Abstract
The increased number of effective therapies and the wider use of combinations that give deeper remissions have resulted in a reassessment of the goals of myeloma therapy. With the advent of new therapeutic strategies and diagnostic tools, achievement of minimal residual disease (MRD)-negative status has become increasingly important, with some even considering it as the primary endpoint for therapy. The level of MRD that is aimed for is a continuous, rather than an absolute variable, with studies in both transplant-eligible and -noneligible patients showing that the level of MRD achieved is predictive of progression-free survival and overall survival, with an improvement in survival of approximately 1 year for each log-depletion in MRD level. The most widely used methods to assess MRD status include flow cytometry and clonality detection, using next-generation sequencing technologies with sensitivity limits of 1:10−3 to 1:10−6. The timing of when to assess MRD depends on the treatment used, as well as the molecular and cytogenetic subgroup of the myeloma itself. It is also becoming clear that the level of MRD negativity, as well as microenvironmental factors, are important prognostically, including the regeneration of normal plasma cells, and the normalization of the immune repertoire. With advances in antibody-based therapy and immunotherapy, the achievement of stable MRD states is now possible for a significant proportion of patients, and is a prerequisite for myeloma cure.
Learning Objectives
To understand the latest data on the prognostic role of achieving minimal residual disease (MRD) states in myeloma
To understand the different methodologies used for MRD assessment in myeloma, their clinical utility, and potential limitations
To understand treatment strategies able to sustain MRD negativity long term
What is the goal of therapy?
The survival of multiple myeloma patients has dramatically improved in the last few decades, moving from a median of approximately 18 months to 72 months, with increasing proportions of long-term survivors, with some patients never relapsing who are effectively cured.1 This improvement is due to an increased number of effective therapies and increased knowledge of how best to combine them together with better supportive care.
One striking feature of the introduction of the novel therapies has been the increase in the complete response (CR) rate, with up to 60% of patients achieving such states as assessed by M component, serum-free light chain ratio, and bone marrow plasma cell numbers.2 As a consequence of the effectiveness and range of therapies, physicians are reassessing their goals for therapy, which are no longer focused on disease stabilization and short-term control, but rather on long-term control, quality of life, and cure. The choice of strategy taken varies depending upon the patient’s age, performance status, and their time in the disease journey (eg, newly diagnosed or relapsed refractory). Thus, in the new world of novel therapies with different mechanisms of actions and the ability to induce deep remissions, perhaps the most important question is whether the achievement of a minimal residual disease (MRD) negativity translates into long-term disease control and cure, and if so, what is the critical level of response that is required?
Methods for assessing disease response
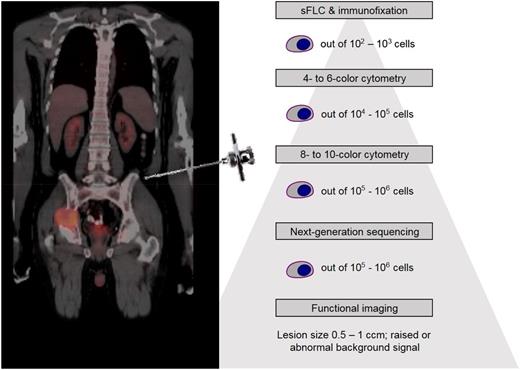
These therapeutic advances have been matched by technological advances in the ability to detect extremely low levels of MRD,2,3 (Figure 1). The most widely used methods for the assessment of MRD are bone marrow flow cytometry or the use of clonality detection with next-generation sequencing (NGS) technologies. These offer practical and reliable approaches to determine the extent of bone marrow involvement and have become ubiquitous assessment tools in clinical trials.3 Reflecting this, the International Myeloma Working Group (IMWG)2 response definitions have been updated to include definitions of standard CR and a number of categories that include the assessment of MRD (Table 1).2
Sensitivity of different techniques for assessing myeloma disease burden.
