD20 positive/negative, CD15 positive, CD30 positive). This set the stage for a major reassessment of LPHL.
The pivotal study, which has transformed our understanding of LPHL, was undertaken by the European Task Force on Lymphoma (ETFL).6,12 This group assembled paraffin blocks and clinical information on a large number of patients thought to have LPHL from 16 centers or cooperative groups in Europe and North America. A full analysis was confined to the 388 adult cases (age > 15 years) with adequate material for immunohistochemical testing and complete clinical information. Each pathology specimen was reexamined with a battery of immunohistochemical stains and reclassified by a panel of expert hematopathologists who were blinded to the clinical outcome data. Table 6 shows the outcome of the reclassification based on the full immunophenotypic profiling. Several themes emerge. First, without reliable, objective measures such as immunophenotypic profiling accurate diagnosis of LPHL is difficult. Only 56% (219/388) of cases submitted as LPHL from centers or groups with special expertise in lymphoma management ultimately proved to have this disease. Second, most of the cases reassigned to diagnoses other than LPHL were found to have the new variety of classical disease called lymphocyte rich classical Hodgkin's lymphoma, making up 115 of the 169 reassigned cases (68%). Third, almost all cases definitely identified as LPHL had the nodular form of the disease (206/219, 94%) and most of the diffuse cases from the original 388 actually had other diagnoses than LPHL, including 35 with lymphocyte rich classical Hodgkin's lymphoma. Fourth, almost all of the 14 non-neoplastic cases had progressively transformed germinal centers. Finally, the expert panel hematopathologists found the immunophenotypic triad of CD20 positive, CD15 negative, CD30 negative very helpful in distinguishing problem cases: 73 cases initially called LPHL were changed to classical Hodgkin's lymphoma when the neoplastic cells were found to be CD15 and CD30 positive; 35/76 initially problematic cases and 9/40 cases initially assigned to classical Hodgkin's lymphoma were changed to LPHL when found to be CD20 positive but CD15 and CD30 negative. Understanding these findings will be essential for the useful interpretation of past and future studies of LPHL.
Natural History and Clinical Outcome
LPHL has long been recognized as an uncommon (3-8% of new cases of Hodgkin's lymphoma) indolent disease seen more frequently in males, with a tendency to present with limited nodal disease and infrequent constitutional symptoms. Table 7 shows the findings from a representative set of larger, more recent studies. Although there is general agreement across these various studies, only the group assembled by the ETFL6,12 is restricted to CD20 positive, CD15 negative, CD30 negative cases. From these studies it is clear that LPHL usually presents without constitutional symptoms or extranodal disease. There is a 2:1 to 3:1 predominance of males and the median age of adult patients is similar to that seen in Hodgkin's lymphoma in general, 35 years. Mediastinal involvement is unusual (∼7%). In the rare patients with stage IV disease (∼6%) extranodal involvement is usually seen in sites typical of Hodgkin's lymphoma: liver (∼3%), bone marrow (∼1%) or lung (∼1%). Bulky disease is seen in only ∼13% of patients. Thus, a clear clinical picture of LPHL emerges from the available studies, which show that it is usually confined to non-bulky peripheral lymph nodes, seldom causes constitutional symptoms and is more often seen in men.
As would be expected given its usually localized presentation LPHL has most often been treated with irradiation. Chemotherapy has been reserved for the uncommon cases with advanced stage disease or as an adjuvant to the primary irradiation. No prospective randomized trials have addressed LPHL exclusively, so all observations about clinical outcome must be based on patients included in single center or cooperative group experiences, usually gathered retrospectively as in the ETFL study. Some conclusions can be drawn. Table 8 shows the range of long-term survivals reported in representative larger institutional or group experiences. Although the range in relapse or progression free survivals is wide, 45-74% at 10 years, the overall survivals are generally consistent in showing 10-year overall survivals of 80-90%. The factors that predict for a lower likelihood of long-term progression free or overall survival are not surprising: advanced stage or older age. However, several studies noted hints of a pattern of late relapse that seems different from classical Hodgkin's lymphoma. Typical of these results were those seen in the ETFL study. Among the 115 patients reclassified to lymphocyte rich classical Hodgkin's lymphoma only two of the 20 relapses (10%) occurred after 10 years and none after 13 years. However, in the 219 patients with LPHL 7 of 45 relapses (16%) occurred after 10 years and 5 of these were after 13 years. No plateau in failure free survival was seen in the LPHL cases. The small number of events and selected nature of the patients must temper conclusions drawn from these observations. Overall there are no compelling data that indicate a major difference in treatment outcome between patients with LPHL and classical forms of Hodgkin's lymphoma.
