Abstract
Myelofibrosis (MF) is a heterogeneous disorder characterized by splenomegaly, constitutional symptoms, ineffective hematopoiesis, and an inherent risk of leukemic transformation. The past decade has seen a massive shift in available therapeutic options for our patients and we are learning how and when to use novel agents, either alone or in combination, during the disease course. This has translated into improved management of splenomegaly, significant amelioration in disease-related symptom burden for many, and may lead to improved survival. But limitations in the therapeutic options remain. Moreover, enhanced delineation of the mutational landscape of MF has offered both increasingly complex prognostic algorithms and yielded further potential therapeutic avenues. In this review, we will focus on stratifying both standard and experimental therapeutic management in 2017 and 2018 and postulate on the emerging treatments that will likely become part of our increasingly complex treatment algorithm.
Learning Objectives
Identify key efficacy and limitations of ruxolitinib therapy
Appreciate the range of different therapeutic targets and which patients may be good candidates for such therapies
Introduction
Myelofibrosis (MF) has the worst prognosis of the myeloproliferative neoplasms (MPNs) and is a complex disorder. Before 2011, treatment options for MF were limited to either allogeneic transplant or palliation. We discuss here current treatment algorithms for MF using patient cases. We manage patients with MF in the same manner regardless of whether they have primary MF, or so-called secondary MF arising from essential thrombocythemia (post-ET MF) or polycythemia vera (post-PV MF).
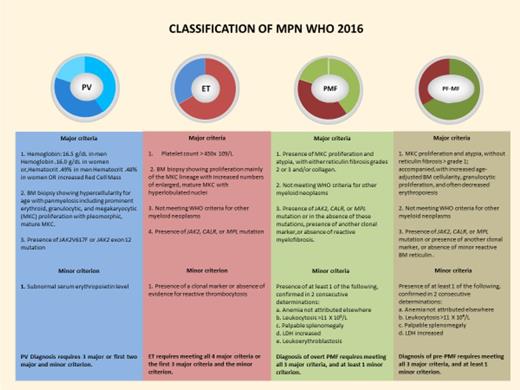
In 2016, the World Health Organization (WHO) revised the diagnostic criteria for MPN, focusing on the interface between ET and PV and between ET and primary myelofibrosis (PMF). In this revision, prefibrotic MF was identified as an entity independent of ET and PMF (Figure 1).1 An accurate diagnosis is critical to the management of MF, but in the earlier stages may be difficult to easily differentiate from ET; likewise, the advanced stage of disease may be difficult to discriminate from disorders such as fibrotic myelodysplasia and chronic myelomonocytic leukemia (CMML). There is a need to focus on so-called triple negative (TN) disease (ie, lacking JAK2, MPL, or CALR mutations). The WHO suggests screening for additional nondriver mutations. It is important to bear in mind that normal elderly individuals may demonstrate age-related clonal hematopoiesis, as they would myelodysplasia or chronic myelomonocytic leukemia.
Classification of MPNs as adapted from the WHO 2017 criteria.1 LDH, lactate dehydrogenase; MKC, megakaryocyte. 2016 WHO grading of myelofibrosis: MF-0, scattered linear reticulin with no intersections (crossovers) corresponding to normal bone marrow; MF-1, loose network of reticulin with many intersections, especially in perivascular areas; MF-2, diffuse and dense increase in reticulin with extensive intersections, occasionally with focal bundles of thick fibers, mostly consistent with collagen and/or focal osteosclerosis; MF-3, diffuse and dense increase in reticulin with extensive intersections and course bundles of thick fibers consistent with collagen, usually associated with osteosclerosis.
Classification of MPNs as adapted from the WHO 2017 criteria.1 LDH, lactate dehydrogenase; MKC, megakaryocyte. 2016 WHO grading of myelofibrosis: MF-0, scattered linear reticulin with no intersections (crossovers) corresponding to normal bone marrow; MF-1, loose network of reticulin with many intersections, especially in perivascular areas; MF-2, diffuse and dense increase in reticulin with extensive intersections, occasionally with focal bundles of thick fibers, mostly consistent with collagen and/or focal osteosclerosis; MF-3, diffuse and dense increase in reticulin with extensive intersections and course bundles of thick fibers consistent with collagen, usually associated with osteosclerosis.
