Abstract
Anti-CD20 therapy has had a truly dramatic impact on treatment and outcome of patients with follicular lymphoma. Unfortunately, the majority of responses to single-agent rituximab are incomplete, and all patients with follicular lymphoma will experience disease progression at some point following rituximab therapy. Rituximab has multiple mechanisms of inducing in vivo cytotoxicity, including antibody-dependent cell-mediated cytotoxicity, complement-dependent cytotoxicity, direct apoptotic signaling, and possible vaccinal effects. The cellular microenvironment within follicular lymphoma has a profound impact on which mechanism is dominant, and confers resistance in many situations. Both tumor-associated and host-associated factors also contribute to rituximab resistance. There are multiple potential approaches to overcoming rituximab resistance, including rational biologic combination immunotherapy, engineered antibodies, and radioimmunoconjugates. Improved ability to overcome resistance will require further elucidation of critical signaling pathways involved in rituximab induced cytotoxicity and a comprehensive understanding of interactions between its multiple mechanisms of action.
Enthusiasm for the use of monoclonal antibodies as directed therapy for lymphoma began in 1979, when a single patient was treated with a murine monoclonal antibody for relapsed non-Hodgkin lymphoma (NHL).1 CD20, a B-cell-restricted cell surface antigen without clear function or ligand, is on virtually all B-cell NHLs, including follicular lymphoma. It is generally believed that CD20 may have kinase activity and function as a calcium channel. CD20 is an “ideal” antigen for such targeted therapy, since it is not shed or internalized and does not circulate in the plasma as free protein. Various monoclonal antibodies have been raised against CD20, which exert differential effects on binding, and may have significant differential mechanisms of cytotoxicity. Rituximab (Rituxan®; BiogenIDEC, Cambridge MA, and Genentech Inc., South San Francisco, CA) is a chimeric anti-CD20 monoclonal antibody with murine variable regions and human IgG and kappa constant regions. Rituximab compares favorably to single-agent chemotherapy, with a significantly better toxicity profile, particularly for patients with follicular lymphoma. Indeed, rituximab has had a truly dramatic impact on treatment and outcome of patients with follicular lymphoma. However, the majority of responses to rituximab are incomplete, and approximately 50% of patients may not respond to initial treatment with rituximab. All patients with follicular lymphoma will experience disease progression at some point following rituximab therapy. Improving on this therapy requires a thorough understanding of multiple mechanisms involved in rituximab-induced cytotoxicity, and resistance.
Mechanisms of Rituximab Cytotoxicity
The mechanism of cytotoxicity induced by anti-CD20 therapy in humans is not completely understood and probably includes several mechanisms.2 The dominant mechanism may change depending upon cellular compartment (node vs blood), histology, and specific antibody utilized.
Antibody-mediated cellular cytotoxicity
Antibody-mediated cellular cytotoxicity (ADCC), mediated through ligation of the Fc portion of the monoclonal antibody to Fc receptors (FcR) expressed by accessory cells, appears to be a major in vivo mechanism of rituximab.3 In studies of normal and malignant human B cells in vitro, B-cell depletion was observed with rituximab therapy in the presence of mononuclear cells, but not in the presence of complement,4 suggesting the importance of cell-mediated mechanisms (ADCC). Moreover, knockout mice deficient in inhibitory FcRIIB are hypersensitive to antibody mediated tumor suppression, indicating that antibody control of tumor growth requires FcR interactions.5 Since FcR-dependent mechanisms contribute substantially to the action of cytotoxic antibodies, optimal anti-tumor antibodies bind preferentially to activation Fc receptors and minimally to the inhibitory partner FcRIIB. The clear role for FcR-bearing effectors in mediating response to rituximab in humans with follicular lymphoma (discussed in detail below) further demonstrates the importance of ADCC.6
A recently published mouse model for anti-CD20 immunotherapy used a panel of twelve mouse anti-mouse CD20 monoclonal antibodies representing all four immunoglobulin G isotypes.7 Anti-CD20 antibodies rapidly depleted the vast majority of circulating and tissue B cells in an isotype-restricted manner that was completely dependent on effector cell Fc receptor expression. B cell depletion used both FcRI- and FcRIII-dependent pathways, whereas B cells were not eliminated in FcR common chain-deficient mice. Monocytes were the dominant effector cells for B cell depletion in this model system.
