Abstract
The recognition of that patients with Immune Thrombocytopenia (ITP) have functional thrombopoietin deficiency and decreased platelet production due to immune-mediated megakaryocytic injury has challenged the traditional view of this disease as predominantly a disorder of antibody-mediated platelet destruction. The therapy of chronic refractory ITP has been transformed by the approval of the thrombopoietin minetics, romiplostim and eltrombopag, which have shown remarkable efficacy in randomized trials. The use of these agents earlier in the disease course after failure of corticosteroid therapy remains controversial. In this article, we review the current data on the efficacy and safety of thrombopoietin receptor agonists and discuss other therapies as well as diagnostic work up of ITP.
Introduction
Immune thrombocytopenia (ITP) is a heterogeneous autoimmune disorder characterized by thrombocytopenia with or without mucocutaneous bleeding manifestations. Because of its complex pathophysiology and its association with a variety of other disorders, ITP is best characterized as a syndrome sharing the common clinical phenotype of immune-mediated thrombocytopenia.1
Definition and epidemiology
ITP is an acquired disorder characterized by isolated thrombocytopenia with a peripheral blood platelet count < 100 × 109/L in the absence of any obvious initiating or underlying cause.2 Therefore, the diagnosis of ITP is one of exclusion and is based principally on patient history, physical examination, complete blood count, and review of the peripheral blood smear.3
The recent ITP international working group consensus report has divided the disorder into three phases: newly diagnosed ITP (≤ 3 months), persistent ITP (3 months-1 year), and chronic ITP (> 1 year).2 ITP can be further characterized as being either primary (idiopathic) or secondary to several associated disorders such as immunodeficiency diseases, autoimmune-rheumatologic disorders, lymphoproliferative diseases, and certain chronic infections.2 It is estimated that ∼ 20% of ITP cases in the United States are secondary to other disorders.1 However, the incidence of secondary ITP worldwide may vary greatly, particularly in populations with a high incidence of HIV, hepatitis C, or Helicobacter pylori infection.
The incidence of newly diagnosed ITP in adults ranges from 1.6-3.9 per 100 000 persons per year.4 Recent studies have found an increased incidence and prevalence with advancing age.4 The female-to-male ratio ranges from 1.2-1.9, with the female predominance more evident among young to middle-age adults.4
Diagnostic approach to patients with suspected ITP
A presumptive diagnosis of ITP is made by a careful history, physical examination, complete blood count, and review of the blood smear.3,5 Response to initial treatment with corticosteroids, intravenous immunoglobulin (IVIg), or anti-RhD supports the diagnosis and confirms the immune nature of the thrombocytopenia. However, additional investigation is necessary to exclude secondary ITP and to provide additional information to assist with patient management.
A complete blood count should reveal isolated thrombocytopenia with normal white and red blood cell numbers. Anemia may exist if there has been significant acute or chronic blood loss or concomitant immune hemolytic anemia (Evan syndrome). A careful review of the peripheral blood smear is mandatory to exclude other causes of thrombocytopenia. Abnormalities in erythrocyte or leukocyte morphology may suggest an underlying BM disorder such as myelodysplastic syndrome or a congenital cause of thrombocytopenia. The presence of a MYH9-related disorder may be suggested by leukocyte inclusion bodies. Many congenital thrombocytopenic disorders are associated with very large platelets (macrothrombocytopenia), which may also be reflected in an abnormally high mean platelet volume. Increased numbers of small lymphocytes or lymphocytes with granular inclusions may suggest a diagnosis of chronic lymphocytic leukemia or large granular lymphocytic leukemia with secondary ITP. Pseudo-thrombocytopenia due to platelet clumping should be excluded, and if platelet clumping is seen on the blood smear, a repeat platelet count using a blood sample collected in citrate or heparin rather than EDTA should be performed. Thrombocytopenia resulting from thrombotic thrombocytopenic purpura or hemolytic uremic syndrome must be considered if the blood smear shows significant numbers of schistocytes.