Early assessment of patients with MF encompasses assessment of vascular risk, comorbidities, comprehensive symptom assessment, and prognosis; although spleen size does not directly affect prognosis, our preference is to document this carefully. To determine symptoms, a robust reproducible tool is preferred because the presence and type of symptoms affects both the choice of therapy and monitoring of response; thus, we use a standardized version of the MPN symptom assessment form (MPN-SAF).2 Several prognostic scores have been validated in large patient cohorts, including the International Prognostic Scoring System (IPSS), dynamic IPSS (DIPSS), and DIPSS-plus. These scores do not perform as well for patients with post-ET or post-PV MF, and alternative scores such as the Myelofibrosis Secondary Prognostic Model may be of utility here (reviewed in Rumi and Cazzola3). Increasingly, data regarding additional nondriver mutations (so-called high molecular risk [HMR]), in particular, ASXL-1, EZH2, IDH1/2, or SRSF2 or cytogenetic abnormalities, are used to refine prognosis.3 Conventionally, these are used to aid decisions regarding eligibility for stem cell transplant (discussed later in this article). More recently, based on a cohort of 344 PMF patients, a prognostic score based on only age, driver mutation, TN status, and JAK2 allele burden was proposed.4 This score requires validation and has the advantage of not requiring more extensive mutational testing; however, a disadvantage is that it does not seem to identify the very low-risk group in the same way that the MIPSS does.3
In 2013, MF response criteria were revised by the International Working Group for Myelofibrosis Research and Treatment and European Leukemia Net to include symptom response and stricter definitions of red blood cell transfusion dependency and independency.3 Morphological remission in bone marrow is required for complete response (CR); criteria for partial response requires morphologic remission in the peripheral blood (not the bone marrow) and includes those otherwise meeting CR criteria but with inadequate blood count recovery. The revised response criteria also include categories for cytogenetic and molecular remission. However, interestingly, these are not required for CR assignment. Three other response categories (anemia, spleen, and symptoms) have also been included. Symptom response requires a ≥50% reduction in the MPN-SAF-Total Symptom Score (MPN-TSS). Spleen response is based on imaging and requires that a ≥35% reduction in spleen volume confirmed by magnetic resonance imaging or computed tomography scan. Additional criteria are also included for clinical improvement, progressive disease, stable disease, and relapse. These criteria are both complex and very stringent and are predominantly designed for clinical trials only rather than for routine clinical application.
Management of PF MF
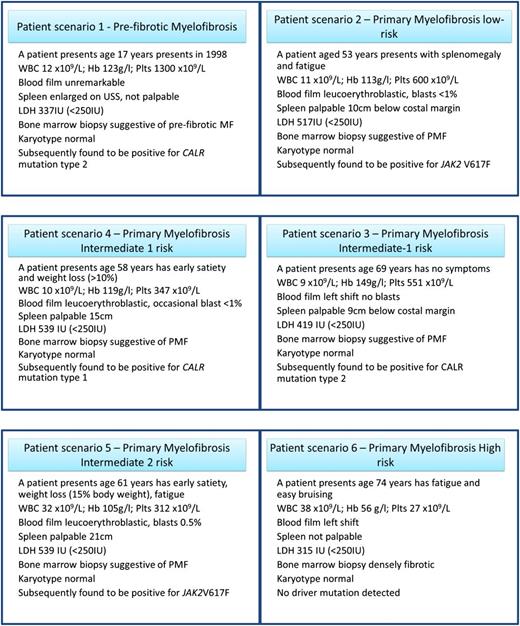
Case 1 displays typical features of prefibrotic MF (PF-MF). Currently, for any patients, but especially for a patient age 17 years, this diagnosis raises a difficult management conundrum (Figure 2). PF-MF has been shown to have a worse prognosis and disease-related complication rate than ET. For example, in a large international study, there was a higher rate of major bleeding episodes in patients with PF-MF compared with WHO-confirmed ET, particularly when those individuals were receiving aspirin.5 However, although PF-MF has an inferior prognosis to ET, when compared with established PMF, the prognosis of PF-MF appears better. In a recent study, Guglielmelli et al6 reported that, compared with PMF, PF-MF was less frequently associated with anemia, thrombocytopenia, leukopenia, higher blast count, symptoms, large splenomegaly, unfavorable karyotype, and high-risk mutations. Median survival was significantly shortened in PMF (7.2 vs 17.6 years), with TN for driver mutations and presence of HMR mutations representing independent predictors of unfavorable outcome. No treatment recommendations exist specifically for PF-MF.
In our institution, we treat these patients as low-risk MF, but are also mindful of the phenotypic similarity to ET and thus consider carefully whether thrombocytosis or leukocytosis should be treated. This patient was asymptomatic; thus, a watchful waiting strategy could be used, and there should be some consideration to low-dose aspirin. However, this is a young patient with a CALR mutation and, in patients with ET, there is evidence against the use of aspirin in such a situation because of a higher risk of hemorrhage.7 There is also variable practice with regard to screening for von Willebrand disease, as demonstrated in an elegant series of patient cases.8 If treatment of the thrombocytosis was considered hydroxycarbamide/hydroxyurea could be an option; alternatively, interferon-α (IFN-α) has been evaluated in small series of patients with MF. In a retrospective study of 62 patients with early MF treated with pegylated-IFN-alfa-2a, improvements in constitutional symptoms, resolution of thrombocytosis, and leukocytosis was observed in 82%, 83%, and 69% of patients, respectively, and a reduction of splenomegaly was seen in 46.5% of patients.9 In a prospective study of 30 MF patients (22 low risk and 8 intermediate-1 risk), 2 achieved CR, 9 partial remission, 4 clinical improvement, 7 stable disease, 3 progressive disease, 1 relapsed, and 4 died. There was no correlation between treatment response and baseline driver mutations or DIPSS scores. Of 8 poor responders, 3 had ASXL1 or SRSF2 mutations. The authors concluded that early treatment with IFN-α in patients without HMR mutations may prevent the development of marked splenomegaly, anemia, and florid myelofibrosis.10
Patient case data. Hb, hemoglobin; plts, platelets; WBC, white blood cells.
