Abstract
Treatment of acute myeloid leukemia (AML) in older adults remains a tremendous challenge. Standard approaches to treatment have resulted in progression-free survival in only a small minority of patients with AML over the age of 60. Elucidation of the molecular genetic events that contribute to the pathogenesis of AML in older patients are providing insights into mechanisms of resistance. This knowledge is also providing new opportunities to begin to refine and direct novel therapies for these heterogeneous diseases. In this case-based review, prognostic factors for treatment outcome in older adults will be covered along with discussion of a risk-based approach to potential therapeutic options, ranging from palliative care to novel therapies and reduced-intensity allogenenic transplant.
Case 1: A 69-year-old woman with a 3-month history of progressive fatigue and dyspnea with exertion is noted to have pancytopenia with a hemoglobin of 7.9 g/dL, WBC count of 2100/μL, and platelet count of 39,000/μL. A bone marrow examination reveals a hypercellular marrow (50%) for age with markedly reduced granulocytic maturation and CD34, CD117, CD13 and CD33-expressing blasts accounting for 76% of the bone marrow cells. Final diagnosis: Acute myeloid leukemia with maturation (WHO). Cytogenetic analysis reveals a normal female karyotype. The patient has a performance status of 0, with well-controlled hypertension and normal renal and hepatic function.
Case 2: An 80-year-old man with a history of adult-onset diabetes, hypertension and coronary artery disease has had a mild anemia that was noted by his internist 1 year earlier. His medical problems are stable and the patient has not seen his physician for the last 6 months. He now presents for a yearly exam and is found to be anemic with a hemoglobin of 8.9 gm/dL with platelets of 113 K/μL. WBC is 1.9/μL with 19% neutrophils. Bone marrow exam reveals AML with multilineage dysplasia (WHO) with 21% myeloblasts. Cytogenetics show del (7q), +8. Performance status is 1.
Case 3: A 63-year-old woman presents with pancytopenia during a follow-up exam 3 years after completing adjuvant therapy for breast cancer. She had a left-sided 2 cm grade 3 ER negative PR negative HER 2 negative infiltrating ductal carcinoma with 2 of 6 positive axillary lymph nodes and was treated with lumpectomy, dose-dense doxorubicin/cyclophosphamide for 4 cycles followed by dose dense paclitaxel for 4 weeks (dose-dense AC-T), then breast radiotherapy. She has been in excellent health and exercises regularly but notes several weeks of progressive fatigue and low-grade fevers. A bone marrow examination demonstrates a monocytic leukemia and cytogenetic analysis returns with a t(11;19)(q23;p13.1).
What Therapy Are You Most Likely to Recommend for These Patients?
The management of an older patient with AML, where the median age at presentation is approximately 68 years, remains a major challenge! An important initial discussion with the patient focuses on determining whether standard AML treatment, investigational therapies in the context of a clinical trial, or palliative care might be the most appropriate option. Many studies have compared the option of best supportive care with that of induction chemotherapy for older patients with AML. Prospective nonrandomized studies show trends toward improved survival when patients received chemotherapy in contrast to supportive care alone.1 This may not, however, be true for the oldest subset of patients, those 80 years of age or older, who do not appear to benefit from the standard chemotherapeutic approaches that have been employed during the last two decades.2 A standard “3 + 7” induction regimen containing an anthracycline (often daunorubicin) and cytarabine may provide some benefit to some older patients; yet, it is important to be reminded of a sobering statistic—older patients with AML, usually defined in clinical trials as above 55 or 60 years of age, have a median time from treatment with 3 + 7 regimens to death of only 5–10 months. When counseling an individual patient about treatment options, it is worthwhile to try to refine these general statements by reviewing prognostic and outcome data that exist after 25 years of employing these “standard” approaches and to look toward more novel therapeutic approaches for these challenging patients.
