Abstract
Ongoing analysis of the seminal AZA-001 study has taught many important lessons in the use of DNA methyltransferase (DNMT) inhibitors. The data emphasize the importance of patience in the use of these drugs, with several cycles required for the manifestations of hematologic responses. Improved survival in patients with high-risk myelodysplastic syndrome (MDS) treated with azacitidine extends to patients with any International Working Group–defined hematologic response; however, the benefit to patients with stable disease is less clear. A great deal remains to be learned about the optimal dosing and scheduling of the DNMT inhibitors, alone and in combination. New information on the impact of DNMT inhibitors on the immune system and on stem cells will likely lead to novel uses of these drugs in MDS and other hematologic and nonhematologic malignancies.
Introduction
The AZA-001 study firmly established azacitidine as the treatment of choice for patients with high-risk myelodysplastic syndrome (MDS) not proceeding to allogeneic stem cell transplantation.1 Compared with physicians' pre-randomization selection of the appropriate conventional therapy for the individual patient (chosen from cytarabine plus anthracycline acute myeloid leukemia (AML)–type induction chemotherapy, low-dose cytarabine, and best supportive care), the azacitidine-treated group demonstrated increased median survival and twice the 2-year survival compared with patients in the conventional care group. In contrast, 2 studies comparing decitabine to best supportive care in high-risk MDS patients, both using the US Food and Drug Administration (FDA)–approved dose schedule of decitabine, failed to demonstrate a survival benefit.2,3 The FDA-approved dose schedule of decitabine administers higher doses in a more toxic schedule than the more commonly prescribed 5-day schedule developed at the M.D. Anderson Cancer Center (MDACC) but never studied in a randomized trial.4,5 In addition to improving survival, treatment with both DNA methyltransferase (DNMT) inhibitors led to transfusion independence in approximately 50% of cases,1,2,4–6 trilineage normalization in approximately 15% (CL Beach, Celgene Corporation, personal communication), and complete and partial responses in 10%-20%. Azacitidine treatment has also been shown to be associated with improved quality-of-life measurements.7
Whereas azacitidine has become accepted as an important therapy for patients with high-risk MDS, outcomes with conventionally dosed azacitidine leave significant room for improvement. The percentage of patients who develop normal hemograms is low, the median duration of hematologic response is only 14 months,1,8 and no patient is cured with a DNMT inhibitor alone. In addition, the extant literature explores the use of DNMT inhibitors as primary treatment for MDS and does not explore alternative uses for these drugs. This article reviews additional information derived from further analysis of AZA-001; new information about dosing, schedule, and preparation; combination therapies including DNMT inhibitors; and alternative use of DNMT inhibitors in remission and in association with allogeneic stem cell transplantation (SCT).
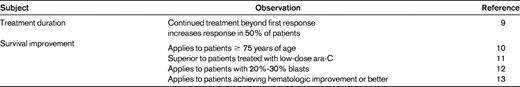
New lessons learned from AZA-001
Ongoing analysis of the AZA-001 data enables the refinement of treatment using azacitidine in patients with MDS (Table 1). While it has long been known that a significant lag time exists between the initiation of DNMT inhibitor therapy and the onset of clinical response, a recent analysis has examined the kinetics of response in greater detail.9 The median number of cycles administered until the first hematologic response was 2; 90% of hematologic responses appeared by the conclusion of cycle 6. However, continued azacitidine administration beyond first response improved the quality of the response in approximately half the patients. The median time to best hematologic response was 3.0-3.5 cycles in patients who achieved a complete or partial response; however, some patients' best response required up to 12 cycles of therapy to manifest.
