Abstract
Multiple and complex abnormalities of hemostasis are revealed by laboratory tests in such common diseases as cirrhosis and end-stage renal insufficiency. Because these abnormalities are associated with a bleeding tendency, a causal relationship is plausible. Accordingly, an array of transfusional and nontransfusional medications that improve or correct these abnormalities is used to prevent or stop hemorrhage. However, recent data indicate that the use of hemostatic drugs is scarcely justified mechanistically or clinically. In patients with uremia, the bleeding tendency (mainly expressed by gastrointestinal bleeding and hematoma formation at kidney biopsy) is reduced dramatically by the improvement of anemia obtained with the regular use of erythropoietin. In cirrhosis, the most severe and frequent hemorrhagic symptom (acute bleeding from esophageal varices) is not explained by abnormalities in such coagulation screening tests as the prothrombin and partial thromboplastin times, because formation of thrombin the final coagulation enzyme is rebalanced by low naturally occurring anticoagulant factors in plasma that compensate for the concomitant decrease of procoagulants. Rebalance also occurs for hyperfibrinolysis and platelet abnormalities. These findings are consistent with clinical observations that transfusional and nontransfusional hemostatic medications are of little value as adjuvants to control bleeding in advanced liver disease. Particularly in uremia, but also in cirrhosis, thrombosis is becoming a cogent problem.
Introduction
End-stage liver and kidney insufficiency are listed among the causes of an acquired bleeding tendency in most hematology textbooks. In uremia, hemorrhagic symptoms span from minor events such as bruising to severe and life-threatening complications such as upper gastrointestinal, pericardial, and intracranial bleeding. In cirrhosis, bleeding from esophageal varices develops in up to 25% of patients, with a case fatality rate as high as 15%-20%. Moreover, major blood losses requiring transfusion of blood components occur during and after operations such as transplantation and hepatectomy. Because in end-stage liver and renal disease, hemorrhagic symptoms are associated with multiple abnormalities shown in laboratory tests exploring the hemostasis system,1,2 a cause-effect relationship was inferred to be plausible. Therefore, it is common clinical practice to treat or prevent bleeding in these patients with an array of transfusional and nontransfusional medications aimed at potentiating hemostasis (ie, fresh-frozen plasma, platelet concentrates, antifibrinolytic drugs, prothrombin complex concentrates, and recombinant activated factor VII in cirrhosis3–6 and cryoprecipitate, desmopressin, and conjugated estrogens in uremia7–9 ). In general, the capacity of these agents to prevent or stop bleeding is not validated by randomized clinical trials, but is surmised on the basis of their demonstrated capacity to improve or correct abnormalities shown by hemostasis laboratory tests.
With this background, we review herein the pattern of hemostasis abnormalities in patients with end-stage kidney and liver disease; changes in these abnormalities induced by the aforementioned hemostatic agents; and the evidence that, particularly in chronic liver disease, questions the time-honored paradigm that the bleeding tendency of these patients is causally related to their abnormalities of hemostasis tests and that transfusional and nontransfusional hemostatic medications are clinically useful to prevent or stop bleeding. Both in kidney and liver disease, thrombosis is becoming a clinical problem, perhaps more prominent than hemorrhage.
Hemostasis defects in uremia
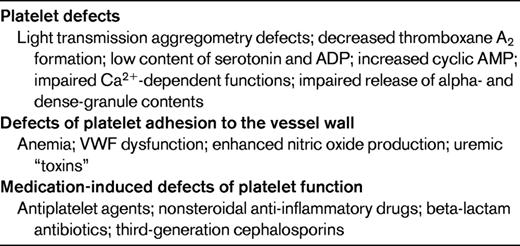
The more than half a million patients in the United States who have end-stage renal insufficiency requiring maintenance dialysis (with an estimated yearly cost of 29 billion US dollars) are the epitome of those who develop bleeding complications. The coagulation phase of hemostasis, as explored by such screening tests as activated partial thromboplastin time and prothrombin time, is normal in uremic patient outside of the period of heparin administration during dialysis aimed to prevent filter clotting. The most common and prominent laboratory abnormality is prolongation of the skin bleeding time,2,10 a term that refers to tests such as the template bleeding time and the Ivy bleeding time, used as surrogate ex vivo measurements of defective platelet interactions with the vessel wall and the delayed formation of the primary hemostatic plug. Thrombocytopenia is a rare cause of prolonged bleeding time, but there are multiple and complex abnormalities of primary hemostasis in uremia that help to explain this prolongation (Table 1).2,10 Even though biochemical platelet alterations and the resulting defects of aggregation do contribute to slowing the formation of the hemostatic plug, impaired platelet adhesion to injured vessels is thought to be the main determinant of the prolonged bleeding time in uremia. The mechanisms of defective platelet adhesion are complex and multifactorial (Table 1).
