Abstract
This paper introduces novel therapeutic strategies focusing on a molecular marker relevant to a particular hematologic malignancy. Four different approaches targeting specific molecules in unique pathways will be presented. The common theme will be rational target selection in a strategy that has reached the early phase of human clinical trial in one malignancy, but with a much broader potential applicability to the technology.
In Section I Dr. Richard Klasa presents preclinical data on the use of antisense oligonucleotides directed at the bcl-2 gene message to specifically downregulate Bcl-2 protein expression in non-Hodgkin's lymphomas and render the cells more susceptible to the induction of apoptosis.
In Section II Dr. Alan List reviews the targeting of vascular endothelial growth factor (VEGF) and its receptor in anti-angiogenesis strategies for acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS).
In Section III Dr. Bruce Cheson describes recent progress in inhibiting cell cycle progression by selectively disrupting cyclin D1 with structurally unique compounds such as flavopiridol in mantle cell lymphoma as well as describing a new class of agents that affect proteasome degradation pathways.
I. Antisense Oligonucleotides Directed at the Bcl-2Gene Message in Non-Hodgkin's Lymphoma
Richard J. Klasa, MD*
Division of Medical Oncology, British Columbia Cancer Agency, 600 West 10th Avenue, Vancouver BC V52 4E6 Canada
Dr. Klasa is on the international advisory boards of Schering AG and Hoffmann-LaRoche, and is on the speakers' bureau and advisory board for Berlex Canada.
Hematologic malignancies in general and non-Hodgkin's lymphomas (NHLs) in particular are frequently associated with gain of function mutations, many characterized by balanced chromosomal translocations. Genome-wide surveys of gene expression are identifying both known and new transcripts that are overexpressed in different histological subtypes of lymphoma.1 As we develop molecular classifications of these diseases it is assumed that a few key genes will account for the particular survival advantage conferred on malignant lymphocytes as compared to their normal counterparts. These genes and their protein products would provide rational targets for the development of therapeutic strategies to reverse this upregulation associated with the malignant phenotype.
Non-Hodgkin's Lymphoma and Bcl-2
Over the past quarter century cytogenetic analysis has identified a number of reciprocal translocations that frequently occur in histologically identifiable subtypes of NHL.2 The transposition of the bcl-2 gene to the immunoglobulin heavy chain promoter region in the t(14;18) translocation is associated with > 90% of follicular lymphomas (FL) at diagnosis and 10% of diffuse large B-cell lymphomas (DLBCL), making it the most frequent event identified in NHL. Additionally, 50% of DLBCL overexpress the BCL-2 protein through other mechanisms, such as gene duplication, and are associated with a poorer prognosis after anthracycline-based combination chemotherapy.3 BCL-2 is also overexpressed in mantle cell lymphoma (MCL), chronic lymphocytic leukemia (CLL), multiple myeloma (MM) and acute myelogenous leukemia (AML).4 This same widespread pattern of distribution is also seen in a variety of solid tumors including melanoma, small cell lung carcinoma, and colon carcinoma as well as prostate and breast carcinoma, especially once the last two are hormone independent. The obvious conclusion is that BCL-2 overexpression, by whatever means, confers a fundamental advantage to malignant cells and that disruption of this overexpression might have therapeutic potential.
Bcl-2 is an anti-apoptotic member of a large family of genes involved in the regulation of programmed cell death.5,6 Pro-apoptotic (BAX and BCL-Xs) and anti-apoptotic (BCL-2, BCL-XL) molecules reside within the inner mitochondrial membrane and can homo- and heterodimerize upon appropriate stimulus. These interactions control the release of substances such as cytochrome C from the mitochondria into the cytosol through the opening or closing of specific pores in the membrane, with permeability determined by the relative abundance of the different molecules. Cytochrome C is central to the activation of caspases that initiate the apoptotic process. Thus, an overabundance of BCL-2 can prevent or retard activation of the apoptotic machinery and allow survival under conditions that might otherwise be lethal to a cell (Table 1 ).
Antisense Oligonucleotide
Reverse complementary or “antisense” oligonucleotides (ASOs) are short sequences of single stranded deoxyribonucleotides complementary to the coding regions of a gene that are designed to hybridize by Watson-Crick base pairing to messenger-RNA (m-RNA) sequences and thus facilitate their degradation.7,8 Naturally occurring antisense sequences have been identified as regulators of gene expression in a number of systems, supporting their potential for therapeutic development.9,10 The formation of a heteroduplex of m-RNA with the DNA of the ASO engages RNaseH, an enzyme that proceeds to specifically cleave off the m-RNA moiety, destroying the message and putatively leaving the therapeutic ASO molecule able to hybridize to another message sequence.11 This results in a reduction in the target m-RNA pool, which subsequently leads to reduction in the specific protein encoded (Figure 1; see color page 551). The presence of the ASO may also prevent the m-RNA from appropriately docking with the ribosomal machinery that would allow translation into a functional protein. The end result is loss of expression of that protein in the cell.
ASOs of 16-24 bases in length provide target specificity while shorter or longer sequences can result in random hybridization within the transcript repertoire. Selecting the target areas within a messenger RNA must ultimately take into account its tertiary structure, which will determine the accessibility of an area for hybridization. These target areas are defined in oligonucleotide arrays where the entire antisense sequence to an m-RNA is displayed in overlapping segments on a slide. The intensity of hybridization of the labeled message determines the candidate therapeutic ASOs.12 Screening of oligonucleotide libraries has also identified RNA sites that are most accessible to hybridization and correlated these sites with protein downregulation and biological function.13,14 More empirically, the first 6 codons of the open reading frame downstream of the AUG start site have repeatedly been found to be accessible to hybridization and have been chosen for initial development of ASOs against a number of genes.
As organisms have developed a sophisticated system for dealing with rogue strands of DNA both inside and outside the cell, the development of therapeutic molecules required chemical modifications to confer nuclease resistance and a favorable pharmacokinetic profile.15,16 Substitutions in the phosphodiester linkage of the bases in the ASO backbone has yielded a number of molecules now in clinical development with phosphorothioates being the most widely studied first generation molecules (Figure 2 ). The sulfur substitution yields an ASO that is nuclease resistant and capable of entering the cell. It demonstrates good hybridization kinetics and has little in the way of non-sequence-dependent effects or toxicities at concentrations required to downregulate the target message. Additionally, although in tissue culture a delivery system such as cationic lipid is required for efficient intracellular penetration of these highly charged molecules, in vivo ASOs have been shown to be active in free form, possibly due to interaction with blood lipoproteins.17,18
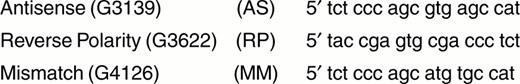
The correlation of a biologic effect with the specific downregulation of target message and protein in vivo has been a major focus of the development of ASOs. However, ASOs can be very potent immune stimulators, by virtue of unmethylated CpG motifs presented in the context of certain flanking sequences, and therapeutic activity could in part be attributed to nonspecific systemic immune effects rather then to a specific ASO/mRNA interaction.19–,22 Additionally, structures such as guanosine quartets can demonstrate sequence specific but non-antisense biological activity in vitro.23,24 Experimental designs therefore strive, by the use of appropriate control oligonucleotides (sense, missense, one and two base mismatch mis-sense) and various strains of immunodeficient animals, to isolate effects that can be attributed to the specific downregulation of target message and protein (Figure 3 ).
ASOs directed at bcl-2
An 18-mer phosphorothiolated oligonucleotide, G3139, directed against the first six codons of the open reading frame of the bcl-2 gene message has been developed by Genta Pharmaceuticals (Figure 3). Studies of G3139 utilizing the BCL-2 overexpressing lymphoma cell lines DoHH-2 and SU-DHL-4 in vitro have shown downregulation of message and protein expression.25 Tumor xenograft models in SCID mice have demonstrated therapeutic activity that is specific when compared to control animals as well as animals treated with reverse polarity sense, 2-base mismatch mis-sense and non-sense oligonucleotides.25,26 Extensive pharmakokinetic as well as toxicity studies have been performed identifying a dose range with a good therapeutic index.15,16 These findings supported the development of clinical trials using G3139 alone as treatment for BCL-2 overexpressing follicular lymphomas.
Further therapeutic potential is suggested by in vitro experiments confirming that bcl-2 plays a major role in the response of malignant cells to various stresses which produce cellular damage, including chemotherapy (Figure 4 ).4,27,28 Malignant cell lines transfected with a bcl-2 gene with resultant overexpression of the protein product demonstrated increased resistance to various chemotherapeutic agents.29–,32 Additionally, cell lines overexpressing BCL-2 were rendered more sensitive to killing by chemotherapeutic agents when either antisense oligonucleotides directed at the bcl-2 message were introduced into the culture or the cells were transfected with a vector bearing the antisense sequence.33,34 This has been correlated with a demonstration of downregulation of bcl-2 expression. With this as background, we set out to test the in vivo combination of ASOs targeting bcl-2 with a cytotoxic agent commonly used in the treatment of lymphoma.