The international working group on ITP recommended several additional laboratory tests to further assist in the diagnosis and management of patients with primary ITP5 (Table 1). BM examination has been recommended in patients refractory to ITP therapy or in those who relapse after an initial remission, patients with systemic symptoms or atypical physical findings, and patients before splenectomy.5 A BM aspirate and biopsy should be performed in patients older than 60 years and should include cytogenetic studies and flow cytometry.5
International ITP Working Group consensus recommendations for the diagnosis of ITP in children and adults
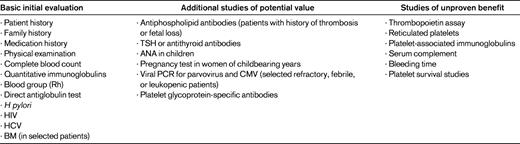
(Adapted with permission from Provan et al.5 )
HCV indicates hepatitis C virus; TSH, thyroid-stimulating hormone; and ANA, antinuclear antibody.
Clinical presentation and natural history of ITP in adults
Adult patients with ITP are more likely to manifest disease with a chronic course. Overall, ∼15% of patients remit within 1 year after disease onset, but rare late remissions occur, even among patients who have failed splenectomy.6,7 Bleeding manifestations are the most common presenting symptoms in patients with ITP, but the increased use of automated blood counts results in the frequent identification of asymptomatic patients or patients with minimal bleeding. Therefore, it is uncertain whether there is a period of mild to moderate thrombocytopenia in adults before the development of severe thrombocytopenia with bleeding. In a study of 217 healthy subjects with incidentally discovered thrombocytopenia and platelet counts between 100 × 109/L and 150 × 109/L, the 10-year probability of developing ITP as defined by platelet counts < 100 × 109/L was 6.9% (95% confidence interval: 4.0%-12.0%). The 10-year probability of developing autoimmune disorders other than ITP was 12% (95% confidence interval: 6.9%-20.8%).8
Mucocutaneous bleeding, including petechiae, purpura, epistaxis, and gum bleeding, is the most common initial manifestation of ITP. Complications of internal bleeding or fatal intracranial hemorrhage are rare and more often occur in older individuals with additional comorbidities.6,7 Symptomatic bleeding is to a degree related to the platelet count, with nearly all major bleeding occurring with platelet counts < 30 × 109/L. Only in patients with hepatitis C–related thrombocytopenia does major bleeding appear to occur with some frequency at higher platelet counts.9
The risk of bleeding and fatal hemorrhage in adults with severe chronic ITP, defined as a platelet count of < 30 × 109/L at least 1 year after diagnosis, was analyzed in a pooled analysis of published clinical series comprising 1800 patients.10 The annual incidence of fatal hemorrhage was 1.6-3.9 cases per 100 patient years, with a lower risk in patients < 40 years of age (0.4% per year) compared with patients > 60 years of age (13% per year).10 The risk of nonfatal hemorrhage was estimated to be 3% per year in patients < 40 years of age and 71% per year for patients > 60 years of age. However, it should be noted that this case series dated from 1954 to 1991 and therefore did not include patients treated with newer agents (eg, rituximab and thrombopoietin [TPO] receptor agonists) or managed with laparoscopic splenectomy.
Clinical presentation and natural history of ITP in children
The peak age of presentation of ITP in children is between 5 and 6 years, with 70% of cases presenting between ages of 1 and 10 years.11 Approximately 50%-60% of children will have a febrile illness that preceded the discovery of thrombocytopenia. Numerous viral infections, including rubella, varicella, mumps, rubeola, and EBV, as well as immunizations with measles-mumps-rubella vaccine, have been associated with the subsequent development of ITP in children.1,11,12
Signs of mucocutaneous bleeding most often occur without other systemic symptoms, and the child frequently does not appear ill.12 Bleeding manifestations vary from little or none to the typical findings of purpura, petechiae, epistaxis, and menorrhagia in older females.12 Most children present with platelet counts < 20 × 109/L.13 In a study of 863 children with newly diagnosed ITP, none or mild bleeding manifestations were reported in 77% of patients, moderate bleeding occurred in 20%, and severe bleeding in 3%.13 Life-threatening bleeding is rare and the estimated risk of intracranial hemorrhage is between 0.1% and 0.5% in newly diagnosed cases.11–13 Approximately 65%-70% of children remit by 6 months and another 15%-20% by 12 months.11,12 The 5%-10% of children who develop chronic ITP tend to be older, are more often female, and usually present with a higher platelet count.12
Pathophysiology of ITP
Assays specific for auto-antibodies directed against specific platelet-specific glycoproteins can detect antibodies in 40%-80% of patients with clinical ITP.14 However, the absence of detectable antibodies does not rule out a diagnosis of ITP, because many patients without detectable antibodies respond to traditional ITP therapies, and antibodies may occur in patients with liver disease and other conditions without clinical ITP. The antigenic target for these antiplatelet auto-antibodies are the ubiquitous platelet glycoproteins such as platelet GPIIb/IIIa in nearly 2/3 of patients, platelet GPIb/IX in approximately 1/5 of patients, and in the remaining patients, antibodies are directed against both of these platelet glycoprotein complexes or other platelet antigens.