A dysfunction of VWF was thought to be an important culprit in bleeding disorders11,12 because both cryoprecipitate (a plasma product rich in VWF) and desmopressin (a synthetic derivative of the antidiuretic hormone that increases plasma VWF levels) shorten the bleeding time in uremia.7,8 A contributory role for the enhanced endogenous production of nitric oxide (a vasodilator and platelet function inhibitor) was postulated on the basis of the effect on the bleeding time induced by conjugated estrogens,9 which quench the production of nitric oxide.13,14 However, the current thinking is that anemia, a constant feature in advanced renal insufficiency, is a critical determinant of defective platelet adhesion to the vessel wall and the resulting prolongation of the skin bleeding time.
A pioneer observation was made in 1982 by Livio et al, who demonstrated in uremic patients that the bleeding time is prolonged in proportion to the degree of anemia, and that this test is shortened or corrected when the hematocrit is increased to at least 30% by RBC transfusion.15 The improvement of anemia improves platelet adhesion because more RBCs in the circulation push more platelets and leucocytes from the axial center of flowing blood toward the periphery, thereby enhancing cell contacts with the vessel wall and the formation of the primary hemostatic plug.16 Additional mechanisms that contribute to the effect exerted by the improvement of anemia on defective primary hemostasis are the release from RBCs of ADP, a powerful inducer of platelet aggregation,17 and the scavenging effect exerted by hemoglobin on nitric oxide.18 The aforementioned defects of primary hemostasis may be exacerbated by multiple medications that are taken by uremic patients (Table 1).
Therapeutic control of bleeding in uremia
The adoption of maintenance dialysis was the first step that improved the bleeding tendency in uremia, although not fully satisfactorily. The management of spontaneous bleeding and its prevention at the time of invasive procedures or surgery was further improved in the 1980s by the demonstration that some drugs shortened the prolonged bleeding time (ie, desmopressin with a short-lasting effect8 and conjugated estrogens with a more prolonged effect9 ). Because these medications cannot be administered prophylactically for prolonged periods of time, the long-lasting prevention of the bleeding tendency in uremia remained unsettled. A step forward was the finding in 1987 that the regular use of recombinant erythropoietin for the management of anemia caused a marked and sustained shortening of the bleeding time.19 This positive effect could be obtained after the attainment of hematocrit values of approximately 30%,20 thereby confirming the early observations on this critical threshold made by Livio et al9 with RBC transfusions. In general, clinical experience is that the improvement of anemia obtained through the regular administration of erythropoietin has minimized the frequency and severity of bleeding symptoms in patients with end-stage renal insufficiency beyond the benefits obtained by dialysis. The hematocrit should be kept at approximately 30%, because higher values and full correction of anemia increase the risk of atherothrombosis, particularly myocardial infarction and ischemic stroke.
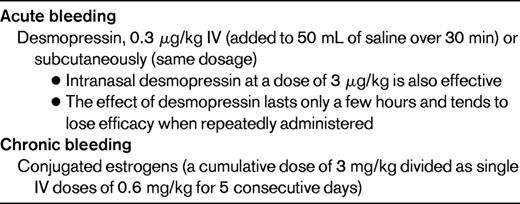
Are therapeutic weapons other than erythropoietin still being used to manage uremic bleeding? In patients not on erythropoietin therapy (eg, in acute or early renal insufficiency) or when the increase in the hematocrit induced by this drug has not yet been achieved, desmopressin is the drug of choice to prevent or stop bleeding at the time of surgery or invasive procedures. An alternative to desmopressin are conjugated estrogens, which shorten the bleeding time more slowly than desmopressin but have a more long-lasting effect.