Complement-mediated cytotoxicity
Rituximab is capable of binding to C1q and in vitro studies have demonstrated the ability of the antibody to mediate complement-dependent cell lysis (CDC) of human B-lymphoid cell lines.8 CDC is highly variable between cell lines, ranging from 100% lysis to complete resistance. Complement inhibitors CD55, and to a lesser extent CD59, are important regulators of CDC in follicular lymphoma cell lines, in that blocking CD55 and/or CD59 function with specific antibodies significantly increased CDC in cells treated with rituximab.3 However, expression of CD55 and CD59 on tumor cells and their susceptibility to in vitro CDC did not predict clinical outcome after in vivo treatment with rituximab in a clinical trial.9
An important mechanistic observation involves the ability of certain anti-CD20 monoclonal antibodies (including rituximab) in vitro to translocate CD20 into lipid rafts and activate lytic complement,10 In these situations, a raft location may favor complement activation by the monoclonal antibody, or rafts may be more sensitive to complement penetration. Additional support for the role of complement in rituximab-induced cytotoxicity includes the observation that complement is consumed during rituximab therapy and the level of complement activation is correlated with the severity of the side-effects associated with rituximab infusions.11 Interestingly, the B1 anti-CD20 antibody (tositumomab) does not redistribute CD20 into membrane rafts, bind C1q, or cause efficient CDC.12 In the mouse model of rituximab therapy, although most anti-CD20 antibodies activated complement in vitro, B cell depletion was completely effective in mice with genetic deficiencies in C3, C4, or C1q complement components.7 The precise role of CDC in rituximab therapy, and the potential that complement inhibition may contribute to rituximab resistance remains controversial and requires further study.
CD20 signaling and apoptosis
Direct apoptosis due to cross-linking of CD20 has been observed in malignant lymphoma cell lines; however, the degree of apoptosis, growth conditions, and specific antibody have been highly variable from study to study.2 Cross-linking appears to be critical for apoptosis to occur. A gene expression analysis was undertaken to define signaling events triggered by rituximab and demonstrated that genes induced by rituximab in vitro were specific and limited in number, and included genes known to be involved in control of cell growth and apoptosis.13 Evidence suggests that some patients with chronic lymphocytic leukemia (CLL) treated with rituximab have in vivo activation of caspase-9, caspase-3, and poly(ADP-ribose) polymerase (PARP) cleavage in circulating leukemia cells immediately following infusion of rituximab. This suggests that direct apoptosis is involved in the elimination of peripheral blood tumor cells after rituximab treatment.14 This caspase activation and mitochondrial triggering may not be obligatory for cells to become apoptotic.15
As previously mentioned, binding of rituximab significantly increases the affinity of CD20 for lipid rafts. In addition to the aforementioned effects on CDC, these rafts appear to play a crucial role for CD20-induced caspase activation through increased calcium conductivity and induction of a close proximity with other raft localizing molecules, including scr-family kinases.16 Alas and colleagues demonstrated downregulation of interleukin (IL)-10 following rituximab treatment, and associated decreased DNA binding activity of STAT3 and decreased Bcl-2 expression.17 Numerous other signaling pathways have been invoked in rituximab-induced apoptosis, including down-modulation of the ERK1/2 and NF-κB transcription factors, leading to downregulation of bcl-xl.18 Rituximab-resistant clones appear to display different phenotypic, genetic and functional properties compared to wild type cells, suggesting resistance may evolve from impaired signaling.