Progressively Transformed Germinal Centers, Diffuse Large B-Cell Lymphoma and LPHL
Several authors have noted a connection between progressively transformed germinal centers (PTGC) and LPHL,4,13,14 finding that PTGC can be seen before, coincident with or after LPHL. In the ETFL study most cases of non-neoplastic disease mistaken for LPHL were cases of PTGC.12 Although anecdotal case reports have linked PTGC with later development of LPHL, no convincing data have been reported indicating a definite increase in such risk. Presently, the major importance of PTGC is that it be recognized as a reactive, usually benign, lesion and not mistaken for a lymphoproliferative neoplasm.
Most of the larger series of cases of LPHL have noted a risk of later non-Hodgkin's lymphoma, usually diffuse large B-cell type. In the 219 confirmed LPHL cases in the ETFL study at least six patients eventually developed non-Hodgkin's lymphoma (2.9%). In a review of 567 cases of LPHL from the medical literature Diehl and his co-authors found 15 cases of non-Hodgkin's lymphoma reported for an incidence of 2.6%. In comparison, among the 12,411 cases recorded in the International Database on Hodgkin's Disease only 0.9% of patients were noted to develop subsequent non-Hodgkin's lymphoma. It is reasonable to conclude that there is a 2- to 3-fold increased risk of developing a secondary non-Hodgkin's lymphoma, usually diffuse large B-cell type, after LPHL in comparison to the rate seen after classical Hodgkin's lymphoma. However, the absolute risk of such secondary non-Hodgkin's lymphoma is low and, in a patient population already being followed carefully for possible Hodgkin's lymphoma recurrence, it does not have any clinical implication other than to make clear the necessity to obtain biopsy proof of the nature of any suspected recurrence.
Where Does the Evidence Lead Us?
Several specific questions are germane to the management of patients with LPHL. First, should patients with LPHL be treated differently from patients with other types of Hodgkin's lymphoma? Second, are there subtypes of LPHL that should be managed differently, for example nodular or diffuse types? Third, are there specific late events that require different monitoring for patients previously diagnosed with LPHL? Each can be addressed using the data cited earlier this section.
Should patients with LPHL be treated differently? The answer depends on one's choice of standard treatment for Hodgkin's lymphoma. Most patients with LPHL present with limited stage disease. Cumulative evidence from extensive clinical trials and single center experiences indicates that all Hodgkin's lymphoma patients with limited stage disease should be treated with an optimized mix of brief chemotherapy and irradiation of modest extent. Such treatment is entirely appropriate for patients with limited stage LPHL and can reasonably be expected to produce 10- and 20-year overall survivals exceeding 90% while minimizing the risks of secondary neoplasms. Patients with advanced stage LPHL seldom have clinical or laboratory features predicting a poor outcome and, therefore, should be treated with regimens such as ABVD that minimize exposure to the more potently carcinogenic antineoplastic agents. Overtreatment should be avoided, and attention to this issue should reduce as much as possible the risk of potentially fatal late complications.
Are there types of LPHL that should be managed differently? If it were clear that some types of LPHL were incurable with currently available treatment techniques, as is true for follicular lymphoma, a case could be made for deferral of initial treatment and reduction in intensity of treatment for relapses. However, there is no definite evidence that LPHL is less curable than classical Hodgkin's lymphoma or that this is true for any subtype of LPHL. Initial observations that diffuse LPHL may have a better prognosis than nodular LPHL have not been reproduced in most studies. Even more important the results of the ETFL study indicate that most cases thought to be diffuse LPHL are in fact not LPHL at all but rather other types of Hodgkin's lymphoma, reactive conditions or non-Hodgkin's lymphoma. Presently there is no reproducibly identifiable subtype of LPHL with a sufficiently different natural history to justify alteration of treatment.
Should patients with LPHL be monitored differently after treatment? Probably. Although the incidence of later non-Hodgkin's lymphoma is modestly increased compared to that seen after classical Hodgkin's lymphoma, the increase is not sufficient to justify departing from standard follow-up guidelines. However, some studies, including the ETFL project, show a tendency to late relapse that, at least until more definitive data are available, would justify continued surveillance for possible relapse beyond the time appropriate for classical Hodgkin's lymphoma.
