Abstract
This update discusses what is known regarding embryonic and adult tissue-derived pluripotent stem cells, including the mechanisms underlying self-renewal without senescence, differentiation in multiple cell types both in vitro and in vivo, and future potential clinical uses of such stem cells.
In Section I, Dr. Lansdorp reviews the structure and function of telomerase, the enzyme that restores telomeric ends of chromosomes upon cell division, highly present in embryonic stem cells but not adult stem cells. He discusses the structure and function of telomerase and signaling pathways activated by the enzyme, with special emphasis on normal and leukemic hematopoietic stem cells.
In Section II, Dr. Pera reviews the present understanding of mammalian pluripotent embryonic stem cells. He discusses the concept of pluripotentiality in its embryonic context, derivation of stem cells from embryonic or fetal tissue, the basic properties of the stem cells, and methods to produce specific types of differentiated cell from stem cells. He examines the potential applications of stem cells in research and medicine and some of the barriers that must be crossed to achieve these goals.
In Section III, Dr. Verfaillie reviews the present understanding of pluripotency of adult stem cells. She discusses the concept of stem cell plasticity, a term used to describe the greater potency described by several investigators of adult tissue-derived stem cells, critically reviews the published studies demonstrating stem cell plasticity, and possible mechanisms underlying such plasticity, and examines the possible role of pluripotent adult stem cells in research and medicine.
I. The Telomere Checkpoint
Peter M. Lansdorp, MD, PhD*
Terry Fox Laboratory, 601 West 10th Avenue, Vancouver, BC V5Z 1L3, Canada
Telomeres are essential genetic elements that consist of specific DNA repeats and associated proteins. Telomeres cap chromosome ends and prevent chromosome fusion and genetic instability. Telomeric DNA is lost with each round of replication and from other causes, including (failed repair of) oxidative DNA damage. To compensate for this loss, telomeres are elongated by the reverse transcriptase enzyme telomerase. In most hematopoietic cells, telomerase activity is tightly controlled and present in limiting amounts. As a result, telomeres in leukocytes shorten with age, upon transplantation in vivo, and when cultured in vitro. Progressive telomere shortening eventually results not only in telomere dysfunction and apoptosis but also in the promotion of chromosome instability in hematological disorders such as MDS and chronic myeloid leukemia (CML). Here, we review the role of telomeres and telomerase in cells of the hematopoietic system in the context of the emerging concept that telomere shortening represents a tumor-suppressor mechanism in long-lived mammals that limits the growth of most (but not all) stem cells and lymphocytes.
Telomere Structure and Function
Telomeres, or the ends of linear chromosomes, consist in all vertebrates of tandem repeats of TTAGGG/CCCTAA)n and associated proteins.1,2 The length of the repeats varies between chromosomes and between species. In humans, the length of telomere repeats varies from 2-15 kilobase pairs depending on the tissue type, the age of the donor, and the replicative history of the cells. Individual chromosome ends also vary in length, and chromosome 17p typically has the shortest track of telomere repeats.3 Telomeres prevent the ends of linear chromosomes from appearing as DNA breaks and protect chromosome ends from degradation and fusion. Telomeres also play a role in meiosis and the organization of chromosomes within the nucleus.4 Telomeres contain DNA-binding proteins specific for duplex telomeric DNA, which include TRF1 and TRF25 and a protein specific for the single strand overhang that is typically present at the 3′ ends of chromosomes.6 In addition, many other proteins are known to indirectly bind to telomeres (e.g., via TRF1 and TRF2 [reviewed in 2]). The single-strand overhang at the 3′ end of telomeres folds back onto duplex telomeric DNA, forming a protective T-loop.7 The 3′ overhang associates with telomere repeats via TRF2 in a way that is incompletely understood but that appears important for telomere stability.8,9
Telomeres and Replicative Senescence
In contrast to embryonic stem cells or tumor cell lines, hematopoietic stem cells are not immortal. Forty years ago, Hayflick suggested that most normal human cells are unable to divide indefinitely but are programmed for a given number of cell divisions.10 In 1990, several papers described loss of telomeres with replication and with age and suggested that progressive telomere shortening could explain Hayflick’s original observation.11–,13 This model was confirmed by subsequent studies showing that transfer of the telomerase reverse transcriptase gene could prevent telomere erosion and resulted in immortalizing of the cells that Hayflick studied in most detail: normal diploid human fibroblasts.14,15 Since then, many studies have appeared that are compatible with the notion that telomere shortening limits the number of times most normal diploid cells can divide (for review see 16). An emerging consensus is that telomere shortening evolved as a checkpoint mechanism in long-lived mammals that controls unlimited and life-threatening proliferation of organ-specific stem cells and lymphocytes.
Checkpoints and Genome Integrity
DNA is under continuous assault by environmental agents as well as by by-products of normal metabolism such as reactive oxygen species (for review see 17). To ensure that accurate copies of genetic information are copied to the next generation, the cell-cycle machinery is overlaid with a series of surveillance pathways termed “cell-cycle checkpoints.”18 The overall function of these checkpoints is to detect damaged or abnormally structured DNA and to coordinate cell-cycle progression with DNA repair. The term “checkpoint” was originally defined as a “control mechanism enforcing dependency in the cell cycle.”19 However, it has become clear that DNA damage checkpoints control DNA repair and replication processes in addition to imposing cell-cycle delay.20 Cells from different organisms have, furthermore, adopted different strategies to respond to stress and DNA damage. Relative to unicellular organisms, multicellular organisms require not only a higher fidelity of DNA replication and repair but also more diversity in the response to DNA damage. Whereas, for example, the response in yeast can be described as binary between cell cycling and arrest, the response in mammals is more complex and includes outcomes such as apoptosis and senescence. The more complex response in multicellular organisms is enabled by a new regulatory control module, which does not exist in yeast, that involves the tumor suppressor gene p53.20 In addition, it now appears that long-lived mammals, such as humans, have acquired an extra layer of genome integrity surveillance that is not operating in short-lived mammals such as rodents. This additional checkpoint is related to the length and function of telomeres. The term “telomere checkpoint” can be used to describe this tumor suppressor function.
Loss of Telomeric DNA
Telomeric DNA is lost in human cells via several mechanisms that are related to DNA replication, remodeling, and repair. Causes of telomere loss include the “end replication problem,”21,22 nucleolytic processing of 5′ template strands following DNA replication to create a 3′ single strand overhang,23,24 and failed repair of oxidative DNA damage to telomeric DNA.25,26 The relative contribution of these different causes of telomere shortening to the overall decline in telomere length with age is not known and most likely varies between cell types and with age. That telomeres shorten as a result of oxidative damage has only recently been realized. It has been shown that telomeric DNA, with its G-rich repeats, is 5- to 10-fold more vulnerable to oxidative damage than nontelomeric, genomic DNA.27,28 Repair of oxidative damage to nucleotides is typically achieved using nucleotide excision repair pathways, which may involve a DNA polymerase template switch.17 This essential mechanism may fail for lesions near chromosome ends: once the replication fork reaches the end of a chromosome, the physical linkage between template and newly synthesized DNA strands is presumably lost. In general, the contribution of oxidative damage to telomere shortening and the importance of the redox state in cells to prevent such damage remain to be precisely defined.
Telomere Signaling Pathways
The mechanism by which short telomeres signal a DNA damage response is poorly understood.26,29 Recent studies have highlighted the dynamic structure of telomeres (reviewed in 30). It now appears that individual telomeres can be either “on” or “off” in terms of signaling downstream DNA damage pathways. It seems likely that the terminal 3′ end is involved in generating such signals, but details other than that ATM18 and p5331 are likely to be involved are lacking.
Another important question is when telomeres signal during the cell cycle. DNA replication inevitably involves remodeling of the telomere structure. Because telomere loss is known to occur during DNA replication, the inability to form functional telomeres following replication is expected to generate a DNA damage signal during the S or G2 phase of the cell cycle. However, when diploid human fibroblasts reach replicative senescence, they typically enter an irreversible growth arrest in G1. It has furthermore been shown that disruption of TFR2 binding to telomeres generates a DNA damage signal that is independent of DNA replication.8 Perhaps telomeres cycle continuously between “on” and “off” states even when the cells are in G0/G1, with the likelihood of the “on” state inversely and indirectly correlated with the length of telomere repeats (Figure 1 ). According to this idea, the strength of DNA damage signals generated by telomeres would gradually increase with overall telomere shortening. Anti-apoptotic effects of long telomeres or telomerase expression as well as increased levels of p53 (and the increased sensitivity to apoptosis) in “older” cells (with shorter telomeres) agree with this model. Differences between individuals and cells in the telomere length required to activate downstream signaling pathways complicate studies attempting to use telomere length as an absolute predictor of cellular responses.33 No doubt such differences explain, in part, the marked variation in telomere length between similar cells from normal individuals of the same age.34,35
Role of Telomerase and ALT
To compensate for the loss of telomere repeats, cells require expression of functional telomerase. Telomerase is a ribonucleoprotein containing the reverse transcriptase telomerase protein (hTERT) and the telomerase RNA template (hTR) as essential components. In addition, a number of proteins have been described that are important for telomerase assembly, nuclear localization, and stability (reviewed in 2). Telomerase is capable of extending the 3′ ends of telomeres. Telomerase levels are typically high in immortal cells that maintain a constant telomere length, such as the stem cells of the germline in the testis and embryonic stem cells. Interestingly, certain rare stem cells, such as mesenchymal stem cells, also express sufficient telomerase to maintain telomeres at a constant length.36 The resulting unlimited proliferative potential provides considerable therapeutic potential because it allows extensive genetic manipulation and selection of karyotypically normal cells without the restrictions that are typically imposed by a limited replicative life span. For reasons that remain to be precisely defined, telomerase levels are insufficient to maintain the telomere length in hematopoietic stem cells (HSC). Nevertheless, existing telomerase levels in HSC are functionally important, as is highlighted in patients with the disorder dyskeratosis congenita. Patients with the autosomal dominant form of this disease have one normal and one mutated copy of the telomerase RNA template gene. As expected, such patients show a modest reduction in telomerase levels, yet they typically suffer from progressive aplastic anemia, immune deficiencies, or cancer and rarely live past the age of 50.2,37–,39 These findings are in stark contrast to those in the mouse, where complete lack of telomerase activity is tolerated for up to 6 generations.40 Together with the age-related decline in telomere length in leukocytes, these observations have provided strong support for the idea that telomerase levels are extremely tightly regulated and limiting in human hematopoietic stem cells.