We offer IFN-α or hydroxycarbamide for patients with PF-MF, but emphasize the lack of data supporting its routine use in this setting and closely observe any patients choosing such treatment of toxicity. There are ongoing studies of ruxolitinib in combination with IFN-α and a study of Peginvera in MF.
Management of low-risk PMF
The patient in case 2 has low-risk disease but complains of fatigue, the most prevalent symptom for patients with MPN and clinicians may feel they have little to offer in terms of effective management. Data collected from large numbers of patients suggest that multiple factors may contribute to fatigue, including lifestyle factors and mood disorders; these should be addressed as much as possible. There is interest in complementary therapeutic modalities such as yoga to manage this symptom. Concerning the use of ruxolitinib to manage fatigue in such a patient, the phase 3 trials did not include low-risk disease, and furthermore fatigue is a reported side effect of this drug. However, a retrospective study of ruxolitinib treatment in 108 patients with 25 patients having low-risk MF and 83 patients having intermediate-1 risk MF reported that patients with low-risk MF experienced a substantial improvement in both splenomegaly and constitutional symptoms. The proportion with moderate or severe fatigue decreased from 90% at diagnosis to 37% at time of best response to ruxolitinib.11
For case 2, we would assess for other reversible causes of fatigue and then refer to a multidisciplinary service including psychology, physiotherapy, dietitian, and occupational therapy. We also find the analysis of the MPN-SAF-TSS or MPN-10 score useful; threshold analyses suggest that either a TSS of 22 or more or an individual score of 5 is useful.
MF is a progressive disease; for example, in 1 study after 1 year, the proportion of patients with anemia rose from 38% to 64% and thrombocytopenia 18% to 31%.12 Whether any intervention could delay progression is unclear. Risks of progressive anemia, progression to acute myeloid leukemia and worsened overall survival have been linked to driver mutation status (TN patients faring worst) and the presence of so-called HMR mutations, as discussed previously. One agent for consideration in this patient scenario is IFN-α as discussed above; the second is ruxolitinib. The phase 3 Study Investigating the Efficacy and Safety of Ruxolitinib in Early Myelofibrosis Patients With High Molecular Risk Mutations (NCT02598297) was designed to evaluate the benefit of ruxolitinib in improving progression-free survival in patients with low-risk disease and an HMR mutation. Unfortunately, this study has been stopped due to difficulty enrolling sufficient patients; hence, the efficacy of JAK inhibitor (JAKi) therapy in this patient population remains unknown.
Treatment algorithms for intermediate-1 risk MF (scenarios 3 and 4)
We consider intermediate-1 risk MF highly heterogeneous, with some patients falling into this category by virtue of having advanced age (>65 years, per case 3) and others with features of more major clinical concern, such as weight loss (case 4). Considerations for these cases would be like those previously discussed. More data exist with regard to considering ruxolitinib for patients with intermediate-1 risk disease; this was recently discussed in some detail in a recent elegant paper by Cervantes and Pereira, although their paper focussed on a patient with intermediate-2 risk.13 However, case 3 was deliberately chosen to illustrate a patient who reaches this prognostic risk group because of age alone. In the absence of symptomatic or rapidly progressive splenomegaly or disease-related symptoms, we do not believe that sufficient evidence exists to use ruxolitinib outside the context of a clinical trial. In contrast, for case 4, we would strongly consider ruxolitinib therapy if weight loss is felt to be due to MF. This case also illustrates a patient in whom we would be actively considering stem cell transplantation (SCT), and would likely ensure cytogenetics and an HMR screen were reviewed. Decision-making here is complex and would be influenced by the availability and quality of a suitable donor; our usual practice would be to move to transplant promptly if HMR or adverse cytogenetics are detected.
Management of intermediate-2 risk MF
Patients with intermediate-2 risk disease have a life expectancy of ∼5 years and usually have disease that significantly encroaches on their quality of life. An active decision regarding suitability for SCT is needed early for such patients and the same considerations we discussed previously for ruxolitinib use apply. Of note in case 5, if the SCT was high risk, for example from recipient comorbidities or poor donor options (mismatched or haploidentical transplant), then cytogenetics or HMR screen could be used to decide whether to proceed more rapidly to SCT regardless of such risks or to wait. However, we also chose to include this case to discuss issues concerning monitoring of disease while using ruxolitinib.