ASOs to bcl-2and Chemotherapy
Escalating doses of G3139, cyclophosphamide and the combination of both agents were evaluated in severe combined immunodeficiency (SCID) mice bearing a systemic human DoHH2 lymphoma xenograft.35 Experiments confirmed that G3139 was able to downregulate BCL-2 expression in vitro and that treatment with G3139 alone resulted in prolongation of median survival and cure of some animals. (Figure 5 , left panel). This effect was dose and schedule dependent with no long-term survivors seen when a dose of 5mg/kg was given daily for 14 consecutive days as opposed to > 40% when the dose was increased to 12.5 mg/kg on the same daily schedule or either 5 or 12.5 mg/kg were administered for 14 treatments on alternate days (28-day schedule). Similarly, cyclophosphamide treatment alone resulted in no long-term survivors at lower doses but was able to cure animals at high doses. The addition of G3139 to low dose cyclophosphamide resulted in the cure of the majority of animals (Figure 5, right panel). The interaction between the two agents does show dose-response correlations; for the two low doses of cyclophosphamide tested, increasing the dose of G3139 from 2.5 to 5 mg/kg resulted in longer median survivals and overall increase in long-term survivors. A rather striking result was achieved when a completely ineffective dose of cyclophosphamide (15 mg/kg, median survival 36 days and no long-term survivors) was combined with a modestly effective dose of G3139 (2.5 mg/kg, 61 day median survival and 16% long-term survivors) to produce a 72-day median survival and 50% long-term survivors. Mice sacrificed at 90 days showed no histological evidence of any disease in all tissues analyzed, including immunoperoxidase staining for BCL-2, or molecular detection of bcl-2, by PCR. This suggests that chemotherapy at very modest doses could be made much more effective without increasing toxicity when combined with an antisense oligonucleotide. Such an increase in the efficacy of currently available agents could significantly alter the prognosis of a large number of moderately chemotherapy sensitive human tumors, resulting in longer median survivals and increasing the potential for cure.
The model has direct relevance to the clinical situation faced in NHL, where patients typically present with a chemotherapy-sensitive tumor at diagnosis that regresses only to recur within months to years post-treatment. The DoHH2 cell line was derived from a follicular lymphoma carrying a t(14;18), which results in bcl-2 gene overexpression. The aggressive nature of the disease in this model is, however, more suggestive of a transformation to a higher-grade histology, a common event in follicular lymphoma. Indeed, a recent re-exploration of the molecular and cytogenetic features of the cell line, using more sensitive detection techniques, has revealed a second translocation involving the c-myc oncogene with a resultant derivative chromosome 8 carrying t(8;14;18).36 We have recently described this phenomenon of double translocation of both bcl-2 and c-myc in a subset of patients with small non-cleaved cell (Burkitt-like) lymphoma, which represents a very aggressive form of the disease.37
Clinical Studies
G3139 has been studied as a single agent in a phase 1 trial in heavily pretreated (median of 4 prior regimens) patients with relapsed NHL.38,39 Twenty-one patients with follicular (9), small lymphocytic (8), diffuse large B-cell (3) or mantle cell (1) lymphomas that expressed BCL-2 were treated at 8 dose levels ranging from 4.6 to 195.8 mg/m2/day by continuous subcutaneous infusion for 14 consecutive days. No significant toxicity was seen up to doses of 110 mg/m2/day. One complete and 2 minor responses as well as 9 disease stabilizations were seen in this heavily pretreated group. BCL-2 protein was decreased in 7 out of 16 samples examined, including 2 from accessible tumor sites and 5 samples of peripheral blood or marrow mononuclear cells.
One study combining a chemotherapeutic agent with G3139 has been reported in metastatic melanoma,40 and studies are ongoing in a number of other solid tumors (melanoma, prostate carcinoma) and hematological malignancies (myeloma, chronic lymphocytic leukemia, and acute myeloid leukemia). A phase 1 study at our institution in relapsed follicular lymphomas combining escalating doses of both cyclophosphamide and G3139 has not identified any unexpected toxicity. The last patient enrolled has received cyclophosphamide 750 mg/m2 with 2.3 mg/kg/day of G3139 by continuous intravenous infusion for 14 consecutive days (Table 2 ).
Conclusions
The identification of overexpression or aberrant expression of genes that result in a gain of function, through genome wide surveys of cells and tissues in varying states, will provide unprecedented insight into the biology of hematological malignancies. Specific downregulation of such overexpression with antisense oligonucleotides allows disruption of single gene function at the messenger RNA and protein level and the study of downstream events in the involved molecular pathways both in vitro and in vivo. Genes that are critical to the differential growth and survival advantage enjoyed by malignant cells are being identified and are logical therapeutic targets. The development of ASOs directed at the bcl-2 gene provides a model by which a systemic therapy for a metastatic disease has been taken from the laboratory through preclinical studies to early phase clinical trials, building on knowledge of this particular gene's role in cellular apoptosis. Combining multiple antisense strategies with other therapeutic modalities has the potential to increase the specificity of the treatments available to our patients, thus improving their efficacy and reducing toxicity.
II. Targeting Angiogenesis in Hematologic Malignancies
Alan F. List, MD*
Arizona Cancer Center, 1515 N Campbell, Room 3945, PO Box 245004, Tucson AZ 85774
The seminal observations that the growth and metastatic potential of solid tumors is dependent upon the formation of new blood vessels triggered an enormous expansion in angiogenic research that has yielded novel therapeutics targeting an array of angiogenic molecules. Investigations of the relevance of angiogenesis in hematologic malignancies are still at an early stage, but accumulating evidence indicates that the angiogenic profile of many hematologic malignancies is distinct from that of solid tumors. As progeny of a common endothelial and hematopoietic stem cell, hematologic malignancies may elaborate and respond to angiogenic factors in a paracrine or autocrine fashion, contributing to tumor cell survival and expansion, adhesion, bone resorption and immune suppression.
Angiogenesis
Blood vessel development is characterized by two distinct biologic processes, vasculogenesis, and angiogenesis. Vasculogenesis, which is largely restricted to embryonic development, involves de novo endothelial cell differentiation from mesodermal precursors as the prerequisite for coordinated blood vessel generation.1 Angiogenesis, the process of new blood vessel formation from preexisting vessels, is responsible for the generation of neovasculature in adult life, and occurs physiologically during wound healing and within female reproductive organs during the menstrual cycle, as well as in pathologic conditions such as proliferative retinopathy, arthritic synovium, and human malignancies.2 Angiogenesis is a multistep process that includes both activation and resolution phases. The activation phase is responsible for the sequential events of basement membrane degradation, endothelial cell proliferation and migration, and capillary lumen formation. The resolution phase is responsible for the maturation and stabilization of the newly formed microvasculature through the recruitment of pericytes, promotion of basement membrane reconstitution, and subsequent extinction of the endothelial cell mitogenic response. A large number of pro-angiogenic molecules and endogenous angiogenesis inhibitors that coordinate the angiogenic response have been delineated (Table 3 ).3 Vascular endothelial growth factor (VEGF), first identified in 1989 and later isolated from the HL-60 myeloid leukemia cell line, is a critical regulator of vascular development that is responsible for activation of endothelial cell proliferation during vasculogenesis and the direction of capillary sprouting during angiogenesis.4 Indeed, gene inactivation studies indicate that VEGF is essential to the neoplastic angiogenic response.5
VEGF and Receptor Tyrosine Kinases
The VEGF-A molecule is a disulfide-linked homodimer represented by five different isoforms generated by alternate exon splicing of gene message.6 The corresponding VEGF monomers range in size from 121 to 206 amino acids, with smaller molecules (i.e., 121, 145, and 165 amino acids) representing the secreted and diffusable isoforms, whereas the larger proteins (189, 206 amino acids) are sequestered by heparin sulfate residues present on cell surfaces or within the extracellular matrix.7,8 Although all isoforms are biologically active, the VEGF165 isoform predominates and is recognized as a more potent and bioavailable endothelial cell mitogen.9,10 Recent investigations indicate that the VEGF family is composed of five members in addition to the prototype, VEGF-A, including VEGF-B, VEGF-C, VEGF-D, VEGF-E and PIGF (placental growth factor).6 Within the arterial wall, VEGF is produced by smooth muscle cells in response to oxidative stress and other stimuli.11 Autocrine production of VEGF and corresponding receptor upregulation is also demonstrable in endothelial cells in response to hypoxia, nitric oxide, VEGF deprivation and other cellular stresses.12,13
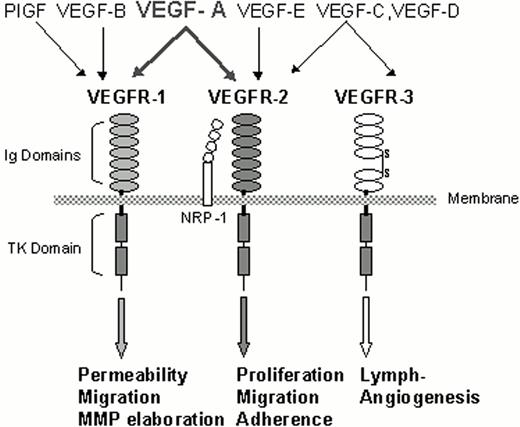
Trophic response to the VEGF family members is directed by selective interaction with structurally homologous type III receptor tyrosine kinases (RTKs), including VEGFR-1, originally termed fms-like tyrosine kinase (FLT-1),14 VEGFR-2 or kinase insert domain-containing receptor (KDR)/fetal liver kinase-1 (flk-1),15 and the recently characterized VEGFR-3 or FLT-4 receptor (Figure 6 ).16 Each of these receptors contains seven extracellular immunoglobulin homology domains that create the ligand-binding site, a single short transmembrane-spanning sequence, and a cytoplasmic tail that contains the tyrosine kinase domain akin to that of the c-kit and PDGF-receptors.17,18 The external ligand-binding component of VEGFR-3 differs from the other VEGF receptors in that the fifth immunoglobulin domain is cleaved during receptor processing to yield covalent, disulfide-linked subunits.19 In adults, VEGFR-1 and VEGFR-2 expression is limited to the vascular endothelium, monocytes (VEGFR-1), and primitive hematopoietic precursors (VEGFR-2), whereas VEGFR-3 is restricted to lymphatic endothelium.20–,24 The critical role for these receptors and that of VEGF has been demonstrated in gene inactivation studies. VEGF-A and the VEGFR-2 receptor are essential to embryonic vasculogenesis and definitive hematopoiesis.25–,27 In vitro investigations indicate that VEGFR-2 signaling is responsible for proliferation and differentiation of endothelial cells in response to VEGF-A stimulation, whereas VEGFR-1 has been implicated as a decoy receptor and potential activator of endothelial permeability.28 Ligand binding to VEGFR-3 is restricted to VEGF-C and VEGF-D, which together direct lymphangiogenesis.17,29,30 The actions of the remaining VEGF family members are less well-defined; however, receptor recognition for VEGF-B appears restricted to VEGFR-1 where it is believed to regulate extracellular matrix (ECM) degradation and endothelial cell migration via protease elaboration.31 VEGF-E is an alternate ligand for VEGFR-2 and has biologic activities similar to VEGF-A.32 Neuropilin-1 (NRP-1), a cell surface glycoprotein, acts as a co-receptor for VEGF-A165 to enhance its binding to VEGFR-2 on endothelial cells. Unlike the VEGF receptors, NRP-1 lacks an intracellular domain and therefore is not a direct mediator of cytokine signaling.33