The role of so-called alternative (ALT) pathways41 in the elongation and/or maintenance of telomeres in hematopoietic cells is not clear. Most likely, such pathways are not very efficient in elongating telomeres in cells that express telomerase. Because telomere lengthening via telomerase and/or ALT appears to be limiting in hematopoietic cells, molecular defects that result in accelerated telomere shortening may result in aplastic anemia. In many cases, it is not possible or straightforward to distinguish direct from indirect causes of telomere shortening. In dyskeratosis, the cause appears to be directly related to telomerase deficiency; whereas, for example, in Fanconi’s anemia,42 telomere shortening could be caused directly by defective repair of telomeric DNA or indirectly by loss of stem cells (resulting from defective DNA repair) that results in increased (compensatory) proliferation of remaining stem cells.
The Telomere Checkpoint
Following loss of telomere repeats, a DNA damage signal is generated that signals cell-cycle arrest, most likely via upregulation of p53. When short telomeres are subsequently elongated by “telomere repair” pathways involving telomerase and/or recombination, the cell-cycle arrest will be transient. However, the continued loss of telomeric DNA eventually generates too many short telomeres for the limited capacity of telomere repair pathways (Figure 2 ). At this point, otherwise normal cells as well as premalignant cells are destined to die by apoptosis or convert to an unresponsive state (“replicative senescence”) depending on the response to high and sustained levels of p53 in a particular cell type. Possibly, the replicative life span of cells in long-lived species has been under selective pressure to (1) permit sufficient divisions for the maintenance of cellular function during a normal life span while (2) acting as a brake to prevent excessive cellular proliferation and tumor development. It appears that, in most hematopoietic cells, the required balance is achieved by regulating telomerase activity at levels that are sufficient to maintain a minimal length in only a proportion of the 92 telomeres in a human cell. Limiting levels of telomerase and the resulting telomere shortening could contribute to organismal aging in at least two ways. First, some increasing proportion of cells could reach the end of their programmed proliferative life span in old age. As a result, T-cell responses could be compromised in the elderly. Second, gene expression in cells near or at senescence may be abnormal, resulting in aberrant secretion of molecules, including enzymes and cytokines (see also 43). Both factors could contribute to impaired immune responses in older individuals. In general, the study of telomere biology in relation to human aging is in its infancy. Major challenges are difficulties related to longitudinal studies in humans and the unsuitability of rodent models.
Telomere Shortening in Human Nucleated Blood Cells
Since the important original observation that telomeres in adult blood leukocytes are significantly shorter compared with germ-line material (sperm) from the same donor,44 the decline of somatic telomeres has been documented in three ways. The original observation was confirmed,13,45 it was shown that telomeres in various tissues were shorter in older donors,11,12 and telomere shortening was documented during in vitro culture of human cells.12,46 In the decade that followed these initial reports, a large number of papers appeared that greatly refined our understanding of telomere shortening in human nucleated blood cells (reviewed in 47). Studies in this general area have been facilitated by the development of quantitative fluorescence in situ hybridization (FISH) techniques to measure the telomere length in suspension cells using flow cytometry (flow FISH48). With this technique, it was shown that the age-related decline in telomere length in lymphocytes is much more pronounced than in granulocytes and that rapid telomere shortening early in life is followed by a much more gradual decline thereafter.35 The telomere length in granulocytes can be used as a surrogate marker for the telomere length in hematopoietic stem cells if one assumes that the number of cell divisions between stem cells and granulocytes is relatively constant throughout life and that telomere shortening in stem cells is (1) primarily resulting from replication and (2) relatively constant with each cell division. This approach has been used to model the turnover of human hematopoietic stem cells on the basis of telomere length data.49
A striking observation is that telomere length at any given age in humans is very heterogeneous.34,48 This variation appears to be primarily genetic.50 For example, monozygotic twins of over 70 years of age were shown to have very similar telomere length in both granulocytes and lymphocytes, whereas dizygotic twins differed more but still not as much as unrelated individuals.35 Using further refinements in the flow FISH method (Baerlocher and Lansdorp, unpublished observations), it was recently shown that the rapid decline early in life is followed by a slow decline until the age of 50-60 years, after which the decline again accelerates (Figure 3 ). The decline in both granulocytes and lymphocytes is non-linear and fits a cubic curve. The pronounced decline in T-cell telomere length could activate the telomere checkpoint in specific T and natural killer (NK) cells during a normal lifetime and compromise, as a result, immune responses in the elderly.
In view of the modest age-related decline in telomere length in granulocytes, it seems unlikely that hematopoietic stem cells during normal hematopoiesis encounter irreversible cell-cycle arrest or undergo apoptosis as a result of telomere shortening. Most likely, the total production of blood cells from a single hematopoietic stem cell is primarily determined by differentiation of stem and progenitor cells and not replicative senescence. Furthermore, the occasional loss of individual stem cells via telomere shortening is not expected to affect overall hematopoiesis (or overall telomere length in granulocytes) in the presence of an excess of additional hematopoietic stem cells. That normal hematopoietic stem cells and tissues have extensive replicative potential is also in agreement with extensive experience using allogeneic and autologous stem cell transplantation. Nevertheless, the telomere checkpoint does appear to operate in hematopoietic stem cells, as is indicated by the age-related loss of telomeres in granulocytes (Figure 3), the (modest) loss of telomeres that follows allogeneic transplantation,47,51 and the aplastic anemia that follows partial telomerase deficiency.2 Recent studies have shown that the number of hematopoietic stem cells can be altered by manipulating decisions that control self-renewal and differentiation.52 Indeed, the number of mature “end” cells, such as granulocytes, produced by individual stem cells is most likely highly variable and primarily determined by the processes that regulate self-renewal versus differentiation at the level of individual stem cells. Even a limited number of additional self-renewal divisions in a stem cell will greatly increase cell output. As a result, individual stem cells can produce staggering numbers of cells. This is illustrated in clonal proliferative disorders such as paroxysmal nocturnal hemoglobinuria and CML. However, even in CML, clonally expanded Philadelphia-positive stem cells eventually appear to encounter the telomere checkpoint.53 Unfortunately, with a large number of cells to select from, the genetic instability triggered by the loss of functional telomeres appears to favor the selection of a subclone with additional genetic abnormalities and more malignant properties.
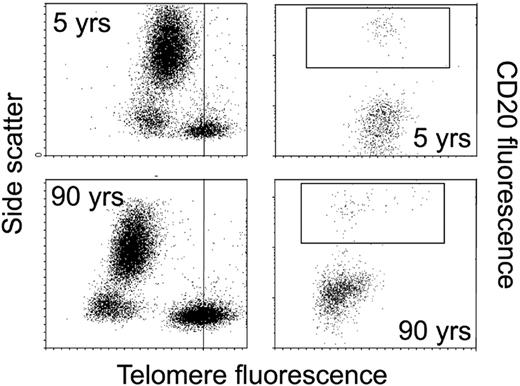
Not all cells in the hematopoietic system are programmed to encounter the telomere checkpoint. B cells appear to be a particularly interesting exception, as the telomere length in B cells is increasingly heterogenous with age (Figure 4 ). Apparently, some B cells express sufficient telomerase (and possibly other factors) to effectively elongate telomeres. Perhaps the many cell divisions required for effective selection and “affinity maturation” of antibody responses favored bypass of the telomere checkpoint. It is tempting to speculate that B cells are, as a result, at a higher risk for tumor development, which could explain the much higher incidence of B- versus T-cell lymphomas in the human population.
Conclusions
Based on observations from several areas, telomeres have emerged as important regulatory elements that control the number of times normal human somatic cells can divide. Activation of the telomere checkpoint results from loss of telomeric DNA with replication and from oxidative damage to telomeric DNA (Figure 2). The DNA damage response that is triggered by activation of the telomere checkpoint can be resolved by telomere elongation pathways that involve telomerase or recombination. However, in most somatic cells, including hematopoietic stem cells, the capacity of such telomere repair pathways appears to be limiting, and telomere shortening effectively limits the proliferative potential of such cells. Most likely, the telomere checkpoint evolved as a tumor suppressor mechanism in long-lived species. The function of the telomere checkpoint may help explain poorly understood aspects of stem cell biology, including stem cell “exhaustion” in aplastic anemia and other proliferative disorders. Cells may bypass the telomere checkpoint by expressing high levels of telomerase or by inactivating downstream signaling events (e.g., by loss of p53 function). Some cells, including subsets of B cells, may avoid the telomere checkpoints altogether, and high levels of telomerase could make such B cells more vulnerable to tumor development. Loss of p53 function also inactivates the telomere checkpoint. This is expected to be a rare event, as both copies of the normal p53 allele in a cell must typically be lost or mutated in order to continue proliferation in the presence of many short and dysfunctional telomeres.3 Loss of p53 function results in chromosome fusions and breakage that drive genetic instability and facilitate malignant progression. This is illustrated in CML, where the onset of blast crisis and additional genetic changes is inversely correlated with the length of telomeres in Philadelphia-positive chronic phase cells.53
II. Embryonic Stem Cells
Martin F. Pera, PhD*
Monash Institute of Reproduction and Development, Monash University, 246 Clayton Road, Clayton, Victoria 3168, Australia
This review discusses the properties and potential applications of human embryonic stem (ES) cells. A stem cell is a primitive cell that can either divide to reproduce itself (undergo self-renewal) or give rise to more specialized (differentiated) cells. Stem cells exist in many adult tissues. With very few exceptions, stem cells in fetal or adult tissue are generally thought to give rise to only a limited range of differentiated cell types. Such limitations on the developmental repertoire of adult stem cells, imposed by powerful molecular constraints on gene expression, are critical to maintenance of tissue integrity during normal cell turnover and tissue repair: these controls ensure that, for example, when the skin is cut, skin cells rather than, say, prostatic epithelium, grow into and repair the wound. By contrast, ES cells are derived from an embryonic cell population at a stage prior to its commitment to form particular tissues of the body. Because of their origin, ES cells are by nature more versatile than most of their adult counterparts.