Consider that the patient has been using ruxolitinib with initial excellent response, including a complete resolution of splenomegaly, return to normal weight, and good quality of life. There are no infectious complications. However, after several years, there can be some evidence of disease progression that need to be considered; these might include progressive cytopenia, leukocytosis, increasing blasts, increased disease-related symptoms, development of extramedullary hematopoiesis, or resurgence of splenomegaly either to or beyond baseline. Concerning cytopenia, anemia and thrombocytopenia are the most commonly occurring factors; also important for consideration are other medical conditions (eg, iron deficiency from blood loss), drug–drug interactions, or other evidence of progression such as circulating blasts. There are no accepted criteria for disease progression on ruxolitinib, and many clinical studies of patients with so-called intolerance or progression on ruxolitinib have therefore used broad criteria, making it difficult to compare results and manage individual cases. If there is clear evidence of progressive disease. then a decision regarding the next alternative therapy is required. Options might include SCT, although, as we discuss later, patients who progress even after an initial response to ruxolitinib may have a worse outcome after SCT than those transplanted at the time of best response. Adding a second therapy to control anemia, thrombocytopenia, or leukocytosis (such as recombinant human erythropoietin, danazol, immunomodulatory drugs [IMiDs], or hydroxyurea; Table 1) or ability to switch to an alternative strategy via a clinical trial with single-agent or combination modalities (see the following section) are also options.
Other agents of interest in MF
| Standard therapies in combination with ruxolitinib . |
|---|
| Danazol |
| ESA |
| Hydroxycarbamide |
| IFN-α (both formulations of pegylated IFN-α) |
| IMiD (thalidomide but pomalidomide and lenalidomide in clinical trials) |
| Radiotherapy (for extramedullary hematopoiesis, bone pain and splenomegaly) |
| Splenectomy |
| SCT |
| Agents either used alone or with ruxolitinib |
| Activin receptor antagonists (sotatercept, luspatercept) |
| Antifibrotic agents (PRM-151 pentraxin analog) |
| CDK4/6 (LEE011) |
| Demethylating agents (azacytidine, decitabine) |
| Drugs acting via apoptosis (LCL-161, navitoclax) |
| Drugs to restore nestin expression (mirabegron) |
| Fedratinib |
| Histone deacetylase inhibitors (panobinostat) |
| Immune checkpoint inhibitors (nivolumab) |
| Itacitinib |
| Pacritinib |
| PI3K/Akt/mTOR inhibitors (BKM120, everolimus) |
| PIM kinase (LGH447 |
| SMO inhibitors (LDE225, glasdegib) |
| Telomerase inhibitors (imetelstat) |
| Type 1 JAKi |
| Standard therapies in combination with ruxolitinib . |
|---|
| Danazol |
| ESA |
| Hydroxycarbamide |
| IFN-α (both formulations of pegylated IFN-α) |
| IMiD (thalidomide but pomalidomide and lenalidomide in clinical trials) |
| Radiotherapy (for extramedullary hematopoiesis, bone pain and splenomegaly) |
| Splenectomy |
| SCT |
| Agents either used alone or with ruxolitinib |
| Activin receptor antagonists (sotatercept, luspatercept) |
| Antifibrotic agents (PRM-151 pentraxin analog) |
| CDK4/6 (LEE011) |
| Demethylating agents (azacytidine, decitabine) |
| Drugs acting via apoptosis (LCL-161, navitoclax) |
| Drugs to restore nestin expression (mirabegron) |
| Fedratinib |
| Histone deacetylase inhibitors (panobinostat) |
| Immune checkpoint inhibitors (nivolumab) |
| Itacitinib |
| Pacritinib |
| PI3K/Akt/mTOR inhibitors (BKM120, everolimus) |
| PIM kinase (LGH447 |
| SMO inhibitors (LDE225, glasdegib) |
| Telomerase inhibitors (imetelstat) |
| Type 1 JAKi |
ESA, erythropoiesis-stimulating agent.
Management of high-risk MF
In general, the management options for high-risk MF are as for intermediate-2 risk disease; having assessed and reversed vascular risk factors and made a decision on low-dose aspirin or not, the main decisions concern SCT or clinical indication-based therapy as discussed previously. Case 6 was selected deliberately because this patient demonstrates several difficult-to-treat issues that require a separate focus. The first is whether this patient has MF because this patient displays some unusual features (ie, marked pancytopenia, lack of splenomegaly, and lack of a driver mutation). Therefore, the patient merits special attention regarding a wider differential diagnosis that could include a variety of conditions, as discussed previously. Patients with a confirmed MF diagnosis but severe thrombocytopenia (platelets <50 × 109/L) have a poor prognosis and more severe disease phenotype, as described in a recent paper from the Spanish registry.14
Anemia also merits specific discussion here because it is difficult to manage and few patients have anemia improvement with ruxolitinib. This means, as outlined in Table 2, that one has to consider addition of transfusions, erythroid-stimulating agent, androgenic steroid, steroid, or IMiD; in fact none of these approaches yielded very satisfactory responses in the pre-ruxolitinib era and the situation in combination with ruxolitinib is the same. This means caution in choosing and using ruxolitinib in an anemic patient and that novel agents to target anemia such as momelotinib, luspatercept, or sotatercept as discussed next are of significant interest.
