Abstract
Monoclonal gammopathy of undetermined significance (MGUS) and smoldering multiple myeloma (SMM) are asymptomatic, pre-malignant disorders characterized by monoclonal plasma cell proliferation in the bone marrow and absence of end-organ damage. Recent advances in the pathogenesis, natural history, and prognosis of MGUS and SMM are reviewed. A new risk stratification system to determine the prognosis of MGUS using the size and type of M protein, and the serum free light chain assay is discussed.
Monoclonal gammopathy of undetermined significance (MGUS) and smoldering multiple myeloma (SMM) are asymptomatic, pre-malignant disorders characterized by monoclonal plasma cell proliferation in the bone marrow and absence of end-organ damage such as osteolytic bone lesions, anemia, or renal failure.1 Patients with MGUS and SMM require indefinite follow-up given their life-long risk of progression to multiple myeloma or related malignancy. Since multiple myeloma has a median survival of only 3 to 4 years,2,3 predicting and preventing the progression of MGUS and SMM to myeloma is of great importance. In the last five years, significant advances have been made in the understanding of the pathogenesis, natural history, and prognosis of MGUS and SMM.
Diagnostic Criteria
The diagnostic criteria for MGUS and SMM have recently been revised. MGUS is defined by the presence of a serum monoclonal (M) protein < 3 g/dL, bone marrow plasma cells < 10%, and absence of anemia, hypercalcemia, lytic bone lesions, or renal failure attributable to the plasma cell proliferative disorder.4,5 The diagnosis of SMM requires a serum M protein ≥ 3 g/dL or bone marrow plasma cells ≥ 10%, plus absence of anemia, hypercalcemia, lytic bone lesions, or renal failure attributable to the plasma cell proliferative disorder.4,5 Clinically, the main reason to divide pre-malignant plasma cell disorders into these two distinct entities is because the risk of progression to malignancy is substantially different between MGUS and SMM, 1% per year versus 10%–20% per year, respectively.6–9 This difference in the risk of progression mandates that patients with MGUS and SMM are managed differently in terms of frequency of follow-up and development of chemopreventive strategies. Biologically, MGUS and SMM likely represent a continuum of limited, clonal plasma cell expansion and are analogous to colonic polyps.
Pathogenesis
Origin of MGUS and SMM
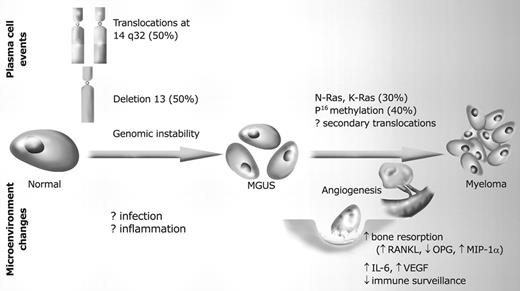
Approximately 50% of patients with MGUS and SMM have primary translocations in the clonal plasma cells involving the immunoglobulin heavy chain (IgH) locus on chromosome 14q32 (IgH translocated MGUS/SMM) (Figure 1 ).2,10 The most common partner chromosome loci and genes dysregulated in these translocations are: 11q13 (CCND1 [cyclin D1 gene]), 4p16.3 (FGFR-3 and MMSET), 6p21 (CCND3 [cyclin D3 gene]), 16q23 (c-maf), and 20q11 (mafB).11–13 It is felt that these translocations are important pathogenetically in initiating and sustaining clonal proliferation. The precipitating event for these translocations may be related to infection or immune dysregulation, and likely occurs during IgH switch recombination or somatic hypermutation.10 The pathogenesis in 40%–50% of MGUS and SMM with no evidence of IgH translocations (IgH non-translocated MGUS/SMM) is unclear. Deletion of chromosome 13, a major prognostic factor in multiple myeloma, is seen in up to 50% of patients with MGUS by interphase fluorescent in situ hybridization; hence, the presence of this abnormality cannot be used to differentiate MGUS from multiple myeloma.13
Progression of MGUS/SMM to multiple myeloma
The constant rate of progression of MGUS to multiple myeloma in a recent epidemiologic study over a period spanning 30–35 years is very suggestive, if not one of the best examples of a simple, random, two-hit genetic model of malignancy.6 The risk of progression is similar regardless of the known duration of antecedent MGUS, suggesting that the second hit responsible for progression is a random event, not cumulative damage.