The derivation of human pluripotent stem cell lines in 19981,2 represented in one sense the culmination of research spanning nearly half a century—research that began with a search for the origin of teratocarcinomas and involved remarkable advances in our understanding of mammalian development and in the treatment of human infertility. Since the development of the human cell lines, there has been extensive public debate about the ethics of using embryos in this research. The outcome of this debate in most countries, including the United States, has been the emergence of a clear consensus that these cells have the potential to revolutionize many of our approaches to the study of human biology and to the treatment of disease. As a consequence, there is now growing public support for stem cell research, and the legal and regulatory framework for the conduct of this research has been laid out in many countries. Despite all this excitement, it is fair to say that the science of pluripotent stem cells is still in its infancy. While stem cells in the mouse were described 20 years ago, for the most part researchers focused on the use of the cell lines as tools to study gene function. Since the cloning of mammals and the derivation of human embryonic stem (ES) cells, there has been a major shift in the focus of research efforts to understand stem cells and the control of their differentiation.
This article reviews the present understanding of mammalian pluripotent stem cells. It discusses work on mouse cells but wherever possible refers to human or primate studies. It begins with a discussion of the concept of pluripotentiality in its embryonic context. It then discusses the derivation of stem cells from embryonic or fetal tissue and discusses their basic properties. The article then examines the ways in which investigators have managed to produce specific types of differentiated cells from stem cells. Finally, it examines the potential applications of stem cells in research and medicine and some of the barriers that must be crossed to achieve those goals.
Embryo and Pluripotential Stem Cells
Fertilization triggers the first cell division of the embryo. At the 2-cell stage in the mouse, and the 4- to 8-cell stages in the human, the embryonic genome undergoes activation. The first cell commitment event in the mammalian embryo occurs with compaction of the embryo and formation of the outer trophoblast layer. The small cluster of cells inside the blastocyst, the inner cell mass (ICM), is destined to give rise to all the tissues of the body. It is at this stage of development when stem cells are isolated.
After compaction and blastocyst formation occur, the cells of the ICM are pluripotent but not totipotent. We can define a totipotent cell as one that can give rise to a new individual if provided with appropriate maternal support. Pluripotent cells can give rise to all tissues of the body plus many of the cells that support the pregnancy but are unable to produce a new individual on their own. Totipotent cells persist only up to the 8-cell stage of mouse development.
The second major differentiation event, formation of the primitive endoderm (precursor cells of the yolk sac) occurs around the time of implantation. The yolk sac, which is like a primitive form of the placenta, plays a role in the uptake and processing of nutrients prior to the establishment of the chorioallantoic placenta. In the past 5 years, it has become apparent that the yolk sac and other extraembryonic tissues, which lie closely apposed to the pluripotent stem cells, play a key role in elaborating molecules that dictate cell fate within the embryo proper.3 Thus, as the embryo implants, signals from these extraembryonic tissues help to drive commitment of cells within the pluripotent tissue, now in the form of a sheet of cells known as the epiblast or primitive ectoderm. These commitment events result in a gradual loss of pluripotentiality within the epiblast. There is one exception to this rule: the germ lineage. Germ cells, which do not undergo commitment to sexual differentiation until midgestation, retain pluripotentiality until that time.
While little is known about the molecular basis of the regulation of pluripotentiality in the embryo, several genes have been identified as essential to the development of pluripotent cells. These include the transcription factor Oct-4,4 the transcription factor FoxD3 (P. Labosky, personal communication), and the novel gene taube nuss.5 Embryos from homozygous mice deficient in any of these genes fail to establish the pluripotent lineage in the embryo. In the case of Oct-4, proper development of the ICM is critically dependent upon the dose of the gene: moderate overexpression results in differentiation into extraembryonic endoderm, while inadequate expression forces differentiation into trophectoderm.6
Derivation and Properties of Embryonic Stem Cells
ES cell derivation
ES cells have been derived in mouse and human in a similar fashion from the ICM of the blastocyst. In the mouse, either whole blastocysts are explanted into culture, or the ICM is isolated and grown on its own. In primates, ES cell lines have been derived from the ICM that have been isolated using immunosurgery. The ICM of the mouse embryo gives rise to all the tissues of the body plus some extraembryonic tissues, including the extraembryonic endoderm, the amnion, and the extraembryonic mesoderm. It is thus clearly pluripotent. Gardner’s laboratory7 showed that it is the epiblast of the expanding blastocyst that actually gives rise to ES cells, and it is widely held that mouse ES cells correspond to the early epiblast of the mouse embryo. However, pluripotent stem cells do not persist long in the peri-implantation mammalian embryo, and it may be that ES cells have undergone certain changes in gene expression to facilitate their immortalized growth in vitro.
To isolate primate ES cells, the ICM is extracted free of trophoblast cells from the embryo using immunosurgery: complement-mediated destruction of the trophoblast cells using an antibody that binds to the latter, leaving the ICM intact. The ICM is then propagated in the presence of embryo fibroblast support to give rise to growing colonies of ES cells. The fibroblast feeder cells used to date have been obtained from midgestation mouse embryos. The mechanism whereby the embryo fibroblast cells support human ES cell growth is not clear but probably involves a combination of secreted factors, membrane-bound factors, and extracellular matrix proteins (below). Recently, many groups have sought to develop alternatives to the use of mouse embryo fibroblasts in ES cell derivation, because it is now apparent that for regulatory purposes cells destined for use in transplantation will be regarded as equivalent to xenografts. The human ES cell colonies are then subcultured, usually as small clumps of cells. Human pluripotent cells are highly sensitive to dissociation and survive poorly as single cells under present growth conditions. Dissection of the colonies under microscopic control reduces them to a size small enough to prevent extensive differentiation of the cells but large enough to ensure stem cell viability.
Key features of pluripotent stem cells
Mouse and human ES cells differ in some respects despite their common origin from pluripotent cells of the blastocyst and the use of similar methods to develop and propagate them (below). Recent studies have shown that many adult stem cells can exhibit a much wider developmental potential than previously anticipated under some circumstances. Therefore, it is important to try to define some general criteria that enable us to assess claims that a cell line is indeed pluripotent. At the same time we must distinguish these fundamental properties from aspects of cell phenotype that might be characteristic of the particular species or developmental stage of origin of the stem cells but not essential aspects of pluripotentiality. What features of the prototype pluripotent stem cell, the mouse ES cell, distinguish it from a wide range of cells that can show developmental plasticity under some circumstances? ES cells are derived directly and at reasonably high frequency from a cell population that is pluripotent under physiological circumstances, the ICM or epiblast. They are stably diploid and karyotypically normal in vitro and can be propagated indefinitely in the primitive embryonic state. ES cells can differentiate spontaneously at high frequency under a range of conditions into multiple cell types representative of all 3 embryonic germ layers, in vitro and in vivo. In the mouse, ES cells can give rise to any cell type in the body, including germ cells, when allowed to colonize a host blastocyst. An important additional criterion for pluripotentiality is the demonstration that the stem cell line may be cloned from a single cell. Cloning the cell line and demonstrating that it can still give rise to the same variety of tissues eliminates the possibility that several distinct committed multipotential cell types are present in the culture and that these together account for the variety of differentiated derivatives produced.
Maintained under the proper conditions, ES cells are immortal cell lines that share many properties of epiblast cells, including the ability to give rise to all tissues of the body. Thus, the essential feature of ES cells is that they can grow indefinitely in the primitive uncommitted state while retaining the ability to give rise to a wide range of body cells. However, it must be remembered that even in the mouse, biological studies of the ability of ES cells to form chimeras suggest that ES cell cultures are heterogeneous. The developmental potential of individual ES cells may in fact be rather variable.
There are some critical differences between mouse and primate ES cells, but they share the key property of pluripotentiality and would appear to have in common patterns of gene expression. In terms of their developmental potential, mouse ES cells do not form trophoblast cells, while primate ES cells do.8 Both cell types are capable of forming extraembryonic endoderm and a wide range of somatic tissues, but in only the mouse has it been possible to demonstrate rigorously that ES cells can give rise to every tissue of the body. By creating aggregation chimeras between mouse ES cells and tetraploid host embryonic cells, researchers have derived mice whose entire somatic tissue consists of ES cells.9 The same experiment proves that mouse ES-derived tissues are functional in the sense that they support a normal living animal. The human ES cell studies to date have reported the formation of an impressive array of cell types in xenografts and in studies in vitro, but many cell types have not yet been observed, and in only a few studies has it been shown that the differentiated cells are indeed functional. These caveats probably reflect limitations on the type of experiments we can do and the early stage of the research, rather than limitations on the developmental capacity of the human ES cells, but we should bear them in mind when discussing the issue of pluripotentiality.
Although there are apparent differences in the phenotype of murine and primate pluripotent cells, it is possible that a universal set of molecular markers might be common to all types of pluripotent stem cells. For example, studies of the transcription factor Oct-4 have clearly established in the mouse that at least this one gene is essential for establishment of the pluripotent lineage, and it seems likely that there are others that are conserved across mammals. While few proteins are expressed in an absolutely cell-specific fashion, it might be expected that some genes found in pluripotent cells would have a rather restricted expression in other cell types. Some common molecular features of primate and mouse pluripotent cells include high molecular weight cell surface polylactosamine glycoconjugates, expression of some form of alkaline phosphatase, expression of the growth factors GDF-3 and Cripto- or Teratocarcinoma-Derived Growth Factor 1, and expression of the transcription factors Oct-4 and FoxD3.10 The biological roles of most of these molecules in the context of ES cell growth remain to be defined, with the exception of Oct-4 (see above). Comparative studies of gene expression and function in pluripotent stem cells from different species should tell us much about the molecular regulation of the pluripotent state.