Recommendations for ruxolitinib use
| Dosing and administration . |
|---|
| The recommended initial dosing of ruxolitinib is dependent on the patient's baseline platelet count. |
| Certain clinical situations may support initiation of ruxolitinib at a lower dose with subsequent dose adjustments. |
| Dose modifications for insufficient response |
| Increase dose as tolerated, aim for maximum tolerated dose, and treat the patient for 6 months before formally assessing response. |
| Doses should not be increased during the first 4 weeks of therapy and not more frequently than every 2 weeks; maximum steps, 5 mg twice daily. |
| Consider dose increases if patients do not achieve treatment target; this will be individual for each patient: for example, a <50% in spleen size may be acceptable |
| Hematological toxicities |
| Anemia and thrombocytopenia begins to resolve after the 12th week. |
| Thrombocytopenia is managed by dose reduction or if severe dose interruption (based on clinical parameters). Platelet transfusions may be necessary. Anemia may require blood transfusions and/or dose modifications. Consideration for ESA,* danazol, or IMiDs such as thalidomide or pomalidomide. |
| Severe neutropenia (ANC <0.5 × 109/L) reversible on withholding ruxolitinib. |
| Nonhematologic toxicities |
| Lipid elevations: Increases in lipid parameters occur. Assess lipids approximately 8 to 12 weeks following initiation of ruxolitinib. Monitor and treat. |
| Renal impairment: Dose reduction is recommended for patients with moderate (CrCl, 30-59 mL/min) or severe renal impairment (CrCl, 15-29 mL/min). Hepatic impairment: Dose reduction recommended for patients with any degree of hepatic impairment. See prescribing information. |
| Infections |
| Increased risk of opportunistic infections. Assess for the risk of serious bacterial, mycobacterial, fungal, and viral infection. Pretreatment screen for HBV, HCV, HIV, and, if appropriate, TB. |
| If a patient develops an infection during ruxolitinib therapy, it is important, where possible, to avoid stopping the agent. |
| TB infection has been reported in patients receiving ruxolitinib; those at higher risk should be tested for latent infection. |
| All patients should be tested for HBV before treatment. Patients with chronic HBV infection should be treated and monitored. |
| Patients with suspected herpes zoster infection should be treated according to clinical guidelines; consider long-term prophylaxis. |
| If progressive multifocal leukoencephalopathy is suspected, ruxolitinib should be discontinued and expert advice sought. |
| Nonmelanoma skin cancer |
| Nonmelanoma skin cancers: basal, squamous, and Merkel cell carcinoma have occurred. Perform periodic skin examinations and warn patients about sun exposure. |
| Stopping ruxolitinib |
| Abrupt withdrawal of ruxolitinib should be avoided, tapering of the dose and warning the patient about resurgence of symptoms and splenomegaly is preferable. Steroid cover may be helpful. |
| Dosing and administration . |
|---|
| The recommended initial dosing of ruxolitinib is dependent on the patient's baseline platelet count. |
| Certain clinical situations may support initiation of ruxolitinib at a lower dose with subsequent dose adjustments. |
| Dose modifications for insufficient response |
| Increase dose as tolerated, aim for maximum tolerated dose, and treat the patient for 6 months before formally assessing response. |
| Doses should not be increased during the first 4 weeks of therapy and not more frequently than every 2 weeks; maximum steps, 5 mg twice daily. |
| Consider dose increases if patients do not achieve treatment target; this will be individual for each patient: for example, a <50% in spleen size may be acceptable |
| Hematological toxicities |
| Anemia and thrombocytopenia begins to resolve after the 12th week. |
| Thrombocytopenia is managed by dose reduction or if severe dose interruption (based on clinical parameters). Platelet transfusions may be necessary. Anemia may require blood transfusions and/or dose modifications. Consideration for ESA,* danazol, or IMiDs such as thalidomide or pomalidomide. |
| Severe neutropenia (ANC <0.5 × 109/L) reversible on withholding ruxolitinib. |
| Nonhematologic toxicities |
| Lipid elevations: Increases in lipid parameters occur. Assess lipids approximately 8 to 12 weeks following initiation of ruxolitinib. Monitor and treat. |
| Renal impairment: Dose reduction is recommended for patients with moderate (CrCl, 30-59 mL/min) or severe renal impairment (CrCl, 15-29 mL/min). Hepatic impairment: Dose reduction recommended for patients with any degree of hepatic impairment. See prescribing information. |
| Infections |
| Increased risk of opportunistic infections. Assess for the risk of serious bacterial, mycobacterial, fungal, and viral infection. Pretreatment screen for HBV, HCV, HIV, and, if appropriate, TB. |
| If a patient develops an infection during ruxolitinib therapy, it is important, where possible, to avoid stopping the agent. |
| TB infection has been reported in patients receiving ruxolitinib; those at higher risk should be tested for latent infection. |
| All patients should be tested for HBV before treatment. Patients with chronic HBV infection should be treated and monitored. |
| Patients with suspected herpes zoster infection should be treated according to clinical guidelines; consider long-term prophylaxis. |
| If progressive multifocal leukoencephalopathy is suspected, ruxolitinib should be discontinued and expert advice sought. |
| Nonmelanoma skin cancer |
| Nonmelanoma skin cancers: basal, squamous, and Merkel cell carcinoma have occurred. Perform periodic skin examinations and warn patients about sun exposure. |
| Stopping ruxolitinib |
| Abrupt withdrawal of ruxolitinib should be avoided, tapering of the dose and warning the patient about resurgence of symptoms and splenomegaly is preferable. Steroid cover may be helpful. |
ANC, absolute neutrophil count; CrCl, creatinine clearance; EPO, erythropoietin; HBV, hepatitis B virus; HCV, hepatitis C virus; TB, tuberculosis.
