Abstract
A 62-year-old woman with chronic lymphocytic leukemia (CLL) who initially presented with lymphocytosis and 13q deletion in 1996 now presents to the clinic for recommendations regarding relapsed disease. The patient has received multiple prior therapies, including single-agent fludarabine, fludarabine and rituximab, and bendamustine and rituximab. She now has recurrent lymphocytosis with a WBC count that has increased from 13 000 2 months ago to 115 000 today and a platelet count of 55 000 but no lymphadenopathy. In addition, your evaluation finds that she has acquired a 17p deletion.
Introduction
Alemtuzumab is a humanized mAb that targets the cell-surface marker CD52. The function of CD52 is unknown, but it is highly expressed on the surface of both healthy B and T lymphocytes and chronic lymphocytic leukemia (CLL) cells.1 Whereas the exact mechanism of alemtuzumab activity continues to be elucidated, evidence suggests that it acts both by antibody-dependent cellular cytotoxicity and by promoting complement-mediated cytotoxicity.2 In 2001, alemtuzumab was granted accelerated US Food and Drug Administration (FDA) approval for CLL refractory to fludarabine and exposed to alkylator on the basis of a phase 2 study.3 A subsequent randomized phase 3 trial demonstrated an improved response rate and progression-free survival for alemtuzumab compared with chlorambucil as a first-line treatment for CLL.4 This trial led to full FDA approval and an expanded indication in September 2007. Despite the success of alemtuzumab in clinical trials and its FDA approval, alemtuzumab is not widely used outside of CLL specialty centers. This review discusses the data on the use of single-agent alemtuzumab in patients with relapsed and refractory CLL, with a focus on indications for use and infectious complications.
To determine the available literature, we performed a search using the PubMed medical subject heading (MeSH) terms “chronic lymphocytic leukemia” (9736 publications) and “alemtuzumab” (1018 publications) with the key words “relapsed” or “refractory.” We limited the search to clinical trials on humans in English. This combination resulted in 22 publications. Six of these publications were prospective, phase 2, single-arm trials looking at single-agent alemtuzumab in CLL3,5–9 and were the ones analyzed in this review. The remaining papers were excluded: 4 trials investigating alemtuzumab in combination with other agents, 4 pilot studies, 3 studies on the biology of alemtuzumab, 4 maintenance or consolidation trials, and 1 retrospective trial. An additional prospective phase 2 trial was found through the bibliographies of the above papers.10
This series of clinical trials has demonstrated the efficacy of alemtuzumab in patients with CLL that is either relapsed (initial response that persists greater than 6 months after prior therapy) or refractory (no response or progression within 6 months of prior therapy) to fludarabine and/or alkylating agents (Table 1).3,5–10 Several interesting observations were made in the first phase 2 trial of alemtuzumab in CLL.5 The overall response rate (42%) was comparable to historical responses to fludarabine and cladribine in relapsed patients. A high percentage of patients (97%) were found to have a complete response in circulating disease. This response was less dramatic in BM (36%) and spleen (32%) and significantly less so in lymph nodes (7%). Furthermore, the response rate was comparable in patients with disease refractory to alkylating agents (43%) and in those with relapsed disease (38%), suggesting a distinct mode of action compared with traditional chemotherapy. Subsequent trials with IV alemtuzumab have demonstrated similar response rates (overall response rate, 23%-33%).3,6,10 These trials also found that alemtuzumab was more likely to induce response in circulating disease (75%-97%)3,5,6 and BM (26%-38%)3,5,10 than in lymph nodes larger than 5 cm (0%-27%).3,5,10
Clinical trials demonstrating the efficacy of alemtuzumab in patients with CLL that was either relapsed or refractory to fludarabine and/or alkylating agents
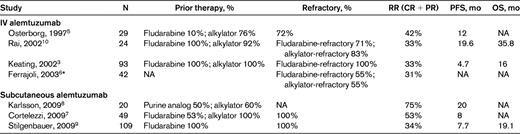
RR indicates response rate; CR, complete remission; PR, partial remission; PFS, progression-free survival; OS, overall survival; NA, not applicable.
