Abstract
The contact pathway of coagulation consists of the proteins factor XI, factor XII, prekallikrein, and high-molecular-weight kininogen. Activation of the contact system leads to procoagulant and proinflammatory reactions. The contact system is essential for surface-initiated coagulation, as exemplified by aPTT, but there is probably no role for the contact system in initiating physiologic in vivo coagulation. However, over the last few years, there has been renewed interest, especially because of experimental evidence suggesting that the contact system contributes to thrombosis. Knockout mice deficient in one of the contact proteins were protected against artificially induced thrombosis. Furthermore, inhibiting agents such as monoclonal antibodies, antisense oligonucleotides, and small molecules were found to prevent thrombosis in rodents and primates in both venous and arterial vascular beds. Although it remains to be established whether targeting the contact system will be effective in humans and which of the contact factors is the best target for anticoagulation, it would constitute a promising approach for future effective and safe antithrombotic therapy.
Learning Objectives
To understand that the contact system consists of 4 proteins: factor XI, factor XII, PK, and HK
To understand that deficiency of factor XII, PK, or HK is not associated with a bleeding tendency in humans
To understand that targeting the contact system is an effective method to prevent thrombosis in mice
To understand that inhibition of the contact system may be a potentially safe alternative for the currently available anticoagulant drugs
Introduction
The contact system consists of 4 plasma proteins: factor XI, factor XII, prekallikrein (PK), and high-molecular-weight kininogen (HK). The proteins were recognized in the 1950s and 1960s after identification of individuals with (severely) prolonged activated partial thromboplastin times (aPTTs). Originally, the proteins were given names such as Hageman factor (factor XII), Fletcher factor (PK), Williams-Fitzgerald-Flaujeac factor (HK), and plasma thromboplastin antecedent (factor XI).1 The contact proteins circulate in an inactive form until blood comes into contact with negatively charged surfaces and will then initiate procoagulant and proinflammatory reactions via the intrinsic pathway of coagulation and the kallikrein-kinin system, respectively.2 With the exception of factor XI-deficient individuals, who have a variable bleeding tendency, a deficiency of one of the other contact factors is not associated with bleeding. Recently, some exciting data have become available that point to a role for the contact system in thrombosis. Even though the majority of the data were obtained from animal experiments, the implications for treatment of thromboembolic diseases are enormous: in vivo inhibition of one of the contact proteins would be ideal because these drugs may be effective against thrombosis and, at the same time, bear no risk of bleeding.
The contact system has a remarkable resemblance to the innate immune system based on the recognition molecules.3 Indeed, the contact system recognizes an increasing number of bacterial pathogens and other types of microorganisms.4 In particular, bradykinin (BK), released from kallikrein-processed HK, is a potent inflammatory mediator and plays a central role in the modulation of the innate immune response. Therefore, the contact system is part of the new research field referred to as “immunothrombosis.”5
In this chapter, we summarize several aspects of the contact system and its role in thromboinflammatory disorders with an emphasis on the preclinical work with (knockout) mice. In the accompanying chapters by Gailani and Key, the preclinical work in other rodents and primates and the epidemiological and clinical studies on the contact system and thrombosis are summarized.
Biochemistry of the contact system
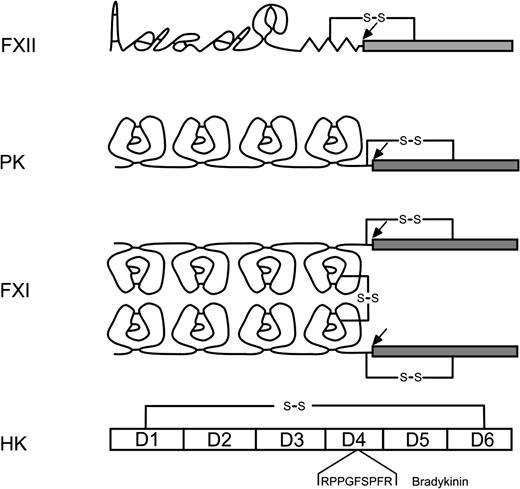
The contact system consists of 3 proenzymes (factor XII, PK, and factor XI) and a cofactor (HK). The domain structure of the contact proteins is shown in Figure 1. The contact system assembles on nonphysiological surfaces such as glass, kaolin, and ellagic acid, agents that are used to promote in vitro clotting in aPTT. Artificial surfaces that are used in catheters or cardiopulmonary bypass will also lead to activation of the contact system and, over recent years, more and more physiological surfaces have been identified, such as RNA, polyphosphates, neutrophil extracellular traps, and misfolded proteins.6-10 Factor XII binds directly to these surfaces. HK also binds directly and, because it is in the circulation in complex with PK and factor XI, the complete contact system becomes assembled on the surface.