Outcome Data from Multicenter Trials in Older Patients with AML
Overall, approximately 45–55% of patients in this age group achieve complete remission, although the probability of remaining in remission 3 years after beginning treatment is less than 15% (Table 1 ). There is little evidence to suggest the superiority of one “standard” approach over another. The use of higher dose daunorubicin, 60 mg/m2/day × 3, significantly improves remission rates over lower dose daunorubicin and allows more patients to move forward with postremission chemotherapy; however, neither disease-free survival (DFS) nor overall survival (OS) have improved. Multicenter randomized trials have failed to convincingly demonstrate a survival advantage with any specific chemotherapy combination over another. Mitoxantrone and etoposide was not superior to the combination of daunorubicin and cytarabine.3 Nor has the use of high-dose cytarabine during induction or during postremission therapy provided any advantage over standard-dose cytarabine for patients over age 60.4 Other drugs, such as etoposide or 6-thioguanine, have been added to induction regimens with mixed results, with some improvement but have not improved DFS.5
No randomized trial has ever demonstrated that any amount of postremission, or consolidation, therapy for older patients provides better outcomes than no postremission therapy. Nevertheless, the only studies that demonstrate that long-term DFS is possible for older patients with AML have included both remission induction and postremission therapy. Therefore, it may be reasonable to administer postremission therapy consisting of a repeat of remission induction therapy, an attenuated course of this therapy (e.g., 2 days of anthracycline and 5 days of cytarabine), or single-agent cytarabine. There does not appear to be any additional benefit achieved from administering more than 1 or 2 courses of consolidation therapy.5 Similarly, the use of long-term maintenance therapy given for up to 3 years, while shown to modestly improve the median relapse-free survival to 12 months in a poor-risk group of patients that included older patients with AML,6 has not been adopted routinely.
Others have hypothesized that an attenuated regimen, or less intensive chemotherapy regimens using standard agents, might improve the outcome of older patients with AML. This has been tested in four major studies. The attenuated or oral regimens showed slight improvements in CR rate and survival over more intensive regimens, but the DFS was not improved significantly in any of the studies, and median survival for the less-attenuated dosing arms was only 12 months or less.7
The benefit of adding hematopoietic growth factors to the treatment of older patients with AML has been tested in at least nine different randomized studies.8 Studies suggest that use of growth factors is safe and almost all studies demonstrated a decrease in the time to recovery of neutrophils, but improvement in CR rate or relapse-free survival has been demonstrated in only three of these randomized trials.8
In summary, while CR rates have improved slightly over the last 25 years, changes in dose, schedule and use of a variety of combinations of known agents has not resulted in significant improvements in survival for the majority of older patients with AML.
Refining Prognosis
These survival data reflect, in part, the association between the poorer performance status of older patients with AML as compared to that of younger patients and the predominance of known adverse biologic features, including unfavorable cytogenetics, an antecedent myelodysplastic syndrome (MDS), AML with multilineage dysplasia, and expression of the multidrug resistance (MDR) mediator, P-glycoprotein.9 In a recent retrospective analysis of 968 adults treated on five recent Southwest Oncology Group trials, older patients with AML presented with poorer performance status and lower white blood cell counts with a lower percentage of blasts in the bone marrow.10 MDR was found in 33% of AML < age 56 compared with 57% in patients > age 75. Similarly, it was noted that the percentage of favorable cytogenetics dropped from 17% in patients < age 56 to 4% in those > 75 years.10 In contrast, the proportion of patients with unfavorable cytogenetics increased from 35% in those < age 56 to 51% in patients > 75 years of age. There was a striking increase in abnormalities of chromosomes 5, 7, and 17 among older adults that contributed to their poor outcome. Interestingly, within each cytogenetic risk group (favorable, intermediate, poor-risk), treatment outcome deteriorated markedly with age, a result also noted previously by others.6 In addition to these biologic risk factors, patients with a poor performance status (Zubrod 3) and age > 75 years had a particularly poor outcome, with 82% mortality within 30 days of initiation of a standard induction regimen.
Using very similar prognostic criteria of increasing age, performance status, organ function, antecedent hematologic disorder and karyotype, a predictive model was recently constructed that divides older patients into three risk groups based on another recent retrospective analysis that included 998 patients with AML or high-risk MDS age ≥ 65 years treated at a single institution between 1980 and 200411: 1) a favorable group (20% of patients) with expected CR rates above 60%, and low induction mortality of 10%, and 1-year survival rates of over 50%; 2) an intermediate group that comprised the majority of patients (50–55%) with expected CR rates of 50%, induction mortality rates of 30% and 1-year survival of about 30%; and 3) a poor-risk group comprising 25–30% of patients who would be expected to have poor CR rates of < 20%, high induction mortality rates > 50%, and 1-year survival of < 10%.