Whereas DNMT inhibitors have been recommended for older patients who may not be eligible for potentially curative SCT, the feasibility of the azanucleosides in the “older elderly” had not been addressed until recently. AZA-001 accrued 87 patients age 75 or older. Investigators preselected best supportive care in 60 of these patients and low-dose cytarabine in 24. As with the overall trial population, azacitidine improved overall survival in this elderly cohort (hazard ratio, 0.48; 95% confidence interval, 0.26-0.89; P = .0193). A similar percentage of patients became transfusion independent as in the overall study population (43%), and hospitalizations for adverse events were not more frequent in the azacitidine-treated cohort.10
Over the years, some have speculated that the impact of azacitidine in MDS was likely similar to that of low-dose cytarabine. AZA-001 was neither designed nor powered to compare survival between azacitidine and each of the individual conventional care regimens. Post hoc analysis compared patients preselected by physicians for the low-dose cytarabine arm; 45 patients were randomized to azacitidine and 49 to low-dose cytarabine. Patient characteristics were well balanced. As with the overall population, the cytarabine-assigned patients treated with azacitidine had twice the 2-year survival of the cytarabine-treated patients. The difference in outcome was especially pronounced for patients with poor-risk cytogenetics, especially in patients with abnormalities of chromosome 7. Hematologic responses were more common and longer lived in the azacitidine-treated group, and that cohort had fewer days in the hospital.11
Another post hoc analysis from AZA-001 involved patients with 20%-30% BM blasts.12 Such patients were previously classified as “RAEB-t”; in current World Health Organization nomenclature, such patients are considered to have AML with features of MDS. A total of 113 such patients were accrued to AZA-001 with the following preassignments: best supportive care (n = 63), low-dose cytarabine (n = 34), and induction chemotherapy (n = 16). Fifty-five patients were assigned to azacitidine; 58 to the preselected conventional care regimen. Baseline characteristics were comparable between the azacitidine and conventional care cohorts. The difference in 2-year survival appeared greater for this group than for the overall cohort (50% vs 16%; median survival, 24.5 vs 16 months).
The last insight to be derived from AZA-001 concerns the appropriate duration of therapy for patients treated with azacitidine. Most experts concur that ongoing therapy is appropriate for patients who are experiencing hematologic responses. The survival benefit appears to extend beyond patients who achieve complete and partial responses. Comparing patients who achieve hematologic improvement in the azacitidine-treated arm with those in the conventional care arm, survival was improved in the former. Whether patients whose best response is stable disease at 6 months of treatment or greater have improved survival is unclear. Comparing such patients to patients who maintained stable disease in the conventional care arm, no survival difference was found. Comparison of the baseline clinical characteristics of the 2 cohorts suggested that those patients who achieved stable disease with azacitidine had worse cytogenetics and a greater incidence of severe thrombocytopenia compared with patients who achieved stable disease with conventional care. Confirmation of that finding would require a trial in which patients with stable disease on azacitidine were randomly assigned to continue therapy versus discontinuation.13
Scheduling of DNMT inhibitors
Both FDA-approved DNMT inhibitors are challenging to administer. The FDA-approved schedule of 5-azacitidine (75 mg/m2/d for 7 days repeated every 28 days) resulted from CALGB9221, a study in which many patients reconstituted the azacitidine at home and self-injected. Drug administration on the weekend is problematic for many practitioners. A community practice–based study randomized patients to one of 3 schedules: (1) 75 mg/m2/d for 7 doses, daily Monday-Friday, then again on the following Monday-Tuesday (5-2-2); (2) 75 mg/m2/d daily for 5 doses Monday-Friday; and (3) 50 mg/m2/d daily Monday-Friday on each of 2 consecutive weeks (10 doses, 5-2-5). The clinical end points were hematologic response; BM response and survival were not monitored. 66% of patients had lower-risk disease by French-American-British criteria; cytogenetics was not required. Overall, there was no difference between the 3 schedules. However, patients with baseline thrombocytopenia were more likely to achieve transfusion independence if treated with the 5-2-5 schedule.14
The 5-2-5 schedule was based on a previous phase 1 study that selected 50 mg/m2/d for 10 days as a clinically tolerable schedule that was particularly effective in reversing promoter methylation.15 The US Leukemia Intergroup Randomized Phase Study E1905 used this schedule as a treatment platform with the goal of doubling the trilineage normalization rate from the 15% seen in CALGB 9221. Preliminary analysis of the E1905 data suggests that the novel schedule did achieve that targeted 30% trilineage response rate, strongly supporting the concept of prolonged administration of lower doses of DNMT inhibitors.16 Such prolonged administration may increase the efficacy of the azanucleosides analog through less cell-cycle inhibition, leading to increased incorporation of the nucleoside into DNA and subsequent increased cell replication necessary for effecting methylation reversal.