Species differences in ES cell biology
Mouse and human ES cells also differ in morphology, immunophenotype, and growth properties. While mouse ES cells grow in attached rounded masses in which single cells are difficult to identify, the primate cells grow in flat colonies with distinct cell borders in monolayer culture. A series of surface antigens characterize primate pluripotent stem cells. The stage-specific embryonic antigens (SSEA) 1, 3, and 4 are globoseries glycolipids recognized by monoclonal antibodies originally raised to distinguish early stages of mouse development. Primate pluripotent cells express SSEA-3 and SSEA-4, expressing SSEA-1 only upon differentiation. Essentially the reverse is true of mouse ES cells. Also characteristic of human embryonal carcinoma (EC) cells is the expression of a set of antigens associated with a pericellular matrix proteoglycan found on the cell surface.11– 13 This molecule is also secreted or shed into the culture medium. The TRA1-60 epitope is a sialidase-sensitive epitope associated with this proteoglycan; the antibody GCTM-2 reacts with its core protein, and antibodies TRA1-80 and K21 react with other unknown epitopes on the same molecule. Human ES cells, as well as monkey ES cells, react with TRA1-60, TRA1-80, and GCTM-2. Although GCTM-2 and TRA1-60 do not label mouse ES or EC cells, it is not clear whether the mouse cells lack the surface proteoglycan or whether the antibodies are species specific. In any case, mouse ES cells carry polylactosamine on their surface, and keratan and chondroitin sulphate are both types of polylactosamine. All primate pluripotent stem cells, like mouse EC and ES cells, express alkaline phosphatase activity. In humans, there are four different isozymes of alkaline phosphatase. EC cells express the tissue-nonspecific form and a form of the enzyme that can be detected by antibodies that react with the germ cell or placental form (available immunological reagents do not distinguish between these closely related isoforms). The functional significance of all these surface molecules is as yet unknown.
Growth requirements of pluripotent cells
Like mouse ES and embryonic gonad (EG) cells, primate pluripotent cells, including some human EC cells, require a mouse embryonic fibroblast feeder-cell layer for support. These feeder cells are usually low-passage diploid cells derived through mass culture of eviscerated and decapitated midgestation mouse fetuses. The feeder cells are not well defined in terms of their phenotype, and they are certainly different from classical adult tissue fibroblasts. In the case of mouse ES and EG cells, the feeder cell requirement can be replaced by LIF or related members of this cytokine family, but pluripotent human EC cells, rhesus monkey ES cells, and human ES cells will not respond to LIF in such a fashion.8,14,15 It has recently been demonstrated that the physiological role of LIF in the mouse embryo is to maintain the viability of the ICM during embryonic diapause, a type of suspended animation during which the preimplantation embryo of some mammals may be held in the reproductive tract until the completion of weaning of the previous litter.16 During diapause, the ICM of embryos of homozygote knockout mice lacking LIF degenerate and die. Thus the function of the molecule in the embryo may be to maintain the viability of the pluripotent stem cell population outside of the normal developmental time frame. Since primates do not display diapause, it may be that LIF is irrelevant to the regulation of pluripotent cells in these mammals.
Even on a feeder cell layer, all primate pluripotent cells grow very poorly when dissociated to single cells, whereas mouse ES cell lines can be cloned at a relatively high efficiency in the presence of LIF under these conditions. The precise mechanism whereby these feeder cells support human ES cell growth is unknown. Some workers have found that human ES cells can be grown using a combination of conditioned medium from mouse embryo fibroblasts plus extracellular matrix components,17 but it is not yet clear how widely applicable this methodology will prove to be. In light of the fact that regulatory bodies will probably regard cells derived from ES cells cocultured with animal cells as equivalent to xenotransplants for therapeutic purposes, the elucidation of the mechanism of action of the mouse feeder layers has become even more urgent. It will be important to determine to what extent the feeder cell effects are mediated by specific soluble, membrane-bound, or extracellular matrix proteins, or by nonspecific actions to detoxify components of the culture medium.
One group has described the use of a serum replacement supplemented with bFGF in human ES cell cultures.18 bFGF had no effect in the presence of serum, but in serum-free conditions bFGF was essential for inhibition of differentiation and maintenance of the stem cell population. bFGF produced some improvement in colony formation efficiency, but the rate was still quite low.
Human EG cells
Although this review deals mainly with ES cells derived from blastocysts, one group has also derived pluripotent cell lines from embryonic or fetal human gonads.1 In the mouse the primordial germ cells retain the capacity for pluripotentiality through midgestation, as evidenced by their ability to give rise to teratocarcinomas. Pluripotent cell lines with properties very similar to those of mouse ES cells were derived from primordial germ cells in this species in the early 1990s. The morphology, marker expression, and growth requirements of pluripotent cells derived from the human gonad differ in some ways from those of other primate pluripotent stem cells. As in the mouse, the process of conversion from a primordial germ cell to a cell that can be continuously cultured and that is pluripotent is poorly defined. Shamblott et al noted that only a small fraction of the cells give rise to embryoid bodies containing multiple types of differentiated cells. It may be that the conversion from primordial germ cell to pluripotent stem cell is a type of transdifferentiation process that occurs at lower frequency in human cells compared to mouse cells. Further investigation of the cultures derived from embryonic human gonads is required to determine whether permanent lines of pluripotent stem cells can in fact be derived from them.
Differentiation of Embryonic Stem Cells
Differentiation in vivo
For obvious ethical reasons it will never be possible to demonstrate that human ES cells can colonize all the tissues of a newborn baby following introduction into a host embryo. The developmental potential of human ES cells is, however, easy to demonstrate by inoculating the cells into an immunodeficient animal host.2,15 Under these conditions, ES cells form benign teratomas consisting of an incredible range of differentiated cells. The differentiated cells are often organized histotypically into complex structures such as ganglia. It is important to note that certain phenomena are never observed in teratomas. For example, no axis formation or segmentation into a body plan is ever observed in a teratoma. This marks an important biological difference between embryos and ES cells; the former generate a body plan and the latter cannot. Another important feature of human ES cell-derived teratomas is that they are benign; they contain neither undifferentiated stem cells with the properties of embryonal carcinoma cells nor malignant derivatives of other undifferentiated tissue. In this respect, human ES cells differ from mouse ES cells, since grafts of the latter always contain undifferentiated tissue in combination with differentiated cells in the teratoma.
Differentiation in vitro
Many proposed applications of human ES cells are predicated on the assumption that it will be possible to obtain pure populations of differentiated cells from the ES cultures. It might be envisioned that in order to achieve this one would treat ES cells with inducing agents that would convert them with high efficiency to the cell type of interest. In practice, that has not proven possible in the mouse ES cell system. It is only within the past 5 years or so that investigators have systematically undertaken studies to obtain specific differentiated cells in vitro from mouse ES cells. A range of approaches have been developed to achieve this. The simplest is to rely upon spontaneous differentiation to develop the cell type of interest. Spontaneous differentiation occurs routinely in ES cell cultures and produces a wide variety of cell types, most of which are uncharacterized. The process of spontaneous differentiation may be accelerated under conditions that are suboptimal for stem cell renewal but support cell survival. In the mouse, the most widely used protocol for the induction of differentiation is that of embryoid body (EB) formation.19 There are several variations on this theme, but they all center around cultivating ES cells in suspension in the absence of adhesion or fibroblast feeder cells or LIF. Under these conditions, ES cells form an aggregate body consisting of 2 layers: an outer layer of cells with the properties of extraembryonic endoderm, the first cell layer to form underneath the blastocyst, and an inner cell layer, which represents pluripotent tissue. The EBs are typically replated in monolayer cultures, and a range of differentiated cells grows out of them. It is likely, though unproven, that the endoderm that forms on the outside produces signals that drive the differentiation of the pluripotent cells. The range of cells can be very striking, including beating muscle and nerve.
Many investigators have formed EBs from human ES cells or EG cells to induce differentiation, and a range of cell types may be obtained from them.1,20 It is not clear that an outside layer of extraembryonic endoderm forms in these structures, but there are certainly cells within them that express markers of this tissue type. Other workers found that simply allowing the cells to overgrow in a monolayer culture to high-density results in spontaneous differentiation accompanied by cyst formation, and similarly a wide variety of cells may be obtained from such cultures.
Because these techniques give rise to a mixture of different cell types, investigators have taken a variety of approaches to enhance the yield of particular cell types of interest from these cultures. Cultures can be treated with specific factors or agents that drive differentiation preferentially along a given lineage. Some investigators believe that there is no evidence that a particular factor can alter the outcome of ES cell differentiation in a highly regulated fashion,21 but there are examples of factor treatment that yields a highly biased outcome favoring one specific lineage. Various means for selecting particular cell types have also been described, including selection on the basis of expression of specific surface markers and the use of fluorescence-activated cell sorting or related methodologies. Some workers have employed selective culture conditions that promote the growth of one particular cell type at the expense of another. Genetic modification of the stem cells themselves can be undertaken to insert a selectable marker under the control of a lineage-specific promoter, for example, a transcription factor that is switched on early during lineage-specific differentiation.22 The selectable marker will then be expressed in cells undergoing differentiation into the lineage in question, and by applying the selective agent it is possible to kill off other cell types in the cultures. Note that whatever approach is used, the conditions in vitro must be sufficient to support the survival and hopefully the growth of the progenitor cells and the particular end-cell type.
Many studies have now shown differentiation of human ES cells in vitro. Reubinoff et al15 showed that under conditions that limit stem cell growth but inhibit extraembryonic differentiation, ES cells gave rise to cells expressing markers of diverse differentiated cell lineages. This differentiation was observed in monolayer cultures grown over a period of weeks to high density, which resulted in the formation of multilayered aggregates of cells in situ. Neuronal differentiation occurred with regular frequency under these conditions, and with careful observation it was possible to identify the precursor cells that gave rise to neuronal cells. When these precursors were selected, dissected out, and transferred to a culture medium that supports neural stem cell growth, neurospheres (round floating aggregates containing neural progenitor cells) were obtained that could be serially propagated or induced to differentiate into cells with the properties of mature neurons.
Subsequent studies have shown that these precursors will engraft into newborn mouse brains and undergo regionally appropriate differentiation into all neural lineages.23,24 This result showed that through “natural selection”—selection achieved through the use of culture conditions that favor growth of one cell type over others—pure populations of committed progenitor cells could be obtained. It is not yet clear whether the neural progenitors isolated by these means show properties distinct to neural stem cells isolated from the embryonic, fetal, or adult central nervous system; some studies suggest that ES cell–derived neural progenitors show more developmental plasticity than their fetal or adult counterparts.25
Many groups have used EB formation to induce differentiation of human ES cells. EB formation involves transfer of the human ES cells at high density to bacteriological dishes, to induce aggregation in the absence of substrate adhesion. The aggregates become cystic over the course of several weeks. In the first study of this kind with human ES cells,20 investigators used in situ hybridization and RT-PCR to demonstrate the expression of transcripts for alpha-fetoprotein, gamma globin, 68 kDa neurofilament protein, and cardiac actin. Contracting cardiomyocytes were observed in some EB cultures. The use of the term EB merits some clarification; the structures described in this study did not show a consistent morphology comparable to any stage of human embryonic development. Shamblott et al1 also showed that human EG cells could undergo differentiation into a number of different cell types following EB formation.