Table 2 shows the recommended regimens of administration of drugs that are indicated in the prevention and control of uremic bleeding for their capacity to shorten the prolonged bleeding time (ie, the laboratory test that reflects the deranged primary hemostasis of uremic patients and the underlying defects causing hemorrhage). A current practical problem is that many laboratories have taken the bleeding time off of their list of approved tests, so that the management of uremic bleeding with drugs can no longer be easily monitored using this test. The successful control of bleeding by erythropoietin has perhaps thwarted the development and evaluation in uremia of tests alternative to the bleeding time, with the exception of PFA-100, the closure time of which has been found to be prolonged in patients with uremia, but the clinical value of this test remains to be established.21
Hemostasis defects in cirrhosis
The majority of patients with end-stage liver disease (approximately 400 000 are on the waiting list for transplantation in the United States) have complex and multifactorial alterations that involve all of the components of hemostasis.1 With regard to primary hemostasis (Table 3), thrombocytopenia is a frequent finding, with platelet counts usually ranging between 30 and 100 × 109/L. Defective platelet aggregation explains why the skin bleeding time is often more prolonged than would be predicted from the degree of thrombocytopenia. At variance with uremia, there are no equivalent data that anemia plays a role in causing the prolongation of the bleeding time and the hemorrhagic tendency in liver disease. The results of screening tests commonly used to explore the coagulation phase of hemostasis (ie, prothrombin time and partial thromboplastin time) are consistently prolonged because multiple coagulation factors are low in plasma in proportion to the degree of compromised protein synthetic capacity of the liver. Plasma hyperfibrinolysis is reported in cirrhosis on the basis of the increase of tissue plasminogen activator and decrease of the naturally occurring inhibitors of plasmin. These multiple and complex alterations of laboratory methods have traditionally led the clinician to infer that in cirrhosis, hemostasis is globally impaired and is the main cause of the bleeding diathesis seen so frequently in these patients.1
This concept was first challenged by the demonstration that routine hemostasis tests fail to reflect the bleeding tendency in cirrhosis, with their poor capacity to predict the onset and severity of bleeding from esophageal varices, after liver biopsy, and at the time of major operations such as transplantation. In addition, more recent findings show unequivocally that the aforementioned laboratory alterations consistent with an impaired hemostasis are indeed accompanied by opposing prothrombotic alterations (Table 3).22–24 With regard to primary hemostasis, thrombocytopenia and thrombocytopathy are paralleled by a marked increase of plasma VWF, the main platelet-vessel wall adhesive protein.25 In vitro experiments carried out under flow conditions that mimic those occurring in vivo demonstrated that due to high plasma VWF, platelet adhesion to the vessel wall is normal or even increased in cirrhosis notwithstanding the presence of thrombocytopenia and platelet function abnormalities.25 Pertaining to blood coagulation, low procoagulant factors are rebalanced by the concomitant decrease of naturally occurring anticoagulants in plasma.26 An additional important contribution to coagulation rebalance is provided by the increase of factor VIII in plasma.26 Similarly, laboratory changes consistent with hyperfibrinolysis tend to be compensated for by antifibrinolytic abnormalities (Table 3).27 That the concomitant alterations of both prohemostatic and antihemostatic components in cirrhosis ultimately result in a restored balance22–24 is unequivocally demonstrated by global tests such as thrombin generation assays,26,28 which explore both the pro- and anticoagulant components at the same time. However, these global tests are not yet standardized, validated, or used widely enough in the clinical context, making it still premature to propose them as routine alternatives to the clearly inadequate traditional tests (prothrombin and partial thromboplastin time).29–31
Therapeutic control of bleeding in cirrhosis
Fresh-frozen plasma is often used to prevent bleeding during liver biopsy or other potentially hemorrhagic invasive procedures in patients presenting with a prolonged prothrombin and/or partial thromboplastin time. Plasma is also used when patients bleed acutely from esophageal varices, despite no evidence of its efficacy from randomized clinical trials. The use of plasma is still a common practice despite the guidelines of the American Association for the Study of Liver Disease32 and in vitro studies showing that plasma shortens the prothrombin time but does not affect the amount of thrombin formed.33 Against the use of plasma stands not only current knowledge that the abnormalities of standard coagulation tests do not reflect the bleeding tendency in liver disease,29–31 but also that plasma may contribute through volume expansion to increase portal vein hypertension, aggravate decompensation, and increase the risk of bleeding and rebleeding from esophageal varices.