Dendritic cells from patients with ITP have up-regulated costimulatory molecules enhancing auto-reactive T- and B-cell responses against platelets.15 The ongoing process of macrophage-mediated platelet destruction and further presentation of new platelet proteins to T and B lymphocytes contributes to the epitope spreading observed over time in patients with ITP, and may contribute to a more refractory disease in patients with ITP of longer duration.1
ITP patients may have significant defects in immune self-tolerance.1,15 Autoreactive cytotoxic CD8-expressing T-lymphocyte clones capable of directly damaging platelets and possibly megakaryocytes have also been demonstrated16 and are likely to proliferate under the influence of similar Th lymphocytes. Quantitative and qualitative defects in the regulatory T-cell population appear to be correlated with persistence of chronic ITP. An association between an improvement in the peripheral blood regulatory T-cell number and function and remission induction with ITP treatment has also been reported.15
Suppression of platelet production
Using indium-111–labeled autologous platelets, investigators have found evidence not only of increased platelet clearance, but also of impaired platelet production.17,18 Recent studies have demonstrated inhibition of in vitro megakaryocyte growth and maturation by antibodies from some ITP patients.19 Evidence that patients with ITP have autoreactive cytotoxic thymic (T) lymphocytes capable of directly lysing platelets suggests that these lymphocytes may also induce megakaryocyte injury and contribute to defective platelet production.16 Whereas megakaryocyte numbers and appearance in BM specimens appear normal in most patients with ITP when viewed under light microscopy, electron microscopic studies of BM from ITP patients show extensive damage in the majority of megakaryocytes.20
TPO is the major physiologic regulator of megakaryocyte growth and differentiation.21,22 It is synthesized and secreted by the liver, and its production is constant, with no translational or posttranslational regulation.21 When TPO is released into the circulation, most of the protein binds to TPO receptors on platelets and is cleared, with the platelets with the remaining TPO binding to receptors on BM precursors.21 TPO levels are inappropriately low for the degree of thrombocytopenia in the majority of patients with ITP, and this observation provided the theoretical basis for treatment with TPO-receptor agonists.21,23
Management of primary ITP in adults
Several factors, including bleeding risk, toxicities of specific therapies, patient age and comorbidities, and patient preference and lifestyle, must be considered before treatment is initiated in adults with primary ITP.5 For children with ITP, when treatment is given, it is initially aimed at rapidly increasing the platelet count to a safe level, then maintaining an adequate and safe count while awaiting a spontaneous remission. For adults, most of whom will have chronic ITP, therapies are used to increase the platelet count to a safe level and/or to prevent further bleeding with minimal toxicities. Maintenance of a platelet count > 30 × 109/L is an appropriate goal. Treatment should be considered when the platelet count is < 20-30 × 109/L, but occasionally it is appropriate to select a higher target count.5 For secondary ITP, treating the underlying disease is usually the preferred approach.
Corticosteroid therapy
Corticosteroids are the standard initial therapeutic agents5 and those used most frequently include prednisone, parenteral methylprednisolone, and dexamethasone. These are frequently used in combination with IVIg and IV anti-RhD to rapidly increase platelet counts in patients with significant thrombocytopenia (< 5 × 109/L) and extensive bleeding manifestations.5
Prednisone is the steroid most frequently used in the treatment of ITP, and is given orally at a dose of 0.5-2 mg/kg daily. In responders, the platelet count will increase to > 50 × 109/L in a few days to several weeks, depending upon the baseline platelet count and whether IVIg or anti-RhD is used in conjunction with the drug. Bleeding may cease before an increase in the platelet count is seen. When used alone, 65%-70% of patients respond.5,24,25 Responses in adults are rarely durable, with only 13%-17% of patients having an unmaintained normal platelet count at 1 year after treatment with prednisone alone.5,24,25
Early studies on the use of high-dose dexamethasone for the treatment of refractory ITP were abandoned due to significant toxicity and marginal efficacy.26 More recently, a study of a single course of high-dose dexamethasone (40 mg/d × 4 days) in newly diagnosed patients reported a high initial response (85%), with half of the responding patients maintaining their response at 6 months.27 A multicenter trial of dexamethasone (40 mg/d × 4 days) repeated every 14 days for 4 courses produced an 86% response rate (platelet count, > 50 × 109/L) and a 65% complete response rate (platelet count > 100 × 109/L).28 At a 15-month median follow-up, 60% of responding adults had not relapsed, and for both adults and children who obtained a complete response, 87% remained in remission.28 However, a recently reported randomized trial comparing 1 or 2 cycles of the high-dose dexamethasone to 1 mg/kg prednisolone failed to demonstrate superiority of the dexamethasone regimen.29 Additional studies will be needed to prove that this approach provides superior long-term benefit.