VEGF-A exerts its biologic effects via interaction with either VEGFR-1 or VEGFR-2. VEGF receptors dimerize in response to ligand engagement, activating the tyrosine kinase located on the intracellular cytoplasmic tail. The resultant auto-phosphorylation of these receptors on specific tyrosine residues creates docking sites for cytoplasmic signaling molecules.34 Activation of VEGF receptors in endothelial cells triggers recruitment of adaptor and signaling proteins that contain Src homology domain-2 (Sh-2) including Shc and Sck.35,36 Recruitment and phosphorylation of these adaptor molecules permit their binding to the p85 subunit of phosphatidyl inositol-3 (PI-3) kinase and to phospholipase-Cg, activating the PI-3 kinase and ERK (stress activated protein kinase-1, 2) kinase signaling cascades.37–,39 PI-3 kinase phosphorylates Akt (protein kinase-B), a serine/threonine kinase involved in antiapoptotic signaling.40 Akt activation permits its translocation to the plasma membrane, where it phosphorylates and inactivates a variety of pro-apoptotic molecules, including BAD, caspase-9, mitochondrial Raf, and the forkhead transcription factor-1 (FKHR-1).41 Similarly, through PI-3 kinase activation, VEGF-A activates focal adhesion kinase in endothelial cells, a step that is critical to the recruitment and activation of cell adhesion molecules containing β1, β2, and β3 integrins.42,43 Indeed VEGFR-2 interaction with its ligand triggers receptor association with PI-3 kinase, vascular endothelial (VE)-cadherin and αVβ3, components that are essential to the creation of an active multimeric signaling complex. Thus, VEGFR-2 activation assures proper juxtaposition of the receptor with cytoskeletal proteins.44,45
VEGF Regulation
Transcriptional regulation of VEGF is influenced by a number of signals that converge upon the oxygen sensitive transcription factor, hypoxia-inducing-factor (HIF)-1a. HIF is a heterodimeric protein composed of α and β subunits.46 The β subunit is expressed constitutively, whereas the a subunit is a member of a family of DNA-binding proteins that contain trans-activation domains within the carboxy-terminus. Under normal oxygen conditions, HIF-1a is degraded rapidly by the ubiquitin-proteasome pathway.47 Hypoxia stabilizes the HIF-1a protein by inhibiting its proteasome degradation. The von Hippel-Lindau (VHL) tumor suppressor gene is one component of the ubiquitin ligase complex that ubiquinates and promotes the degradation of HIF-1a under normoxic conditions. Inactivation of VHL, as occurs in the von Hippel-Lindau syndrome, stabilizes HIF-1a and sustains tumor production of VEGF.48 Inactivation of a negative regulator of HIF-1a such as VHL is only one of many signals which converge upon HIF-1a to activate VEGF expression. Alternate signals include sustained RAS activation, β-integrin activation, stress-induced ERK signaling, and inactivation of p53.49–,52 In addition to its regulatory effects on VEGF, HIF-1a is a transcriptional activator of other genes including erythropoietin, inducible nitric oxide synthetase (iNOS), insulin growth factor (IGF-2), glycolytic enzymes, and tumor growth factor-β (TGF-β).53
Hemangioblast and Hematopoiesis
During embryogenesis, pluripotential hematopoietic stem cells originate from cell clusters in the ventral floor of the pre-umbilical dorsal aorta.54 These common hematopoietic/endothelial (HE) precursors share an antigenic phenotype characterized by expression of the progenitor cell antigen, CD34, and VEGFR-2.27,55 Murine gene knockout studies indicate that VEGFR-2 expression is required for vasculogenesis and for establishment of definitive hematopoiesis. Although HE progenitors can be generated in vitro from VEGFR-2 deficient embryonal stem cells, VEGFR-2 signaling is essential for progenitor migration and endothelial commitment. Post-natally, hemangioblasts, or HE progenitors, persist and contribute to long-term hematopoiesis and to the generation of circulating endothelial cells. Confirmation of leukemia specific gene expression (i.e., bcr/abl in chronic myeloid leukemia) and the identification of donor-specific DNA alleles (i.e., in allograft recipients) within vascular endothelium provides definitive proof that bone marrow-derived hemangioblast progeny contribute to the maintenance of endothelium in adults.56–,58 These primitive hemangioblast progenitors represent less than 2% of circulating CD34+ cells and display a surface phenotype characterized by CD34+, AC133+, VEGFR-2+, platelet endothelial cell adhesion molecule (PECAM), and the stromal derived factor-1 (SDF-1) receptor, CXCR-4.59 Under appropriate culture conditions, hematopoietic commitment of these precursors is demonstrable by acquisition of the leukocyte common antigen, CD45, and β1 integrins, whereas angioblasts display VE-cadherin.
VEGF receptorexpression extends beyond the primitive progenitor compartment during adult hematopoiesis. VEGFR-1 is expressed by monocytes and committed CD34+ progenitors, and is responsible for activation of migration and maturation skewing, respectively.22,23,60 With the exception of primitive hematopoietic progenitors, VEGFR-2 expression appears restricted to megakaryocytes.20 Within the adult bone marrow, cellular expression of angiogenic molecules outside of stromal elements is restricted to erythroblastic islands. Both VEGF-A and PIGF are secreted by erythroblasts within erythroid islands,61 suggesting that these cytokines may serve to recruit nurse macrophages and promote β-integrin activation in a paracrine fashion.
Laboratory and animal studies employing recombinant human VEGF (rhu-VEGF) have shown that the cytokine exerts both growth-promoting and growth-suppressive effects on hematopoietic progenitors that are lineage- and maturation-dependent. Rhu-VEGF impairs maturation of dendritic cells from CD34+ cells and promotes expansion of immature granulocyte-macrophage progenitors in animal models60 while inhibiting the formation of primitive erythroid and multipotent progenitors.62 Similarly, VEGF promotes osteoclast differentiation and bone remodeling and, as a consequence, contributes to bone resorption in animal models.63,64 In receptor-competent hematopoietic cells VEGF promotes resistance to radiation via induction of the antiapoptotic BCL-2 homologue, MCL-1, and activation of the Krüppel-type zinc finger transcription factor, ZK7.65– 67
Hematologic Malignancies
Tumor cells elaborate angiogenic factors as an essential feature of the malignant phenotype providing paracrine signaling for tumor growth. Hematopoietic malignancies, as progeny of receptor-competent HE progenitors, are distinguished from other tumors by the potential for autocrine growth stimulation and thereby offer the prospect of clinical benefit with antiangiogenic therapy. Thus, in AML and MDS, for example, myeloblasts and leukemic monocytes secrete VEGF and display VEGF receptors.68,69 In leukemia cell lines, rhu-VEGF directly promotes colony-forming capacity and β-1 integrin activation via the PI-3 kinase/Akt signal pathway, analogous to its effects in endothelial cells.69–,71 Similarly, neutralizing VEGF suppresses TNFα generation in MDS bone marrow stroma and promotes the recovery of primitive progenitors.69Table 4 summarizes the angiogenic profile of a number of hematologic malignancies and the relationship to clinical and biological features. Although basic fibroblast growth factor (bFGF) production is demonstrable in the majority of hematologic malignancies, expression on the malignant cells of functional bFGF receptors appears limited to chronic myeloid leukemia (CML)72,73 and MM.74 The relevance of tumor-derived angiogenic molecules to disease pathobiology is demonstrated by their linkage to prognosis and/or disease behavior. In NHL, for example, VEGF expression is common; however, co-expression of VEGF receptor(s) appears limited to intermediate- or high-grade lymphomas and adversely impacts overall survival.75–,77 Similarly, in AML, elevated cellular VEGF content is an independent prognostic variable associated with resistance to induction chemotherapy and inferior overall and disease-free survival. Leukemia-derived VEGF appears essential for bone marrow engraftment of AML cells in SCID mouse models.78,79 Indeed, rhu-VEGF promotes clonogenic growth of receptor competent AML cell lines and serves as an autocrine signal implicated in the central coalescence of immature myeloid precursors (i.e., abnormal localized immature precursors [ALIP]) in advanced MDS.69–,71 The encouraging results of treatment with the antiangiogenic agent thalidomide in patients with refractory myeloma suggests that angiogenesis represents an appropriate therapeutic target in the hematologic malignancies.80
Antiangiogenic Agents
The explosion in our understanding of neoplastic angiogenesis in the past decade has generated an ever-expanding catalogue of potential targets and therapeutics in clinical development. The angiogenesis antagonists can be classified into five distinct types, including the protease inhibitors that impact extracellular matrix remodeling, inhibitors of activated endothelial cell proliferation, inhibitors of survival signaling via vascular adhesion molecules, and agents that interfere with the generation of angiogenic molecules or receptor activity (Table 5 ). Among protease inhibitors, the matrix metalloprotease (MMP) inhibitors have undergone extensive testing in patients with solid tumors and are now being tested in hematologic malignancies. Most MMPs are soluble proenzymes that upon activation initiate proteolysis of basement membrane constituents such as collagen, laminin and proteoglycans.3 MMPs are classified according to their domain structure and substrate specificity. A leading MMP candidate for antiangiogenic therapy in hematologic malignancies is the synthetic gelatinase inhibitor, AG3340 (Prinomastat™),81 which, because of its selectivity, has limited clinical toxicity. The biological targets of gelatinases extend beyond basement membrane dissolution, and include the disruption of integrin interactions and the generation of soluble TNFα and fas ligand via liberation from membrane bound isoforms.82– 84 A common structural feature of MMP inhibitors is the presence of a metal binding group, in this case hydroxamate, that chelates the zinc ion present within the catalytic domain of the enzyme. AG3340 is currently completing phase II investigations in patients with MDS.