IMWG response and MRD criteria
| Criteria . | Definition . | |
|---|---|---|
| Standard IMWG response criteria | ||
| Complete response | Negative immunofixation on the serum and urine and disappearance of any soft tissue plasmacytomas and <5% plasma cells in bone marrow aspirate | |
| Stringent complete response | CR as defined above plus normal free light-chain ratio and absence of clonal cells in bone marrow biopsy by immunohistochemistry (ĸ/λ ratio ≤4:1 or ≥1:2 for ĸ and λ patients, respectively, after counting ≥100 plasma cells) | |
| IMWG MRD criteria (requires a CR as defined above) | ||
| Flow MRD-negative | Absence of phenotypically aberrant clonal plasma cells by NGF on bone marrow aspirates using the EuroFlow standard operation procedure for MRD detection in multiple myeloma (or validated equivalent method) with a minimum sensitivity of 1 in 105 nucleated cells or higher | |
| Sequencing MRD-negative | Absence of clonal plasma cells by NGS on bone marrow aspirate in which presence of a clone is defined as less than 2 identical sequencing reads obtained after DNA sequencing of bone marrow aspirates using the LymphoSIGHT/ClonoSEQ platform (or a validated equivalent method) with a minimum sensitivity of 1 in 105 nucleated cells or higher | |
| Imaging plus MRD-negative | MRD negativity as defined by NGF or NGS plus disappearance of every area of increased tracer uptake found at baseline or a preceding PET-CT or decrease to less than mediastinal blood pool standardized uptake value or decrease to less than that of surrounding normal tissue | |
| Sustained MRD-negative | MRD negativity in the marrow (NGF or NGS, or both) and by imaging as defined above, confirmed minimum of 1 y apart. Subsequent evaluations can be used to further specify the duration of negativity (e.g, MRD-negative at 5 y) | |
| Criteria . | Definition . | |
|---|---|---|
| Standard IMWG response criteria | ||
| Complete response | Negative immunofixation on the serum and urine and disappearance of any soft tissue plasmacytomas and <5% plasma cells in bone marrow aspirate | |
| Stringent complete response | CR as defined above plus normal free light-chain ratio and absence of clonal cells in bone marrow biopsy by immunohistochemistry (ĸ/λ ratio ≤4:1 or ≥1:2 for ĸ and λ patients, respectively, after counting ≥100 plasma cells) | |
| IMWG MRD criteria (requires a CR as defined above) | ||
| Flow MRD-negative | Absence of phenotypically aberrant clonal plasma cells by NGF on bone marrow aspirates using the EuroFlow standard operation procedure for MRD detection in multiple myeloma (or validated equivalent method) with a minimum sensitivity of 1 in 105 nucleated cells or higher | |
| Sequencing MRD-negative | Absence of clonal plasma cells by NGS on bone marrow aspirate in which presence of a clone is defined as less than 2 identical sequencing reads obtained after DNA sequencing of bone marrow aspirates using the LymphoSIGHT/ClonoSEQ platform (or a validated equivalent method) with a minimum sensitivity of 1 in 105 nucleated cells or higher | |
| Imaging plus MRD-negative | MRD negativity as defined by NGF or NGS plus disappearance of every area of increased tracer uptake found at baseline or a preceding PET-CT or decrease to less than mediastinal blood pool standardized uptake value or decrease to less than that of surrounding normal tissue | |
| Sustained MRD-negative | MRD negativity in the marrow (NGF or NGS, or both) and by imaging as defined above, confirmed minimum of 1 y apart. Subsequent evaluations can be used to further specify the duration of negativity (e.g, MRD-negative at 5 y) | |
Flow cytometry for MRD detection
Numerous studies have shown the efficacy of flow cytometry to distinguish myeloma plasma cells from normal plasma cells. The most commonly used surface markers include CD138, CD38, CD45, CD56, CD19, and cytoplasmic κ or λ immunoglobulin light chains. Other markers that are aberrantly expressed on myeloma cells include CD20, CD27, CD28, CD81, CD117, and CD200. Given the heterogeneity of expression of these antigens, a panel of antibodies is required to accurately distinguish myeloma cells from normal plasma cells, with 7- or 8-color approaches offering the optimum approaches. The quality of the bone marrow specimen, the number of colors and components of the antibody panel, the number of cells analyzed, the analysis software, and the experience of the laboratory staff, all affect the theoretical analytical sensitivity, with laboratories reporting detection limits of 1 in 103 up to 2 in 1 million, with the recommended 10 million cell acquisitions by the 8-color 2-tube EuroFlow method (including 10 specific antigens).4 An inevitable drawback with the EuroFlow method is increased cost resulting from multiple antibody duplication and labor, which pose barriers for wide clinical adoption of the test outside dedicated centers and for applicability to patients treated outside major clinical trials. For example, in the United States, reimbursement is not provided for the increased cost and effort of implementing this resource-intensive method. To overcome this problem, a recent study shows that a 10-color single-tube MRD method reduces the costs of performing the test (associated with reagents, instrument time, and labor) without losing analytical performance (6 cells in 1 million with at least 3 million cell acquisitions).5 In the absence of standardization of flow cytometry-based MRD assays,6 it is important for clinicians to be aware of the sensitivity of the assay used at their institutions in order to correctly interpret the clinical meaning of the results. Importantly, the recent introduction of therapeutic monoclonal antibodies has forced an adaptation of some flow cytometry panels to recognize different epitopes of CD38 (Table 2).