The specific second hit that initiates the cascade of events associated with progression is unknown and may even be different in IgH translocated versus non-translocated MGUS/SMM, even within IgH translocated MGUS depending on the partner chromosome involved. Several abnormalities have been detected with progression in both the plasma cell and its microenvironment that likely play a role in the progression of MGUS/SMM, but little is known about the sequence of events (Figure 1 ). Ras mutations, p16 methylation, abnormalities involving the myc family of oncogenes, secondary translocations, and p53 mutations have been identified in the clonal plasma cells.11 Clearly the bone marrow microenvironment undergoes marked changes with progression, including induction of angiogenesis, which is markedly different in MGUS than in multiple myeloma,14 suppression of cell-mediated immunity,15 and paracrine loops involving cytokines such as interleukin-6 and VEGF (vascular endothelial growth factor).16
The transition from MGUS to MM may involve an angiogenic switch as in solid tumors. In solitary plasmacytoma, which is the closest analogy to a solid tumor among the spectrum of plasma cell disorders, induction of angiogenesis at the time of diagnosis has been shown to be a predictor of progression to myeloma, suggesting a pathogenetic role for the process in disease progression.17 Angiogenesis is a striking characteristic of multiple myeloma (MM) and has prognostic importance. Increased angiogenesis in MM is correlated with disease activity, bone marrow plasma cell involvement, and plasma cell proliferative capacity. The formation of new blood vessels is induced by the malignant plasma cells and may contribute to disease progression by ensuring an adequate tumor nutrient supply as well as by paracrine stimulation of tumor growth. There is a gradual increase in degree of bone marrow angiogenesis along the disease spectrum from MGUS to SMM to newly diagnosed myeloma (NMM) and relapsed myeloma (RMM). In a study of 400 patients, the median microvessel density (MVD) was 1.3 (range, 0–11) in controls, 1.7 (0–10) in amyloidosis, 3 (0–23) in MGUS, 4 (1–30) in SMM, 11 (1–48) in NMM, and 20 (6–47) in RMM, P < 0.001.14 In another study, 61% of MM bone marrow plasma samples stimulated angiogenesis in an in vitro angiogenesis assay, compared to 0% of SMM and 7% of MGUS, P < 0.001.18 The increased angiogenesis seen in MM may be related to expression of proangiogenic cytokines.19 However, no significant difference was seen in expression of VEGF, basic fibroblast growth factor (bFGF), or their receptors between MGUS, SMM and MM. Recently, we have described loss of angiogenesis inhibitory activity with disease progression from MGUS to MM, which may in part account for the increase in angiogenesis that occurs in MM.18 In an in vitro human angiogenesis assay, 63% of MGUS bone marrow plasma samples inhibited angiogenesis, compared to SMM (43%) and NMM (4%), P < 0.001. The inhibitory activity was heat stable, not overcome by addition of VEGF and studies are ongoing to determine the nature and identity of angiogenesis inhibitors in MGUS. The role of angiogenesis in myeloma has triggered an interest in anti-angiogenic therapy for the disease. Studies show that while increased MVD in MM may not regress following conventional dose or high-dose chemotherapy, regression has been noted in responders with thalidomide, an agent with known anti-angiogenic properties.20 Clinical trials have been initiated to test the hypothesis that therapy with antiangiogenic agents may inhibit angiogenesis and delay progression in SMM.
Pathogenesis of bone lesions
The development of bone lesions in MM is caused by an imbalance between the activity of osteoclasts and osteoblasts. There is an increase in RANKL (receptor activator of nuclear factor κB ligand) expression by osteoblasts (and possibly plasma cells) accompanied by a reduction in the level of its decoy receptor, osteoprotegerin (OPG).21,22 This leads to an increase in RANKL/OPG ratio, which causes osteoclast activation and bone resorption. In addition, increased levels of macrophage inflammatory protein–1α (MIP-1α), interleukin (IL)-3 and IL-6 produced by marrow stromal cells contribute to the overactivity of osteoclasts. At the same time, increased levels of IL-3, IL-7 and DKK1 produced by marrow stroma inhibit osteoblast differentiation. These changes lead to osteoclast activation and bone resorption without any repair activity by osteoblasts.