IVIg and IV anti-RhD
Several treatment trials have clearly demonstrated that in 65%-80% of patients treated with IVIg, the platelet counts increase within 24-48 hours.3,5,30 Duration of response is rarely greater than 10-14 days. Initial treatment regimens, in which 0.4 g/kg was infused daily for 5 days, have been supplanted by a higher-dose regimen of 1 g/kg daily for 1 or 2 days. This latter regimen is associated with longer daily infusion time and greater toxicity, including infusion reactions, headaches, occasional aseptic meningitis, hemolytic anemia due to alloantibodies, acute renal failure, and rare thrombotic events, primarily in the elderly. The concomitant use of corticosteroids may enhance the platelet response, reduce infusion reactions, and result in fewer headaches.
Patients who are Rh positive, not significantly anemic, and still have their spleens are candidates for treatment with anti-RhD. Before initiating treatment with anti-RhD, patients should be Rh typed and have a direct antiglobulin test performed. Treatment with the US Food and Drug Administration (FDA)–approved dose of 50 μg/kg can result in an increase in the platelet count to > 50 × 109/L in nearly 80% of patients, but requires 48-72 hours for a clinically significant response.3,5,31 Infusions of 75 μg/kg have been associated with a more rapid increase in the platelet count equivalent to that reported with IVIg treatment.32 The duration of response to anti-RhD therapy is usually longer than that observed with IVIg treatment, averaging 21 days.33 Treatment with anti-Rh immunoglobulin typically results in a mild hemolytic anemia with an average decrease in hemoglobin of 1-1.5 g. Occasional episodes of intravascular hemolysis resulting in renal failure and rare cases of disseminated intravascular coagulation and death have also been reported.5
Splenectomy
Splenectomy is the historical “gold standard” for the treatment of chronic ITP. A systematic review of the medical literature has shown that 65% of patients will have unmaintained remissions lasting 10 years or longer. In the majority of these patients, the procedure appears to be curative.34 The response rate in the first week is nearly 85%, with 20% of patients relapsing within weeks to years.34 However, even after relapse, patients appear to be less refractory to medical treatment.34 Patients older than 45 years appear to have a lower response to splenectomy.34 At present, there are no readily available clinical or laboratory markers that are predictive of response to splenectomy, although there it has been suggested that hepatic sequestration of autologous indium-111–labeled platelets may be predictive of a poor response.35
Laparoscopic splenectomy is associated with lower complication rates and faster recovery, no greater need for accessory splenectomy, and no loss in efficacy.36 Splenectomized patients should have yearly influenza vaccinations and, if a fever occurs, the patient should immediately receive parenteral broad-spectrum antibiotics that are effective against pneumococcus. This is true no matter how many years have elapsed since the splenectomy and despite immunization. Other long-term outcomes after splenectomy are unknown, particularly in regard to uncommon events such as pulmonary hypertension or vascular dementia.37,38
Anti-CD20 therapy (rituximab)
B-lymphocyte depletion using rituximab, a humanized anti-CD20 mAb, has shown limited but reproducible efficacy in patients with chronic ITP.39,40 Up to 60% of patients will have an initial increase in their platelet count, with an estimated 1/3 of patients obtaining an initial (1-year) unmaintained complete response (platelet count, > 100 × 109/L) with the use of the standard lymphoma regimen of 375 mg/m2 rituximab weekly for 4 weeks.39,40 Nearly all partial responders will relapse within 1 year, whereas nearly all complete responders will maintain their response for at least 1 year. Approximately one-half of complete responders will relapse within 4 more years. Although repeat treatment of the relapsed complete responder can result in a high rate of response,41 the safety of this approach has not been fully evaluated. Concerns about the use of anti-CD20 therapy include the development of progressive multifocal leukoencephalopathy and reactivation of hepatitis B. These risks may be lower in ITP patients than in patients with lymphoma and other systemic autoimmune disorders, because patients with ITP are generally not intrinsically immunosuppressed by their disease or receiving additional immunosuppressive therapies. Common, but less serious, toxicities include first-infusion reactions such as fever and chills and serum sickness, the latter being especially common in children.42 Although total Ig levels rarely decrease, patients cannot mount a normal humoral antibody responses to some vaccines for months after treatment. Therefore, it may be preferable to immunize patients before the initiation of rituximab therapy because splenectomy may need to be performed within the 6- to 9-month period after rituximab therapy. The optimal dose and frequency of rituximab administration for the treatment of ITP remains unknown.43
TPO receptor agonists: romiplostim and eltrombopag
Romiplostim was the first TPO receptor agonist to enter clinical trials.44 Subsequently, 2 randomized, placebo-controlled studies were published, one in splenectomized patients and the other in nonsplenectomized patients.45 In both studies, the same dosing regimen was used with progressive weekly increases in dose depending on the platelet count, beginning at 1 μg/kg and increasing to 15 μg/kg. Rescue medications were allowed for overt bleeding or very low counts associated with a high risk of bleeding. Concomitant medications such as prednisone could be decreased or stopped as the platelet count increased.