Domain structure of the contact proteins. Cleavage sites for activation are indicated with an arrow.
Domain structure of the contact proteins. Cleavage sites for activation are indicated with an arrow.
Contact activation
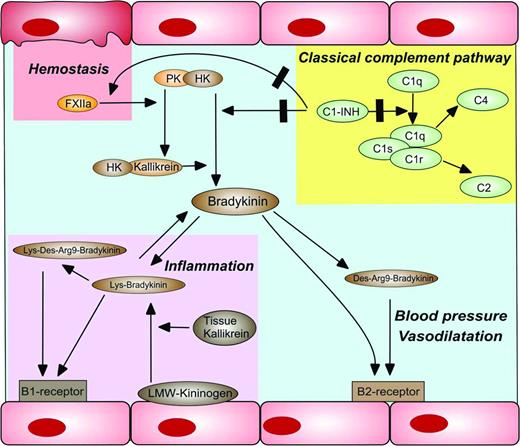
The significance of contact activation for hemostasis is not completely clear. According to current insights, the contact system is not involved in injury-induced clot formation. The most important argument for this statement is the lack of a bleeding diathesis in patients deficient in factor XII, PK, or HK. Coagulation occurs when the plasma protease activated factor VII comes into contact and subsequently forms a complex with tissue factor (TF). The TF/factor VIIa complex can activate factor X, which can convert prothrombin into thrombin. Thrombin, in turn, is involved in multiple pathways, one of which is the conversion of fibrinogen into fibrin, which constitutes the clot. Therefore, for this sequence of events, TF must come into contact with blood, for example, upon injury or inflammation. In addition, a TF-independent pathway has evolved in vertebrates: the contact system. Assembly of the contact system on (negatively) charged surfaces results in a series of procoagulant and proinflammatory reactions. Binding of factor XII to a negatively charged surface causes a conformational change of the protein and results in (limited) activation to factor XIIa. Activated factor XII cleaves PK into kallikrein (Kal), which reciprocally activates additional factor XIIa (Figure 2). Factor XIIa can activate factor XI to factor XIa, which further initiates thrombin and fibrin formation. HK serves as a nonenzymatic cofactor for the activation of both PK and factor XI. Apart from factor XIIa, PK can also be activated by prolylcarboxypeptidase on endothelial cells.11 Plasma kallikrein cleaves BK from HK. BK has many physiological and pathophysiological effects (Figure 3)12 ; it is involved in blood pressure regulation, increases vascular permeability, and causes vasodilation via the B2 receptor. Furthermore, as a vasoactive peptide, BK can cause venular dilatation and constriction of coronary arteries, bronchi, and gastrointestinal smooth muscles.13 Most of these processes are regulated via cytokines such as IL-6 and IL-8 or TNF-alpha, making BK an important player during inflammatory processes.13 Because BK has many functions, it is linked to several disorders such as hereditary angioedema, allergic reactions including asthma, high blood pressure, but also rheumatoid arthritis, pancreatitis, and Alzheimer's disease.13
Activation of the contact system. Factor XII (FXII) can be activated by negatively charged surfaces such as polyphosphates (polyP) derived from activated platelets or neutrophil extracellular traps (NETs). PK can be activated to kallikrein (Kal) by prolylcarboxylase (PRCP) on endothelial cells. Factor XIIa will also activate PK and thereby allows reciprocal activation, resulting in the generation of additional factor XIIa. Factor XIIa can initiate coagulation via the activation of factor XI. Both PK and factor XI are in complex with their cofactor, HK.