Comparison of different bone marrow MRD techniques
| Characteristic . | Flow cytometry . | Immunoglobulin NGS . |
|---|---|---|
| Applicability | Nearly 100% | ≥90% |
| Diagnostic sample | Ideally, sample with myeloma present, although abnormal plasma cells can be identified in any sample by their distinct immunophenotypic pattern vs normal plasma cells | Sample with myeloma present (e.g., presentation) required for identification of the dominant clonotype |
| Sample requirements | 2-5 million cells | 1 million cells |
| Sample processing | Requires fresh sample; assessed within 24-48 h | Can use both fresh and stored samples |
| Standardization | Methodology varies between laboratories. Some attempts at standardization (e.g., EuroFlow) | Standardized methodology available from commercial companies. Academic methodologies also available |
| Quantitative | Yes | Yes |
| Sensitivity | 1 in 104 to 1 in 106 | 1 in 105 to 1 in 106 |
| Turnaround and complexity | Hours. Requires skilled flow cytometrist. Automated software available | 1 wk. Bioinformatic analysis available |
| Clonal evolution | Considers all clones with similar phenotype but evolving clone with change in phenotype may not be evaluable | Can take into account all minor clones with infrequent occurrence |
| Availability | Many laboratories with 4 color; 8 or more colors restricted to more specialized centers | One company commercially and a number of academic platforms |
| Characteristic . | Flow cytometry . | Immunoglobulin NGS . |
|---|---|---|
| Applicability | Nearly 100% | ≥90% |
| Diagnostic sample | Ideally, sample with myeloma present, although abnormal plasma cells can be identified in any sample by their distinct immunophenotypic pattern vs normal plasma cells | Sample with myeloma present (e.g., presentation) required for identification of the dominant clonotype |
| Sample requirements | 2-5 million cells | 1 million cells |
| Sample processing | Requires fresh sample; assessed within 24-48 h | Can use both fresh and stored samples |
| Standardization | Methodology varies between laboratories. Some attempts at standardization (e.g., EuroFlow) | Standardized methodology available from commercial companies. Academic methodologies also available |
| Quantitative | Yes | Yes |
| Sensitivity | 1 in 104 to 1 in 106 | 1 in 105 to 1 in 106 |
| Turnaround and complexity | Hours. Requires skilled flow cytometrist. Automated software available | 1 wk. Bioinformatic analysis available |
| Clonal evolution | Considers all clones with similar phenotype but evolving clone with change in phenotype may not be evaluable | Can take into account all minor clones with infrequent occurrence |
| Availability | Many laboratories with 4 color; 8 or more colors restricted to more specialized centers | One company commercially and a number of academic platforms |
Molecular methods for MRD detection
To date, 2 methods have been used for MRD molecular sequencing: allele-specific oligonucleotide-quantitative polymerase chain reaction (ASO-PCR) and NGS. ASO-PCR is a sensitive method but technically cumbersome and time consuming, as it requires sequencing of each patient’s unique immunoglobulin region in the presenting sample and the design of patient-specific primers, which are then applied to follow-up samples. Some of these issues have been overcome by the introduction of NGS techniques that overcome the need for patient-specific primers, instead relying on a bioinformatic approach to identify clonally related cells. The mostly widely used of these approaches has been the Sequenta/Adaptive platform (LymphoSIGHT/ClonoSEQ) that analyzes the unique clonotypic immunoglobulin region using multiple primers that recognize the IgH-VDJH, IGH-DJH, or IgK regions. Once amplified, the gene is sequenced and the frequency of clonotypic reads determined. The test can reach sensitivities of up to 1 in 106 (Table 2).
Imaging methods for MRD detection
Myeloma is a patchy disease and the more widespread use of functional whole-body imaging techniques,7,8 such as positron emission tomography (PET-CT) and diffusion-weighted magnetic resonance imaging (DW-MRI), have highlighted the problem of spatial heterogeneity, where the bone marrow examination is negative but a positive lesion is seen elsewhere in the skeleton. Ongoing studies are examining the sensitivity of such techniques in comparison with flow cytometry and sequencing analysis of the bone marrow; however, it seems most likely that both a bone marrow and whole-body imaging will be required to accurately assess remission status.