Natural History
Natural history of MGUS
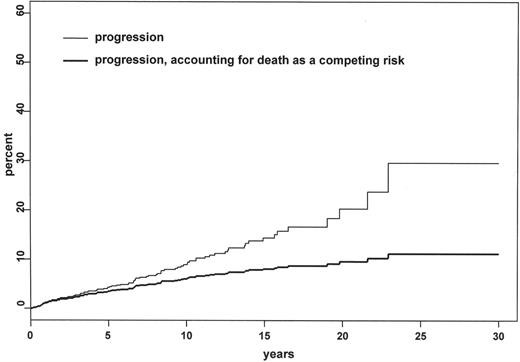
MGUS is the most common plasma cell dyscrasia, present in approximately 3% of the general population 50 years of age and older.23 The prevalence increases with age; 1.7% in those 50–59 years of age, and over 5% in those over the age of 70. The rate of progression to multiple myeloma or related malignancy is 1% per year (Figure 2 ).6,7 Thus, the risk of malignancy for a 50-year-old patient with a 25-year life span is 25%. However, because of the relatively low annual risk of progression, one needs to take into consideration other competing causes of death such as heart disease and unrelated malignancies. In fact, the true life-time probability of progression is substantially lower when these competing causes of death are taken into account, 11.2% at 25 years (Figure 2 ).24 The risk of progression with MGUS does not diminish even after 25–35 years, making lifelong follow-up necessary in all persons diagnosed with MGUS.6,25
Natural history of SMM
SMM accounts for approximately 15% of all cases with newly diagnosed multiple myeloma.1,26 The prevalence estimates for SMM are distorted since many reports include asymptomatic patients with small lytic bone lesions on skeletal survey. Others exclude patients with bone lesions on skeletal survey, but include patients who have lytic lesions by magnetic resonance imaging (MRI). A true prevalence using strict criteria for SMM as defined earlier is not available.
Most patients with SMM progress eventually to symptomatic disease, and the risk of progression is substantially higher than with MGUS.26 However, as illustrated in the first description of the entity, some patients can remain free of progression for a number of years.27 The time to progression (TTP) to symptomatic disease is approximately 3–4 years, but differs greatly depending on the definition used for SMM.9 In SMM patients having bone marrow plasma cells ≥ 10%, the median time to progression is approximately 2–3 years.28 In another study, the risk of progression was only 20% at 6 years.29 However, this study considered patients to have SMM only if patients demonstrated no disease progression after one year of follow up. Preliminary data from a large study by Kyle and colleagues using the current criteria for SMM indicate a risk of progression of approximately 10% per year, a rate much higher than observed with MGUS.30
Prognosis
All patients with MM are felt to evolve from a MGUS/SMM stage, although in many MM patients these premalignant stages are unrecognized clinically due to their asymptomatic nature. A prior history of MGUS or SMM has no impact on the prognosis of MM.
Risk factors for progression of MGUS
Given the baseline risk of progression of MGUS, the potential adverse effects of prophylactic approaches and the duration for which such interventions will be needed, only patients at a high risk for progression can be considered candidates for testing preventive strategies. Similarly it is also important to identify low-risk patients who can be reassured and should not be subjected to potentially harmful or expensive tests or preventive interventions. It is therefore important to identify risk factors that can accurately predict the subset of patients with the greatest likelihood of progression. In a large population-based study of MGUS, out of 13 potential risk factors, only the size and type of M protein (IgM and IgA subtypes) were predictive of progression.6 In another study, bone marrow plasma cell percentage of 6%–9% carried twice the risk of progression compared to marrow involvement that is ≤ 5%.29
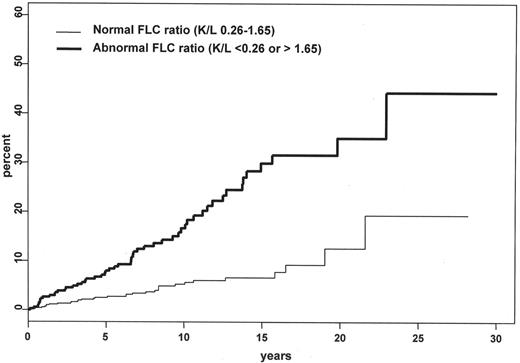
Recently, an abnormal serum free light chain (FLC) ratio at baseline has been shown to be an important risk factor for progression of MGUS to malignancy in a large population-based study of 1148 patients (Figure 3).24 In this study, the risk of progression in MGUS patients with an abnormal FLC ratio was significantly higher compared to patients with a normal ratio (hazard ratio, 3.5; 95% CI, 2.3–5.5; P < 0.001) and was independent of the size and type of the serum M protein. The risk of progression to myeloma or related malignancy at 10 years was 17% with an abnormal ratio compared to 5% with a normal ratio; corresponding rates at 20 years were 35% and 13%, respectively. An abnormal serum FLC ratio is interpreted as evidence of free monoclonal light chains in the serum. The mechanisms by which presence of monoclonal free light chains increase risk of progression in MGUS are not understood, but they may either represent clonal evolution of the neoplastic plasma cell or function as a surrogate marker for cytogenetic subtypes of MGUS that possess an inherently higher tendency progression. The mechanism of the imbalance in heavy and light chain production is more likely related to suppression of heavy chain expression rather than overexpression of light chains.