Platelet concentrates are used in the attempt to increase the low platelet count of cirrhosis patients, even though it is unclear which count threshold triggers the need for concentrate transfusion. Most clinicians set this threshold to at least 50 × 109/L and optimally at 100 × 109/L, but there are limited laboratory28 and clinical data34 providing evidence that these are the critical values. Neither is it known which dose of platelet should be transfused; the most commonly used regimen is one standard adult concentrate (corresponding to approximately 300 ± 33 × 109 platelets). According to our clinical experience, this regimen barely increases the platelet count and fails to ensure the normalization of such global hemostasis tests as thrombin generation and thromboelastography, perhaps because most transfused platelets are trapped in the spleen and liver. Preliminary results indicate that the thrombopoietin receptor agonist eltrombopag increases platelet counts in cirrhosis more markedly than transfusion, but the study of this drug was interrupted due the occurrence of thrombotic complications.35
Recombinant activated factor VII (rFVIIa), originally developed and licensed for the treatment of bleeding in hemophilia A complicated by alloantibodies inhibiting factor VIII, was also used off-label for its capacity to generate a strong thrombin burst at the site of bleeding in clinical conditions such as variceal bleeding and major surgical operations such as hepatectomy and liver transplantation. The majority of studies carried out in these settings are negative with regard to the effect of rFVIIa on clinically relevant outcomes (ie, arrest of bleeding, reduction of rebleeding, and mortality),36 with the exception of a modest reduction of transfusion need and hematocrit loss in liver transplantation.37 Accordingly, the use of rFVIIa is not recommended as an adjunctive hemostatic treatment for variceal bleeding, nor for bleeding prophylaxis in patients undergoing liver biopsy, transplantation, or resection.38,39 Concentrates of vitamin K–dependent factors (also called prothrombin complex concentrates) had been used in patients with advanced liver disease when our current knowledge on the poor clinical relationship between bleeding and coagulation factor deficiencies was not available.3 Indeed, these plasma-derived products shorten or fully correct the prolonged coagulation tests and factor deficiencies,3 but their clinical effect on actual bleeding is not substantiated, and the risk of thrombosis is significant with them and rFVIIa.
Among the antifibrinolytic drugs, a potential candidate is tranexamic acid, which, given orally or IV, blocks the binding to fibrin of plasminogen and thus the activation of this fibrinolysis proenzyme to the enzyme plasmin. According to a Cochrane meta-analysis, this medication is not effective in the management of acute variceal bleeding as an adjuvant along with endoscopic therapy and such drugs as cimetidine and protein pump inhibitors.40 In patients undergoing orthotopic liver transplantation, tranexamic acid reduces to a small degree blood loss and transfusion requirements,41,42 but the overall clinical benefit is generally trivial because the marked improvement of surgical and anesthesiological methods has dramatically reduced the need for transfusion during this operation.