These prognostic models, both of which still require prospective validation in multi-institutional trials, provide a context for advising older patients about potential therapeutic strategies and may help clinicians to advise patients about whether they are likely to benefit from standard treatment approaches, and what the expected survival benefits may be, and may also serve as a platform for discussion of alternative therapeutic approaches.
The patients described above in Cases 1–3 have AML with characteristics that are typical of many older patients. From the historical data presented above, standard remission induction and postremission therapies are not likely to provide significant benefit for any of these patients. What alternative therapies have been tested that might improve outcome for older patients with AML? Three alternatives that have already been explored are discussed below followed by a brief discussion of novel therapies (Table 2 ).
Multidrug Resistance and Modulation
Resistance to chemotherapy in older patients with AML appears related, in part, to more frequent expression of MDR efflux mechanisms. Therefore, several studies have tested the addition of several different MDR modulators to standard chemotherapy regimens. The most promising results were obtained in a randomized phase III trial conducted by SWOG that randomized high-risk patients (relapsed/refractory, ages 18–70 years) to a high-dose cytarabine and infusional daunorubicin induction with and without cyclosporine A (CSA). They demonstrated significant improvement in DFS (34% vs 9% at 2 years) and survival (22% vs 12%) with the CSA-containing arm.12 Similar improvements in DFS were noted when CSA was added to induction chemotherapy in a randomized study confined to patients over the age of 60 years with AML that had evolved from a prior MDS.13 The Cancer and Leukemia Group B investigated induction with chemotherapy in a phase III randomized trial consisting of daunorubicin, etoposide, and cytarabine with or without the addition of a second generation MDR-modulator, PSC-833.14 This trial was confined to previously untreated patients > age 60 with AML but was discontinued because of excessive early mortality in the PSC-833 arm. Significantly more hyperbilirubinemia, stomatitis, anorexia, and esophagitis, possibly as a result of the pharmacokinetic interactions of PSC-833 with anthracycline and etoposide, were noted in patients randomized to the PSC-833–containing arm of the study. Despite the excessive toxicities, there were hints that this approach might be worth exploring with less toxic regimens. Although the number of patients was limited, patients randomized to the control arm (without PSC-833) whose pretreatment cells demonstrated PSC-modulated drug efflux had worse outcomes in comparison to those without efflux, while DFS was similar in both groups (those with and without PSC-modulated efflux) when PSC-833 was added to the chemotherapy regimen. Alternative MDR-modulators are currently in clinical trials. LY335979, or Zosuquidar, a third-generation modulator that is highly specific for Pgp and seems to have only modest effects on drug clearance (in contrast to PSC-833), has recently been tested in combination with chemotherapy in a randomized phase III trial for older patients with AML by the Eastern Cooperative Oncology Group (ECOG). The trial was completed successfully and outcome analysis is underway.
AntibodyTherapy
Gemtuzumab ozogamicin (GO) is a calicheamicin conjugated monoclonal antibody directed against the CD33 epitope that is expressed on leukemic blasts in the majority of patients with AML. The efficacy of this antibody was established in a phase II trial of patients with relapsed AML.15 There have now been a few trials employing this agent as frontline therapy for frail older patients with AML who do not benefit from standard approaches, as reviewed above. In two recently published trials GO was administered as a single agent at a dose of 9 mg/m2/dose or in combination with interleukin 11. Unfortunately, toxicity was significant and response rates were inferior to those seen with standard chemotherapy.16,17 Therefore, there is little to recommend GO when used at the standard dose/schedule for high-risk older patients with AML. The feasibility of combining lower doses of GO (3 mg/m2) with standard chemotherapy induction in frontline therapy of AML has been demonstrated for patients under the age of 60.18 In this trial, a promising CR rate of 91% was achieved. Several large randomized studies are now being performed by the cooperative groups in the United Kingdom, Europe and in the US that explore this approach with the addition of lower doses of GO to standard frontline therapies (either during remission induction or as postremission therapy) in untreated eligible patients over the age of 55–60 years.