Importance of the cellular microenvironment
The microenvironment has recently been demonstrated to play critical roles in B cell homeostasis and also appears to contribute to rituximab-induced cytotoxicity. In a murine model of human CD20 expression in which rituximab therapy mimics B cell depletion seen in humans,19 circulating B cells are cleared through the RES, and B cells residing within lymphoid tissues required access to the vasculature to deliver targeted B cells to effector cells within the RES. B cells within the marginal zone compartment exhibited a greater dependence on CDC than on FcR-mediated mechanisms for depletion. An apparent interrelationship of B cell survival factors present in the microenvironment (BAFF/BLyS) and depleting ability of antiCD20 antibodies was also observed. The importance of the microenvironment in rituximab-induced cytotoxicity is also inferred by differential responses to rituximab therapy in various histologies of CD20 positive lymphomas (which have unique microenvironments), and the observation that rituximab-induced molecular remissions in the blood and bone marrow can occur in the setting of progressive nodal disease.
“Vaccinal effect” of rituximab
Treatment of tumor cells with antibodies such as rituximab that are capable of inducing a proapoptotic signal via their cell surface target structure may induce cellular responses against the tumor. Rituximab therapy of lymphoma cells may promote uptake and cross-presentation of lymphoma cell-derived peptides by antigen-presenting dendritic cells (DC), induce maturation of DC, and allow the generation of specific cytotoxic T cell responses.20 Studies have demonstrated that monoclonal antibody therapy can induce specific antitumor immunity through dendritic cells.21 The prolonged time to response, and improved responses observed following retreatment with rituximab (“boost effect”) both lend credence to this hypothesis.
Mechanisms of Rituximab Resistance
Tumor-associated resistance
Since the exact mechanisms of rituximab activity in vivo remain elusive, the nature of both primary and secondary resistance to rituximab is also poorly understood. A relatively small study (N = 24) using cDNA microarrays at Stanford University attempted to investigate whether gene expression patterns in primary lymphoma specimens could predict sensitivity to subsequent rituximab therapy.22 Two subtypes of follicular lymphoma were studied in this cohort, with a subset of follicular lymphoma specimens exhibiting a gene expression pattern more similar to normal lymph nodes than the other subset of follicular lymphoma. Most of the rituximab nonresponders clustered with this “normal”-appearing lymph node group. Many of the high expressing genes in this nonresponder group were involved in cellular immune responses, including cytokine, complement, and T cell receptor signaling, suggesting that the microenvironment, more than the malignant cells, may have a profound impact on responsiveness to rituximab. These data are in keeping with a larger international gene profiling study demonstrating that length of survival among patients with follicular lymphoma correlates with the molecular features of nonmalignant immune cells present in the tumor at diagnosis.23 An appealing implication of these findings is that targeting the microenvironment may be a rational way to overcome rituximab resistance. Such efforts are currently underway.
CD20 expression is heterogeneous among cells in a follicular lymphoma specimen and between specimens. Small lymphocytic lymphoma has lower CD20 expression, and a concomitantly lower response rate to rituximab; however, there are no data supporting that staining intensity of CD20 predicts response in patients with follicular lymphoma. CD20-negative relapses have been reported,24,25 but some have suggested that false-negative CD20 studies can result from blockade by bound rituximab. The true incidence of this is unknown as biopsies post relapse are rare, but loss of CD20 expression is not generally felt to be an important resistance mechanism of rituximab. Further evidence that CD20 expression modulation does not contribute to resistance is the observation that effective CD20 binding by radioimmunoconjugates can occur in the setting of rituximab-resistant disease.26
Host-associated resistance
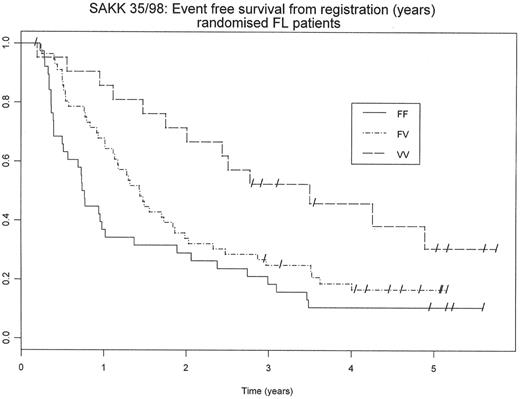