The Future
One of the most promising types of new treatments for lymphoma is that of targeted immunotherapy. The anti-CD20 monoclonal antibody rituximab has proven useful for several different types of B-cell lymphomas. The nearly universal expression of CD20 on the neoplastic cells of LPHL suggests that this lymphoma may be usefully treated with rituximab. Preliminary data from several small series show response rates exceeding 50%.15– 17 If these response rates hold up and, even better, prove durable, treatment with rituximab will become very attractive for this disease because of the lack of cumulative or late toxicity with this agent. In addition, efficacy of one type of targeted immunotherapy hints that others may also be useful. Monoclonal antibodies aimed at other B-cell or lymphocytic antigens, radio-immunoconjugates and immunotoxin molecules and, eventually, tumor specific immunization strategies all hold promise. The specificity of each of these techniques is especially attractive as we try to improve treatment effectiveness while holding acute and especially late toxicity to a minimum. LPHL is already a highly treatable, often curable disease. It should be possible to build on the sound foundation of solidly reproducible pathologic identification based on immunophenotypic profiling and assemble even more effective, less toxic treatments in the future.
Randomized clinical trials in favorable prognosis stage I-II Hodgkin's lymphoma.
| Group . | Treatment arms . | n . | FFS . | OS . | Time (y) . |
|---|---|---|---|---|---|
| Abbreviations: FFS, failure-free survival; OS, overall survival; VBM, vinblastine, bleomycin, methotrexate; IFRT, involved field radiotherapy; EORTC, European Organization for Reserach and Treatment of Cancer; EBVP, epirubicin, bleomycin, vinblastine, prednisone; STLI, sub-total lymphoid irradiaton; MSKCC, Memorial Sloan-Kettering Cancer Center; TBV, thiotepa, bleomycin, methotrexate; MOPP, nitrogen mustard, vincristine, procarbazine, prednisone | |||||
| Stanford | VBM × 6 + IFRT 36 Gy | 35 | 88% | 94% | 5 |
| STLI 30-40-44 Gy | 43 | 93% | 98% | ||
| p=0.60 | p=0.50 | ||||
| EORTC H7F | EBVP × 6 + IFRT 36 Gy | 168 | 92% | 98% | 6 |
| STLI 36-40 Gy | 165 | 81% | 96% | ||
| p=0.004 | p=0.156 | ||||
| MSKCC | TBV × 4 + mantle field | 59 | 81% | 91% | 5 |
| MOPP × 4 + mantle field | 61 | 89% | 91% | ||
| p=0.23 | p=0.83 | ||||
| Group . | Treatment arms . | n . | FFS . | OS . | Time (y) . |
|---|---|---|---|---|---|
| Abbreviations: FFS, failure-free survival; OS, overall survival; VBM, vinblastine, bleomycin, methotrexate; IFRT, involved field radiotherapy; EORTC, European Organization for Reserach and Treatment of Cancer; EBVP, epirubicin, bleomycin, vinblastine, prednisone; STLI, sub-total lymphoid irradiaton; MSKCC, Memorial Sloan-Kettering Cancer Center; TBV, thiotepa, bleomycin, methotrexate; MOPP, nitrogen mustard, vincristine, procarbazine, prednisone | |||||
| Stanford | VBM × 6 + IFRT 36 Gy | 35 | 88% | 94% | 5 |
| STLI 30-40-44 Gy | 43 | 93% | 98% | ||
| p=0.60 | p=0.50 | ||||
| EORTC H7F | EBVP × 6 + IFRT 36 Gy | 168 | 92% | 98% | 6 |
| STLI 36-40 Gy | 165 | 81% | 96% | ||
| p=0.004 | p=0.156 | ||||
| MSKCC | TBV × 4 + mantle field | 59 | 81% | 91% | 5 |
| MOPP × 4 + mantle field | 61 | 89% | 91% | ||
| p=0.23 | p=0.83 | ||||
Randomized clinical trials in unfavorable prognosis stage I-II Hodgkin's lymphoma.