Level of MRD negativity
Importantly, the level of MRD negativity is a continuous rather than an absolute variable and studies have shown that when using flow cytometry, the level of MRD negativity achieved is predictive of outcome, with an additional improvement in survival for each log depletion in MRD-negativity level.9 More recent studies using a combination of flow cytometry with a sensitivity of 104 to 105, a more sensitive flow cytometry panel [sometimes referred to as next-generation flow cytometry (NGF)] with a sensitivity of 105 to 106, or NGS have shown that even at these very low levels of disease, the lower the level of MRD negativity the better the outcome, with cut-points of 1:10−6 postulated to be the best. For example, 25% of patients classified as negative by 8-color flow cytometry were shown to be positive by NGF, and these cases had a shorter progression-free survival (PFS) than cases classified as negative by both techniques.4
Prognostic implications of attainment of MRD negativity
A large number of studies have looked at the prognostic significance of achieving a MRD-negative state (Table 3) and 2 meta-analyses have recently been performed, which summarize and take into account the different trial designs and statistical methodologies used in the studies.26,27
Selected studies of MRD assessment in myeloma
| Study* . | Treatment arms . | Test method . | % MRD negative . | Outcomes (MRD-negative vs MRD-positive) . |
|---|---|---|---|---|
| Paiva et al.10 | Six alternating cycles of VBMCP and VBAD, followed by ASCT (n = 577) | Four-color flow cytometry | 42% | Median PFS 71 mo vs 37 mo (P < .001) |
| Median OS not reached vs 89 mo (P = .002) | ||||
| Paiva et al11 | Six cycles of VMP or VTP (n = 102) | Four-color flow cytometry | 30% | Median PFS not reached vs 35 mo (P = .02) |
| Median OS not significantly different | ||||
| Korthals et al.12 | Idarubicin or dexamethasone plus ASCT (n = 53) | ASO-PCR | 49% | Median EFS 35 mo vs 20 mo (P = .001) |
| Median OS 70 mo vs 45 mo (P = .04) | ||||
| Paiva et al.13 | Conv chemo or TD or VTD and ASCT (n = 241) | Four-color flow cytometry | 74% of BM CR | PFS 86% vs 58% at 3 y (P < .001) |
| OS 94% vs 80% at 3 y (P = .001) | ||||
| Rawstron et al.14 | CVAD or CTD plus ASCT (n = 378) | Six-color flow cytometry | 62% | Median PFS 28.6 mo vs 15.5 mo (P < .001) |
| Median OS 80.6 mo vs 59 mo (P = .018) | ||||
| Rawstron et al.14 | MP vs CTD (n = 245) | Six-color flow cytometry | 15% | Median PFS 10.5 mo vs 7.4 mo (P = .1) |
| Martinez-Lopez et al.15 | VBMC or VBAD induction therapy plus ASCT or 6 cycles of VMP or VTP (n = 133) | NGS | Median TTP 80 mo vs 31 mo (P < .0001) | |
| Median OS not reached versus 81 mo (P = .02) | ||||
| Puig et al.16 | VBMC or VBAD induction therapy plus ASCT or 6 cycles of VMP or VTP (n = 170) | ASO-PCR | 47% | VBMCP or VBAD induction therapy plus HDT–ASCT: median PFS 54 mo vs 27 mo (P = .001); OS not significantly different 6 cycles of VMP or VTP: median PFS not reached versus 31 mo (P = .029); OS not significantly different |
| Roussel et al.17 | VRD plus ASCT plus VRD plus Len (n = 31) | Seven-color flow cytometry | 68% | PFS 100% vs 30% at 3 y |
| Ferrero et al.18 | VTD plus ASCT (n = 39) | ASO-PCR | — | OS 72% vs 48% at 8 y (P = .0041) |
| Korde et al.19 | KRD (n = 45) | NGS | — | PFS 100% vs 79% at 12 mo (P < .001) |
| Ludwig et al.20 | VTD ± C (n = 42) | Four-color flow cytometry | 80% of BM CR | Median PFS not reached vs 38.6 mo (P = .085) |
| Avet-Loiseau et al21 | VD or RD ± Daratumumab (n = 474, n = 557) | NGS | 0.8%–9.8% | MRD-negative patients experienced fewer progression events than MRD-positive patients |
| Oliva et al.22 | Induction plus VMP, CRD, or ASCT, followed by Len (n = 105) | ASO-PCR | 45% | Median PFS not reached vs 48.8 mo (P = .01) |
| Paiva et al.23 | Alternating VMP plus RD (n = 162) | NGF | 34% | Median TTP not reached vs 15 mo OS 70% vs 55% at 3 y |
| de Tute et al.24 | CTDa or RCDa = /− Len (n = 297) | Six-color flow cytometry | 13.8% (10.8%–16.0%) | Median PFS 34 mo vs 18 mo (P < .0001) |
| Attal et al.25 | VRD ± ASCT plus VRD plus Len (n = 543) | Seven-color flow cytometry | 65%–79% | MRD-negative patients experienced longer PFS than MRD-positive patients (adjusted HR 0.30 P < .001) |