Alternative dosing schedules for decitabine have also been developed. In a phase 1B study, investigators at the MDACC originally selected 15 mg/m2/d daily for 10 days as an optimal schedule with which to move forward.17 Based on a subsequent 3-arm randomized phase 2 trial, the now common 20 mg/m2/d daily for 5 days schedule was promoted.4 This schedule appears to be less toxic than the FDA-approved schedule and is given on an outpatient basis, which is not feasible with the FDA-approved schedule.5 The impact of this schedule on survival has not been tested. A high rate of hematologic response, including 47% complete remissions, was demonstrated in a cohort of elderly AML patients, many of whom had documented antecedent MDS treated with decitabine 20 mg/m2/d daily for 10 days.18
An oral preparation of azacitidine has been studied in a phase 1 dose-escalation study on a typical 7-/28-day schedule. At the maximum tolerated dose, oral bioavailability was approximately 13% that of parenteral azacitidine. Nonetheless, methylation reversal was similar to that seen with parenteral azacitidine, although fewer loci were significantly demethylated; 73% of previously untreated patients developed clinical responses.19 This oral preparation is now being studied in daily 14- and 21-day schedules, further testing the concept of prolonged administration of lower doses of DNMT inhibitors.
Combination therapies
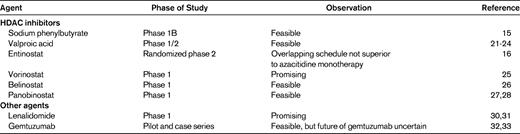
Another strategy for increasing the response rate, quality, or duration of responses has been to combine azanucleosides with other agents, either strategically or empirically (Table 2). The most common class of agents to be combined with DNMT inhibitors has been histone deacetylase (HDAC) inhibitors. Such combinations were based on the observation that optimal in vitro reexpression of genes for which transcription was silenced through promoter methylation was achieved by the sequential application of a DNMT inhibitor followed by an HDAC inhibitor.20 This synergistic effect was highly sequence specific and has been shown for a large variety of methylated tumor-suppressor genes in a variety of malignancies. The earliest combinations to be studied included combinations of DNMT inhibitors with the short-chain fatty acids sodium phenylbutyrate15 and valproic acid.21–23 These fatty acids require millimolar concentrations to demonstrate HDAC-inhibitory activity, but such levels can be transiently achieved in vivo with both compounds. A randomized trial of decitabine with and without valproic acid is under way at the MDACC.24 The orally bioavailable, class I–specific HDAC inhibitor entinostat has been combined with azacitidine, and an overlapping schedule of this combination did not appear to be superior to azacitidine alone (E1905).16 The most promising report of clinical responses derives from a phase 1 study of concomitant azacitidine and the non-class-specific HDAC inhibitor vorinostat; a multicenter phase 2 trial is ongoing to confirm these data.25 Other pan-HDAC inhibitors combined with azanucleosides include panobinostat and belinostat.26–28 It has been difficult to link gene reexpression to clinical response in these trials.15,18,21,29
In the category of empiric combination therapy, a small phase 1 trial of azacitidine plus lenalidomide demonstrated dramatic responses; phase 2 development of this combination is under way.30,31 A high complete response rate (11%/20%) was reported among 20 elderly patients with AML or high-risk MDS treated with azacitidine in combination with the CD33 immunotoxin gemtuzumab ozogamicin; 3 of 8 patients in another case series achieved complete response with similar treatment.32,33 The withdrawal of FDA approval for gemtuzumab makes further feasibility of this combination unlikely.