EPO levels will be high on ruxolitinib.
Practical aspects of using ruxolitinib
Ruxolitinib was evaluated in the Controlled Myelofibrosis Study With Oral JAK Inhibitor Treatment-I and -II studies and was approved based upon spleen volume reduction and improvement in symptoms and quality of life. Dose-limiting myelosuppression, particularly in the first 3 months of therapy, was common. Increased risk of infection has also been documented, ranging from common bacterial/viral ailments to rare severe infections such as John Cunningham virus–related progressive multifocal leukoencephalopathy (reviewed in O’Sullivan et al15 ). Recently published 5-year updates from these trials demonstrate that benefits were generally maintained and provided compelling evidence of possible overall survival benefit with ruxolitinib. This was confirmed in comparison with historical cohorts and for molecularly defined higher risk disease but remains controversial (discussed in Cervantes and Pereira13 ).
Speculation continues as to the reason for survival advantage with ruxolitinib: improvements in clinical status (eg, reversal of cachexia, control of systemic inflammation) are potential reasons.16,17 Individual cases have reported that significant changes in bone marrow fibrosis and mutant allele burden are seen, but complete histopathological and/or molecular remission has only rarely been observed.18,19 Finally, recent data suggests the likelihood of achieving spleen response and time to treatment failure diminishes incrementally with the presence of multiple adverse prognostic mutations.20
There are many considerations in the use of ruxolitinib and several national and international guidelines exist. Some practical recommendations are shown in Table 2. Factors of importance are to screen for infections before treating, maximize response of the spleen and managing hematological toxicities. It is important to warn patients not to run out of tablets or to stop taking them suddenly and well as educating them regarding controlling their weight. Drug:drug as well as drug;diet interactions are also important aspects for patient education.
Ruxolitinib and SCT
Although the focus of this paper is not SCT, the role of ruxolitinib or other novel therapies used before SCT and indeed considerations regarding timing of SCT in a patient established on ruxolitinib remain of key importance. Current practice suggests that many patients being brought forward for SCT have had therapeutic exposure to least 1, or indeed more, JAKi agents. Benefits of ruxolitinib therapy before SCT in a responder predominantly consist of improvements in symptom burden and performance status, hence potentially facilitating more intensive therapeutic approaches, and reductions in splenomegaly, which may result not only in augmented hematological recovery but also improved graft function. Moreover, it is tempting to hypothesize that ruxolitinib-mediated modulation of T-, natural killer, and dendritic cell function may alter the incidence and perhaps grade of graft-versus-host disease rates, although this requires verification in prospective clinical trials. Potential drawbacks to ruxolitinib therapy before SCT include a higher risk of infectious complications, the rare risk of tumor lysis syndrome or unexpected toxicity, and drug-related cytopenia, which may increase transfusion-dependence of patients.
One difficult clinical scenario remains when best to proceed with SCT for a transplant-eligible ruxolitinib-responding patient who has a good donor source identified. Should we proceed at the time of best response to ruxolitinib or, given the inherent risk of transplant-related morbidity and indeed mortality, wait until we see further adverse warning signs such as loss of response, increasing circulating blasts or acquisition of high-risk cytogenetic anomalies? A retrospective analysis from a multi-institutional cohort of 100 patients who received JAKi therapy before SCT suggested that improved outcomes were observed in those patients who demonstrated clinical improvement following exposure to JAKi and then were transplanted compared with those who demonstrated loss of response or progressive disease.21 Longer follow-up is required to determine later outcomes. In our institution, we use a relatively rapid tapering of therapy and start to downtitrate the JAKi therapy at approximately 10 days before beginning chemotherapy and aim to stop the day before conditioning begins. With this approach, we have not observed any safety issues or rebound phenomena. To date, it remains unclear what effect other agents being explored in the clinical trial setting for MF such as antifibrotic or telomerase inhibitors may have on post-SCT outcome.
Other JAKis
Unfortunately, several JAKi have been halted in development, eg, fedratinib due to development of Wernicke’s Encephalopathy despite having positive results from a phase 3 clinical trial.22 Recently results of the JAKARTA2 trial of fedratinib in second line therapy were published and call for re-instigation of assessment of feasibility of this drug in clinical practice.23 Pacritinib, momelotinib and itacitinib are discussed here.
Pacritinib was evaluated in phase 3 trials Pacritinib in Combination With Low Dose Decitabine in Intermediate-High Risk Myelofibrosis or Myeloproliferative Neoplasm (MPN)/Myelodysplastic Syndrome (MDS) (PERSIST)-1 and PERSIST-2. Results are available from both. In both studies, myelosuppression was not as marked as anticipated and anemia/transfusion responses were reported independent.24,25 Pacritinib is potentially attractive for cytopenic MF patients; indeed, the PERSIST-2 study enrolled only patients with platelets less than 100 × 109/L. In February 2016, pacritinib was put on a clinical hold because of concern over survival, increased bleeding, and cardiac events; this was lifted in 2017 and further evaluation of dosing and benefit of pacritinib is under way.