In both trials, unequivocal efficacy was demonstrated. Durable response (platelet count, ≥ 50 × 109/L for 6 of the last 8 weeks and no rescue therapy) was seen in 38% of splenectomized patients and in 61% of nonsplenectomized patients. The overall response rate (platelet count, ≥ 50 × 109/L on 4 of 24 weeks) was 79% in splenectomized patients and 88% in nonsplenectomized patients.45 There were no responses in the splenectomized patients and only a 14% response rate in nonsplenectomized patients taking placebo. There were significant reductions in the use of concomitant medications such as prednisone and reduced use of rescue medications (eg, IVIg, anti-RhD, or prednisone).45 No tachyphylaxis was seen over the 6 months of study, nor did any important toxicities emerge, such as an increased incidence of thromboembolic events or myeloid malignancies. Due to rare instances of increased BM reticulin that were observed in patients at higher doses, the highest recommended dose for treatment is now 10 μg/kg. “Rebound” thrombocytopenia with platelet counts decreasing to less than pretreatment baseline levels occurred in up to 5%-10% of patients who stopped treatment abruptly. Romiplostim was licensed in August 2008 based on these 2 studies.
Patients who entered 1 of the 2 previous studies were eligible to enter a long-term maintenance study validating the efficacy and safety of romiplostim use for up to 3 years of follow-up.46 Overall, this study showed that the long-term use of romiplostim as a maintenance therapy was feasible. Platelet counts could be maintained for years without the need to significantly increase the dose. Many patients learned to give weekly injections at home. No important new toxicities were identified with extended use. Nine cases of BM reticulin fibrosis were identified, but no cases of myelofibrosis/myeloid metaplasia. Whether this incidence is significantly higher than that which occurs in patients with ITP successfully treated with other agents requires additional study.