In vitro studies of spontaneously differentiating cultures have shown that human ES cells can produce several cell types of clinical significance in addition to neurons. Itskovitz-Eldor and collaborators have shown that the human ES cell line H9 can give rise to insulin-producing cells and cardiomyocytes.26,27 Insulin-producing cells were generated by culture of ES cells in the absence of a feeder layer in monolayer or in EBs. Insulin production in a minority of cells was documented by RT-PCR, immunostaining, and measurement of insulin in the supernatant, but insulin secretion did not respond to changes in glucose levels. RT-PCR indicated that other markers of early pancreatic differentiation were also expressed. In the cardiomyocyte study, a modest proportion of EBs derived from the H9 line gave rise to areas of contracting muscle. The report provided detailed evidence, including marker expression, ultrastructural studies, and electrophysiological and pharmacological data, to support the contention that the contracting cells were indeed early-stage cardiomyocytes.
More recently, endothelial cells have been cultured from EBs. After spontaneous differentiation, cells positive for the surface marker PECAM1 were selected and grown in culture. Approximately 2% of the cells in late embryoid bodies were PECAM1 positive, and most of these expressed other markers of endothelial cells. When they were transplanted into immune-deprived mice, the PECAM1-positive cells formed microvessels.28
Attempts to direct the differentiation of cells within EBs have been limited. The EB technique has been used to study the action of growth factors on human ES cells and their early differentiated progeny. Schuldiner et al29 formed EBs, then disaggregated them and transferred the mixed populations of differentiating cells to monolayer cultures. These monolayer cultures were in turn exposed to a range of growth factors, and the effects on cell differentiation were monitored by RT-PCR for expression of stem cell-specific genes and genes characteristic of specific differentiation lineages. While it appeared that distinct patterns of gene expression were observed following treatment with each growth factor, the results did not indicate whether differentiation was induced or survival and proliferation of specific cell types was favored. Studies relying heavily on RT-PCR often do not prove that marker gene expression was actually associated with specific mature types of cells; it should be borne in mind that differentiation entails more than alterations in the patterns of RNA transcript accumulation in cells.
Kaufman and coworkers30 have shown that cultivation of human ES cells on mouse bone marrow or yolk sac stromal cell lines can induce differentiation of a small proportion of the cells into hematopoietic progenitor cells. The hematopoietic precursors were positive for CD34 and expressed transcription factors characteristic of early blood cell precursors. Colony formation assays in vitro demonstrated that the ES-derived cells could differentiate along erythroid, myeloid, and megakaryocytic lineages. It is possible that the stromal feeder cells induced differentiation of ES cells directly or that they promoted survival of hematopoietic progenitors arising spontaneously from mesodermal progenitors.
Shamblott et al used a similar approach to generate committed progenitor cell lines from EG embryoid bodies.31 A committed progenitor cell is a cell that is no longer pluripotent but not yet overtly differentiated, is capable of considerable division and can give rise to differentiated offspring. The study began with EB formation to induce differentiation; then the differentiated cells were subjected to treatment with a matrix of combinations of 2 different culture media with 3 cell culture substrates. Cell lines that could be serially cultivated were developed; the lines were then classified according to their patterns of gene expression, analyzed using RT-PCR and immunocytochemistry. RT-PCR analysis indicated that these cell lines expressed transcripts for genes characteristic of multiple differentiation lineages, even after cloning, but the most compelling evidence (transcript profile and immunochemistry) for lineage-specific gene expression was obtained for what appeared to be neuronal progenitor cells.
In the mouse there are potentially important differences between ES cells and EG cells, in particular epigenetic differences in genomic imprinting status between EG and ES cell lines.32 It will be interesting to compare the differentiation of the 2 types of cells in more detail.
Applications of Embryonic Stem Cells
Use as research tools
Both mouse and human ES cells represent powerful tools for many basic and applied aspects of cell biology. The use of mouse ES cells in targeted manipulation of the genome has led to a revolution in our understanding of gene function in mammals, unlocking the function of many genes in normal development, normal physiology, and disease pathogenesis. Most applications of mouse ES cell technology have been in the study of gene function in the whole animal. While ES cell knockouts analysis is sometimes highly informative about what the key genes are and what the outcome of their absence is, they do not often yield insight into precisely how the gene product functions in a particular context. It is surprising that more mouse ES cell work has not focused on in vitro differentiation, where the events at the cellular level may be much more amenable to analysis.
It is highly likely that as techniques for making targeted genetic modifications in human ES cells become available, the ES system will become a powerful tool for human functional genomics. The effect of deletions or mutations of specific genes on cell differentiation and function in vitro will be amenable to analysis, and importantly, it will be possible to study gene function in a human cellular context. The ability to create specific disease models in this fashion will also enable drug screening on proximate models of human disease rather than on animal surrogates.
Use in transplantation therapy
The potential application of human ES cells that has attracted the greatest attention is, of course, their use as a source of cells for transplantation therapy. Since ES cell lines are immortal and pluripotent, they provide in principle a renewable source of any type of body cell. There is a wide range of severe debilitating diseases whose underlying pathology involves cell degeneration or death or acute injury, and for which present therapies are unsatisfactory. In some cases it is clear that transplantation will work as a treatment or cure, but an inadequate supply of tissue, often related to a decline in road traffic fatalities, has severely limited this approach.
In the mouse, there is now proof of concept for the use of ES cell–derived tissue to treat models of diabetes,33 Parkinson’s disease,34 myocardial infarction,35 spinal injury,36 and a severe genetic immune disorder.37 Inasmuch as this type of experimentation with mouse ES cells has gotten under way in only the past 5 years, the progress is encouraging. However, there are significant challenges to be overcome before these approaches can be applied in the clinic. The first challenge is to generate sufficient numbers of the desired cell type in a pure form. For most cell types of interest, this is not yet really feasible, though in some areas (neural progenitors) pure populations of precursor cells may routinely be obtained from ES cultures, expanded in numbers, and differentiated into mature cells. A second challenge is to understand what cell type to supply to correct a specific pathology, and how to deliver it. For neurodegenerative diseases, is it better to transplant neural progenitor cells or fully mature neurons? In some cases, simple injection or inoculation of cells will be satisfactory, but in other cases it is likely the graft will need to be incorporated into some form of scaffold in order to function effectively.
A third challenge is that of rejection by the immune system. This is a complex issue, and there are many unknowns. It is unclear how visible embryonic cells or their derivatives will be to the immune system. Some tissues will likely be immunoprivileged, while others will be fully vulnerable to immune surveillance. It is certainly likely that some ES cell–derived tissues will be vulnerable to attack by host immune mechanisms. A number of solutions to this problem have been considered. Some envision that large banks of stem cells will be created, representing a wide array of histocompatibility backgrounds. Other immunologists hold that manipulation of T cell activity will advance in coming years to the point where the whole issue will become much more tractable.38 Other researchers advocate the use of a combined transplant, which will replace the patient’s hematopoeitic and lymphoid systems with ES-derived cells, followed by engraftment of the target cell type.30 In this respect, it is interesting to note that a recent study suggests that embryonic cells can themselves induce a state of immune tolerance in a nonirradiated host.39 A final solution that has attracted a good deal of attention is therapeutic cloning, a procedure that combines cloning by somatic cell nuclear transfer with ES technology to create stem cells that are a custom match to a patient’s own cells. Dramatic proof of concept for therapeutic cloning in the mouse has recently been presented.37 In this study, somatic cell nuclei from immunodeficient Rag2(/) mice were transferred into enucleated eggs, and the resulting cloned blastocysts were used to produce ES cell lines. The genetic defect in the ES cells was corrected using homologous recombination to replace a defective Rag2 allele. Hematopoietic stem cells derived from the ES cells were then injected into Rag2(/) mice, resulting in engraftment of the host myeloid and lymphoid lineages, and restoration of immunoglobulin syntehsis. Practical difficulties with therapeutic cloning include an inadequate supply of eggs and a long turnaround time as well as safety issues related to the well-known occurrence of a wide variety of developmental defects in cloned animals. Discussion of these issues is beyond the scope of this overview, but it is certain that experimentation aimed at understanding the basic mechanisms of cell reprogramming will yield important insights into the molecular specification of the pluripotent state and adult stem cell plasticity.
Conclusions
It is now clear that pluripotent cell lines can be generated readily from human preimplantation embryos, and that a broad range of differentiated cell types can be produced in vitro from human ES cell cultures using a variety of different approaches. The challenge now is to improve our ability to manipulate human ES cultures in vitro, to facilitate basic and applied research into gene function and development of new medicines, and to produce differentiated cells in large numbers and pure form for preclinical studies in disease models prior to clinical trials.
III. Adult Stem Cell Plasticity: Dream or Reality?
Catherine M. Verfaillie, MD*
MMC #716, University of Minnesota, 420 Delaware St., SE, Minneapolis, MN 55455
Stem Cell—Definition
To define a cell as a stem cell, scientists have used four criteria (Figure 5, see Color Figures, 521).1 First, stem cells undergo multiple, sequential self-renewing cell divisions, a prerequisite for sustaining the population. Second, single stem cell-derived daughter cells differentiate into more than one cell type. Examples include hematopoietic stem cells (HSC) that give rise to all hematopoietic cells; neural stem cells (NSC) that give rise to neurons, astrocytes, and oligodendrocytes;2 and mesenchymal stem cells (MSC) that differentiate into fibroblasts, osteoblasts, chondroblasts, and adipocytes.3 Some adult stem cells may give rise to only a single mature cell type, such as the corneal stem cell. A third criterion is that stem cells functionally repopulate the tissue of origin when transplanted in a damaged recipient, which has been shown extensively for HSC and more recently for liver progenitors4 and NSC.5,6 A final, less well established criterion is that stem cells contribute differentiated progeny in vivo even in the absence of tissue damage.
The criteria are all fulfilled when defining ES cells.7,8 ES cells can be expanded in an undifferentiated state indefinitely. ES cells give rise to all cell types when injected into the blastocyst. Generation of viable chimeric animals in which wild-type ES cells compensate for lethal defects present in the host blastocyst9 and creation of viable mice from tetraploid blastocysts10 prove that ES cells functionally differentiate into all tissue cells. This is reviewed in Section II.