Hematopoietic Stem Cell Transplantation
An alternative approach to postremission therapy for older patients explores the role of allogeneic stem cell transplantation. Allogeneic hematopoietic stem cell transplant (HSCT) using reduced-intensity conditioning regimens attempts to maintain the advantage of a graft-versus-leukemia effect while minimizing the toxicity of a fully ablative regimen.2 Preliminary studies have demonstrated that durable complete remissions may be maintained with this treatment. One example is a recently published multicenter trial where low-dose (2 Gy) total body irradiation and fludarabine was used for the preparative regimen with cyclosporine and mycophenolate mofetil for graft-versus-host disease (GVHD) prophylaxis in 122 high-risk AML patients where the median age was 57.5 years.19 Among a subset of these patients, 9 of 14 patients ≥ age 60 (range, 60–74 years) had durable responses. While GVHD remains a significant problem with this preparative regimen, clinical outcomes were encouraging. Among patients transplanted in CR1, the 2-year overall survival was 44% after HLA-related and 63% after HLA-unrelated HSCT, suggesting a stronger graft-versus-leukemia effect of the unrelated allogeneic graft. Overall, with a median follow-up of 417 days, transplant-related mortality was only 6.7%. In another study examining reduced-intensity HSCT in 26 older patients (median age, 60) with therapy-related AML or AML evolving from antecedent MDS, a treosulfan and fludarabine preparative regimen was used. Acute GVHD was noted in 35% of patients (grades I – III) and treatment-related mortality at day 100 was 28%. The 2-year estimated overall survival was 36% with no differences noted between unrelated and related HSCT.20 These studies suggest the possibility of improved outcomes for older adults with AML when allogeneic HSCT is performed in first remission; however, treatment-related mortality remains a significant concern in these high-risk patients. It is also important to be cognizant that even modest decreases in performance status are associated with poor outcomes when using reduced-intensity conditioning regimens21 and that careful pretransplant evaluation and counseling of the older patient using objective assessment parameters is essential. These promising early data have prompted the US cooperative groups to explore the role of HSCT in older AML patients in CR1.
Since these trials demonstrate feasibility of transplant for older patients up to age 70–72 years, investigators have taken an even more dramatic step. A recently published trial22 has demonstrated that it is possible to use allogeneic stem cell transplant with a reduced-intensity conditioning regimen as the initial treatment for high-risk patients with newly diagnosed AML. These transplants were performed a median of 40 days (range: 22–74 days) after diagnosis using a fludarabine-based conditioning regimen that was started following cytoreductive AML induction chemotherapy (while patients were still cytopenic) and as soon as a donor (either related or unrelated) was identified. In this small pilot study of 26 patients, after a median follow-up of 22 months, DFS was estimated at 61%. The success of this approach has led to the randomized testing of this concept in a multicenter German trial in which patients with high-risk AML defined by karyotype, FLT-3 ITD status and blast clearance in response to the first cycle of induction chemotherapy are randomized to receive either an up-front allogeneic HSCT or transplantation performed after 2–3 cycles of chemotherapy with normal hematopoietic reconstitution.
NovelTherapeutic Approaches to Target the Leukemia Stem Cell
As discussed above, despite a small long-term survival benefit for standard chemotherapy approaches for good-risk patients, it is very reasonable to consider the use of investigational agents as initial therapy for older patients with AML. As noted by the SWOG investigators, older patients with AML typically have less proliferative disease that may not be as susceptible to S-phase specific cytotoxics, such as cytarabine or anthracyclines. Several new agents may have a specific role for older patients with AML based on efforts to target the leukemic “stem cell”23 in this heterogeneous subset of patients. Two of these agents are currently being tested in frontline therapy for older adults with AML. Overexpression of the anti-apoptotic protein, Bcl-2, has been noted in AML blasts and may be another mechanism of chemotherapy resistance. Compelling laboratory data and phase I clinical experience have demonstrated potential synergism between chemotherapy and oblimersen (a Bcl-2 antisense oligonucleotide).24 Consequently, the CALGB is currently exploring the use of oblimersen in combination with standard induction and postremission therapy in a randomized phase III trial of previously untreated AML patients > age 60. Activating mutations of RAS family members, including KIT and FLT3, may also provide a survival advantage to leukemic blasts and are relevant targets for AML therapy in older patients that are being explored (see reviews by Drs. Bloomfield and Small in this volume). Zarnestra, a farnesyl transferase inhibitor initially developed to target activation of the RAS pathway in AML and other malignancies, was shown to induce complete responses in 20% of chemotherapy-naïve high-risk, largely older patients with AML.25 Based on these encouraging results of this preliminary report, the efficacy of this agent has recently been tested as frontline therapy for AML patients > 70 years old in a US intergroup study. The study is now closed to accrual and outcome results are pending.