| Group . | Treatment arms . | n . | FFS . | OS . | Time (y) . |
|---|---|---|---|---|---|
| Abbreviations: See Table 1; PAVe, procarbazine, melphalan (Alkeran), vinblastine; MF, mantle field; ABVD, doxorubicin, bleomycin, vinblastine, dacarbazine; MOPP, nitrogen mustard, vincristine, procarbazine, prednisone; IFRT, involved field irradiation; ABV, doxorubicin, bleomycin, vinblastine | |||||
| Stanford | PAVe × 3 + MF + PAVe × 3 | 12 | 56% | 73% | 15 |
| ABVD × 3 + MF+ ABVD × 3 | 12 | 83% | 100% | ||
| p=0.1 | p=0.06 | ||||
| EORTC H6U | MOPP × 3 + MF + MOPP × 3 | 165 | 77% | 87% | 10 |
| ABVD × 3 + MF +ABVD × 3 | 151 | 88% | 87% | ||
| p<0.01 | p=0.52 | ||||
| EORTC H7U | EBVP × 6 + IFRT 36 Gy | 160 | 68% | 82% | 6 |
| MOPP/ABV × 6 + IFRT 36 Gy | 156 | 90% | 89% | ||
| p<0.0001 | p=0.18 | ||||
| Group . | Treatment arms . | n . | FFS . | OS . | Time (y) . |
|---|---|---|---|---|---|
| Abbreviations: See Table 1; PAVe, procarbazine, melphalan (Alkeran), vinblastine; MF, mantle field; ABVD, doxorubicin, bleomycin, vinblastine, dacarbazine; MOPP, nitrogen mustard, vincristine, procarbazine, prednisone; IFRT, involved field irradiation; ABV, doxorubicin, bleomycin, vinblastine | |||||
| Stanford | PAVe × 3 + MF + PAVe × 3 | 12 | 56% | 73% | 15 |
| ABVD × 3 + MF+ ABVD × 3 | 12 | 83% | 100% | ||
| p=0.1 | p=0.06 | ||||
| EORTC H6U | MOPP × 3 + MF + MOPP × 3 | 165 | 77% | 87% | 10 |
| ABVD × 3 + MF +ABVD × 3 | 151 | 88% | 87% | ||
| p<0.01 | p=0.52 | ||||
| EORTC H7U | EBVP × 6 + IFRT 36 Gy | 160 | 68% | 82% | 6 |
| MOPP/ABV × 6 + IFRT 36 Gy | 156 | 90% | 89% | ||
| p<0.0001 | p=0.18 | ||||
Treatment results in bulky and advanced Hodgkin's disease.
| Group/Reference . | Patients/Treatment . | N . | FFS% . | OS% . | Time (Yr) . |
|---|---|---|---|---|---|
| * p <0.05 | |||||
| Abbreviations: FFS, failure-free survival; OS, overall survival; CALGB, Cancer and Leukemia Group B ; ECOG, Eastern Cooperative Oncology Group; Milan, Milan Tumor Group; NCI-C, National Cancer Institute of Canada; GHSG, German Hodgkin Study Group; pRT, recurrence after therapy; ABVD, doxorubicin, bleomycin, vinblastine, dacarbazine; MOPP, nitrogen mustard, vincristine, procarbazine, prednisone; ABV, doxorubicin, bleomycin, vinblastine; RT, radiotherapy; COPP, cyclophosphamide, vincristine, procarbazine, prednisone; BEACOPP, bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, prednisone; escBEACOPP, escalated BEACOPP | |||||
| Chemotherapy Only | |||||
| CALGB | IIIA2,IIIB, IV, after RT | 361 | 5 | ||
| ABVD | 61* | 76 | |||
| MOPP/ABVD | 65* | 75 | |||
| MOPP | 50* | 66 | |||
| ECOG | IIIA2,IIIB, IV, after RT | 691 | 8 | ||
| MOPP → ABVD | 54* | ||||
| MOPP/ABV | 64* | ||||
| CALGB | III, IV, after RT | 856 | 3 | ||
| ABVD | 65 | 87 | |||
| MOPP/ABV | 67 | 85 | |||
| Chemotherapy + Radiotherapy | |||||
| Milan | IB, IIAbulky,IIB, III, IV | 427 | 10 | ||
| MOPP/ABVD + RT | 67 | 74 | |||
| Hybrid + RT | 69 | 72 | |||
| NCI-C | IIIB, IV, after RT | 301 | 5 | ||
| MOPP/ABVD + RT | 67 | 83 | |||
| Hybrid + RT | 71 | 81 | |||
| GHSG | IIB-IIIArisk, IIIB, IV | 1180 | 3 | ||
| COPP/ABVD + RT | 70* | 86* | |||
| BEACOPP + RT | 79* | 91* | |||