Adult Stem Cells
For adult stem cells, these criteria have been most extensively used to characterize HSC. Single HSC can undergo at least asymmetric self-renewing cell divisions, give rise to all blood elements, reconstitute the hematopoietic system when transplanted in lethally irradiated recipients, and engraft and differentiate in animals, even if the recipient is not irradiated (Figure 5, 521).11 In mice, HSC have been purified to near-homogeneity based on cell surface characteristics: HSC express CD45, Thy1.1, cKit, and Sca-1 and do not express lineage antigens (Lin).12 In mice, HSC also do not express significant levels of the CD34 antigen.13 In addition, HSC can be purified based on their ability to exclude Hoechst via the ABC transporter, breast cancer receptor protein (BCRP-1),14 and are therefore present in the side population (Sp) when analyzed by fluorescence-activated cell sorting (FACS).15 In humans, purification of HSC can be obtained using a similar Sp criterion.16 Human HSC do not express lineage antigens but are CD45+. In contrast to mouse HSC, most human HSC are present within the CD34+ cell fraction of bone marrow (BM), blood, or umbilical cord blood; do not express CD38; and express c-kit and Thy1.17–,19 Whether human HSC have been enriched to near-homogeneity, as has been achieved for murine HSC, is not clear, given that characterization of human HSC depends on transplantation in xenogeneic hosts. A minimum of 200-500 cells is still required to achieve human hematopoietic cell progeny in immunodeficient mice or fetal sheep.19 It is not clear whether this is due to the xenotropic nature of the assay system or may reflect the lack of purity of human HSC.
Proof that a single HSC can differentiate in multiple blood cell lineages comes from transplants of single mouse HSC.13 Alternatively, retroviral marking has been used. As retroviruses integrate randomly into the host cell DNA, the DNA sequence flanking the viral integrant is cell specific and can be used to follow progeny of individual cells in vitro or in vivo. This approach has been used to demonstrate in both mice20 and humans21 that single HSC can give rise to multiple progeny cells. In addition, this approach has allowed for the demonstration that single HSC undergo self-renewing cell divisions and that multiple daughter cells have multilineage differentiation potential.20
More recently, these criteria have also been applied to identify other adult stem cells. As an example, NSC can be purified from human brain using a combination of antibodies against CD133 and CD24.6 CD133+CD24− cells generate neural spheres that can be subcultured and can give rise to astrocytes, oligodendrocytes, and neurons in vitro as well as in vivo. As has been done for HSC, retroviral marking studies have allowed investigators to demonstrate that single NSC can give rise to multiple daughter cells, each of which has the ability to differentiate into astrocytes, oligodendrocytes, and neurons.22
In contrast to ES cells, adult stem cells have less self-renewal ability, in part because of lack of high levels of telomerase (see Section I). In addition, the array of differentiated cells that can be generated from adult stem cells is more limited, and adult stem cells generate daughter cells that can differentiate into cells of the tissue of origin but not other cell types.
Adult Stem Cells—Plasticity
Over the past 5 years, a series of reports has been published suggesting that the previous dogma of tissue specificity associated with adult stem cells may not be correct. The presumed ability of tissue-specific stem cells to acquire the fate of cell types different from the tissue of origin has been termed adult stem cell plasticity (Figure 6, see Color Figures, 521). These reports have generated considerable excitement in the scientific community. However, these studies have also met with significant skepticism, in part because (1) most studies still await independent confirmation, (2) because of the low frequency with which the apparent lineage switch occurs, (3) because most studies fall short in proving that the plasticity is the result of a single stem cell that differentiates into more than one functionally characterized lineages, and (4) probably most of all because such lineage-switch defies established developmental biology and stem cell principles.
Most studies have shown “plasticity” using cells derived from bone marrow (BM), which contains—aside from HSC—MSC and endothelial progenitor cells. Following transplantation of BM in lethally irradiated recipients, several reports have shown that donor-derived cells of mesodermal lineage other than the hematopoietic lineage can be detected, even though the level of contribution was usually less than a few percent. In some studies, BM cells were enriched for HSC using either cell surface markers23 or functional characteristics such as the Sp phenotype.24,25 Tissues where such contribution has been seen include skeletal muscle,24,26 endothelium,25,27,28 and cardiac muscle.23,25,29 At first sight, even more surprising are studies suggesting that BM cells differentiate into cells of tissues of a different germ layer. Several studies have been published suggesting that cells from BM may differentiate in vitro or in vivo into cells with neuroectodermal morphology and phenotype.30–,34 Differentiation of mesodermal cells into cells with endodermal morphology and phenotype has also been shown. Petersen et al were the first to show that oval cells in the regenerating liver may be derived from BM.35 Similar findings have since been reported by a number of groups,36–,39 and donor BM-derived cells in other epithelial tissues, such as skin and lung, have also been detected.38 Taken as a whole, these studies suggest that stem cells with multipotent nature—akin to ES cells—are present in BM and perhaps in other tissues such as brain and muscle.
Plasticity—Possible Mechanisms
Several mechanisms may underlie this apparent plasticity (Figure 7, see Color Figures, 521): (1) multiple tissue-specific stem cells are present in different organs, (2) plasticity is the result of fusion of the donor cell with resident cells in an organ, (3) cells undergo de- and re-differentiation, or (4) true multi- or pluripotent stem cells persist in postnatal life. Data exist that would support all four models.
Multiple tissue-specific stem cells are present in different organs
It has been well established that HSC exit the BM space, circulate in the peripheral blood, and “home” in different organs, a concept used clinically in peripheral blood transplantations.40 Therefore, HSC could be found in other tissues. This appears to be the case for muscle, as two studies have now shown that the perceived repopulation of the hematopoietic system following transplantation of muscle cells into lethally irradiated mice is the result of HSC that reside within muscle.41,42 Another example is that BM contains cells with characteristics of oval cells, the progenitor for hepatic and biliary epithelial cells.43 Thus, contribution of BM-derived cells to liver regeneration could be the result of infusion of hepatic oval cells present in the BM sample.
Plasticity is the result of fusion of the donor cell with resident cells in an organ
The concept that cellular fusion can change the fate of a cell is not new. Heterokaryon studies were performed since early in the 20th century, and a number of studies have shown that cell fate can be changed upon heterokaryon formation.44 For instance, myoblast fusion with fibroblasts induces expression of muscle proteins in the fibroblasts. This indicates that cytoplasm of myoblasts contains factors that induce muscle differentiation of non-muscle cells. Two recent studies documented that coculture of adult tissue cells with ES cells also leads to cell fusion. Indeed, coculture of murine BM cells with ES cells,45 or murine fetal or adult NSC with ES cells,46 yielded what appeared initially to be “transdifferentiated” BM cells or NSC that had acquired ES characteristics. Although several in vitro studies have shown that lineage switch is possible without co-culture of adult stem cells with ES cells or other cell types and that cells with novel lineage characteristics are not tetraploid,27,47,48 no study to date has formally excluded the possibility of cell fusion for in vivo plasticity phenomena. However, the apparent switch in the studies by Terada et al45 and Ying et al46 was rare (fusion between adult cells and ES cell occurred in 1/105-1/106 cells), required considerable selectable pressure to select for the fused cell, and this was only shown in vitro. Nevertheless, it remains possible that this mechanism underlies “plasticity” occurring in the setting of extensive selectable pressure such as acute organ failure and tissue death, in tissues that “tolerate” tetraploidy, such as muscle, hepatocytes, Purkinje cells and others. Finally, fusion may underlie “plasticity” in circumstances where the frequency of trans-differentiation is extremely low.
Cells undergo dedifferentiation and redifferentiation
In the era of “Dolly” it has become clear that the genetic information of a cell can be reprogrammed and that somatic cells can dedifferentiate into pluripotent cells.49 It has long been known that dedifferentiation and redifferentiation occur in amphibians such as Urodeles, which can regenerate whole limbs. A number of studies have suggested that similar although less dramatic processes may cause dedifferentiation of somatic cells. For instance, when oligodendrocyte progenitors from the optical nerve were maintained in serum-free, low-density culture conditions, they acquired NSC characteristics.50 Yet other studies have suggested that cells committed to pancreatic epithelium can be switched to a hepatic phenotype, even though the functional properties of the hepatocyte lineage cells were not defined.51
These findings suggest that dedifferentiation and redifferentiation might be a third explanation for adult stem cell plasticity. Then, adult stem or progenitor cells would be reprogrammed when removed from their usual microenvironment and introduced into a different niche that imparts signals to activate a novel genetic program needed for the new cell fate.52 Insights in the molecular mechanisms underlying nuclear reprogramming during the cloning process may therefore help us to better understand the phenomenon of adult stem cell plasticity and may be exploited in the future to induce lineage switch even without nuclear transplantation. Likewise, insights in the molecular mechanisms underlying de- and re-differentiation phenomena in amphibians and fish that allow regeneration of a limb might aid in understanding adult stem cell plasticity. For instance, Msx1 is expressed in the regenerating blastema. A recent study demonstrated that overexpression of this homeobox gene in myotubes derived from the C2C12 cell line causes regression of the myotubes into multiple mononuclear myoblasts, which then proliferate and gain the ability to differentiate into osteoblasts, chondrocytes, and adipocytes.53 Whether pathways that have been identified in fish and amphibians to cause de- and re-differentiation, play a role in higher mammalian stem cell plasticity will need to be defined.
True multi- or pluripotent stem cells persist in postnatal life
Finally, there is evidence supporting the notion that precursors for defined somatic stem cells may persist beyond the earliest steps of embryogenesis. For instance, Suzuki et al isolated cells from mouse fetal liver that can be expanded in vitro at the clonal level and can reconstitute not only liver and biliary epithelial cells but also epithelium of pancreas and the gastrointestinal tract.54 This study suggests that cells that precede the known somatic stem cells may persist beyond early embryological development and, depending on the milieu, differentiate to cells different than the organ of origin. Jiang et al demonstrated that cells known as multipotent adult progenitor cells (MAPC), copurifying with MSC from BM, can, at the single-cell level, differentiate in vitro into cells with characteristics of mesodermal lineages, neuroectodermal lineages, and endodermal lineages.48 MAPC can also contribute to most, if not all, cells when injected into the blastocyst.