Several other approaches are being tested with the goal of improving outcome for older patients with AML and are beginning to work their way forward to frontline therapy. A novel alkylating agent, cloretazine, has recently been shown to have efficacy in untreated older patients with poor-risk de novo AML, resulting in a 49% CR rate and DFS at 1 year of 27%.26 A confirmatory phase II trial of induction therapy with single-agent cloretazine in high-risk older AML patients > age 70 has recently been initiated. Clofarabine, a purine nucleoside that was recently approved for use in relapsed pediatric ALL, also has activity in AML. Clofarabine can be combined safely with other agents including cytarabine. A recently reported phase II study that tested clofarabine in combination with cytarabine demonstrated an overall response rate of 60% in chemotherapy-naïve, high-risk AML patients > age 50.27 Based on this promising response rate, the ECOG is initiating a randomized phase III trial testing single-agent clofarabine compared to standard chemotherapy with daunorucibin and cytarabine in frontline therapy for older patients. A block in differentiation that results from epigenetic modifications such as hypermethylation and/or histone deacetylation may provide other relevant targets for therapy.28 The hypomethylating agents, 5-azacytidine or 2-deoxy-5-azacytidine, both approved for treatment of MDS, are being tested in combination with a variety of histone deacetylase inhibitors for patients with relapsed AML and have demonstrated activity in patients with relapsed disease.29 Several combinations are currently being tested in frail or high-risk patients not eligible for standard induction therapy. Synergistic activity of chemotherapy with Bortezomib, a proteasome inhibitor that appears to target constitutively active NF-κB in leukemia stem cells,30 has spurred the clinical development of this agent in chemotherapy combinations for relapsed AML.31 Finally, immunologic approaches other than allogeneic stem cell transplantation are being examined. Currently, two trials in the US are in planning stages that will test the potential efficacy of vaccine therapy in older patients with AML in first remission. The vaccines target epitopes expressed in AML cells and have been shown to induce T cell responses in patients with AML, with some preliminary data to suggest that T-cell responses correlate with eradication of minimal residual disease.32,33
How Do We Choose Treatment Today?
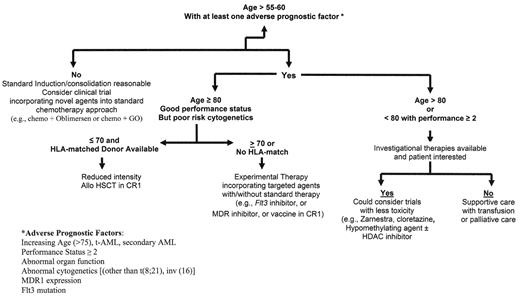
As mentioned previously, the patients described in the three cases at the beginning of this section are each very different from one another, but none of them is likely to benefit significantly from a standard approach to treatment. A potential treatment algorithm for guiding therapeutic approach in 2006 is outlined in Figure 1 . The patient in Case 1 has the most favorable prognosis of the three cases. However, even this relatively “favorable-risk” patient has a predicted median survival of 12 months with standard therapies, using the SWOG prognostic data. Therefore, although one could consider standard induction and consolidation, it might be preferable to offer this patient a clinical trial that is evaluating novel agents (MDR inhibitors, Bcl-2 inhibitors) in combination with standard therapies as discussed above and summarized in Table 2 . A slightly different consideration is treatment of the rare older adult with AML and a favorable karyotype such as those involving core binding factor (CBF) transcription factors, the inv(16) or t(8;21), who comprise only 4–17% of patients over age 55 in the SWOG report. Data suggest that these favorable-risk patients do more poorly than their younger counterparts (age < 60) with standard therapy. One potential explanation for this poorer outcome is the hesitation to use high-dose cytarabine during consolidation therapy, which is currently the standard of care for younger patients with these CBF leukemias,34 due to increased incidence of neurologic and other toxicities in older AML patients. In these cases, in patients with good performance status and normal renal function, it might be reasonable to consider careful administration of higher-dose cytarabine during consolidation therapy.