The inhibitors of endothelial cell activation have undergone the most extensive testing in hematologic malignancies. These agents, such as endostatin and synthetic pharmacophores, interfere with angiogenic factor-induced endothelial cell migration and proliferation and may possess additional biological effects. Thalidomide, a synthetic phamacophore, is a sedative and potent teratogen that has both antiinflammatory and antiangiogenic properties. Its biological effects include inhibition of bFGF- and VEGF-induced angiogenesis, suppression of TNFα generation by potentiating mRNA degradation, and the modulation of cell adhesion molecule activation.85,86 Thalidomide and its analogs augment natural killer cell cytotoxicity and exert direct cytostatic effects in myeloma cell lines unrelated to their antiangiogenic properties.87,88 Indeed, in a study involving 84 patients with refractory myeloma, durable antitumor responses were reported in up to 30% of patients.80 In MDS, approximately 30% of patients may achieve red blood cell transfusion independence following treatment with thalidomide.89 Although phase II and phase III testing of thalidomide in both myeloma and MDS are underway, its use is limited by neurologic toxicity. The thalidomide analog, CC-5013 (Revimid™), displays greater in vitro potency, costimulates the Th 1 immune response, and appears to be devoid of neurotoxicity. CC-5013 recently entered clinical trials in myeloma and MDS. Other angiogenic inhibitors that are completing testing in hematologic malignancies include arsenic trioxide and the farnesyl transferase inhibitors (FTI), SCH66336 (Schering Pharmaceuticals) and R115777 (Janssen). The FTIs inhibit ras protooncogene activation, an upstream transcriptional regulator of VEGF essential for endothelial cell proliferation. Moreover, gene inactivation studies indicate that VEGF is necessary for ras-induced cell transformation, suggesting that tumorigenicity of the ras oncogene is VEGF-dependent.90 Preliminary results of phase I studies of R115777 have shown single agent activity in AML.91
Agents that directly target angiogenic factors or their receptors offer the prospect for greater activity in receptor-competent hematologic malignancies by interrupting autocrine receptor signaling. The humanized monoclonal anti-VEGF antibody, Bevacizumab (Genentech) produces sustained neutralization of circulating VEGF and is now in phase II testing in MDS, lymphoma, AML, and solid tumors. The receptor tyrosine kinase inhibitors (RTKI) represent a particularly exciting class of synthetic, small molecule inhibitors of angiogenic receptor signaling. The first receptor antagonist to enter clinical testing in hematologic malignancies is SU5416 (Sugen), which impairs ligand-induced autophosphorylation of the VEGFR-1 and VEGFR-2 receptors and c-Kit. SU5416 inhibits VEGF-induced clonogenic response in leukemia cell lines and promotes apoptosis in myeloblasts from AML patients.70,92 Although it shows promising clinical activity in initial phase II testing,93 the utility of SU5416 is limited by its solubility and necessity for intravenous administration. Other RTKIs are entering phase II testing in AML and other receptor-competent hematologic malignancies, including SU11248 (Sugen), PTK787/ZK222584 (Novartis), and AG13736 (Agouron). These orally bioavailable inhibitors demonstrate broad receptor specificity, inhibiting the VEGF receptors, c-kit, PDGF, bFGF, and c-FMS. Although these agents may have inherent antineoplastic effects in receptor-competent malignancies, they may be more effective when combined with traditional DNA-interactive antineoplastics. As a group, this class of agents presents enormous potential to impact survival signaling from cytokine receptors, selected constitutively active TKs, integrin activation state, and angiogenic response. The angiogenic inhibitors are one of the most exciting classes of therapeutics to enter clinical testing in hematologic malignancies. Their clinical potential, however, will not be realized for several years to come.
III. Inhibiting Cell Cycle Progression and Proteasome Degradation Pathways: New Agents for Lymphoma and Myeloma
Bruce D. Cheson, MD*
NCI-CTEP, Executive Plaza, No.-741, Bethesda MD 20892
During the past few decades, results of clinical trials in the NHLs have failed to demonstrate a major impact on patient survival. Research strategies in the indolent NHL largely focused on comparisons of combinations and permutations of regimens including alkylating agents or nucleosides with or without anthracyclines or interferon. After decades of comparing various combination regimens in the aggressive NHL, CHOP (cyclophosphamide, doxorubicin, vincristine and prednisone) remained the standard. The recent availability of clinically active monoclonal antibodies has the potential to alter our approach to these patients. Nevertheless, there is considerable room for improvement in our current chemotherapy. The recent recognition of distinct molecular targets provides an opportunity to identify new drugs with unique mechanisms of action rather than relying on empiric combinations of nonspecific chemotherapy agents (Table 6 ). This section will present information on two such novel compounds as examples for the future development of chemotherapy agents.
Flavopiridol
Progression through the cell cycle is a tightly regulated process controlled by the phosphorylation and proteolysis of regulatory proteins including cyclins, cyclin-dependent kinases (cdk), and their inhibitors (Figure 7; see color page 551). Positive regulatory function of the cell cycle is afforded by p53, the retinoblastoma protein (Rb), and the p16 (INK4A) family of cyclin-dependent kinase inhibitors. Protein kinases play a central role in the function, proliferation, growth, transformation, and death of cells. The process of malignant transformation is associated with a progressive loss of cdk inhibitors and overexpression of cyclins, leading to a growth and proliferation advantage for the malignant cell. An important regulatory checkpoint occurs late in the G1 phase of the cell cycle where cyclin-dependent kinases are activated by cyclins to drive cells to the S phase.
The D-type cyclins, which associate with cdk4 and cdk6 to traverse G1 and with Rb and p53 to regulate G1/S progression, are often mutated in malignancy. Thus, blocking cell cycle progression with cdk inhibitors may lead to growth arrest and apoptosis.
Mantle cell lymphoma (MCL) is a distinct clinical, genetic and molecular entity. Clinically, it exhibits the worst features of the aggressive and indolent NHL and can behave in an aggressive manner. Like the indolent NHL, it is not a curable disease and has a median survival of only 2.5-3 years.1 At the molecular level, MCL is characterized by overexpression of the G1 cyclin, cyclin D1, generally in association with the chromosomal translocation t(11;14)(q13;q32).2 This translocation juxtaposes the enhancer element of the immunoglobulin heavy chain region on chromosome 14 to the bcl-1 or PRAD-1 protooncogene encoding the cyclin D1 protein on chromosome 11. As a consequence of the overexpression of cyclin D1, there is excess progression of cells from G1 through the S phase of the cell cycle. In addition, p53 mutations in patients with MCL are associated with a poor outcome and also with blastic morphology.3 The overexpression of cyclin D1 makes MCL a suitable tumor against which to study agents that target cyclin D1 (Figure 8; see color page 552).
Flavopiridol is a semisynthetic nonchlorinated flavone derivative that was first isolated from the plant alkaloid rohitukine from the leaves and stems of Amoora rohituka, and later from Dysoxylum binectariferum. Both plants are used in India as herbal medicines. It is the first active cyclin dependent kinase inhibitor to enter clinical trials in the US. Initial studies with a human breast cancer line showed that flavopiridol could inhibit in vitro growth with arrest of cells at G1 or G2 phases of the cell cycle. In vitro activity against cycling as well as noncycling cells has now also been demonstrated in a number of tumor cell lines. Flavopiridol inhibits a variety of protein kinases including cyclin D1, which is implicated in the pathogenesis of MCL, as well as cdk1, cdk23, and cdk4 through targeting of the ATP-binding site (Figure 9; see color page 552). It is active against all cdks at concentrations of 100-300 nM, which may be a major factor in its in vitro antitumor activity. In addition, it induces growth arrest, cytotoxic cell death and apoptotic changes in a variety of tumor types, including leukemias and lymphomas. The drug exhibits comparable activity against resting and proliferating cells.