Activation of the contact system. Factor XII (FXII) can be activated by negatively charged surfaces such as polyphosphates (polyP) derived from activated platelets or neutrophil extracellular traps (NETs). PK can be activated to kallikrein (Kal) by prolylcarboxylase (PRCP) on endothelial cells. Factor XIIa will also activate PK and thereby allows reciprocal activation, resulting in the generation of additional factor XIIa. Factor XIIa can initiate coagulation via the activation of factor XI. Both PK and factor XI are in complex with their cofactor, HK.
The contact system in health and disease. Activation of the contact system leads to the liberation of BK from HK by kallikrein. BK and its derivatives have important functions in blood pressure regulation, vasodilation, and inflammation. The major inhibitor of the classical complement pathway (C1 esterase inhibitor, C1INH) is also in important regulator of kallikrein and factor XIIa activity.
The contact system in health and disease. Activation of the contact system leads to the liberation of BK from HK by kallikrein. BK and its derivatives have important functions in blood pressure regulation, vasodilation, and inflammation. The major inhibitor of the classical complement pathway (C1 esterase inhibitor, C1INH) is also in important regulator of kallikrein and factor XIIa activity.
BK can be further cleaved after which the various kinins are involved in both acute and chronic inflammatory responses.3 For example, BK can activate the B2 receptor and Toll-like receptor 2, leading to an IFN-γ response in dendritic cells, inducing type 1 immunity in a Trypanosoma cruzi infection model. BK can also activate the B1 receptor in response to tissue injury and inflammation in an IL- and TNF-dependent manner, thereby modulating the immune response.14 Furthermore, contact activation can lead to the release of kininogen-derived antimicrobial peptides, providing a principal first-line defense against invading pathogens.15
Hemorrhagic phenotypes associated with contact factor deficiencies
The only contact factor deficiency that is associated with a bleeding phenotype is factor XI.16 However, the bleeding tendency of factor XI-deficient patients is usually mild and injury induced. Spontaneous bleedings are rare, with the exception of menorrhagia and postpartum hemorrhage, in factor XI-deficient women. Bleeding typically occurs after trauma or surgery, especially when surgery involves tissues with high fibrinolytic activity, such as oral and nasal cavities, tonsils, and the urinary tract. The management of factor XI-deficient patients can be troublesome, though, because the bleeding tendency is unpredictable and not clearly associated with factor XI plasma levels.
Deficiencies of factor XII, PK, and HK are not associated with a hemorrhagic phenotype, not even during extensive surgery or when there is a complete (<1%) deficiency.2 Apparently, these proteins are not necessary for clot formation during normal hemostasis. Paradoxically, these patients have an immense in vitro clotting defect, with prolonged to immeasurable aPTT clotting times. Factor XII is an important factor for the aPTT clotting time and this test requires factor XII autoactivation. However, the molecular basis for factor XII autoactivation in vivo is not known. Nonetheless, patients with a deficiency of factor XII, PK, or HK do not require any form of therapy before surgery despite a prolonged aPTT clotting time.
Hereditary angioedema
The major inhibitor of plasma kallikrein is C1-esterase inhibitor (C1INH), a protease belonging to the serine protease inhibitor (serpin) family. Patients with either a deficiency of C1INH (type 1) or a dysfunctional C1INH protein (type 2) have a disease called hereditary angioedema (HAE). This rare, autosomal-dominant disorder is characterized by life-threatening swelling episodes that can develop suddenly and unexpectedly. Some episodes are accompanied by urticaria. Patients can be treated with IV infusion of recombinant or plasma-derived C1INH concentrates, which shorten the extent and duration of attacks. These substances can also be used as prophylaxis.17 In addition to being an important inhibitor of factor XIIa and kallikrein, C1INH is also the major inhibitor of the proteases C1r and C1s, which belong to the classical complement pathway (Figure 3). Therefore, a deficiency of C1INH or a dysfunctional C1INH protein will lead to uncontrolled activation of the complement and contact system, as well as massive BK release. This BK is responsible for edema formation during an attack; indeed, BK levels are up-regulated during an angioedema episode, whereas BK levels are normal or marginally increased during remission.14 However, the paroxysmal nature of the disorder is not completely understood.