As is discussed extensively in Section II, pluripotent ES cells are characterized at the molecular level by a number of transcription factors highly specific for these undifferentiated cells, including oct-455,56 and Rex-1.57,58 Oct-4 is a transcription factor expressed in the pregastrulation embryo, early cleavage stage embryo, cells of the inner cell mass of the blastocyst, and in embryonic carcinoma cells,56,59 and is downregulated when cells are induced to differentiate in vitro.60 Oct-4 is required for maintaining the undifferentiated phenotype of ES cells and plays a major role in determining early steps in embryogenesis and differentiation.55,61 In the adult animal, oct-4 is only found in germ cells. Rex-1 cooperates with oct-4 for maintaining ES cells undifferentiated.57,58 Except for MAPC, which express oct-4 and Rex-1—albeit at significantly lower levels than what is seen in ES cells—no adult cell has been identified that is characterized by these criteria. As it not yet known whether MAPC exist as such in vivo or are the result of dedifferentiation of an MSC-like cell into a cell with greater potential, there is currently no definitive proof that true pluripotent stem cells exist in vivo during post-natal life.
Stem Cell Plasticity—Definition?
There is no “official” definition of stem cell plasticity. One possible definition is that tissue-specific adult stem cells—for instance, HSC—thought to be committed to a given cell lineage can under certain microenvironmental conditions acquire the ability to differentiate into cells of a different tissue. This definition implies that (1) different cell lineages are derived from a single initial cell, (2) all differentiated cell types are functional in vitro and in vivo, and (3) engraftment is robust and persistent in the presence (and absence) of tissue damage. These criteria can be used to evaluate the studies describing stem cell plasticity.
The majority of studies have been performed in rodent models, and a smaller number of studies have addressed the notion of stem cell plasticity in humans. Most studies were based on in vivo transplantation of sex-mismatched cells, enhanced green fluorescent protein, or β-galactosidase marked cells, and detection of donor cells was based on presence of the Y-chromosome or the marker gene. Several reviews have addressed potential pitfalls associated with the detection of donor cells using either marking system.62,63
Different cell lineages are derived from a single initial cell
The majority of studies describing BM cell plasticity have used non-purified BM populations as graft or BM enriched for a HSC phenotype. However, even when enriched HSC were used, multiple cells were grafted. It is therefore possible that engraftment outside the hematopoietic system is due to coexistence of multiple stem cells within the BM. As alluded to above, BM may contain oval cells.43 The cell responsible for hematopoietic reconstitution—for instance, liver reconstitution—may thus be different. Likewise, muscle contains HSC. Therefore hematopoietic engraftment from transplantation of muscle derived cells may be the result of contaminating HSC.41,42 Even though such tissue regeneration may be of clinical benefit, such a phenomenon could not be termed “plasticity.”
However, a number of studies have shown that single cells may differentiate into cells of multiple different tissues. Using retroviral marking, several studies have shown that single, BM-derived MAPC differentiate into multiple mesodermal,64 neuroectodermal,48 and endodermal lineage47,48 cells in vitro. In vivo studies by Krause et al,38 Grant et al,28 Bjornson et al,65 Clarke et al,66 and Jiang et al48 have also shown that single cells or cells obtained from single-cell sub-cloning experiments differentiate beyond cells of the organ of origin. Krause et al38 showed that single “homed” HSC did not only give rise to progeny that restores the hematopoietic system but could also be found at low frequency in epithelia of liver, gut, lung, and skin, where they acquired morphologic and phenotypic, but not functional, characteristics of these epithelial tissues. Using a similar approach, Grant et al28 showed that single HSC transplanted in lethally irradiated murine recipients give rise not only to hematopoietic cells but also to endothelial cells of retinal blood vessels that had been previously damaged. In contrast to the study by Krause et al, the study by Grant et al also proved functional differentiation, as blood flow was restored in the damaged retina. Bjornson et al65 sub-cloned NSC and found contribution of progeny of presumed single NSC to the hematopoietic system. It should be noted that a similar study conducted more recently could not confirm these results.67 Clarke et al used sub-cloned NSC and found contribution of progeny of presumed single NSC to multiple tissues when introduced in the blastocyst.66 However, none of the offspring was born, making assessment of functional differentiation difficult. Likewise, Jiang et al48 showed that 30% of single BM-derived MAPC, introduced in the blastocyst, gave rise to viable, balanced chimeric offspring. As is discussed below, additional studies will be needed to prove that MAPC-derived progeny gave rise to functional tissue specific cells in this setting.
All differentiated cell types are functional in vitro and in vivo
The second criterion is that differentiated cells have, aside from morphological and phenotypic features of the differentiated cell type of the new tissue, functional characteristics of that lineage. In other words, transplantation of stem cells results in functional repopulation in tissues other than the tissue of origin. However, most studies have defined plasticity based on the acquisition of morphologic and phenotypic characteristics of the non-hematopoietic tissue. Because the degree of engraftment in non-hematopoietic tissues was low (usually less than 1%), acquisition of phenotypic characteristics alone, such as expression of dystrophin in skeletal muscle of muscular dystrophy mice,24 presence of albumin and cytokeratin in liver cells,36,37 and so on, without assessment of the function of the individual grafted cells, can not be used to prove functionality. The study by Lagasse et al39 is one of the notable exceptions. In this study, the investigators demonstrated functional replacement of hepatocytes following transplantation of non-purified murine BM or enriched HSC in an animal model of hereditary tyrosinemia, caused by deletion of the fumarylacetoacetate hydrolase (FAH) gene.68 This mutation is lethal, although animalslike humanscan be kept alive by administration of 2-(2-nitro-4-fluoromethylbenzoyl)-1,3-cyclohexanedione (NTBC), which inhibits 4-hydroxyphenylpyruvate dioxygenase, upstream of FAH.69 The only curative therapy is replacement of hepatocytes by normal, wild-type hepatocytes.68 Lagasse et al showed that animals transplanted with wild-type BM or wild-type BM enriched for HSC could be weaned of NTBC, and that donor BM and HSC differentiated into cells with phenotypic characteristics of hepatocytes that must be functional, as they rescued the otherwise lethal phenotype.39 Reyes et al showed that undifferentiated MAPC or endothelial differentiated progeny from MAPC contribute to neoangiogenesis in tumors or wound healing.27 Likewise, Grant et al showed that progeny of single HSC gave rise to functional endothelium in animals in which retinal vasculature had been damaged.28 Orlic et al showed improved cardiac function and presence of cells with markers of cardiomyocytes.23 However, the study did not prove that the cells with cardiomyocyte markers were functioning cardiac muscle cells, as no evidence was provided that donor cells with cardiac myoblast features were electrically coupled to the host cardiac myoblasts. Finally, animals generated by injection of MAPC into the blastocyst in the study by Jiang et al showed levels of chimerism up to 45%.48 As these animals appeared normal, one might conclude that MAPC gave rise to functional progeny. However, as the host blastocysts were from wild-type mice, presence of up to 45% MAPC-derived progeny in most if not all organs does not fully prove that progeny of MAPC introduced in the blastocyst functionally replaces tissues in vivo, and injection of MAPC in blastocysts of mice with a gene defect or generation of tetraploid-complementation chimeric animals would be needed to fully prove functional differentiation in vivo.
In addition, several in vitro studies have demonstrated that cells that apparently switch lineage acquire not only phenotypic but also functional characteristics of the new cell type. For instance, BM-derived MAPC differentiate into cells with not only morphologic and phenotypic characteristics of hepatocytes, but also functional characteristics of liver cells such as secretion of albumin and urea, and phenobarbital-inducible cytochrome p450.47
Engraftment is robust and persistent in the presence (and absence) of tissue damage
A characteristic of HSC is the robustness of hematopoietic recovery seen in the presence, or even absence, of tissue damage. Although transplantation of BM or HSC resulted in robust hematopoietic engraftment, less than 1% engraftment has been seen in skeletal muscle or epithelial tissues in most plasticity studies. Exceptions are the Lagasse study, where robust engraftment was seen when BM or enriched HSC were transplanted in animals with hereditary tyrosinemia-1.39 Robust engraftment in the liver was seen only when NTCB was withheld, leading to acute necrosis of the diseased liver. In the study by Jiang et al, MAPC gave rise to 2-4% hematopoietic cells in unirradiated recipients, which increased to between 5% and 10% when animals underwent minimal irradiation.48
Potential Uses of Adult Stem Cells
Basic stem cell biology
Adult stem cells represent powerful tools to study self-renewal and differentiation. Even in the era before stem cell plasticity, investigators used stem cells and their defined intermediate, committed progeny cells to evaluate growth factor and other extracellular signals required for their development. With the advent of the completion of the human and, more recently, mouse genome projects, stem cells and their differentiated progeny can be used to define genetic programs that need to be activated or inactivated for cell differentiation to occur.70
Because some of the stem cell plasticity may be caused by de- and re-differentiation processes, studies aimed at understanding the genetic mechanisms underlying these processes will be invaluable. Indeed, a better understanding of the factors that govern this process should ultimately lead to improved methods to induce de- and re-differentiation, which may make this phenomenon clinically relevant. As some of the plasticity recently identified in adult stem cell populations may reflect persistence of more primitive stem cells even in adult life, comparative analysis of the expressed gene profile, protein profile, and growth factor or other extracellular signal requirements of tissue-committed stem cells (such as HSC or NSC), more primitive adult stem cells (such as perhaps MAPC), and the quintessential pluripotent stem cell (the ES cell) should yield invaluable information regarding factors important for the pluripotent versus multipotent nature of stem cells.