Preclinical studies
Based on in vitro observations that flavopiridol can kill noncycling cells, studies were conducted to test the hypothesis that it might be advantageous to combine the drug with agents that inhibit cell cycle progression. Flavopiridol demonstrated sequence specific synergy in vitro with cell cycle active agents including fludarabine and cytarabine, as well as paclitaxel, topotecan, gemcitabine, irinotecan, doxorubicin, etoposide, cisplatin, and 5-FU.4 The greatest activity is observed when chemotherapy agents are administered prior to flavopiridol. The sequence specificity has been thought to reflect the arrest of cells in G1 and G2 during and 24 hours following flavopiridol administration. Although schedules that approximate continuous infusion have been active in a number of cell lines, intermittent bolus schedules have shown activity against lymphoma and solid tumor cell.
Flavopiridol induces apoptosis of B cell chronic lymphocytic leukemia (B-CLL) and lymphoma cells (Table 7 )58. Flavopiridol is cytotoxic to CLL cells at concentrations of 0.1-0.3 μM with only a 24-hour drug exposure, with no additional benefit from more prolonged exposure. Whether apoptosis occurs in association with a change in expression of bcl-2 or bax is controversial.57 Whereas König et al5 noted an association with bcl-2 expression, Byrd et al found apoptosis without bcl-2 modulation, even in the setting of decreased p53 expression, possibly related to cleavage of caspase 3.6,7 The mean attainable concentration in vivo was 2.4 times the concentration that resulted in apoptosis of 50% of human CLL cells in vitro.7 Unfortunately there was no apparent selectivity between the malignant lymphocytes and normal mononuclear cells. In the studies by Achenbach et al9 induction of apoptosis by flavopiridol appeared to be independent of bcl-2. In other studies, flavopiridol induced concentration dependent apoptosis of CLL cells with decreases in antiapoptotic proteins Mcl-1, X-linked inhibitor of apoptosis (XIAP), and BAG-1 in nearly all cases.10 Whether the disparities among these various studies regarding the role of bcl-2 reflects differences in doses or other factors is not clear. Flavopiridol may also have antiangiogenic properties.11 Arguello et al12 studied the toxicity and activity of flavopiridol in mice xenografts with either a leukemia or lymphoma cell line. There was little effect on most normal tissues; however, the spleens were smaller with reduced white pulp and absent follicle centers. The size of the thymus was decreased and markedly depleted of lymphocytes. Peripheral lymph nodes were also reduced in size and without follicle centers. Following administration of flavopiridol by bolus i.v. or intraperitoneal administration, 11 of 12 human HL-60 xenografts underwent complete regressions, and the animals remained disease-free for several months. Six of 8 animals with a lymphoma cell line (SUDHL-4) underwent either a major (n = 2) or complete (n = 4) regression, and the animals remained disease free for more than 60 days. This effect was shown to be both dose and schedule dependent.
Clinical trials
Flavopiridol is the first cdk inhibitor to be tested in clinical trials. The first two phase I trials with this agent used a 72-hour infusion schedule given every 2 weeks. This schedule resulted in blood levels that were inhibitory in vitro. The recommended phase II dose using this schedule was 78 mg/m2/d for 3 days. The dose limiting toxicity in the initial studies was secretory diarrhea. When antidiarrheal prophylaxis with cholestyramine and loperamide was used, hypotension became dose-limiting, along with a proinflammatory syndrome characterized by fever, fatigue, tumor pain, and alterations in acute phase reactants. Responses were observed in one patient each with renal cell carcinoma and colon cancer, and a minor response was reported in a patient with NHL. A number of patients also experience prolonged stable disease, suggesting the possibility of a cytostatic effect. Other schedules of administration, including a 1-hour daily bolus, have also been tested. The maximum tolerated dose (MTD) on the 1-, 3-, and 5-day schedules were 37.5, 50, and 62.5 mg/m2/d, respectively. Other trials are exploring schedules involving 1- and 3-hour infusions or a bolus followed by a continuous infusion in CLL and other hematologic diseases and solid tumors.
Because of its effect on cyclin D1, flavopiridol was considered early on as a potential agent for the treatment of patients with MCL. Two such trials have been conducted: the Dana-Farber Institute, using a 72-hour infusion, and in the National Cancer Institute (NCI)-Canada trial. In the latter flavopiridol was administered at a dose of 50 mg/m2 over 1 hour daily for 3 days every 3 weeks. Patients received from one to more than 6 cycles. Severe toxicities included diarrhea (n = 5, including 3 patients who did not receive appropriate prophylaxis) and fatigue (78% overall, < 5% grade IV). The diarrhea correlates inversely with systemic glucuronidation of flavopiridol.13 Hematologic toxicity has been mostly mild to moderate with a few cases of severe neutropenia. A number of patients also experienced thrombosis that was thought to be drug related. In the Dana-Farber trial, activity was minimal (M. Shipp, personal communication). In the NCI-Canada trial there were 3 partial responses and 11 patients with stable disease (E. Eisenhauer, J. Connors, personal communication). These disparate observations suggest a possible schedule-dependent difference in efficacy. Similar observations have been made in CLL trials (J. Byrd, personal communication). Thus, in phase II trials using a 1-hour schedule, activity has been observed both in MCL and CLL where no activity was noted using the longer infusion schedules.
Clearly, this agent has limited potential as monotherapy in the lymphoid malignancies studied thus far; however, it has potential in combination with a variety of chemotherapy agents. Multiagent strategies are being planned, primarily with the shorter infusion schedule in a collaborative effort between Aventis Pharmaceutical and the NCI.
Proteasome Inhibitors
The proteasome is a large, multicentric protease complex with a pivotal role in cellular protein regulation. It is composed of a two copies of a 19S regulatory protein that recognizes substrates adorned with ubiquitin chains. The two copies form the 20S core particle that contains the catalytic protease functions. The proteasome degrades proteins that have been conjugated to ubiquitin (the ubiquitin-proteasome pathway)14– 17 (Figure 10 ). The ubiquitin-proteasome pathway plays a critical role in the degradation of intracellular proteins involved in cell cycle control, transcription factor activation, apoptosis, cell trafficking, and tumor growth through an ATP-dependent process. Some of the proteins that undergo the degradation include the cyclins and cdk inhibitors. Many tumor cells depend on rapid cell cycling, which requires expression and degradation of numerous regulatory proteins. Cells accumulate in the G2-M phase of the cell cycle with a decrease of cells in G1. Unfortunately, the indolent lymphoid malignancies are not rapidly cycling and tend to be in G0. Nevertheless, proteasome inhibitors also induce apoptosis despite cellular accumulation of the cdk inhibitors p21 and p27 and irrespective of p53 status.
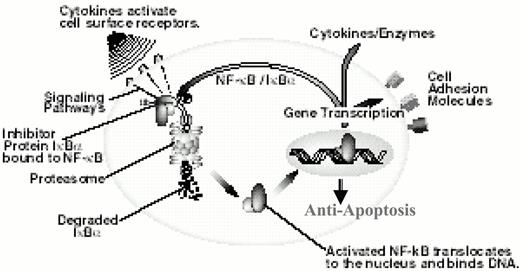
The proteasome is also required for activation of the nuclear transcription factor NF-κB, which plays a role in maintaining cell viability through the transcription of inhibitors of apoptosis in response to environmental stress or cytotoxic agents.18
Based on these observations, targeting the proteasome has become a novel new approach to cancer therapy. Several naturally occurring and synthetic proteasome inhibitors have been identified including the boronic acid peptides such as PS-341; the natural product lactacystin, a streptomyces metabolite; MG0132; and a synthetic peptide aldehyde. PS-341 is the compound being most widely studied in the clinic. This dipeptidyl boronic acid is a specific and selective inhibitor of the 26S proteasome.17 PS-341 may also lead to an induction of apoptosis (Figure 11 ). Moreover, enhanced tumor efficacy in combination with other chemotherapy agents and radiation has been suggested. In vitro studies have demonstrated marked synergy between PS-341 and chemotherapy drugs such as the topoisomerase I inhibitor irinotecan (CPT-11). CPT-11 can increase NF-κB leading to greater transcription of factors that protect cells from apoptosis.19 PS-341 may block activation of NF-κB, thus potentiating the activity of the chemotherapy drug. Since NF-kB can induce drug resistance, this agent may make cells more chemosensitive.20
PS-341 has demonstrated activity against many tumor types in vitro and is a poor substrate for the multi-drug resistance transporter. It is also active even in the setting of overexpression of bcl-2 and has shown a lack of acquired drug resistance. Using a prostate cancer cell line, Adams et al17 found that exposure of the cells to PS-341 results in accumulation in the G-M phase of the cell cycle. Intravenous treatment of animals with this agent led to a 60% decrease in tumor size. Another proteasome inhibitor, PSI, also induces apoptosis of myeloid leukemia cells to a greater degree than it affects normal hematopoietic progenitors.21 PSI has also shown activity against a murine model of Burkitt's lymphoma.22 PS-341 has also been shown to inhibit growth, induces apoptosis conferred by IL-6, and overcomes drug resistance in human myeloma cells.23 These effects have been shown to be additive with dexamethasone, a highly active agent in MM. Low levels of the cdk inhibitor p27 in MCL may result from increased proteasome-mediated degradation,24 making this tumor also a possible target for proteasome inhibitors.