| MRD-negative patients experienced longer OS than MRD-positive patients (adjusted HR 0.34 P < .001) |
| Study* . | Treatment arms . | Test method . | % MRD negative . | Outcomes (MRD-negative vs MRD-positive) . |
|---|---|---|---|---|
| Paiva et al.10 | Six alternating cycles of VBMCP and VBAD, followed by ASCT (n = 577) | Four-color flow cytometry | 42% | Median PFS 71 mo vs 37 mo (P < .001) |
| Median OS not reached vs 89 mo (P = .002) | ||||
| Paiva et al11 | Six cycles of VMP or VTP (n = 102) | Four-color flow cytometry | 30% | Median PFS not reached vs 35 mo (P = .02) |
| Median OS not significantly different | ||||
| Korthals et al.12 | Idarubicin or dexamethasone plus ASCT (n = 53) | ASO-PCR | 49% | Median EFS 35 mo vs 20 mo (P = .001) |
| Median OS 70 mo vs 45 mo (P = .04) | ||||
| Paiva et al.13 | Conv chemo or TD or VTD and ASCT (n = 241) | Four-color flow cytometry | 74% of BM CR | PFS 86% vs 58% at 3 y (P < .001) |
| OS 94% vs 80% at 3 y (P = .001) | ||||
| Rawstron et al.14 | CVAD or CTD plus ASCT (n = 378) | Six-color flow cytometry | 62% | Median PFS 28.6 mo vs 15.5 mo (P < .001) |
| Median OS 80.6 mo vs 59 mo (P = .018) | ||||
| Rawstron et al.14 | MP vs CTD (n = 245) | Six-color flow cytometry | 15% | Median PFS 10.5 mo vs 7.4 mo (P = .1) |
| Martinez-Lopez et al.15 | VBMC or VBAD induction therapy plus ASCT or 6 cycles of VMP or VTP (n = 133) | NGS | Median TTP 80 mo vs 31 mo (P < .0001) | |
| Median OS not reached versus 81 mo (P = .02) | ||||
| Puig et al.16 | VBMC or VBAD induction therapy plus ASCT or 6 cycles of VMP or VTP (n = 170) | ASO-PCR | 47% | VBMCP or VBAD induction therapy plus HDT–ASCT: median PFS 54 mo vs 27 mo (P = .001); OS not significantly different 6 cycles of VMP or VTP: median PFS not reached versus 31 mo (P = .029); OS not significantly different |
| Roussel et al.17 | VRD plus ASCT plus VRD plus Len (n = 31) | Seven-color flow cytometry | 68% | PFS 100% vs 30% at 3 y |
| Ferrero et al.18 | VTD plus ASCT (n = 39) | ASO-PCR | — | OS 72% vs 48% at 8 y (P = .0041) |
| Korde et al.19 | KRD (n = 45) | NGS | — | PFS 100% vs 79% at 12 mo (P < .001) |
| Ludwig et al.20 | VTD ± C (n = 42) | Four-color flow cytometry | 80% of BM CR | Median PFS not reached vs 38.6 mo (P = .085) |
| Avet-Loiseau et al21 | VD or RD ± Daratumumab (n = 474, n = 557) | NGS | 0.8%–9.8% | MRD-negative patients experienced fewer progression events than MRD-positive patients |
| Oliva et al.22 | Induction plus VMP, CRD, or ASCT, followed by Len (n = 105) | ASO-PCR | 45% | Median PFS not reached vs 48.8 mo (P = .01) |
| Paiva et al.23 | Alternating VMP plus RD (n = 162) | NGF | 34% | Median TTP not reached vs 15 mo OS 70% vs 55% at 3 y |
| de Tute et al.24 | CTDa or RCDa = /− Len (n = 297) | Six-color flow cytometry | 13.8% (10.8%–16.0%) | Median PFS 34 mo vs 18 mo (P < .0001) |
| Attal et al.25 | VRD ± ASCT plus VRD plus Len (n = 543) | Seven-color flow cytometry | 65%–79% | MRD-negative patients experienced longer PFS than MRD-positive patients (adjusted HR 0.30 P < .001) |
| MRD-negative patients experienced longer OS than MRD-positive patients (adjusted HR 0.34 P < .001) |
Abbreviations: ASCT, high-dose (chemo) therapy and autologous stem-cell transplantation; ASO-PCR, allele-specific oligonucleotide PCR; BM, bone marrow; CTD, cyclophosphamide, thalidomide, and dexamethasone; CVAD, cyclophosphamide, vincristine, Adriamycin, and dexamethasone; EFS, event-free survival; HR, hazard ratio; KRD, kyprolis revlimid, dexamethasone; Len, lenalidomide; MP, melphalan and prednisolone; MRD, minimal residual disease; NGF, next-generation flow cytometry; NGS, next-generation sequencing; OS, overall survival; PFS, progression-free survival; RCDa, revlimid, cyclophosphamide and dexamethasone (attenuated); TD, thalidomide and dexamethasone; TTP, time to progression; VRD, velcade revlimid, dexamethasone; VBAD, vincristine, carmustine, adriamycin, and dexamethasone; VBMCP, vincristine, carmustine, melphalan, cyclophosphamide, and prednisone; VMP, bortezomib, melphalan, and prednisone; VTD, velcade, thalidomide, and dexamethasone; VTP, bortezomib, thalidomide, and prednisone.