| EscBEACOPP + RT | 89* | 92* | |||
| Group/Reference . | Patients/Treatment . | N . | FFS% . | OS% . | Time (Yr) . |
|---|---|---|---|---|---|
| * p <0.05 | |||||
| Abbreviations: FFS, failure-free survival; OS, overall survival; CALGB, Cancer and Leukemia Group B ; ECOG, Eastern Cooperative Oncology Group; Milan, Milan Tumor Group; NCI-C, National Cancer Institute of Canada; GHSG, German Hodgkin Study Group; pRT, recurrence after therapy; ABVD, doxorubicin, bleomycin, vinblastine, dacarbazine; MOPP, nitrogen mustard, vincristine, procarbazine, prednisone; ABV, doxorubicin, bleomycin, vinblastine; RT, radiotherapy; COPP, cyclophosphamide, vincristine, procarbazine, prednisone; BEACOPP, bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, prednisone; escBEACOPP, escalated BEACOPP | |||||
| Chemotherapy Only | |||||
| CALGB | IIIA2,IIIB, IV, after RT | 361 | 5 | ||
| ABVD | 61* | 76 | |||
| MOPP/ABVD | 65* | 75 | |||
| MOPP | 50* | 66 | |||
| ECOG | IIIA2,IIIB, IV, after RT | 691 | 8 | ||
| MOPP → ABVD | 54* | ||||
| MOPP/ABV | 64* | ||||
| CALGB | III, IV, after RT | 856 | 3 | ||
| ABVD | 65 | 87 | |||
| MOPP/ABV | 67 | 85 | |||
| Chemotherapy + Radiotherapy | |||||
| Milan | IB, IIAbulky,IIB, III, IV | 427 | 10 | ||
| MOPP/ABVD + RT | 67 | 74 | |||
| Hybrid + RT | 69 | 72 | |||
| NCI-C | IIIB, IV, after RT | 301 | 5 | ||
| MOPP/ABVD + RT | 67 | 83 | |||
| Hybrid + RT | 71 | 81 | |||
| GHSG | IIB-IIIArisk, IIIB, IV | 1180 | 3 | ||
| COPP/ABVD + RT | 70* | 86* | |||
| BEACOPP + RT | 79* | 91* | |||
| EscBEACOPP + RT | 89* | 92* | |||
Second cancers after treatment for Hodgkin's disease.
| Group/Reference . | Patients/Treatment . | N . | MDS/Leukemia . | Solid Tumors . | Time (Yr) . |
|---|---|---|---|---|---|
| * Figures indicate non-Hodgkin's lymphoma only | |||||
| Abbreviations: see Table 3; MDS, myelodysplastic syndrome | |||||
| Chemotherapy Only | |||||
| ECOG | IIIA2,IIIB, IV, after RT | 691 | 8 | ||
| MOPP → ABVD | 9 | N/A | |||
| MOPP/ABV | 1 | N/A | |||
| CALGB | III, IV, after RT | 856 | 3 | ||
| ABVD | 0 | 2 | |||
| MOPP/ABV | 6 | 6 | |||
| Chemotherapy + Radiotherapy | |||||
| Milan | IB, IIAbulky,IIB, III, IV | 427 | 11 | 12 | 10 |
| MOPP/ABVD + RT | |||||
| Hybrid + RT | |||||
| GHSG | IIB-IIIArisk, IIIB, IV | 1180 | 3 | ||
| COPP/ABVD | 233 | 0 | 6* | ||
| BEACOPP | 457 | 2 | 4* | ||
| EscBEACOPP | 460 | 8 | 4* | ||
| Group/Reference . | Patients/Treatment . | N . | MDS/Leukemia . | Solid Tumors . | Time (Yr) . |
|---|---|---|---|---|---|
| * Figures indicate non-Hodgkin's lymphoma only | |||||
| Abbreviations: see Table 3; MDS, myelodysplastic syndrome | |||||
| Chemotherapy Only | |||||
| ECOG | IIIA2,IIIB, IV, after RT | 691 | 8 | ||
| MOPP → ABVD | 9 | N/A | |||
| MOPP/ABV | 1 | N/A | |||
| CALGB | III, IV, after RT | 856 | 3 | ||
| ABVD | 0 | 2 | |||
| MOPP/ABV | 6 | 6 | |||
| Chemotherapy + Radiotherapy | |||||
| Milan | IB, IIAbulky,IIB, III, IV | 427 | 11 | 12 | 10 |
| MOPP/ABVD + RT | |||||
| Hybrid + RT | |||||
| GHSG | IIB-IIIArisk, IIIB, IV | 1180 | 3 | ||
| COPP/ABVD | 233 | 0 | 6* | ||
| BEACOPP | 457 | 2 | 4* | ||
| EscBEACOPP | 460 | 8 | 4* | ||
Risk factors for International Prognostic Score.