The FLC ratio is measured using a highly sensitive serum free light chain assay currently available in clinical practice.31 The assay quantitates free kappa (κ) and lambda (λ) chains (i.e., light chains that are not bound to intact immunoglobulin) secreted by plasma cells (normal range for free κ, 0.33 to 1.94 mg/dL; normal range for free λ, 0.57 to 2.63 mg/dL).32 The normal FLC ratio (free κ/free λ) is 0.26 to 1.65.33 Patients with a serum FLC ratio < 0.26 are defined as having monoclonal λ free light chain and those with ratios > 1.65 are defined as having a monoclonal κ free light chain.
A new risk stratification system has been developed to predict the risk of progression of MGUS based on 3 risk factors: size of the serum M protein, the type of immunoglobulin, and the serum FLC ratio (Table 1 ).24 Patients with an abnormal serum FLC ratio, non-IgG MGUS, and a high serum M protein level (≥ 1.5 g/dL) had a risk of progression of 58% at 20 years (high-risk MGUS), compared to 5% when none of the risk factors were present (low-risk MGUS). In fact, the low-risk MGUS subset (constituting almost 40% of the cohort) carries a lifetime risk of only 2% when competing causes of death are taken into account. Patients with low-risk MGUS can be reassured and can be monitored less frequently than once a year, perhaps only if symptoms of myeloma or related disorder become apparent. In contrast those with high-risk MGUS need to be monitored more closely and will serve as the base from which additional risk factors can identify a suitable cohort for chemo-prevention trials.
The presence of circulating plasma cells detected by a sensitive slide-based immunofluorescent assay is an adverse predictor of progression in MGUS.34 This suggests that alterations in expression of adhesion molecules may be involved in the progression of MGUS to MM; alternatively the presence of circulating plasma cells may be a marker of plasma cell proliferative rate. The clinical application of this finding is presently limited by the lack of widespread availability of the test in clinical practice.
Risk factors for progression of SMM
As discussed earlier the risk of progression in SMM is significantly higher than MGUS. Although most patients with SMM are candidates for clinical trials evaluating preventive strategies, using selected risk factors it may be possible to identify a cohort of patients who may benefit the most and in whom the risks of chronic therapy are acceptable.
Abnormal peripheral blood monoclonal plasma cell studies, defined as an increase in the number or proliferative rate of circulating plasma cells by immunofluorescent assays, have been shown to indicate a higher risk of progression in SMM.28 This test is, however, not widely available. Weber and colleagues have shown, in a study of 109 patients, that the size and type of immunoglobulin are important predictors of progression.8 Patients with a serum M protein ≤ 3 gm/dL and IgG type (comprising about 45% of patients) had a median TTP of over 4 years. Patients with either serum M protein > 3 gm/dL or IgA type (about 45% of patients) had a median TTP of approximately 2 years, while a small subset of patients with > 3 gm/dL IgA SMM had a median TTP of 9 months.
In patients determined to have SMM by using standard clinical, laboratory and roentgenographic studies, the presence of occult bone lesions on MRI magnetic resonance imaging greatly increases the risk of progression in asymptomatic MM.26 In a recent study, Wang and colleagues estimated risk of progression in 72 patients with SMM in whom an MRI of the spine was also performed.9 The median TTP was significantly shorter with an abnormal MRI compared to normal MRI, 1.5 years versus 5 years, respectively.
There are no data on the use of the serum FLC assay to predict risk of progression in SMM at present.
Management
MGUS
The current standard of care for both MGUS and SMM is observation alone, without therapy.2,35 Patients with MGUS may benefit from risk-stratification based on Table 1 , to guide follow up. Patients with low-risk MGUS can be rechecked in 6 months and then once every 2 years or only at the time of symptoms for evidence of progression. All other subsets of patients need to be rechecked in 6 months and then yearly thereafter on an indefinite basis. In addition to history and examination, laboratory tests required at follow-up include a complete blood count, serum calcium, serum creatinine, and serum protein electrophoresis. Chemo-prophylactic trials with agents such as dehydroepiandrosterone (DHEA), anakinra, and celecoxib are underway.
SMM
No specific therapy is recommended for SMM, but patients require more frequent follow-up than MGUS, at least once every 3–4 months. In addition to follow-up studies recommended for MGUS, a skeletal survey should be repeated at least once every year. In addition if the patient has evidence of baseline urinary paraprotein excretion, a 24-hour urine protein electrophoresis should also be done periodically during follow-up.