Innate resistance to rituximab has been observed in certain settings of follicular lymphoma. Successful ADCC requires leukocyte receptors for the Fc portion of IgG (FcR), whose function is to link the IgG-sensitized antigens to FcR-bearing cytotoxic cells and to trigger the cell activation mechanisms. Three classes of FcR (FcRI, FcRII, and FcRIII) exist in humans, and functional polymorphisms of these genes exist. The polymorphism that encodes FcRIIIa with either a phenylalanine (F) or a valine (V) at amino acid position 158 results in a higher affinity for human immunoglobulin GI, and increased ADCC, when V is the allotype. The clinical relevance of the FCGR3A-158V/F genotype was determined in 49 patients treated with rituximab for a de novo follicular non-Hodgkin lymphoma. The objective response rate at 12 months was 90% in FCGR3A-158V homozygous patients compared with 51% in FCGR3A-158F carriers, a statistically significant difference. The homozygous FCGR3A-158V genotype was confirmed to be the single parameter associated with clinical and molecular responses by multivariate analysis in this small series. Ghielmini and colleagues have evaluated the role of the FCGR3A genotype in response to single agent rituximab in a larger series of patients with follicular lymphoma (see Figure 1 ), again observing dramatic differences. Patients with the 158V genotype had a median EFS of 41 months compared with only 9 months for the FF genotype.27 This mechanism of resistance could, in theory, be overcome with more effective antibody constructs (see “Targeting CD20 in folicular NHL: novel anti-CD20 therapies, antibody engineering, and the use of radioimmunoconjugates” by Dr. Leonard in this volume).
Although early data suggested that serum rituximab levels were higher in responding patients than in non-responders,28 more recent data suggest that serum rituximab levels and the classical pharmacokinetics of rituximab do not appear to have a significant impact on response in patients with follicular lymphoma. Gordan et al followed standard four weekly infusions of rituximab with a single infusion of rituximab when the serum rituximab level decreased below 25 μg/mL in a cohort of patients with CD20-positive lymphoma. Rituximab resistance was not regularly associated with lower serum antibody levels, and 95% of patients required three or fewer infusions to be maintained in the target range.29 In further support of rituximab level having minimal impact on resistance is the low rate of human anti-chimeric antibody (HACA) formation following rituximab therapy.
Overcoming Resistance and Improving Rituximab Therapy
Table 1 outlines potential ways of overcoming rituximab resistance.
Enhancing ADCC
Since ADCC appears to play an important role in the response to rituximab and other monoclonal antibodies, several approaches to stimulate effector cell function have been suggested to augment the response to monoclonal antibody therapy. In an early attempt to improve ADCC in the context of monoclonal antibody therapy, Vlasveld and colleagues treated 7 patients with indolent B-cell lymphoma with a combination of a murine anti-CD19 antibody and continuous infusion low-dose IL-2, a lymphokine that enhances ADCC in vitro.30 Lymphocytes from involved lymph nodes showed enhanced ADCC, which provided proof-of-principle.
More recently, several human studies have evaluated the role of cytokines in combination with rituximab (Table 2 ). For example, interferon (IFN)-α, an immunomodulatory cytokine that induces antigen expression and enhances cytotoxicity of immunotoxins, has been combined with rituximab. In one study, 38 patients received IFN-α-2a subcutaneously 3 times a week for 12 weeks, with rituximab given in a standard fashion on weeks 5 through 8.31 In this study, combination immunotherapy was well tolerated, and although the overall response rate did not differ significantly from that expected with rituximab alone, time to progression in responding patients appeared prolonged. Randomized studies evaluating the combination of IFN with rituximab are ongoing; however, the substantial toxicity associated with IFN will no doubt limit the overall utility of this approach. Rituximab has also been safely combined with IL-12,32 another cytokine that mediates effector cell number and function. Objective responses occurred in 29 of 43 patients treated in a phase I study (69%), with 8 of 11 complete responses seen at optimal IL-12 doses. Toxicity was moderate in this study. Rituximab has also been safely combined granulocyte colony-stimulating factor (G-CSF),33 which greatly enhances the cytotoxicity of neutrophils in ADCC.