Use of adult stem cells for therapy of genetic or degenerative diseases
HSC have been used for several decades to treat hematopoietic disorders or to rescue patients with other malignancies undergoing intensive chemotherapy or radiation therapy. It is conceivable that with progress made in characterizing stem cell populations for other tissues—such as NSC, keratinocyte stem cells, and corneal stem cells—stem cell therapy may become a mainstay for treatment of inherited or acquired defects in these tissues. Indeed, there is already proof in mouse models that NSC can be used to treat Parkinson’s disease.71
If studies indicating that adult stem cells may have greater differentiation potential can be confirmed and extended, adult stem cells, like their embryonic counterparts, may be used to treat degenerative or genetic disorders of many more organs. However, studies to convincingly prove this thesis will be required. In addition, a large amount of work lays ahead to determine how such cells would be used. Provided that signals in vivo are sufficient to induce organ- and lineage-specific differentiation at levels sufficient to repair the target organ, adult stem cells could be used without prior differentiation in vitro to lineage-specific cells, given that there is so far no evidence that undifferentiated adult stem cells will cause tumor formation. As we know very little regarding “homing” of adult stem cells to non-hematopoietic microenvironments, it will be necessary to determine whether undifferentiated adult stem cells that are capable of lineage switch should be infused intravenously versus locally to obtain levels of engraftment sufficiently high to replace a damaged non-hematopoietic tissue. In addition, as it is possible that local cues are not sufficiently strong to mediate efficiently lineage switch, it will be necessary to test whether stem cells should be predifferentiated in vitro prior to infusion to obtain optimal tissue repair and, if so, whether tissue-committed progenitor cells or fully mature cells should be used. In contrast to ES cells, adult stem cells could be used as autologous grafts. However, for acute illnesses such as myocardial infarctions or immune-based diseases such as diabetes, allogeneic therapy will still be needed, unless a sufficiently large number of stem cells can be collected from the patient. Then, as is true for ES cell–based therapy, strategies will need to be developed to overcome immune rejection (see Section II).
Conclusions
Adult stem cells, such as HSC, are used clinically for transplantation. In addition, identification of stem cells for other tissues such as liver and the central nervous system may lead to stem cell–based therapies for diseases that affect the host organ. Because of the mounting evidence that adult stem cells may have greater differentiation potential than previously known, it is possible that adult stem cells from one tissue may at some time be used to treat genetic or degenerative disorders of tissues other than the tissue of origin. If these observations can be further confirmed, adult stem cells, like their embryonic counterparts, may be useful for drug discovery and drug toxicity screening. More important, multipotent or even pluripotent adult stem cells might then be used for therapies of degenerative or genetic disorders of multiple different organs. However, whether multi- or pluripotent adult stem cells will have the same longevity and in vivo functional differentiation potential as ES cells still needs to be proven in studies in which both cell sources are compared side by side.
Dynamic model of DNA damage signals generated by short telomeres.
Following replication and processing, a chromosome end with a G-rich single-strand overhang is created (A). This structure is processed and bound by various telomere binding proteins, including hPOT16 (indicated by the small clear circle), which binds to the 3′ single-strand overhang, and TRF1 and TRF2 (indicated by light and dark gray circles), which are capable of folding telomeric DNA.32 If the length of telomere repeats is sufficiently long (L), double-stranded telomere repeats can easily fold back onto the single-strand overhang, resulting in a relatively stable structure.7 The stability of the poorly understood fold-back structure could be compromised when telomeres are short (S), resulting in a shift of the equilibrium between capped and uncapped telomeres4 that is independent of DNA replication.
Dynamic model of DNA damage signals generated by short telomeres.
Following replication and processing, a chromosome end with a G-rich single-strand overhang is created (A). This structure is processed and bound by various telomere binding proteins, including hPOT16 (indicated by the small clear circle), which binds to the 3′ single-strand overhang, and TRF1 and TRF2 (indicated by light and dark gray circles), which are capable of folding telomeric DNA.32 If the length of telomere repeats is sufficiently long (L), double-stranded telomere repeats can easily fold back onto the single-strand overhang, resulting in a relatively stable structure.7 The stability of the poorly understood fold-back structure could be compromised when telomeres are short (S), resulting in a shift of the equilibrium between capped and uncapped telomeres4 that is independent of DNA replication.
The telomere checkpoint.
Loss of telomere repeats following replication and oxidative damage results in activation of a DNA damage signal that triggers DNA repair reactions involving telomerase and/or molecules involved in recombination such as BRCA1, WRN, and BLM. Following effective repair, cells can go through another round of cell division. However, eventually too many short telomeres accumulate for the limited telomere repair capacity. The resulting high levels of p53 will trigger apoptosis or replicative senescence. Because telomerase levels are limiting in hematopoietic stem cells, such a threshold will be reached earlier in cells that express subnormal levels of telomerase, as in dyskeratosis congenita.
The telomere checkpoint.
Loss of telomere repeats following replication and oxidative damage results in activation of a DNA damage signal that triggers DNA repair reactions involving telomerase and/or molecules involved in recombination such as BRCA1, WRN, and BLM. Following effective repair, cells can go through another round of cell division. However, eventually too many short telomeres accumulate for the limited telomere repair capacity. The resulting high levels of p53 will trigger apoptosis or replicative senescence. Because telomerase levels are limiting in hematopoietic stem cells, such a threshold will be reached earlier in cells that express subnormal levels of telomerase, as in dyskeratosis congenita.
The decline in telomere length with age is more pronounced in lymphocytes than in granulocytes.
Shown is the mean telomere length for both cell types extracted from several hundred measurements over the entire age range (Baerlocher and Lansdorp, unpublished). Not shown is the considerable variation in telomere length values between individuals at any given age.35 The gray bar at the bottom represents nontelomeric DNA contributing to the telomere length measurements (flow fluorescence in situ hybridization [FISH] measurements were calibrated using Southern blot analysis in which on average 2-4 kb of subtelomeric DNA between restriction sites and start of telomere repeats is included in the measurement). Both granulocytes and lymphocytes show a highly significant decline in telomere length with age, which is best described by a cubic function.
The decline in telomere length with age is more pronounced in lymphocytes than in granulocytes.
Shown is the mean telomere length for both cell types extracted from several hundred measurements over the entire age range (Baerlocher and Lansdorp, unpublished). Not shown is the considerable variation in telomere length values between individuals at any given age.35 The gray bar at the bottom represents nontelomeric DNA contributing to the telomere length measurements (flow fluorescence in situ hybridization [FISH] measurements were calibrated using Southern blot analysis in which on average 2-4 kb of subtelomeric DNA between restriction sites and start of telomere repeats is included in the measurement). Both granulocytes and lymphocytes show a highly significant decline in telomere length with age, which is best described by a cubic function.
Lansdorp Figure 4 (in Verfaillie et al). Telomere length analysis in subpopulation of human nucleated blood cells using flow fluorescence in situ hybridization (FISH; Baerlocher and Lansdorp, unpublished).
For this type of analysis, nucleated blood cells following red cell lysis are hybridized with fluorescently labeled telomere probe together with fixed cow thymocytes (with long telomeres: vertical bars, left panels) as internal controls. Following wash steps to remove unlabeled probe and incubation with labeled antibodies (e.g., phycoerythrin-labeled anti-CD20, right panels) the cells are analyzed by flow cytometry. Note the decline in telomere fluorescence (on a linear scale) with age in both granulocytes (with high side scatter, left panels) and lymphocytes (low side scatter, increased heterogeneity with age, left panels) and the presence of some CD20+ B cells with very long telomeres in the 90-year-old normal donor.
Lansdorp Figure 4 (in Verfaillie et al). Telomere length analysis in subpopulation of human nucleated blood cells using flow fluorescence in situ hybridization (FISH; Baerlocher and Lansdorp, unpublished).
For this type of analysis, nucleated blood cells following red cell lysis are hybridized with fluorescently labeled telomere probe together with fixed cow thymocytes (with long telomeres: vertical bars, left panels) as internal controls. Following wash steps to remove unlabeled probe and incubation with labeled antibodies (e.g., phycoerythrin-labeled anti-CD20, right panels) the cells are analyzed by flow cytometry. Note the decline in telomere fluorescence (on a linear scale) with age in both granulocytes (with high side scatter, left panels) and lymphocytes (low side scatter, increased heterogeneity with age, left panels) and the presence of some CD20+ B cells with very long telomeres in the 90-year-old normal donor.

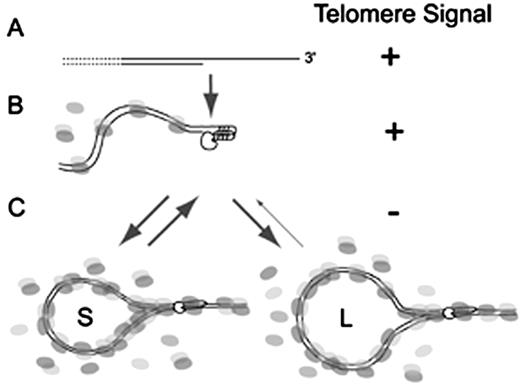
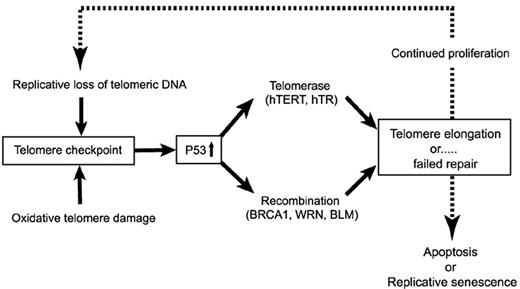
![Figure 3. The decline in telomere length with age is more pronounced in lymphocytes than in granulocytes. / Shown is the mean telomere length for both cell types extracted from several hundred measurements over the entire age range (Baerlocher and Lansdorp, unpublished). Not shown is the considerable variation in telomere length values between individuals at any given age.35 The gray bar at the bottom represents nontelomeric DNA contributing to the telomere length measurements (flow fluorescence in situ hybridization [FISH] measurements were calibrated using Southern blot analysis in which on average 2-4 kb of subtelomeric DNA between restriction sites and start of telomere repeats is included in the measurement). Both granulocytes and lymphocytes show a highly significant decline in telomere length with age, which is best described by a cubic function.](https://ash.silverchair-cdn.com/ash/content_public/journal/hematology/2002/1/10.1182_asheducation-2002.1.369/3/m_verfaillie_fig3.jpeg?Expires=1767730659&Signature=BPlSqEQ3XAyNQZ-qJpq70Z0wbEgjL7-WldbilWKD43hgVIBcpTF1nKETYJcZ21DDmCOkavd391~HlkhgDf4fbont9oynQTWXaMey1IHozQml--mQLO1UD5bu6iLsVGY1DnISa3PQYMGkMc1kOWOp1lAa2K9SmrRREZJDc2JaKBLH2KjQxk24xAPiokYwYGn5CvqMCRNZCHcR-G7ZAOpWHqtlkigyDkcPD1pgqAA-bMxqHI9QZX8-QP3Nder2Wf2qzsdYd1wbaWiCACBXYjNE61WdlyNRN8OQFFvS5zoZrkkBarTj8SGpm86~29W68k95l3hm7lKqcQMMmnFYM7~ApA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)