Momelotinib a JAK1/2 inhibitor produced anemia responses in addition to improvements in spleen and symptoms. Peripheral neuropathy was reported and may be important in deciding where momelotinib sits in the therapeutic algorithm. Results of phase 3 studies (SIMPLIFY-1) comparing momelotinib with ruxolitinib, and SIMPLIFY-2 assessing momelotinib in patients who have failed ruxolitinib (but importantly, the majority of the control arm received ruxolitinib), were reported at the American Society of Clinical Oncology meeting with mixed results because of consistent anemia/transfusion-related responses.26,27 The future of momelotinib is unclear, but the clinical importance of anemia response should be emphasized.
Itacitinib (INCB039110), a selective JAK1 inhibitor, in an open-label phase 2 study for intermediate-/high-risk MF and platelet counts >50 × 109/L delivered 35% symptom response, 15% spleen response, and 53% had a ≥50% reduction in transfused red cell units.28 This drug is in ongoing studies, both alone and in combination with ruxolitinib.
JAKi in combination
There is significant interest in combining JAKi with traditional and experimental agents. The rationale for such combination therapy would be to maximize the dose of ruxolitinib by, for example, maintaining the platelet count with danazol, hemoglobin with pomalidomide, or to improve outcomes (eg, for better spleen response). Multiple studies with IMiDs, androgens, HDAC inhibitors, phosphatidylinositol 3-kinase (PI3K) inhibitors, smoothened inhibitors, and before SCT have been initiated (recently reviewed in Vannucchi and Harrison29 ) Criteria used for judging success in this situation are complex and not validated, so there is a risk of missing real signals and a robust strategy for how combination trials are pursued in this disease setting is needed.
Non–JAKi-based therapy
Standard care
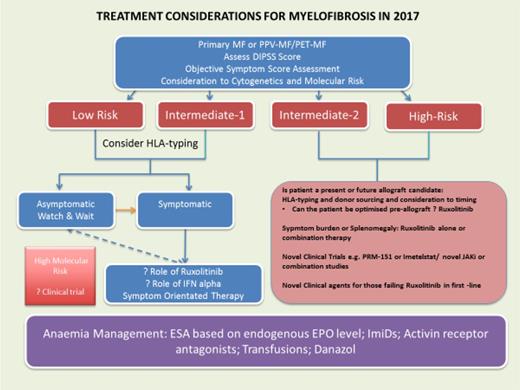
Multiple non–JAKi-based treatment strategies are actively being used in the management of MF both in routine and experimental settings. In standard care, agents are commonly used to manage symptoms either in addition to or instead of ruxolitinib and these include drugs such as prednisolone, bisphosphonates, and radiotherapy. In addition, drugs commonly used to manage anemia, thrombocytopenia, or leukocytosis include androgens, erythroid-stimulating agents, thalidomide, or, rarely, other IMiDs, hydroxycarbamide/hydroxyurea, and, as discussed previously, IFN-α. SCT also needs to be accommodated in these algorithms, which we have discussed in the context of JAKi and show its use in the cases and Figure 3. We refer the reader to excellent recent reviews for other agents.29
Dynamic assessment of considerations for intervention in those with either PMF or sMF in 2017. EPO, erythropoietin; ESA, erythroid-stimulating agent; HLA, human leukocyte antigen; PET, postessential thrombocythemia; PPV postpolycythemia vera.
Dynamic assessment of considerations for intervention in those with either PMF or sMF in 2017. EPO, erythropoietin; ESA, erythroid-stimulating agent; HLA, human leukocyte antigen; PET, postessential thrombocythemia; PPV postpolycythemia vera.
Experimental therapies
As listed in Table 1, multiple different targets either have been recently evaluated or are undergoing evaluation in MF. We have chosen to expand on a selection as discussed here.
BEZ235 a PI3K/mTOR inhibitor, showed activity in JAK2V617F-mutated Hel cells30 and induced apoptosis in PMF progenitor cells synergized with fedratinib and TG101209.31 No trial has been initiated in MF to date. Buparlisib (BKM120), a PI3K inhibitor, was tested in combination with ruxolitinib but there was no incremental response. Everolimus was evaluated in a phase 1/2 study and yielded an overall response rate of 23%.32
Panobinostat used alone in MF demonstrated clinical effects at low doses given over a long period with minimal side effects.33 Two phase 1/2 trials are assessing the safety and tolerability of the combination of panobinostat and ruxolitinib.