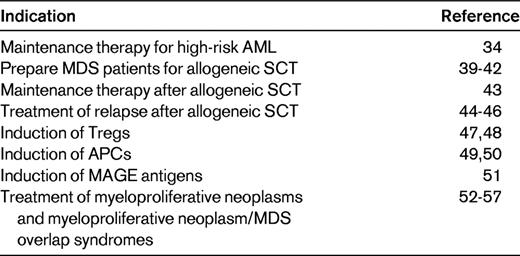
Azacitidine as maintenance therapy
A potentially attractive use of azanucleosides is as maintenance therapy in patients induced into remission with intensive chemotherapy (Table 3). Grovdal et al treated 64 patients (median age 68) with high-risk MDS or AML with myelodysplastic features with cytarabine-based induction therapy with the intent to follow this with azacitidine maintenance therapy.34 In that study, 24 patients achieved remission and 23 patients (10 MDS, 10 AML, and 3 chronic myelomonocytic leukemia [CMML] patients) continued on to azacitidine. The azacitidine dose required reduction for cytopenias; the median dose administered in all cycles was approximately 56 mg/m2/d. The mean dose per patient administered ranged from 30-63 mg/m2/d. The median duration of complete response was 13.5 months (range, 2-49+). The median overall survival for the azacitidine-treated group was 20 months (range, 4-52+). This phase 2 trial could not determine whether the azacitidine maintenance therapy improved survival.
Azanucleosides in the transplantation setting
Allogeneic SCT remains the only curative therapy for MDS; however, the percentage of patients who are cured does not exceed 30% (Table 3).35–38 DNMT inhibitors have been proposed for the induction of response before allogeneic SCT, as part of conditioning therapy, as post-SCT maintenance, and for the treatment of relapse after SCT.
Several studies have examined the use of DNMT inhibitors before SCT; 72 patients have been reported to have received allogeneic SCT after DNMT therapy in retrospective analyses. The majority of patients received reduced-intensity conditioning. With various lengths of follow-up, approximately 45% of patients were alive.39–42 The Moffitt group's analysis compared patients who had received azacitidine before SCT with those who had not. No differences in GVHD, relapse, nonrelapse mortality, or overall survival were found.41
The MDACC group treated patients with AML and high-risk MDS who were not in first complete remission with gemtuzumab ozogamicin, fludarabine, and melphalan with allogeneic stem cell infusion.43 Patients who achieved complete remission by day 30 were assigned to receive azacitidine on day 5 of a 30-day schedule. Azacitidine was given at 1 of 5 dose levels, ranging from 8-40 mg/m2/dose. Of 90 patients enrolled, 74 survived and achieved complete remission and 45 of these patients received azacitidine; 62% of all patients died or relapsed. Factors associated with improved overall and event-free survival included a greater number of cycles of azacitidine administered, although the dose of azacitidine received was not associated with survival. Azacitidine administration in this context did not appear to be associated with an increase in GVHD or other toxicities.
We reported 10 patients relapsed after allogeneic SCT who were treated with azacitidine as a salvage therapy. Six achieved complete remission, in 4 cases associated with restoration of complete donor chimerism.44 Five of the 6 remained alive and disease-free at a median follow-up of 624 days; 3 of these patients received donor lymphocyte infusions after azacitidine. The German Cooperative Group for hematopoietic SCT described 22 patients relapsed after allogeneic SCT who were subsequently treated with azacitidine.45 Five achieved complete remission and 4 partial remissions. The estimated 2-year survival was 23%; only one patient remained in remission at the time of publication. The Freiburg group detailed 26 relapsed patients treated with azacitidine and donor lymphocyte infusions (DLIs).46 The plan was to give 3 days of azacitidine followed by DLI on day 10, and commence further azacitidine on day 22. In that study, 14 of 26 patients had received DLI before azacitidine and 4 of 26 patients achieved sustained complete response; 3 of these developed complete donor chimerism. The estimated 2-year survival was 20%. These retrospective analyses suggest an approximately 20% salvage rate for these patients.