Trials combining IL-2 with rituximab have demonstrated safety and effector cell enhancement, and suggested a prolonged time to progression in patients with follicular NHL.34,35 In one trial, increased ADCC as a result of IL-2 therapy correlated with clinical response to rituximab therapy. In our study, CD8-positive and CD56-positive cells increased over baseline by day 29 of IL-2 therapy, and remained increased on day 56 of therapy, with a median percentage increase of CD56-positive cells from baseline to day 56 of 115% (P = 0.0002). Eleven patients showed clinical response (1CR, 10PR) for an overall response rate of 55%, and the median progression-free survival exceeded 13 months, with a median of 22 months follow-up.
Other means of enhancing ADCC, including the use of novel anti-CD20 constructs engineered to facilitate binding with Fc receptors, are discussed in detail in article by Dr. Leonard in this volume. Clearly, the approach of enhancing effector mechanisms, including ADCC, in combination with monoclonal antibody therapy holds promise, and is worthy of additional study.
Targeting the microenvironment
Immunostimulatory CpG DNA sequences are short sequences of DNA that have multiple effects on the human immune system.36 Immunostimulatory effects of these sequences include induction of B-cell proliferation and immunoglobulin production, secretion of numerous cytokines including IFN-α, IFN-β, IL-12, and IL-18 by macrophages and dendritic cells (DCs), and secretion of IFN-γ induced by IL-12 and IFN-α from natural killer cells.37 This cytokine milieu can induce the differentiation of naive CD4+ T cells into Th1 cells on encountering specific antigens. Moreover, CpG sequences also increase antigen presentation and costimulatory molecule expression.38 CpG sequences could have potentially synergistic effects with monoclonal antibodies through both augmentation of ADCC and enhancement of presentation of antigens released by killed tumor cells in the microenvironment.
We have recently completed a phase I trial combining a CpG oligonucleotide with rituximab.39 The combination was well tolerated and demonstrated significant dose-dependent biological activity, measured through a defined a set of gene expression markers. All of the genes significantly induced were regulated by type-1 interferons. Given these promising results, we are currently enrolling patients on a phase II trial that will further explore the effects of this rational combination on both T cell function and ADCC, with a critical examination of the cellular microenvironment before and after therapy.
Conclusions
Rituximab has multiple complex mechanisms of cytotoxicity in vivo, including ADCC, CDC, direct apoptotic signaling, and possible vaccinal effects. The cellular microenvironment within follicular lymphoma may have a profound impact on which mechanism is dominant and confer resistance in many situations. Overcoming resistance to rituximab is possible utilizing multiple approaches, including rational biologic combination immunotherapy, engineered antibodies, and radioimmunoconjugates. Improved ability to overcome resistance will require further elucidation of critical signaling pathways involved in rituximab-induced cytotoxicity, and comprehensive understanding of interactions between the aforementioned multiple mechanisms of action.
Potential mechanisms of anti-CD20 resistance and possible ways to overcome resistance.