I apologize that I am only able to mention a small number of the studies concerning MRD in myeloma. I would like to acknowledge the work of all of my colleagues who have contributed to the knowledge of MRD in myeloma.
Newly diagnosed transplant-eligible
The prognostic value of achieving a MRD-negative state is well established in the setting of newly diagnosed patients undergoing autologous transplantation. All studies show that patients who achieve a MRD-negative state have a PFS of at least twice that of patients who are in a MRD-positive CR and, in many cases, the prognostic value of MRD also translates into an improvement in overall survival (OS).
There is still some debate as to whether all MRD-negative CRs are the same (ie, asking the question: Does the treatment method used to achieve a MRD negative CR make any difference to the length of the CR?). Recent results from the United Kingdom and French studies suggest it is the level of response that is important, but the results need to be interpreted in the context of the treatments used in these studies. In the Dana-Farber Cancer Institute (DFCI)-Intergroupe Francophone Du Myelome (IFM) study comparing the role of transplant in the era of proteasome/immunomodulatory drugs (IMiD) induction, consolidation, and maintenance, more patients in the transplant arm achieved a MRD-negative state; however, the PFS was similar for patients achieving MRD negativity regardless of the treatment arm.28 Similar results were seen in a United Kingdom Medical Research Council study comparing conventional chemotherapy to IMiD prior to transplantation where, although more patients achieved MRD negativity with the IMiD-based induction, the outcome was similar for patients achieving MRD negativity regardless of the induction regimen used.29 Thus, both studies highlight that achieving MRD negativity is important, and that there is up to a threefold difference in the ability of some regimens to achieve this. Therefore, choosing the regimen that increases the chance of achieving MRD negativity is crucially important clinically. These types of data also raise questions as to whether patients should receive sequential therapies with multiple mechanisms of actions to increase the chance of achieving a MRD-negative state, and therefore improve long-term outcomes.
Newly diagnosed nontransplant-eligible
Initially, the value of MRD assessment in the older less-fit patient was unclear, as few patients achieved such responses because it was thought that these were confined to patients receiving intensive high-dose approaches. The introduction of proteasome inhibitors and IMiDs changed this, with the value of MRD detection in nontransplant-eligible patients having been recognized, and it has now been clearly shown that MRD negativity is associated with longer survivals.11,16,29
Maintenance therapy
The role of MRD in the maintenance setting has been evaluated and, in the early Medical Research Council studies comparing thalidomide maintenance to observation, MRD-positive patients randomized to the maintenance arm were associated with a significantly longer PFS compared with the placebo arm. In the MRD-negative patients, a similar trend was observed,14 suggesting that both the attainment of MRD and ongoing therapy may be important in long-term disease control.30
Relapse regimens
The complete response rate for therapy at relapse has increased following the introduction of the novel agents and the more widespread use of triplet therapies. Many of the agents approved by the Food and Drug Administration in the last 18 months have used MRD as a secondary or exploratory end point in their pivotal phase 3 trials (eg, Aspire, Endeavor, Castor, Pollux, Eloquent, and Tourmaline). A good example of this are the MRD data derived from the Castor and Pollux studies, which explored novel agent combinations with daratumumab and used NGS with a sensitivity of 105 to show that more patients achieve a MRD-negative status when novel agents are combined with Daratumumab, and show that patients who achieved a MRD-negative status had fewer PFS events compared with MRD-positive patients.21
Timing and durability of assessment
It is known that myeloma is a collection of molecular distinct clinical entities with unique biological characteristics. It has also been shown that there are profound differences in the time to maximum response and the level of response, depending on cytogenetic risk status and molecular subtype. Patients in the t(11;14) CD20+ (CD2 subgroup) or hyperdiploid subgroup take longer to respond to therapy, with improvements in responses still being seen up to 3 years after presentation.1,31,32 Consequently, the timing of MRD assessment and the molecular subtype of disease are essential items of information for the clinical interpretation of MRD data. This observation highlights the importance of using defined time points for comparison of MRD results across trials and in future to incorporate a breakdown of data by molecular subgroups.