*Study included CLL, prolymphocytic leukemia, and other chronic lymphoproliferative disorders; response rate is for CLL.
Based on the success of the initial trials using IV alemtuzumab and on the severity of infusion reactions associated with IV administration, a series of phase 2 trials with subcutaneous alemtuzumab were performed.7–9 Overall response rates in these 3 trials (34%-75%) were similar to or somewhat better than those with IV administration. It is notable that the significantly higher response rate of 75% was seen in a population that did not include any patients with lymph nodes larger than 5 cm.8 This result is consistent with prior data suggesting that alemtuzumab activity is limited in lymph nodes. Two studies looked at fludarabine-refractory patients only and had similar response rates (34%-53%) to trials that included both refractory and relapsed patients.7,9 This equivalent activity of alemtuzumab in purine analog–refractory patients suggested that alemtuzumab might also have good activity in those patients with high-risk cytogenetics. This was observed for those with 17p deletions in one study, and the patients had a comparable response rate to the overall group (60% vs 53.1%).7 A second study found that patients with 17p and 11q deletions had a similar overall survival relative to patients without those deletions (18.3 months vs 22.7 vs 18.6 months, respectively),9 again suggesting that alemtuzumab has activity in this difficult patient group for whom most standard therapeutic options have very limited activity.11
Concern about infectious complications has contributed to the limited use of alemtuzumab. In the initial phase 2 trial, opportunistic infectious complications were significant, with 38% of patients developing HSV reactivation, 20% developing pneumonia, and 13% developing oral candidiasis; CMV reactivation was not commented on.5 The infection rate in a second study was again significant, with 42% of patients developing an opportunistic infection and 33% of patients developing pneumonia.10 In a third trial, the mandatory administration of trimethoprim sulfamethoxazole and antiviral prophylaxis decreased the rate of opportunistic infections to 19% during and for 6 months after the administration of alemtuzumab.3 Whereas all 3 of the subcutaneous trials mandated pneumocystis and viral prophylaxis, infections continued to be a significant side effect (grade 3 or 4 infections, 20%-29%; CMV reactivation, 24%-30%),7–9 although they were similar to previously described rates of infection in heavily pretreated, high-stage CLL.12 We agree with current management guidelines, which suggest both pneumocystis and viral prophylaxis during therapy with alemtuzumab and for 6 months after completing therapy, as well as weekly monitoring for CMV reactivation with initiation of therapy at first signs of reactivation.13 Additionally, patients should be managed with myeloid growth factors to avoid neutropenia.7,8 Based on the experience in the above trials, we recommend (grade 1B) the above strategy to decrease infectious complications.
Alemtuzumab is an approved single-agent therapy for CLL. The accumulation of data from clinical trials suggests that alemtuzumab is particularly appropriate for patients with disease relapsed after or refractory to alkylating agents and/or purine analogs, who have minimal nodal disease, and who may have 17p or 11q deletions. Whereas infectious complications continue to be significant, they are decreased and generally manageable with appropriate prophylaxis. Based on this review, we recommend (grade 1B) the use of alemtuzumab in patients with relapsed or refractory CLL without significant lymphadenopathy, particularly those with 17p or 11q deletions. Based on our findings, the above patient, with multiply pretreated, non-nodal-recurrent disease with a 17p deletion, is an ideal candidate for alemtuzumab therapy.
Disclosures
Conflict-of-interest disclosure: J.A. declares no competing financial interests. J.B. has consulted for Calistoga; has received honoraria from Celgene; and has received research funding from Calistoga, Celgene, Genzyme, and GSK. Off-label drug use: Alemtuzumab given subcutaneously.
Correspondence
Jon Arnason, BIDMC 330 Brookline Avenue, KS 121, Boston, MA 02215, Phone: (617) 667-9235; Fax: (617) 667-9922; e-mail: jarnason@bidmc.harvard.edu.