| Mechanism of Resistance . | Overcoming Resistance . |
|---|---|
| Abbreviations: ADCC, antibody-mediated cellular cytotoxicity; IFN, interferon; IL, interleukin; G-CSF, granulocyte colony-stimulating factor; CpG, immunostimulatory oligonucleotides | |
| Fc receptor polymorphism | Engineered antibodies to facilitate Fc receptor binding |
| CD20 modulation | IFN-α; CpG; higher dose |
| Pharmacokinetics | Prolonged schedule; higher dose |
| Complement inhibitors | Anti-CD55; Anti-CD59; Bispecific antibodies |
| Decreased ADCC | IL-2; IL-12; IFN-α; G-CSF; CpG |
| Microenvironmental altercations | CpG |
| Impaired CTL generation | Avoid immunosuppressive therapy; CpG; prolonged schedule |
| Tumor-associated resistance | Small molecules; chemotherapy combinations; radioimmunoconjugates |
| Mechanism of Resistance . | Overcoming Resistance . |
|---|---|
| Abbreviations: ADCC, antibody-mediated cellular cytotoxicity; IFN, interferon; IL, interleukin; G-CSF, granulocyte colony-stimulating factor; CpG, immunostimulatory oligonucleotides | |
| Fc receptor polymorphism | Engineered antibodies to facilitate Fc receptor binding |
| CD20 modulation | IFN-α; CpG; higher dose |
| Pharmacokinetics | Prolonged schedule; higher dose |
| Complement inhibitors | Anti-CD55; Anti-CD59; Bispecific antibodies |
| Decreased ADCC | IL-2; IL-12; IFN-α; G-CSF; CpG |
| Microenvironmental altercations | CpG |
| Impaired CTL generation | Avoid immunosuppressive therapy; CpG; prolonged schedule |
| Tumor-associated resistance | Small molecules; chemotherapy combinations; radioimmunoconjugates |
Selected clinical trials combining immunostimulatory agents with rituximab for patients with indolent non-Hodgkin lymphoma (NHL).
| Reference . | Agent . | Suggested Activity . | N . | Major Findings . |
|---|---|---|---|---|
| Abbreviations: IL, interleukin; GCSF, granulocyte colony-stimulating factor; IFN, interferon; ADCC, antibody-mediated cellular cytotoxicity; NK, natural killer; ORR, overall response rate; CR, complete response; CpG, Immunostimulatory oligonucleotides | ||||
| Friedberg34 | IL-2 | Enhance ADCC: NK | 20 | ORR 55%; prolonged response duration |
| Gluck35 | IL-2 | Enhance ADCC: NK | 34 | ADCC activity correlated with response |
| Ansell32 | IL-12 | Enhance ADCC: NK | 43 | ORR 69%; High CR rate |
| van der Kolk33 | GCSF | Enhance ADCC: neutrophil | 26 | ORR 42%; prolonged response duration |
| Davis31 | IFN-α | Enhance ADCC: NK; CD20 | 38 | ORR 45%; prolonged response duration |
| Sacci40 | IFN-α | Enhance ADCC: NK; CD20 | 64 | ORR 70%; prolonged response duration |
| Friedberg39 | CpG | Microenvironment | 20 | ORR 32%; Type 1 IFN induction |
| Reference . | Agent . | Suggested Activity . | N . | Major Findings . |
|---|---|---|---|---|
| Abbreviations: IL, interleukin; GCSF, granulocyte colony-stimulating factor; IFN, interferon; ADCC, antibody-mediated cellular cytotoxicity; NK, natural killer; ORR, overall response rate; CR, complete response; CpG, Immunostimulatory oligonucleotides | ||||
| Friedberg34 | IL-2 | Enhance ADCC: NK | 20 | ORR 55%; prolonged response duration |
| Gluck35 | IL-2 | Enhance ADCC: NK | 34 | ADCC activity correlated with response |
| Ansell32 | IL-12 | Enhance ADCC: NK | 43 | ORR 69%; High CR rate |
| van der Kolk33 | GCSF | Enhance ADCC: neutrophil | 26 | ORR 42%; prolonged response duration |
| Davis31 | IFN-α | Enhance ADCC: NK; CD20 | 38 | ORR 45%; prolonged response duration |
| Sacci40 | IFN-α | Enhance ADCC: NK; CD20 | 64 | ORR 70%; prolonged response duration |
| Friedberg39 | CpG | Microenvironment | 20 | ORR 32%; Type 1 IFN induction |
Event-free survival following rituximab monotherapy of follicular lymphoma in patients by genotype of FcRIIIa with either a phenylalanine (F) or a valine (V), or both.
Event-free survival following rituximab monotherapy of follicular lymphoma in patients by genotype of FcRIIIa with either a phenylalanine (F) or a valine (V), or both.
Dr. Friedberg is supported in part by a career development award from the National Cancer Institute (CA-102216).