Proteasome inhibitors may have a potential role in the therapy of patients with CLL. First, the ubiquitin proteasome-dependent protein processing may be altered in CLL cells.25 In addition, proteasome inhibition has been shown to induce apoptosis of CLL lymphocytes at concentrations that do not have that effect on normal cells. Masdehors et al25 studied cells from 50 patients with previously untreated CLL. They found that CLL lymphocytes were significantly more sensitive to the induction of apoptosis by the proteasome inhibitor lactacystin than were normal lymphocytes. Furthermore, lactacystin sensitized chemoresistant and radioresistant CLL cells to apoptosis induced by TNFα.26,27 Proteasome inhibition also induces DNA fragmentation and apoptosis of CLL lymphocytes, even those resistant to glucocorticoids.28,29 The changes were also associated with inhibition of NF-κB.
Toxicology studies in rodents and primates identified adverse effects including gastrointestinal toxicity, anorexia, emesis and diarrhea. Hematologic toxicity was not noted. Of interest was that there was lymphocyte depletion of the spleen and thymus.
PS-341 is currently in clinical trials for a variety of solid tumors, leukemias and lymphomas. A number of doses and schedules of administration are under investigation. In a phase I trial in patients with hematologic malignancies30 PS-341 was administered as a twice weekly bolus injection for 4 consecutive weeks followed by a 2-week rest period. Responses were assessed after each 6-week cycle. As of the preliminary publication, 3 patients were treated at each of the first three dose levels, most of whom were heavily pretreated. Included were 1 patient with refractory anemia with excess blasts (RAEB), 2 with Hodgkin's disease, 3 with NHL, and 3 with MM. Although the MTD had not yet been reached, two of the MM patients experienced responses with one major response with > 50% decrease in IgG and normal numbers of bone marrow plasma cells. Other schedules under investigation include twice weekly every other week, and weekly for 4 weeks.
The maximum pharmacodynamic effect of PS-341 on 20S proteasome activity in the peripheral blood is observed at 1-hour post dose, measured by an inhibition assay.31 The compound has been well tolerated at the levels of 20S inhibition of > 60% that are considered essential for its antitumor efficacy. Toxicities encountered to date including dose-limiting neuropathy as well as fatigue, gastrointestinal symptoms, and thrombocytopenia. An active development strategy is planned by Millennium Pharmaceuticals in collaboration with the NCI.
We are in an exciting period in the treatment of the NHL. The therapeutic paradigm for the treatment of indolent NHL is rapidly moving away from alkylating agent-based regimens to those that include purine analogs and, more recently, monoclonal antibodies. However, no single chemotherapeutic or biologic agent alone is likely to significantly prolong the survival of these patients. Future trials should develop rational combinations of chemotherapy and biological agents based on a better understanding of mechanisms of drug action and resistance, interactions among agents, and tumor biology. To expedite the identification of effective strategies, patients should be entered onto clinical trials addressing important research questions. Identification of the most promising of these drugs and regimens will be facilitated by recently published guidelines for assessment of treatment response.32 The large number of new, unique therapeutic agents available for clinical trials should provide optimism for improving the cure rate for patients with NHL.
Properties of BCL-2.
| •Oncogenic protein |
| •Anti-apoptotic |
| •Mitochondrial, endoplasmic reticulum, nuclear membrane localizations |
| •Homotypic and heterotypic dimerization within family |
| •Membrane channel/pore function |
| •Cytochrome C release from mitochondria via BCL-2 family channels regulates cell fate under stress |
| •Oncogenic protein |
| •Anti-apoptotic |
| •Mitochondrial, endoplasmic reticulum, nuclear membrane localizations |
| •Homotypic and heterotypic dimerization within family |
| •Membrane channel/pore function |
| •Cytochrome C release from mitochondria via BCL-2 family channels regulates cell fate under stress |
Phase I study of G3139 and cyclophosphamide in relapsed follicular lymphoma.
| Level . | G3139 mg/kg/day CIVI (day 1 to 14) . | Cyclophosphamide mg/m2/IV (day 8) . |
|---|---|---|
| 1 | 0.6 | 250 done |
| 2 | 1.2 | 250 done |
| 3 | 2.3 | 250 done |
| 4 | 2.3 | 500 done |
| 5 | 2.3 | 750 ongoing |
| 6 | 3.1 | 1000 |
| 7 | 5.0 | 1000 |
| Level . | G3139 mg/kg/day CIVI (day 1 to 14) . | Cyclophosphamide mg/m2/IV (day 8) . |
|---|---|---|
| 1 | 0.6 | 250 done |
| 2 | 1.2 | 250 done |
| 3 | 2.3 | 250 done |
| 4 | 2.3 | 500 done |
| 5 | 2.3 | 750 ongoing |
| 6 | 3.1 | 1000 |
| 7 | 5.0 | 1000 |
Endogenous stimulators and inhibitors of angiogenesis.
| . | Angiogenic Molecules . | Native Inhibitors . |
|---|---|---|
| Abbreviations: VEGF, vascular endothelial growth factor; PIGF, placental growth factor; iNOS, inducible nitric oxide synthetase; MMP, matrix metalloproteases | ||
| Growth factors | VEGF (A-D), PIGF | Interferon (IFN)-α,γ |
| Angiogenin | ||
| Angiotropin | ||
| Epidermal growth factor (EGF) | ||
| Fibroblast growth factor (acidic and basic; FGF) | Prolactin (16 Kd fragment), IFN-α,γ | |
| Hepatocyte growth factor/scatter factor (HGF, SF) | ||
| Platelet-derived growth factor (PDGF) | ||
| Tumor necrosis factor-α (TNFα) | ||
| Interleukin-8 (IL-8) Insulin-like growth factor-1 (IGF-1) | ||
| Proteases and Protease Inhibitors | Cathepsin | Tissue inhibitor of metalloprotease (TIMP-1, TIMP-2) |
| Gelatinase-A, -B (MMP2,9) | ||
| Stromelysin | ||
| Urokinase-type plasminogen activator (uPA) | Plasminogen activator- inhibitor-1 (PAI-1) | |
| Trace Elements | Copper | Zinc |
| Oncogenes | c-myc | p53 Rb |
| ras | ||
| c-src | ||
| v-raf | ||
| c-jun | ||
| Signal Transduction Enzymes | Thymidine phosphorylase | |
| RAS - arnesyl transferase | ||
| Geranylgeranyltransferase | ||
| Cytokines | Interleukin-1 | Interleukin-10 |
| Interleukin-6 | Interleukin-12 | |
| Interleukin-8 | ||
| Endogenous | αvβ3 integrin | Angionpoietin-2 |
| Angionpoietin-1(Ang-1) | Angiotensin | |
| Antionstatin II (AT1 receptor) | Angiotensin II (AT2 receptor) | |
| Endothelin (ETB receptor) | Caveolin-1, caveolin-2 | |
| Erythropoietin | Endostatin | |
| Hypoxia | Interferon-α | |
| iNOS | Isoflavones | |
| Platelet-activating factor (PAF) | Platelet factor-4 | |
| Prostaglandin E, COX-2 | ||
| Thrombopoietin | Thrombospondin | |
| Troponin-1 | ||
| . | Angiogenic Molecules . | Native Inhibitors . |
|---|---|---|
| Abbreviations: VEGF, vascular endothelial growth factor; PIGF, placental growth factor; iNOS, inducible nitric oxide synthetase; MMP, matrix metalloproteases | ||
| Growth factors | VEGF (A-D), PIGF | Interferon (IFN)-α,γ |
| Angiogenin | ||
| Angiotropin | ||
| Epidermal growth factor (EGF) | ||
| Fibroblast growth factor (acidic and basic; FGF) | Prolactin (16 Kd fragment), IFN-α,γ | |
| Hepatocyte growth factor/scatter factor (HGF, SF) | ||
| Platelet-derived growth factor (PDGF) | ||
| Tumor necrosis factor-α (TNFα) | ||
| Interleukin-8 (IL-8) Insulin-like growth factor-1 (IGF-1) | ||
| Proteases and Protease Inhibitors | Cathepsin | Tissue inhibitor of metalloprotease (TIMP-1, TIMP-2) |
| Gelatinase-A, -B (MMP2,9) | ||
| Stromelysin | ||
| Urokinase-type plasminogen activator (uPA) | Plasminogen activator- inhibitor-1 (PAI-1) | |
| Trace Elements | Copper | Zinc |
| Oncogenes | c-myc | p53 Rb |
| ras | ||
| c-src | ||
| v-raf | ||
| c-jun | ||
| Signal Transduction Enzymes | Thymidine phosphorylase | |
| RAS - arnesyl transferase | ||
| Geranylgeranyltransferase | ||
| Cytokines | Interleukin-1 | Interleukin-10 |
| Interleukin-6 | Interleukin-12 | |
| Interleukin-8 | ||
| Endogenous | αvβ3 integrin | Angionpoietin-2 |
| Angionpoietin-1(Ang-1) | Angiotensin | |
| Antionstatin II (AT1 receptor) | Angiotensin II (AT2 receptor) | |
| Endothelin (ETB receptor) | Caveolin-1, caveolin-2 | |
| Erythropoietin | Endostatin | |
| Hypoxia | Interferon-α | |
| iNOS | Isoflavones | |
| Platelet-activating factor (PAF) | Platelet factor-4 | |
| Prostaglandin E, COX-2 | ||
| Thrombopoietin | Thrombospondin | |
| Troponin-1 | ||
Angiogenic profile of hematologic malignancies.