Transfusional and nontransfusional hemostatic medications have an uncertain role in the prevention and treatment of bleeding in an array of clinical settings associated with end-stage liver disease. This is not surprising, given the current knowledge that bleeding is not caused mainly by hemostasis defects, but rather by hemodynamic alterations of portal hypertension, endothelial dysfunction, bacterial infections, and renal failure. Therefore, we find it unnecessary to provide specific recommendations on how to manage actual bleeding by hemostatic medication in cirrhosis as we have done with Table 2, which describes recommendations for uremic bleeding. This negative recommendation is supported by a review article on handling variceal bleeding, which does not mention any hemostatic medications,43 whereas specific recommendations are given on therapeutic approaches based upon vasoconstrictors, antibiotics, and endoscopic therapy.43
Thrombotic complications in liver and renal disease
Whereas it is known that liver and renal diseases are associated with a bleeding diathesis, it is less understood that they both share a thrombotic tendency, that with the aging of the population, is likely to become more and more clinically relevant. Clinicians tend to think that because of the prolongation of standard coagulation tests, patients with chronic liver disease are naturally anticoagulated and protected from thrombosis. A recent population-based study has indeed shown that the risk of venous thromboembolism is 2-fold higher in patients with liver disease than in controls.44 The corresponding clinical manifestations are not only portal-vein thrombosis (which has a frequency as high as 8%-25% in patients with advanced disease who are candidates for liver transplantation45 ), but also peripheral vein thrombosis and pulmonary embolism.44 The occurrence of thrombotic complications in cirrhosis is consistent with recent findings that these patients have a procoagulant imbalance related to the impairment of the thrombomodulin/protein C anticoagulant pathway combined with very high plasma levels of factor VIII.46 Accordingly, anticoagulant drugs should be used in patients with liver disease who develop venous thromboembolism notwithstanding the widespread belief that these drugs are contraindicated in patients with severe liver disease. Similarly, patients with cirrhosis are not protected from clinical manifestations of atherothrombosis (ie, coronary artery disease and ischemic stroke),47 even though it is unknown whether they are at higher risk than people with no liver disease. When atherothrombotic complications occur, antiplatelet agents should be considered for secondary prophylaxis, even though in patients with more severe thrombocytopenia (< 50 × 109/liter), the risk of bleeding is not trivial.
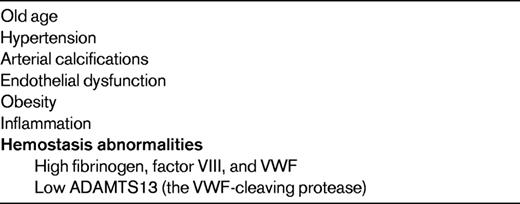
Chronic kidney disease, even in its early clinical stages, increases by 25%-30% the risk for premature atherothrombotic manifestations of cardiovascular diseases,48,49 which are in turn the most frequent clinical outcome in patients with end-stage disease on dialysis, accounting for approximately 40% of all deaths.50,51 Mechanistic links between cardiovascular and renal diseases are the high prevalence of shared risk factors (Table 4). Despite increasing awareness that patients with chronic renal disease are at very high risk for incident cardiovascular events, there is a paucity of clinical trials evaluating whether the adoption of prophylactic and therapeutic measures of consolidated efficacy in patients with cardiovascular disease without renal dysfunction are also useful in chronic renal disease. For example, a systematic review and meta-analysis on the effect of antiplatelet agents in patients with chronic kidney disease found that these drugs have uncertain effects on reducing mortality, but induce a definite increase of bleeding complications.52 It is important to intervene in these patients with medications and lifestyle changes to control risk factors for atherothrombosis, such as high blood pressure, serum LDL cholesterol, body mass index, and prothrombotic stimuli.53
Conclusions
The association between end-stage kidney and liver disease and a bleeding tendency has been demonstrated. The pathogenesis of bleeding in these common diseases is complex and multifactorial and the hemorrhagic tendency, particularly in cirrhosis, is not explained by the multiple abnormalities revealed by hemostasis tests. Anemia in patients with uremia and portal hypertension with related hemodynamic alterations in those patients with cirrhosis are much more critical than hemostasis defects in causing the bleeding tendency. Accordingly, medications that potentiate hemostasis have a limited role in the prevention and treatment of bleeding. Despite the bleeding tendency, hypercoagulability and the frequent concomitant presence of atherothrombosis risk factors predispose these patients to thrombotic complications. Antithrombotic prophylaxis and treatment should be implemented as needed in these patients, but the risk of increasing the hemorrhagic diathesis demands careful evaluation of the balance between benefits and risks in each patient.
Disclosures
Conflict-of-interest disclosure: P.M.M. has been affiliated with the speakers' bureau for Novo Nordisk. A.T. declares no competing financial interests. Off-label drug use: NovoSeven (rFVIIa).
Correspondence
P. M. Mannucci, Via Pace 9, 20122 Milano, Italy; Phone: 39-02-55035421, extension 8377; Fax: 39-02-50320723; e-mail: pmmannucci@libero.it.