For the older, “older” adult with AML in Case 2, prognostic models suggest that this patient who is 80 years old is likely to have a high induction mortality rate of over 50% that might preclude consideration of standard approaches to treatment. Transfusion support or palliative care options are reasonable considerations; however, if this patient is interested in considering active therapy, one might offer a less intensive induction approach as has recently been tested by the US intergroup by examining Zarnestra as frontline therapy for patients over age 70. Since this patient has a low percentage of marrow blasts and evidence of trilineage dysplasia, trials that are examining hypomethylating agents in combination with histone deacetylase inhibitors could also be considered. The patient in case 3 has t-AML and an excellent performance status. The possibility of attaining prolonged DFS might be achieved with reduced intensity allogeneic transplant approaches in CR1 or after cytoreductive induction as outlined above.
As the insights into disease pathogenesis continue to expand, the therapeutic options for these older patients who comprise the majority of AML cases will increase rapidly. It will be critical to evaluate each case comprehensively with careful clinical workup, and detailed molecular cytogenetic analysis as we move forward with subset-specific therapies to try to improve outcomes for these heterogeneous diseases.
Selected large multicenter trials of older patients with acute myeloid leukemia (AML).
| Publications . | Age . | No of Pts . | CR % . | CCR at 4–5 yrs % . | Comments . |
|---|---|---|---|---|---|
| Abbreviations: TG, thioguanine; DFS, disease-free survival; ara-C, cytarabine; GM-CSF, granulocyte-macrophage colony-stimulating factor; CR, complete response | |||||
| Goldstone et al, 20015 | 56–80 | 1311 | 50–62 | 15–18 | 6-TG added to induction superior to etoposide (p = 0.002). No benefit from more than 1–2 courses of consolidation. |
| Lowenberg et al,199835 | 60–88 | 489 | 38–47 | 7–13 | Mitoxantrone-containing induction regimen resulted in a slightly higher CR rate over daunorubicin-containing induction but had no significant effect on DFS or survival benefit to ara-C maintenance |
| Rowe et al, 200436 | 56–86 | 362 | 42 | 4 | No difference in disease-free survival using idarubicin, mitoxantrone, or daunorubicin during induction. Priming with GM-CSF did not improve response rate. |
| Stone et al, 199538 | >60 | 388 | 53 | 13 | Shorter duration of neutropenia in patients randomized to GM-CSF vs. placebo (p = 0.02) but no difference in life-threatening infections or response rate. |
| Godwin et al, 199837 | 56–88 | 234 | 45 | Not given | G-CSF reduced time to neutrophil recovery (compared to placebo) but did not improve CR rate, survival, or hospitalization days |
| Mayer et al, 19944 | 60–86 | 346 | 47 | 16 | Intensification of cytarabine dose during post-remission therapy did not improve outcome. |
| Buchner et al, 20036 | 60–82 | 297 | 60 | 13 | Prolonged maintenance therapy resulted in modest improvements in relapse-free survival for poor-risk patients. |
| Publications . | Age . | No of Pts . | CR % . | CCR at 4–5 yrs % . | Comments . |
|---|---|---|---|---|---|
| Abbreviations: TG, thioguanine; DFS, disease-free survival; ara-C, cytarabine; GM-CSF, granulocyte-macrophage colony-stimulating factor; CR, complete response | |||||
| Goldstone et al, 20015 | 56–80 | 1311 | 50–62 | 15–18 | 6-TG added to induction superior to etoposide (p = 0.002). No benefit from more than 1–2 courses of consolidation. |
| Lowenberg et al,199835 | 60–88 | 489 | 38–47 | 7–13 | Mitoxantrone-containing induction regimen resulted in a slightly higher CR rate over daunorubicin-containing induction but had no significant effect on DFS or survival benefit to ara-C maintenance |
| Rowe et al, 200436 | 56–86 | 362 | 42 | 4 | No difference in disease-free survival using idarubicin, mitoxantrone, or daunorubicin during induction. Priming with GM-CSF did not improve response rate. |
| Stone et al, 199538 | >60 | 388 | 53 | 13 | Shorter duration of neutropenia in patients randomized to GM-CSF vs. placebo (p = 0.02) but no difference in life-threatening infections or response rate. |
| Godwin et al, 199837 | 56–88 | 234 | 45 | Not given | G-CSF reduced time to neutrophil recovery (compared to placebo) but did not improve CR rate, survival, or hospitalization days |
| Mayer et al, 19944 | 60–86 | 346 | 47 | 16 | Intensification of cytarabine dose during post-remission therapy did not improve outcome. |
| Buchner et al, 20036 | 60–82 | 297 | 60 | 13 | Prolonged maintenance therapy resulted in modest improvements in relapse-free survival for poor-risk patients. |
Selected ongoing or recently completed trials for untreated older patients with acute myeloid leukemia (AML).