There is a third type of HAE, called type III, which is linked to factor XII,18 resulting in enhanced factor XII enzymatic activity in these patients. However, this activity is not detected in routine coagulation tests, and specialized (genetic) testing is necessary for identification of patients. Several mutations in the factor XII gene have been identified in patients with HAE type III and all of these mutations are in the same factor XII gene region.18-20 This suggests an association between altered processing of the factor XII protein and the disorder. However, how a defective factor XII protein affects BK levels is not understood yet. The fact that not all members of a family with a factor XII mutation are symptomatic suggests that other factors or proteins are involved in HAE type III.
Contact system in thrombosis
As discussed under Hemorrhagic phenotypes associated with contact factor deficiencies, the contact system plays a minor role during hemostasis because the contact factors are not required for fibrin generation and clot formation. However, in recent years, the role of the contact system in thrombosis has regained new interest due to several observations in animal studies in knockout mice, other rodents, and primates. We will summarize the results from knockout mice in the following paragraphs for the individual contact factors. The accompanying chapter by Gailani will highlight the data obtained in other rodents and primates.
Factor XI
Factor XI knockout mice, first described in 1997 by Gailani et al,21 have a comparable phenotype to their wild-type counterpart and a normal reproductive capacity. Despite a severely prolonged aPTT in the knockout strain, no increased bleeding time is present in these mice. Factor XI knockout mice are protected against several forms of artificially induced thrombosis, both arterial and venous.21-24 These developments led to the generation of various factor XI inhibitors, including small-molecule inhibitors, antibodies against factor XI, factor XI antisense oligonucleotides, and “naturally occurring” factor XI inhibitors derived from bats. Without exception, these approaches showed thromboprotective effects in rodent thrombosis models using ferric chloride or vena cava ligation.22-26 For example, inhibitory factor XI antibodies, which prevent the activation of factor XI by factor XII, protected mice from ferric chloride-induced arterial and venous thrombosis.27,28 Furthermore, factor XI and factor XI antisense oligonucleotides have been studied in higher species using a vascular graft occlusion model in primates,29,30 which paved the way for human studies using factor XI antisense oligonucleotides. Human data from patients undergoing total knee replacement surgery are expected this year.
All of the prothrombotic models were performed on mice with a normal, healthy vasculature. However, many thrombotic disorders are caused by atherosclerosis and occur at later age. Recently, we investigated whether factor XI inhibition with antisense oligonucleotides would be successful in reducing thrombus formation in an atherosclerosis mouse model.31 ApoE knockout mice were given a Western-type diet containing 0.25% cholesterol and, after 18 weeks, thrombus formation was induced on atherosclerotic plaques with an ultrasound-induced injury. Factor XI was not involved in platelet plug and initial thrombus formation. However, inhibition of factor XI resulted in less stable cots and less fibrin formation without increased bleeding in this model. This suggests that factor XI inhibition can be a safe alternative, not only for venous thrombosis, but also for thrombus formation in atherosclerotic disorders such as myocardial infarction and stroke.
Factor XII
Since the factor XII-deficient index patient John Hageman died of pulmonary embolism, there has not been much interest in factor XII as an antithrombotic target.32 Therefore, the available data on factor XII is much more limited compared with factor XI. In recent years, however, there is renewed interest in factor XII and its role in thrombosis. In part, this is due to unexpected observations in factor XII-knockout mice. Like humans, these mice have significantly prolonged aPTTs without an obvious bleeding tendency. However, these mice were protected against artificially induced thrombosis, both arterial and venous, in combination with normal bleeding times.33 This led to the development of several inhibitors of factor XII, such as a recombinant infestin-4-based inhibitor. This compound prevented thrombosis in mice using ferric chloride-induced arterial thrombosis34 and it protected mice from lethal pulmonary embolism.35 Furthermore, it prevented thrombus formation on acutely ruptured atherosclerotic plaques in mice,36 suggesting that factor XII-induced coagulation plays a role in atherothrombosis in a similar fashion as factor XI. These results might pave the way for new and safer drugs for patients with stroke or coronary artery disease. Several factor XII-inhibiting antibodies have been developed. Monoclonal 15H8 not only protected mice from arterial thrombosis, but also reduced platelet accumulation and fibrin formation in a primate vascular graft occlusion model.37 Antibody 15H8 inhibited factor XIIa generation, which reduces thrombus formation by decreasing thrombin generation. Interestingly, factor XIa inhibition had a more pronounced effect in these models, which suggests that factor XI might be a superior target for anticoagulation than factor XII.