In many of the studies published to date, different time points have been used for the analysis of MRD, including after 6 to 8 cycles of therapy, at the end of induction chemotherapy, 100 days posttransplant, and during maintenance therapy. Despite these differences in timing, the attainment of MRD remains prognostically significant. For example, patients treated with the total therapy approach who achieve at least a very good partial response, who were assessed for MRD at 24 months, showed that patients who were MRD-negative at this time point had an improved outcome, with 83% remaining relapse-free at 5-years follow-up compared with 57% of patients with detectable residual disease (P = .04). In addition, when MRD-negative status was achieved, this was associated with a significantly better 5-year OS rate, with 93% still alive compared with only 64% of patients who were MRD-positive (P = .009).32
In some instances a number of time points have been assessed (eg, pre- and posttransplant or posttransplant and during maintenance). For all studies, the number of patients who achieve a MRD-negative state increases with time. For example, early studies using 4-color flow cytometry showed patients who were MRD-negative both pre- and posttransplant had a longer PFS than those who were MRD-positive before and MRD-negative after or positive at both time points. Importantly, patients who have a sustained MRD state have a better outcome.26
Discordant results between technologies
Results of MRD with different technologies (eg, M component response, flow cytometry, molecular and imaging responses) can be discordant. There are a number of possible explanations for this, including the half-life of M components that disappear over a prolonged time compared with the relatively rapid induction of apoptosis, which is seen in bone marrow assessments.11 A number of groups have now compared the results obtained from flow cytometry and molecular testing by ASO-PCR or NGS, with discordance being seen in 12% to 15% of patients, presumably due to differences in the sensitivities of the techniques.15,16,33
The impact of high-risk status
Numerous studies have identified a number of genetic features in high-risk, including the presence of t(4;14), t(14;16), t(14,20), 1q+, 1p−, and 17p−. These patients characteristically achieve a rapid response; however, it is not sustained. Despite this, the achievement of a MRD-negative state in high-risk patients still has prognostic significance. In the United Kingdom Myeloma IX study, there was no difference in the proportion of patients achieving MRD negativity when comparing those with high-risk and standard-risk genetics. However, when outcome was assessed in the high- and standard-risk subgroup, MRD status was predictive of PFS (standard-risk subgroup MRD-positive 33.7m vs 44.2m in MRD-negative, P = .014; high-risk subgroup MRD-positive 9.7m vs 15.7m in MRD-negative, P = .009).14 The Spanish data are in keeping with this observation, with the presence of baseline high-risk genetics and persistent MRD at day +100 posttransplant being associated with early relapse.13 A recent study has suggested that the significance of MRD may depend on the genetic abnormalities present, with patients who were MRD-negative with a t(4;14) having a longer PFS and OS compared with those who were MRD-positive, whereas in patients with a 17p− or more than 2 abnormalities, the depth of response did not translate into an improved outcome.34
In gene-expression profiling (GEP), defined high risk achieving MRD negativity is also significantly associated with an improved prognosis. In the University of Arkansas for Medical Sciences-based total therapy studies, patients who are GEP70 high risk and MRD-positive had a dismal outcome, with 2-year PFS and OS of 33% and 52%, respectively. However, patients who achieve MRD negativity by 2 years had a better outcome, with 41% of patients remaining relapse-free and 58% being alive at 5 years.35
Using MRD to detect relapse
Serial MRD analysis has been used to predict clinical relapse in myeloma. Using ASO-PCR to assess MRD over time, a change in MRD status from negative to positive was seen to predate clinical relapse. Unfortunately, the routine use of this approach is hampered by the need for frequent bone marrow aspirate and biopsy. The rate of relapse will also impact on the value of such an approach, with a negative bone marrow MRD result being possible before a fast clinical relapse.
Other confounding factors include data from recent imaging studies that highlight the spatial heterogeneity of myeloma, with some patients relapsing with a morphologically clear bone marrow but the presence of a plasmacytoma or focal lesions on functional imaging at a site other than where the bone marrow biopsy was performed. It remains unclear whether more-sensitive analysis of the patient’s bone marrow could detect early relapse or whether very sensitive MRD assessment of the blood, which could be performed more frequently, has the potential as a monitoring test.