| . | . | . | Angiogenic Receptors . | ||||
|---|---|---|---|---|---|---|---|
| Malignancy . | Pro-Angiogenic Molecules . | MVD . | VEGFR-1 . | VEGFR-2 . | FGF-R . | Clinical/Biological Correlation . | Reference . |
| Abbreviations: CR, complete remission; s, serum or plasma; u, urinary; c, cellular; CRP, C-reactive protein; B2M, beta2-microglobulin; LN, lymph node; MMM, myelofibrosis with myeloid metaplasia; Unk, unknown; IL-6, interleukin-6; ALIP, abnormal localized immature precursors; AML, acute myelogenous leukemia; MDS, myelodysplastic syndrome; ALL, acute lymphoblastic leukemia; NHL, non-Hodgkin's lymphoma; CLL, chronic lymphocytic leukemia; CML, chronic myeloid leukemia; MVD, microvessel density; OS, overall survival; DFS, disease-free survival; BM, bone marrow; VEGF, vascular endothelial growth factor; FGF, fibroblast growth factor; bFGF, basic FGF; SDF-1, stromal-derived factor 1 | |||||||
| * Denotes independent prognostic factor. | |||||||
| AML | s,cVEGF* | ↑BM | ++ | +/- | Unk | Leukocytosis; ↓CR*, OS*, DFS* (VEGF) | 68,69,71,72,78, 94-96 |
| cMMP 2,9 | |||||||
| sFGF | |||||||
| sSDF-1 | |||||||
| MDS | VEGF | ↑BM | ++ | +/- | Unk | Survival (VEGF); | 69,72,96-9 |
| cMMP-2,cMMP-9 | blast % (MVD); | ||||||
| sSDF-1 | TNFα generation; ALIP | ||||||
| sIL-8 | |||||||
| MMM | ↑BM | Unk | Unk | Unk | Survival (MVD)* | 99 | |
| Splenomegaly (MVD) | |||||||
| Myeloma | s,cVEGF | ↑BM | - | - | + | Overall survival (MVD) | 20,74,100-102 |
| sbFGF* | Trisomy 13, CRP, B2M | ||||||
| cMMP-2 | ↑ stromal IL-6 | ||||||
| ALL | s,ubFGF | ↑BM | Unk | Unk | Unk | 72,103,104 | |
| sSDF-1 | |||||||
| cMMP-2,cMMP-9 | |||||||
| NHL | sbFGF* | ↑LN | + | +/- | Unk | Survival* (VEGF, FGF) | 75-77,105,106 |
| s,cVEGF* | High grade histology (VEGF, FGF) | ||||||
| Advanced stage | |||||||
| CLL | s,cVEGF | ↑BM | Unk | Unk | - | Advanced stage (MVD, VEGF) | 72,73,107-109 |
| c,sbFGF | Time to progression (VEGF) | ||||||
| sSDF-1 | Fludarabine resistance (cFGF) | ||||||
| CML | sVEGF | ↑BM | Unk | Unk | + | 72,73 | |
| c,sbFGF | |||||||
| sSDF-1 | |||||||
| . | . | . | Angiogenic Receptors . | ||||
|---|---|---|---|---|---|---|---|
| Malignancy . | Pro-Angiogenic Molecules . | MVD . | VEGFR-1 . | VEGFR-2 . | FGF-R . | Clinical/Biological Correlation . | Reference . |
| Abbreviations: CR, complete remission; s, serum or plasma; u, urinary; c, cellular; CRP, C-reactive protein; B2M, beta2-microglobulin; LN, lymph node; MMM, myelofibrosis with myeloid metaplasia; Unk, unknown; IL-6, interleukin-6; ALIP, abnormal localized immature precursors; AML, acute myelogenous leukemia; MDS, myelodysplastic syndrome; ALL, acute lymphoblastic leukemia; NHL, non-Hodgkin's lymphoma; CLL, chronic lymphocytic leukemia; CML, chronic myeloid leukemia; MVD, microvessel density; OS, overall survival; DFS, disease-free survival; BM, bone marrow; VEGF, vascular endothelial growth factor; FGF, fibroblast growth factor; bFGF, basic FGF; SDF-1, stromal-derived factor 1 | |||||||
| * Denotes independent prognostic factor. | |||||||
| AML | s,cVEGF* | ↑BM | ++ | +/- | Unk | Leukocytosis; ↓CR*, OS*, DFS* (VEGF) | 68,69,71,72,78, 94-96 |
| cMMP 2,9 | |||||||
| sFGF | |||||||
| sSDF-1 | |||||||
| MDS | VEGF | ↑BM | ++ | +/- | Unk | Survival (VEGF); | 69,72,96-9 |
| cMMP-2,cMMP-9 | blast % (MVD); | ||||||
| sSDF-1 | TNFα generation; ALIP | ||||||
| sIL-8 | |||||||
| MMM | ↑BM | Unk | Unk | Unk | Survival (MVD)* | 99 | |
| Splenomegaly (MVD) | |||||||
| Myeloma | s,cVEGF | ↑BM | - | - | + | Overall survival (MVD) | 20,74,100-102 |
| sbFGF* | Trisomy 13, CRP, B2M | ||||||
| cMMP-2 | ↑ stromal IL-6 | ||||||
| ALL | s,ubFGF | ↑BM | Unk | Unk | Unk | 72,103,104 | |
| sSDF-1 | |||||||
| cMMP-2,cMMP-9 | |||||||
| NHL | sbFGF* | ↑LN | + | +/- | Unk | Survival* (VEGF, FGF) | 75-77,105,106 |
| s,cVEGF* | High grade histology (VEGF, FGF) | ||||||
| Advanced stage | |||||||
| CLL | s,cVEGF | ↑BM | Unk | Unk | - | Advanced stage (MVD, VEGF) | 72,73,107-109 |
| c,sbFGF | Time to progression (VEGF) | ||||||
| sSDF-1 | Fludarabine resistance (cFGF) | ||||||
| CML | sVEGF | ↑BM | Unk | Unk | + | 72,73 | |
| c,sbFGF | |||||||
| sSDF-1 | |||||||
Anti-angiogenic agents in clinical trials.
| Target . | Agent (Source) . | Description . | Action . | Ref. . |
|---|---|---|---|---|
| Abbreviations: MoAb, monoclonal antibody; VEGF, vascular endothelial growth factor; EC, endothelial cell; ECM, extracellular matrix; MMP, matrix metalloprotease; TKI, tyrosine kinase inhibitor; IFN, interferon; FTI, farnesyl transferase inhibitor; i.v., intravenous; po, per oral; IL, interleukin; FGF, fibroblast growth factor; bFGF, basic FGF; TNFα, tumor necrosis factor-α | ||||
| Angiogenic Factors | Bevacizumab (Genentech) | humanized MoAb | VEGF neutralization | 110,111 |
| IM862 (Cytran) | small peptide | ↓VEGF + bFGF production, ‐IL-12 | 112 | |
| IFNα (Schering, Roche) | recombinant protein | ↓VEGF + bFGF production, | 113 | |
| ↓EC proliferation | ||||
| Angiongenic Receptors | 2C3 | murine MoAb | VEGFR-2 antagonist | 114 |
| CD101 (ImClone) | rat MoAb | VEGFR-2 antagonist | 115 | |
| Angiozyme (Ribozyme) | VEGFR catalytic ribozyme | VEGFR-1,2 mRNA inactivation | 116 | |
| SU5416 (Sugen) | small molecule, i.v. | VEGFR1,2-TKI, c-kit, PDGFR | 92,117 | |
| SU11248 (Sugen) | small molecule, po | VEGFR1,2-TKI, c-kit, PDGFR, FGF | ||
| PTK787/ZK222584 (Novartis) | small molecule, po | VEGFR1,2-TKI, c-kit, PDGFR, FGF, c-fms | 118 | |
| AG13736 (Agouron) | small molecule, po | VEGFR1,2-TKI, c-kit, PDGFR, FGF | ||
| Vascular Adhesion Molecules | SCH221153 (Schering) | peptidomimetic | αvβ3 + αvβ5 antagonist, EC apoptosis | 119 |
| Vitaxin (Ixsys) | humanized MoAb | αvβ3antagonist, EC apoptosis | 120 | |
| Activated Endothelial Cells | Endostatin (EntreMed) | collagen XVIII fragment | ↓EC proliferation, EC apoptosis | 121,122 |
| Vasostatin | calreticulin fragment | ↓EC proliferation | 123 | |
| TNP-470 (TAP Pharma.) | fumagillin analogue | ↓EC proliferation | 124 | |
| 2-methoxyestradiol | estrogen metabolite | EC apoptosis | 125 | |
| Thalidomide (Celgene) | phthalimidoglutarimide | ↓EC proliferation (bFGF,VEGF) ↓TNFα | 85 | |
| CC-5013 (Celgene) | phtaloyl analogue | ↓EC proliferation, ↓TNFα, Th1 stimulator | 86 | |
| Arsenic trioxide (CTI) | trivalent arsenical | EC apoptosis, tumor cytotoxin | 126 | |
| SCH66336 (Schering) | non-peptide, FTI | ↓EC proliferation, ↓VEGF | 127,128 | |
| R115777 (Janssen) | non-peptide, FTO | ↓EC proliferation, ↓VEGF | 91 | |
| ECM Remodelling | Prinomastat (Agouron) | non-peptide hydroxymate | MMP inhibition | 81 |
| Target . | Agent (Source) . | Description . | Action . | Ref. . |
|---|---|---|---|---|
| Abbreviations: MoAb, monoclonal antibody; VEGF, vascular endothelial growth factor; EC, endothelial cell; ECM, extracellular matrix; MMP, matrix metalloprotease; TKI, tyrosine kinase inhibitor; IFN, interferon; FTI, farnesyl transferase inhibitor; i.v., intravenous; po, per oral; IL, interleukin; FGF, fibroblast growth factor; bFGF, basic FGF; TNFα, tumor necrosis factor-α | ||||
| Angiogenic Factors | Bevacizumab (Genentech) | humanized MoAb | VEGF neutralization | 110,111 |
| IM862 (Cytran) | small peptide | ↓VEGF + bFGF production, ‐IL-12 | 112 | |