So far there is no evidence to support early therapy prior to development of symptomatic myeloma. Two small randomized trials with alkylating agents showed similar overall survival with early therapy compared to therapy at the time of symptomatic progression. However, clinical trials are now underway to determine if newer agents and bisphosphonates can delay progression. A recent phase II clinical trial demonstrated significant paraprotein responses, and prolongation of time to progression compared to historical controls with thalidomide.36 However, thalidomide has significant nonhematologic side-effects and confirmatory data from randomized trials are needed before such therapy can be recommended for patients with SMM. A randomized phase III trial at Mayo Clinic is currently testing thalidomide plus zoledronic acid versus zoledronic acid in patients with smoldering myeloma and the results of this study will shed light on the utility of thalidomide in this setting. Outside of a clinical trial, therapy with bisphosphonates is not recommended.
Risk-stratification model to predict progression of monoclonal gammopathy of undetermined significance to myeloma or related disorders.
| Risk Group . | No. of Patients . | Relative Risk . | Absolute Risk of Progression at 20 Years . | Absolute Risk of Progression at 20 Years Accounting for Death as a Competing Risk . |
|---|---|---|---|---|
| This table was originally published in Blood and is reproduced with permission. Rajkumar SV et al., Serum free light chain ratio is an independent risk factor for progression in monoclonal gammopathy of undetermined significance (MGUS) © the American Society of Hematology Blood . 2005 ;106 :812 –817. | ||||
| Low-risk (Serum M protein < 1.5 gm/dL, IgG subtype, normal FLC ratio (0.26–1.65) | 449 | 1 | 5% | 2% |
| Low-Intermediate-risk (Any 1 factor abnormal) | 420 | 5.4 | 21% | 10% |
| High-Intermediate-risk (Any 2 factors abnormal) | 226 | 10.1 | 37% | 18% |
| High-risk (All 3 factors abnormal) | 53 | 20.8 | 58% | 27% |
| Risk Group . | No. of Patients . | Relative Risk . | Absolute Risk of Progression at 20 Years . | Absolute Risk of Progression at 20 Years Accounting for Death as a Competing Risk . |
|---|---|---|---|---|
| This table was originally published in Blood and is reproduced with permission. Rajkumar SV et al., Serum free light chain ratio is an independent risk factor for progression in monoclonal gammopathy of undetermined significance (MGUS) © the American Society of Hematology Blood . 2005 ;106 :812 –817. | ||||
| Low-risk (Serum M protein < 1.5 gm/dL, IgG subtype, normal FLC ratio (0.26–1.65) | 449 | 1 | 5% | 2% |
| Low-Intermediate-risk (Any 1 factor abnormal) | 420 | 5.4 | 21% | 10% |
| High-Intermediate-risk (Any 2 factors abnormal) | 226 | 10.1 | 37% | 18% |
| High-risk (All 3 factors abnormal) | 53 | 20.8 | 58% | 27% |
Risk of progression to myeloma or related disorder in 1148 patients with monoclonal gammopathy of undetermined significance (MGUS). The upper curve illustrates risk of progression of all patients without taking into account competing causes of death. The lower curve illustrates risk of progression after accounting for other competing causes of death. This figure was originally published in Blood and is reproduced with permission.
Risk of progression to myeloma or related disorder in 1148 patients with monoclonal gammopathy of undetermined significance (MGUS). The upper curve illustrates risk of progression of all patients without taking into account competing causes of death. The lower curve illustrates risk of progression after accounting for other competing causes of death. This figure was originally published in Blood and is reproduced with permission.
Risk of progression of monoclonal gammopathy of undetermined significance (MGUS) to multiple myeloma based on the serum free light chain ratio. The upper curve illustrates risk of progression of monoclonal gammopathy of undetermined significance in patients with an abnormal serum kappa/lambda free light chain ratio (< 0.26 or > 1.65). The lower curve illustrates the risk of progression in patients with a normal ratio. This figure was originally published in Blood and is reproduced with permission
Risk of progression of monoclonal gammopathy of undetermined significance (MGUS) to multiple myeloma based on the serum free light chain ratio. The upper curve illustrates risk of progression of monoclonal gammopathy of undetermined significance in patients with an abnormal serum kappa/lambda free light chain ratio (< 0.26 or > 1.65). The lower curve illustrates the risk of progression in patients with a normal ratio. This figure was originally published in Blood and is reproduced with permission
This work was supported in part by research grants CA 107476 and CA 62242 from the National Cancer Institute.
Acknowledgment: I am greatly indebted to Dr. Robert A. Kyle, whose studies and data are the basis of much of the findings in this paper and without whom most of this work would not have been possible.