Azacitidine showed limited clinical activity in a phase 2 study, with 23% of MF patients having a response, and myelosuppression remained the major toxicity.34 There may be more efficacy, however, when there is evidence of an acute leukemic transformation. The current UK-based phase 1b Study to Assess the Safety and Tolerability of Oral Ruxolitinib in Combination With 5-Azacitidine in Patients With Advanced Phase Myeloproliferative Neoplasms (MPN), Including Myelodysplastic Syndromes (MDS) or Acute Myeloid Leukaemia (AML) Arising From MPN is investigating the efficacy of combination azacytidine and ruxolitinib in accelerating/blast phase patients.35
Imetelstat, a telomerase inhibitor, was evaluated in 33 patients with intermediate-2 or high-risk MF, CR, or partial response was observed in 21%, with median duration of 10 to 18 months.36 Reversal of bone marrow fibrosis occurred in 3 of 4 patients in CR and reductions of JAK2V617F allele burden were seen. Interestingly, 28% of JAK2V617F-mutated patients responded but no wild-type JAK2 patients did; ASXL1 mutations were associated with lack of response and SF3B1 or U2AF1 mutations predicted response. A randomized phase 2 study (IMBARK) in MF patients relapsed or refractory to ruxolitinib is ongoing.
PRM-151, a recombinant form of human pentraxin-2, a regulator of tissue repair, prevented and/or reversed fibrosis in preclinical models. Interestingly, clonal fibrocytes producing collagen and fibronectin were abundantly present in the bone marrow of MF patients; mice xenografted with MF patients’ cells developed a lethal myelofibrosis-like disease that was slowed by PRM-151.37 A phase 2 study of PRM-151 in combination with ruxolitinib showed that the combination was well tolerated; spleen volume, symptomatic improvement, and improvement in fibrosis grade were documented, but infrequently.38 PROMOTE, a phase 2 trial in patients intolerant/refractory/ineligible for ruxolitinib, is ongoing and cumulative results awaited.
Fresolimumab, a monoclonal antibody neutralizing all isoforms of TGF-β, induced reduction in transforming growth factor-β (TGF-β) levels in 2 evaluable patients, improvements of anemia, but no significant changes in fibrosis were documented.39 Lysyl oxidase and lysyl oxidase like are amine oxidases involved in crosslinking and stabilization of collagen and elastin fibers. Simtuzumab, a humanized antibody against lysyl oxidase like 2, was used in 54 patients with MF; treatment was well tolerated but no clear signal of response was observed.40
Activin receptor antagonists
Luspatercept has a novel structure consisting of a soluble fusion protein with a modified extracellular domain of the activin receptor type IIB inhibits SMAD2/3 signaling and demonstrated improvement of anemia both in refractory anemia with ring sideroblasts and β-thalassemia; a phase 2 trial to investigate efficacy in addressing MF-related anemia is planned. Preliminary results from the phase 2 study of sotatercept (NCT01712308), which also sequesters ligands of the TGF-β superfamily and relieves blockade of terminal erythroid differentiation in MF, were presented at the 2016 Annual Meeting of the American Society of Hematology. Early results were promising, with improvements in both anemia and red blood cell transfusion dependence and therapy appearing to be well tolerated.41
Apoptosis as a target
A number of agents targeting components of the apoptotic pathway, either directly or indirectly, are being explored in MF. One of key interest is LCL-161, an oral second mitochondria-derived activator of caspase mimetic, which is being investigated in a single-center phase 2 trial for MF; importantly, prior SCT or thrombocytopenia are not exclusion criteria. Of the small cohort of patients reported (n = 21) as of July 2016, many of whom had failed or were intolerant of JAKi, 8 of 13 demonstrated reductions in the antiapoptotic protein cIAP1.42 Clinical efficacy signals were identified in some individuals and LCL-161 is being investigated in stage 2 of the trial.
Immune-based therapy via the novel protein terminal originated by CALR frameshift mutations might be a suitable target for either antibody- or cell-mediated immune therapy. Regarding immune checkpoint inhibitors, a study is currently under way.
Conclusions
MF remains a challenging condition, yet one in which great advances have recently radically altered our therapeutic algorithms and, most important, significantly improved disease-related symptoms, quality of life, and survival for many patients. Clinicians have focused attention on the conventional aspects of disease management, such as vascular risk, and aspirin and agents such as hydroxyurea and IFN-α, etc, but also on the symptoms and impact on quality of life. Ruxolitinib brings new challenges, such as how to improve upon it, but also the significant challenge of what to offer patients progressing or not responding. There is a gap between our ability to profile patients at a molecular level and applying such knowledge in clinical practice. Another major gap is the lack of a surrogate marker for disease response; positron emission tomography scanning has been evaluated and could be of interest.43 We should focus our efforts on finding a better therapy and being able prove that superiority. In the words of Marcel Proust, “The real voyage of discovery consists not in seeking new landscapes but in having new eyes.”
Correspondence
Claire Harrison, Department of Haematology, Guy’s and St Thomas’ National Health Services Foundation Trust, Guys Hospital, Great Maze Pond, London SE1 9RT, United Kingdom; e-mail: claire.harrison@gstt.nhs.uk.
References
Competing Interests
Conflict-of-interest disclosure: C.N.H. has received research funding from Novartis; consulted for Novartis; received honoraria from Baxalta, Gilead, Celgene, Novartis, and CTI; and been affiliated with the Speakers Bureau for Gilead, Shire, Novartis, and CTI. D.P.M. has received honoraria from and been affiliated with the Speakers Bureau for Novartis and JAZZ Pharmaceuticals.
Author notes
Off-label drug use: None disclosed.