Should MRD negativity be a treatment endpoint?
Generally, response rates are higher with triplet regimens compared with doublet regimens, and are increased further by the addition of transplantation. Different treatment phases (eg, induction, transplantation, consolidation, and maintenance) using drugs with different mechanisms of action, which serially increase response rates over time, are now routinely used at many academic centers. Moving forward, taking this approach and treating to a MRD-negative state is plausibly the initial aim of treatment, which will translate to increased numbers of cures. This approach will aim to personalize care based on an individual’s myeloma biology (eg, genetics and molecular subtype), response to a particular agent (response-adapted therapy), as well as taking account of patient factors (eg, fitness, side effects, and so forth). Although some general principles can be applied across all patients groups, the frequency of MRD assessment will depend on the patient’s molecular subgroup, risk group, and rate of response to therapy. Using this approach, the components of therapy and the length of treatment of an individual patient will be adjusted to achieve a sustained MRD state, leading to improved cure rates.
An interesting question that is always raised around the role of MRD assessment surrounds stopping therapy for patients who become MRD-negative. The real question in this setting, however, should be whether these patients are truly disease-free, whether they still have disease present below the sensitivity of our tests, or whether they are positive at other sites in the bone marrow. Thus, such patients should be continued on treatment, as they are responding well and potentially have the best clinical outcomes. If the goal of therapy is to cure myeloma, then the most appropriate question is, what should we do to improve outcomes for patients who are MRD-positive postinitial therapy?
Currently, the most commonly used MRD assessments are bone marrow-based and analyzed from a single aspirate site. In order to overcome some of the errors introduced by this single-site approach, a number of peripheral blood technologies examining both peripheral myeloma cells and cell-free approaches are being explored.36-40 These offer great potential. However, at present they require a relatively large sample to be drawn and are not able to detect disease to the same level of sensitivity as a bone marrow assessment. It is expected over the coming years that improvements in sequencing technology will enable such approaches to attain greater levels of sensitivity and to be used routinely in clinical practice. The ability to monitor MRD more frequently using such approaches will increase MRD’s general applicability and this ease of use will lead to its general uptake. Ongoing studies are also looking at MRD in the context of whole-body imaging3,7,8 (PET-CT or DW-MRI) to determine the relative sensitivity levels and value of each test.
Ongoing work is determining the nature of the residual cells following therapy, as this information will be important in designing future therapeutic strategies. It is reasonable to assume that the MRD cells have a drug-resistant phenotype, as they have persisted following therapy.41 Whether this is a temporary resistant state (eg, the cells are quiescent or dormant and therefore unresponsive to therapy) or permanent (ie, truly drug resistant due to the downregulation of the drug target) is unknown. However, this residual population of cells must contain myeloma-propagating cells, which later lead to relapse.
It is also becoming clear that a number of bone marrow microenvironmental factors, as well as the level of MRD, are important in determining long-term disease control. For example, patients who achieve MRD negativity with the regeneration of normal plasma cell numbers and normal immunoglobulin levels have a better prognosis than those patients who are MRD-negative but fail to regenerate normal levels.14 Early results suggest a similar phenomenon, with normalization of the immune repertoire and normalization of the gene expression of the bone marrow microenvironment, and that they are important factors in addition to MRD level in predicting prognosis.42 This will become critical information as we explore ways of therapeutically manipulating the microenvironment and immune system.
Conclusions
Inducing deep sustainable remissions is a prerequisite to a cure for myeloma. With the advances in therapy targeting the myeloma cell itself, as well as the microenvironment and the immune system, achieving minimal residual disease states is now possible. Data clearly support the prognostic value of MRD, with patients achieving a MRD-negative state having improved PFS and OS. Outstanding questions moving forward include determining what level of MRD is required (the assumption being the lower the better), whether additional therapy should be offered to patients who do not achieve a MRD-negative state, and how long patients should continue therapy once they have achieved a sustained MRD-negative state. Ongoing clinical trials are designed to answer these questions as we aim to translate the increasing number of molecular remissions into a cure.
Correspondence
Faith E. Davies, Myeloma Institute, University of Arkansas for Medical Sciences, 4301 West Markham St, Little Rock, AR 72205; e-mail: fedavies@uams.edu.
References
Competing Interests
Conflict-of-interest disclosure: The author has consulted for and received honoraria from Celgene, Takeda, Bristol-Myers, AMGEN, and Seattle Genetics.
Author notes
Off-label drug use: None disclosed.