| IFNα (Schering, Roche) | recombinant protein | ↓VEGF + bFGF production, | 113 | |
| ↓EC proliferation | ||||
| Angiongenic Receptors | 2C3 | murine MoAb | VEGFR-2 antagonist | 114 |
| CD101 (ImClone) | rat MoAb | VEGFR-2 antagonist | 115 | |
| Angiozyme (Ribozyme) | VEGFR catalytic ribozyme | VEGFR-1,2 mRNA inactivation | 116 | |
| SU5416 (Sugen) | small molecule, i.v. | VEGFR1,2-TKI, c-kit, PDGFR | 92,117 | |
| SU11248 (Sugen) | small molecule, po | VEGFR1,2-TKI, c-kit, PDGFR, FGF | ||
| PTK787/ZK222584 (Novartis) | small molecule, po | VEGFR1,2-TKI, c-kit, PDGFR, FGF, c-fms | 118 | |
| AG13736 (Agouron) | small molecule, po | VEGFR1,2-TKI, c-kit, PDGFR, FGF | ||
| Vascular Adhesion Molecules | SCH221153 (Schering) | peptidomimetic | αvβ3 + αvβ5 antagonist, EC apoptosis | 119 |
| Vitaxin (Ixsys) | humanized MoAb | αvβ3antagonist, EC apoptosis | 120 | |
| Activated Endothelial Cells | Endostatin (EntreMed) | collagen XVIII fragment | ↓EC proliferation, EC apoptosis | 121,122 |
| Vasostatin | calreticulin fragment | ↓EC proliferation | 123 | |
| TNP-470 (TAP Pharma.) | fumagillin analogue | ↓EC proliferation | 124 | |
| 2-methoxyestradiol | estrogen metabolite | EC apoptosis | 125 | |
| Thalidomide (Celgene) | phthalimidoglutarimide | ↓EC proliferation (bFGF,VEGF) ↓TNFα | 85 | |
| CC-5013 (Celgene) | phtaloyl analogue | ↓EC proliferation, ↓TNFα, Th1 stimulator | 86 | |
| Arsenic trioxide (CTI) | trivalent arsenical | EC apoptosis, tumor cytotoxin | 126 | |
| SCH66336 (Schering) | non-peptide, FTI | ↓EC proliferation, ↓VEGF | 127,128 | |
| R115777 (Janssen) | non-peptide, FTO | ↓EC proliferation, ↓VEGF | 91 | |
| ECM Remodelling | Prinomastat (Agouron) | non-peptide hydroxymate | MMP inhibition | 81 |
New chemotherapy drugs for non-Hodgkin's lymphomas.
| Mechanism of Action . | Representative Agents . |
|---|---|
| Cytotoxic | Oxaliplatin |
| Apoptosis induction | nucleosides, retinoids, arsenicals |
| Protein kinase C inhibition | Bryostatin |
| Cyclin inhibition | Flavopiridol, UCN-01, rapamycin |
| Farnesyl transferase inhibitors | R115777, BMS-214662 |
| Histone deacetylation | Depsipeptide |
| Antiangiogenesis | Thalidomide, SU5416, SU6668 |
| Proteasome inhibition | PS-134 |
| Antitutubulin agents | Epophilone |
| Mechanism of Action . | Representative Agents . |
|---|---|
| Cytotoxic | Oxaliplatin |
| Apoptosis induction | nucleosides, retinoids, arsenicals |
| Protein kinase C inhibition | Bryostatin |
| Cyclin inhibition | Flavopiridol, UCN-01, rapamycin |
| Farnesyl transferase inhibitors | R115777, BMS-214662 |
| Histone deacetylation | Depsipeptide |
| Antiangiogenesis | Thalidomide, SU5416, SU6668 |
| Proteasome inhibition | PS-134 |
| Antitutubulin agents | Epophilone |
Effects of flavopiridol on CLL cells.
| Induction of apoptosis |
| Independent of prior fludarabine |
| Activation of caspase 3 |
| Cell cycle arrest |
| Decreased expression of p53 protein |
| Cytotoxicity independent of p53 status |
| Down-regulation of Mcl-1 |
| Induction of apoptosis |
| Independent of prior fludarabine |
| Activation of caspase 3 |
| Cell cycle arrest |
| Decreased expression of p53 protein |
| Cytotoxicity independent of p53 status |
| Down-regulation of Mcl-1 |
Phosphodiester substitutions in first generation antisense oligonucleotides.
Targeting Bcl-2 may promote apoptosis following chemotherapy and irradiation.
Survival of cohorts of 6 mice treated with oligonucleotides alone (left panel) or with cyclophosphamide (CY) (right panel).
All six surviving animals treated with cyclophosphamide and G3139 sacrificed at 90 days with no molecular evidence of disease detected.
Saline=control animals ; AS=antisense oligonucleotide G3139 directed at bcl-2 ; SN=reverse sequence sense control ; MM= 2-base mismatch control.
Survival of cohorts of 6 mice treated with oligonucleotides alone (left panel) or with cyclophosphamide (CY) (right panel).
All six surviving animals treated with cyclophosphamide and G3139 sacrificed at 90 days with no molecular evidence of disease detected.
Saline=control animals ; AS=antisense oligonucleotide G3139 directed at bcl-2 ; SN=reverse sequence sense control ; MM= 2-base mismatch control.
Interaction of vascular endothelial growth factor (VEGF) family members with their cognate receptors on endothelial cells.
The VEGF receptors harbor seven extracellular immunoglobulin (Ig)-homology domains. The fifth Ig domain of VEGFR-3 is cleaved after biosynthesis to yield a stable disulfide bond linking the Ig subunits. VEGFR-1 and VEGFR-2 initiate signals essential to the angiogenic response, whereas VEGFR-3 regulates lymph angiogenesis. NRP-1 (neuropilin-1) binds to the carboxy-terminal sequence of VEGF165 to enhance binding of the angiogenic molecule to the VEFGR-2 receptor.
Abbreviations: TK, tyrosine kinase; MMP, matrix metalloproteases; PIGF, placental growth factor.
Interaction of vascular endothelial growth factor (VEGF) family members with their cognate receptors on endothelial cells.
The VEGF receptors harbor seven extracellular immunoglobulin (Ig)-homology domains. The fifth Ig domain of VEGFR-3 is cleaved after biosynthesis to yield a stable disulfide bond linking the Ig subunits. VEGFR-1 and VEGFR-2 initiate signals essential to the angiogenic response, whereas VEGFR-3 regulates lymph angiogenesis. NRP-1 (neuropilin-1) binds to the carboxy-terminal sequence of VEGF165 to enhance binding of the angiogenic molecule to the VEFGR-2 receptor.
Abbreviations: TK, tyrosine kinase; MMP, matrix metalloproteases; PIGF, placental growth factor.
The ubiquitin-proteasome pathway.
The proteasome is a multicentric protease complex that plays a pivotal role in cellular protein regulation. In order for a protein to be suitable for degradation, it must first be adorned with ubiquitin. The ubiquitin-proteasome pathway plays a critical role in the degradation of intracellular proteins involved in cell cycle control and tumor growth.
The ubiquitin-proteasome pathway.
The proteasome is a multicentric protease complex that plays a pivotal role in cellular protein regulation. In order for a protein to be suitable for degradation, it must first be adorned with ubiquitin. The ubiquitin-proteasome pathway plays a critical role in the degradation of intracellular proteins involved in cell cycle control and tumor growth.
PS-341 is a specific and selective inhibitor of the 26S proteasome.
NF-κB is activated when the proteasome degrades the inhibitor protein 1κBa resulting in downregulation of multiple gene products. NF-κB plays a role in maintaining cell viability through the transcription of inhibitors of apoptosis. PS-341 can block activation of NF-κB, which may induce apoptosis and also make cells more sensitive to a variety of chemotherapy agents.
PS-341 is a specific and selective inhibitor of the 26S proteasome.
NF-κB is activated when the proteasome degrades the inhibitor protein 1κBa resulting in downregulation of multiple gene products. NF-κB plays a role in maintaining cell viability through the transcription of inhibitors of apoptosis. PS-341 can block activation of NF-κB, which may induce apoptosis and also make cells more sensitive to a variety of chemotherapy agents.