DNMT inhibitor as immunomodulators
DNMT inhibitors have recently received attention as potential useful modulators of the immune system (Table 3). DiPersio et al studied the impact of azanucleosides on CD4+CD25−FOXP3− T cells with the intention of increasing FOXP3 expression and converting these cells to Treg cells that could modulate GVHD.47 Both nucleosides induced FOXP3 in vitro; the cells so induced function as suppressor cells. The administration of azacitidine but not decitabine to mice who received a T-cell-depleted allogeneic SCT with additional mismatched T cells completely protected the mice from GVHD and increased circulating FOXP3+ Tregs. Azacitidine did not appear to inhibit a GVL effect in mice transplanted with an A20 leukemia model. The induction of suppressor cells by azacitidine persisted in FOXP3-knockout cells and knockout mice; interestingly azacitidine reversed the negative phenotype of FOXP3-knockout mice when administered shortly after birth. This was attributed to the putative conversion of autoimmune T cells to FOXP3− Tregs.
A similar impact of azacitidine on T cells was described by Sanchez-Abarca et al from Salamanca.48 Azacitidine administration led to the demethylation of the FOXP3 promoter and the expansion of Treg cells. The administration of azacitidine after allogeneic SCT abrogated GVH in a complete mismatch model and led to an increased percentage of Treg cells in the peripheral blood, BM, and spleen.
DNMT inhibitors may be useful in the immunotherapy of nonhematopoietic tumors. Azacitidine treatment converted CD11b myeloid cells infiltrating murine colon carcinomas into APCs. Vaccination with these cells protected the mice against tumor outgrowth when challenged with the parental tumor.49 Expression of the minor histocompatibility antigen HA-1 appears to be silenced through promoter methylation in a variety of solid tumor cell lines and primary solid tumor specimens. Decitabine induced the expression of HA-1 in such cells and sensitized them to killing by HA-1–specific cytotoxic T cells. In contrast, HA-1 expression was not induced in normal nonhematopoietic cells.50
A combination of azacitidine plus valproic acid up-regulated the expression of melanoma associated (MAGE) antigens in AML and myeloma cell lines, increasing their recognition by a MAGE-specific cytotoxic T-cell clone. MAGE-reactive cytotoxic T cells were induced in 10 of 21 patients receiving azacitidine plus valproic acid for MDS or AML. Six such patients achieved a partial or complete response; however, such responses were also seen in patients who did not develop MAGE-reactive cytotoxic T cells.51
Use in myeloproliferative neoplasms and myeloproliferative neoplasm/MDS overlap syndromes (Table 3)
Treatment of CD34+ cells from patients with chronic idiopathic myelofibrosis but not normal CD34+ cells with decitabine followed by an HDAC inhibitor led to increased apoptosis and decreased repopulation of NOD/SCID mice.52 Such treatment also improved trafficking of such cells to the BM rather than the spleens in NOD/SCID mice.53 Eight of 34 patients with idiopathic or post-essential thrombocythemia/polycythemia vera myelofibrosis responded to azacitidine; however, most responses were not profound and were short-lived.54
Fourteen of 36 patients with CMML responded to azacitidine in a retrospective study. This included 5 complete and partial responses.55 Similarly, 25% of 31 patients treated for CMML with decitabine achieved complete or partial response (using the FDA-approved schedule).56 Eleven of 19 patients with CMML treated at a single institution developed complete responses with decitabine treatment (20 mg/m2/d for 5 days).57 Interestingly, a complete cytogenetic response in a patient with the related disease juvenile myelomonocytic leukemia with monosomy 7 has recently been reported.58
Disclosures
Conflict-of-interest disclosure: The author has received research funding, has equity ownership in, and has consulted for Celgene. Off-label drug use: Azacitidine for the treatment of leukemia and the use of histone deacetylase inhibitors for MDS and AML.
Correspondence
Steven D. Gore, MD, Professor of Oncology, Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins, 1650 Orleans St, Baltimore, MD 21231; Phone: (410) 955-8781; Fax: (410) 614-3809; e-mail: gorest@jhmi.edu.