An open-label, 52-week randomized trial of romiplostim versus standard of care reported a higher rate of platelet response (platelet count, > 50 × 109/L at any scheduled visit), lower incidence of treatment failure and splenectomy, and less bleeding in the romiplostim-treated patients The starting romiplostim dose in this study was 3 μg/kg and the rate of platelet response was 2.3 times that observed in the standard-of-care group.47 However, utility beyond 52 weeks compared with patients who were treated with splenectomy is unknown. Another study has reported safety and efficacy of romiplostim in 22 children.48 In this small, 12-week randomized trial of patients 12 months to 18 years of age, platelet counts of > 50 × 109/L for 2 consecutive weeks was achieved in 88% of patients in the romiplostim group compared with none in the placebo group. Romiplostim treatment was well tolerated, with no serious adverse events.48
Eltrombopag is the first oral TPO receptor agonist to complete clinical trials and to be licensed for use in the United States. In the initial published study, eltrombopag was given for 6 weeks in daily doses of 30 mg, 50 mg, and 75 mg, and results were compared with patients given placebo.49 Responses were seen in 70%-80% of patients at the 2 highest eltrombopag doses compared with 11% in those receiving placebo.48 No important toxicity was seen and bleeding decreased as the platelet counts increased. A second study reported similar results for thrombocytopenic patients with hepatitis C infection, allowing continued antiviral chemotherapy without dose reduction or interruption.50
A third confirmatory study was a 6-week randomized, placebo-controlled trial that compared 50 mg of eltrombopag against placebo.51 That study demonstrated a 59% response rate in the eltrombopag arm, based on an increase in platelet count to > 50 × 109/L compared with a 16% increase in platelet count in those taking placebo. Bleeding manifestations were decreased in responders, but returned to baseline levels after the medication was discontinued and platelet counts declined. In that study, rebound thrombocytopenia upon drug withdrawal was rare and no statistically significant organ toxicity was seen. However, some patients developed significant liver enzyme increases requiring cessation of medication. Accordingly, the FDA has required a black box warning concerning the need to monitor liver function in patients taking eltrombopag.51
A 6-month randomized study trial comparing eltrombopag with placebo showed results comparable to the 6-month pivotal trial of romiplostim.52 A long-term extension study reported in abstract form has confirmed the durability of platelet responses.53 In addition, long-term follow-up of all patients enrolled in eltrombopag trials found a lower frequency of thromboembolic events than was reported in earlier studies.54
Monitoring and management of side effects of TPO mimetics
Given the mechanism of action of TPO mimetics, the side effects of concern are the development of BM fibrosis, venous thromboembolism, myeloid malignancies, and rebound thrombocytopenia. Reticulin fibrosis (grade 2 or above) is rare with the use of TPO mimetics and can be monitored by paying close attention to blood counts and morphologic abnormalities on peripheral blood smear. The exact incidence of this complication is unclear, but reticulin fibrosis appears to be a rare, dose-dependent phenomenon that resolves after cessation of the TPO mimetic.55 No significant increase in incidence of venous thromboembolism has been reported in patients who received romiplostim or eltrombopag compared with the incidence in ITP patients, and thromboembolic events have not been shown to be correlated with platelet counts.54 However, these agents should be used with caution in patients with known predispositions to arterial or venous thrombosis. No increase in myeloid malignancies has been reported so far in patients treated with either agent. The incidence of rebound thrombocytopenia is < 10% with either agent and can be managed by close monitoring of platelets count in the 4 weeks after discontinuation of treatment. Patients who develop hepatotoxicity with eltrombopag should not be rechallenged with the drug except under exceptional circumstances. Hepatotoxicity has not been observed with romiplostim.
Single-agent treatment of refractory ITP
Azathioprine, danazol, cyclophosphamide, cyclosporine A, and mycophenolate mofetil have shown limited efficacy in the treatment of ITP. No single agent induces unmaintained remission in > 30% of refractory cases, and this is particularly true in patients refractory to splenectomy.56 In one report, pulse cyclophosphamide induced a complete response in 13 of 20 patients, 8 of whom remained in remission with a median follow-up of 2.5 years.57 Even autologous stem cell transplantations have only been found to have a 25%-33% response rate and are without multi-year follow-up data.58
Controversies in ITP therapy
The high response rates reported in randomized trials of refractory postsplenectomy patients treated with TPO receptor agonists have established these agents as the drugs of choice for this group of patients. However, the choice of second-line therapy in newly diagnosed patients who fail corticosteroids is much more controversial. Options include: (1) laparoscopic splenectomy, with its low morbidity and the highest documented rate of durable remission; (2) rituximab treatment before splenectomy, with 1 of 5 patients in unmaintained remission at 5 years; or (3) chronic and potentially indefinite therapy with a TPO receptor agonist to maintain a safe platelet count without the use of additional immunosuppression or splenectomy. A long-term randomized trial of sequenced postcorticosteroid therapy could provide clinical data for a more logical treatment algorithm.
Disclosures
Conflict-of-interest disclosure: H.A.L. has received research funding from Shionogi and Amgen, has consulted for GSK and Amgen, and has been affiliated with the speakers' bureau for GSK. V.P. has been affiliated with the speakers' bureau for and received honoraria from Amgen and GlaxoSmithKline. Off-label drug use: This manuscript discusses the use of eltrombopag and romiplostim in liver disease and ritmiximab in ITP.
Correspondence
Howard A. Liebman, Professor of Pathology and Medicine, Division of Hematology, Keck School of Medicine, 1441 Eastlake Ave, NOR 3466, 9172, Los Angeles, CA 90033; Phone: (323) 865-3950; Fax: (323) 865-0060; e-mail: liebman@hsc.usc.edu.