| Group . | Age . | Trial . |
|---|---|---|
| CALGB | >60 | Randomized Phase III Trial Comparing Daunorubicin/Ara-C With or Without Oblimersen (bcl-2 antisense) |
| ECOG | >60 | Randomized Phase III Trial Comparing Daunorubicin/Ara-C with or Without L4335979 (MDR Modulator, Zosuquidar) |
| SWOG | >55 | Randomized Phase III Trial Comparing Continuous Infusion Daunorubicin/Ara-C With or Without Cyclosporine A (MDR Modulator) Followed by Assignment to Reduced Intensity Allogeneic HSCT (if HLA-matched Donor) |
| EORTC | >60 | Randomized Phase III Trial Comparing Idarubicin/Ara-C With or Without Gemtuzumab Ozogomycin (conjugated anti-CD33 with Calicheamycin) |
| HOVON | >60 | Randomized Trial comparing Different Doses of Daunorubicin/Ara-C Induction and Consolidation Followed by Gemtuzumab Ozogomycin Maintenance versus Observation |
| MRC | >60 | Comparison of Intensive Chemo (Daunorubicin/Ara-C at various doses) versus Non-Intensive Chemo (Hydroxyurea/low dose Cytarabine ± ATRA) |
| US Intergroup | >60 | Phase II Study comparing two different schedules and doses of the farnesyl transferase inhibitor, R115777 (Tipifarnib, Zarnestra) |
| Group . | Age . | Trial . |
|---|---|---|
| CALGB | >60 | Randomized Phase III Trial Comparing Daunorubicin/Ara-C With or Without Oblimersen (bcl-2 antisense) |
| ECOG | >60 | Randomized Phase III Trial Comparing Daunorubicin/Ara-C with or Without L4335979 (MDR Modulator, Zosuquidar) |
| SWOG | >55 | Randomized Phase III Trial Comparing Continuous Infusion Daunorubicin/Ara-C With or Without Cyclosporine A (MDR Modulator) Followed by Assignment to Reduced Intensity Allogeneic HSCT (if HLA-matched Donor) |
| EORTC | >60 | Randomized Phase III Trial Comparing Idarubicin/Ara-C With or Without Gemtuzumab Ozogomycin (conjugated anti-CD33 with Calicheamycin) |
| HOVON | >60 | Randomized Trial comparing Different Doses of Daunorubicin/Ara-C Induction and Consolidation Followed by Gemtuzumab Ozogomycin Maintenance versus Observation |
| MRC | >60 | Comparison of Intensive Chemo (Daunorubicin/Ara-C at various doses) versus Non-Intensive Chemo (Hydroxyurea/low dose Cytarabine ± ATRA) |
| US Intergroup | >60 | Phase II Study comparing two different schedules and doses of the farnesyl transferase inhibitor, R115777 (Tipifarnib, Zarnestra) |
Algorithm for approach to treatment of the older patient with untreated acute myeloid leukemia (AML).
Algorithm for approach to treatment of the older patient with untreated acute myeloid leukemia (AML).