Another inhibiting factor XII antibody, 3F7, has been developed recently and described by Larsson et al.38 3F7 binds to residues in the factor XIIa enzymatic pocket and blocked experimental thrombosis in mice and rabbits. Furthermore, this antibody proved to be as effective as heparin in preventing fibrin deposition and thrombosis using an extracorporeal membrane oxygenation system in mice and rabbits. Treatment with 3F7 did not impair hemostasis, suggesting that targeting factor XII can be a clinically relevant anticoagulation strategy without inducing a bleeding diathesis.
Recent evidence demonstrated that factor XII can bind directly to fibrinogen, after which factor XII can modulate fibrin structure/elasticity and its susceptibility to clot lysis.39 By inhibiting factor XII, it is therefore possible to affect clot structure directly, which may be an interesting strategy for the treatment of thrombosis.
Factor XII synthesis can also be blocked by antisense oligonucleotides. Similar to what was seen for factor XI, antisense oligonucleotides to factor XII reduced thrombus formation in several mouse thrombosis models in both venous and arterial beds.40 To our knowledge, no human trials have been performed with factor XII-inhibiting agents.
PK
Because PK is essential for factor XII activation, its inhibition should theoretically produce similar results to factor XII inhibition. Indeed, PK antisense oligonucleotides revealed thromboprotective effects in mouse models of chemically and mechanically induced thrombosis.40 Comparable results have been obtained using PK-knockout mice, which indicates that PK inhibition could be a potential target for anticoagulation.41 However, there are some contradictory results: inhibition of plasma kallikrein with different inhibitors produced a prothrombotic state,42 which is a relevant observation for the further development of kallikrein inhibitors.
HK
Knock-down of the murine kininogen gene 1 resulted in a mouse without HK and low-molecular-weight kininogen.43 These mice displayed a delayed time to carotid artery occlusion and normal bleeding times. Furthermore, targeting HK reduced thrombus formation in ischemic vessels and improved cerebral blood in mice, and this was accompanied by a less severe inflammatory response.44
BK receptors
The contact system provides a direct link between coagulation and inflammation. Cleavage of HK by kallikrein produces the vasoactive protein BK, which has several inflammatory effects, but is also involved in thrombosis. Mice deficient for the BK B2 receptor are protected against artificially induced arterial thrombosis, an effect that is probably mediated by the renin-angiotensin system.45,46 These data provide evidence for an anticoagulation strategy targeting BK and its receptors.
Conclusions
The contact pathway has seen a resurgence in interest because of the intriguing observations that knockout mice with deficiencies in one of the contact proteins are protected against thrombosis. These observations led to the development of several compounds targeting the contact pathway. With its minimal role in hemostasis, an approach to target (one of the) contact proteins would constitute an effective and safe strategy for antithrombotic treatment. However, this premise still needs to be established in humans and first results are expected this year. In addition, it will be essential to identify the best target(s) and compound(s) in the years to come.
Disclosures
Conflict-of-interest disclosures: J.C.M.M. has consulted for rEVO Biologics and is an employee of Sanquin. M.L.v.M. declares no competing financial interests. Off-label drug use: None disclosed.
Correspondence
Joost C.M. Meijers, PhD, Department of Plasma Proteins, Sanquin Research, Plesmanlaan 126, 1066 CX Amsterdam, the Netherlands; Phone: 31-20-5123151; Fax: 31-20-5123310; e-mail: j.meijers@sanquin.nl.