| Age ≥ 45 years |
| Male sex |
| Stage IV |
| Hemoglobin < 10.5 g/dl |
| Albumin < 4 g/dl |
| Lymphocytes < 600/μl or < 8% |
| White blood count ≥ 15,000/μl |
| Age ≥ 45 years |
| Male sex |
| Stage IV |
| Hemoglobin < 10.5 g/dl |
| Albumin < 4 g/dl |
| Lymphocytes < 600/μl or < 8% |
| White blood count ≥ 15,000/μl |
Final diagnosis based on re-classification of 388 cases initially diagnosed as lymphocyte predominance Hodgkin's lymphoma (adapted from12).
| Total | 388 |
| Final diagnoses | |
| Non-Hodgkin's lymphoma | 12 |
| Reactive hyperplasia | 14 |
| Unclassifiable | 9 |
| Classical Hodgkin's lymphoma | 134 |
| Nodular sclerosing/mixed cellularity | 19 |
| Lymphocyte rich | 115 |
| Lymphocyte predominance Hodgkin's lymphoma | 219 |
| Total | 388 |
| Final diagnoses | |
| Non-Hodgkin's lymphoma | 12 |
| Reactive hyperplasia | 14 |
| Unclassifiable | 9 |
| Classical Hodgkin's lymphoma | 134 |
| Nodular sclerosing/mixed cellularity | 19 |
| Lymphocyte rich | 115 |
| Lymphocyte predominance Hodgkin's lymphoma | 219 |
Clinical characteristics of patients with lymphocyte predominance Hodgkin's lymphoma from representative larger series.
| Abbreviations: NR, not reported | ||||||
| Number of cases | 110 | 50 | 73 | 64 | 68 | 219 |
| Age, median (y) | 39 | 36 | 29 | 29 | 35 | 35 |
| % males | 75 | 86 | 84 | 81 | 68 | 74 |
| % stage I | 59 | 52 | 40 | 55 | 51 | 53 |
| II | 11 | 26 | 36 | 27 | 24 | 28 |
| III | 21 | 16 | 23 | 17 | 13 | 14 |
| IV | 9 | 6 | 1 | 1 | 12 | 6 |
| % B symptoms | 12 | 6 | NR | 9 | 15 | 10 |
| Reference | (8) | (10) | (7) | (9) | (18) | (6) |
| Abbreviations: NR, not reported | ||||||
| Number of cases | 110 | 50 | 73 | 64 | 68 | 219 |
| Age, median (y) | 39 | 36 | 29 | 29 | 35 | 35 |
| % males | 75 | 86 | 84 | 81 | 68 | 74 |
| % stage I | 59 | 52 | 40 | 55 | 51 | 53 |
| II | 11 | 26 | 36 | 27 | 24 | 28 |
| III | 21 | 16 | 23 | 17 | 13 | 14 |
| IV | 9 | 6 | 1 | 1 | 12 | 6 |
| % B symptoms | 12 | 6 | NR | 9 | 15 | 10 |
| Reference | (8) | (10) | (7) | (9) | (18) | (6) |
Results of treatment of lymphocyte predominance Hodgkin's lymphoma (LPHL).
| . | Survival (%) . | . | |||||
|---|---|---|---|---|---|---|---|
| n . | Relapse free . | Progression free . | Overall . | Ref. . | |||
| 5 y | 10 y | 5 y | 10 y | 5 y | 10 y | ||
| 110 | 88 | 80 | (8) | ||||
| 145 | 90 | (19) | |||||
| 75 | 80 | 93 | (11) | ||||
| 73 | 60 | 82 | (7) | ||||
| 68 | 45 | 71 | (18) | ||||
| 64 | 74 | 85 | (9) | ||||
| 219 | 70 | 92 | (6) | ||||
Probability of freedom from progression in 1618 patients according to the number of risk factors described in Table 5. Reprinted with permission from the New Eng J Med.
Probability of freedom from progression in 1618 patients according to the number of risk factors described in Table 5. Reprinted with permission from the New Eng J Med.