Abstract
Development of exercise guidelines for individuals with sickle cell trait (SCT) and sickle cell anemia (SCA) is hampered by the need to weigh the benefits against risks of exercise in these populations. In SCT, concern for exercise collapse associated with sickle cell trait has resulted in controversial screening of student athletes for SCT. In SCA, there exists unsubstantiated concerns that high-intensity exercise may result in pain and other complications. In both, finding the “right dose” of exercise remains a challenge for patients and their providers. Despite assumptions that factors predisposing to adverse events from high-intensity exercise overlap in SCT and SCA, the issues that frame our understanding of exercise-related harms in both are distinct. This review will compare issues that affect the risk-benefit balance of exercise in SCT and SCA through these key questions: (1) What is the evidence that high-intensity exercise is associated with harm? (2) What are the pathophysiologic mechanisms that could predispose to harm? (3) What are the preventive strategies that may reduce risk? and (4) Why do we need to consider the benefits of exercise in this debate? Addressing these knowledge gaps is essential for developing an evidence-based exercise prescription for these patient populations.
Learning Objectives
Review the epidemiological and scientific data that underlie current concerns related to high-intensity exercise in SCT and SCA
Review the potential benefits of regular exercise and steps necessary to develop evidence-based guidelines for exercise in SCT and SCA
Introduction
The benefits of regular exercise are well described and span the life cycle from childhood throughout adulthood, ranging from physiological to psychological to social. Growing evidence suggests that exercise in all forms triggers epigenetic changes in several pathways that underlie the physiological benefits of exercise.1-3 As a prevention strategy, exercise prescription in the general healthy population aims to reduce future cardiovascular risk. There is now growing acceptance that exercise prescription among individuals with chronic illness is equally important both for preventing comorbid conditions and, in some cases, conferring disease-modifying effects. Thus, the adoption of the mantra that “exercise is medicine” is essential for both healthy individuals as well as those with chronic medical conditions.
Despite the importance of regular exercise in the general population and individuals with other chronic conditions, exercise prescription guidelines do not currently exist for individuals affected by sickle cell trait (SCT) and sickle cell anemia (SCA) due to concerns about the adverse effects of high-intensity exercise in these populations. SCT and SCA are both characterized by the presence of sickle hemoglobin in erythrocytes, the amount of which is determined by the inheritance of 1 (heterozygous) vs 2 (homozygous) copies, respectively, of the same mutation caused by a single-nucleotide substitution (GAG → GTG) at position 6 in the β-globin gene. Although SCA may also refer to less common sickling syndromes that result from the inheritance of SCT and another hemoglobin variant (eg, hemoglobin C or β-thalassemia trait), SCA in this review will refer to homozygous disease. In SCT, erythrocyte sickling is minimal at baseline, and potential adverse health effects (eg, increased risk of kidney disease, venous thromboembolism, adverse pregnancy outcomes) are generally limited to adulthood; in SCA, an increased risk of erythrocyte sickling and downstream pathophysiological consequences result in the development of disease-related complications (eg, chronic anemia, vaso-occlusive pain episodes, infection, acute organ injury, chronic end-organ damage) throughout the life span. More recently, increasing evidence for exertional rhabdomyolysis and associated sudden death, now termed exercise collapse associated with sickle cell trait (ECAST), has raised concerns for high-intensity exercise in SCT.4,5 In SCA, there exists unsubstantiated or anecdotal concerns for an association between moderate- to high-intensity exercise and vaso-occlusive complications such as pain. Thus, finding the right “dose” of exercise in either condition remains an enigmatic challenge for patients and their providers.
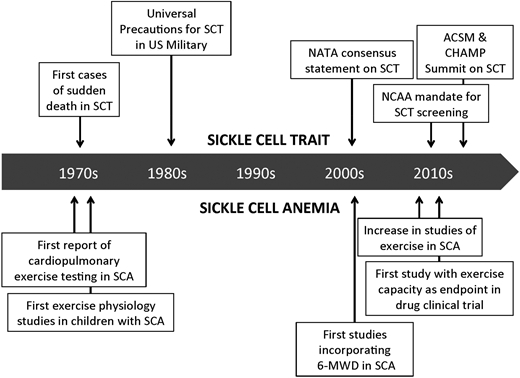
The goal of this review is to discuss the evidence underlying concerns for adverse events related to high-intensity exercise in SCT and SCA and the potential pathophysiologic basis for these concerns. To underscore the need to consider both sides of the risk-benefit balance, the potential negative implications of limiting exercise in these populations, given growing evidence for the unique benefits that regular exercise and improved fitness may confer in SCT and SCA, will also be discussed. This review will be framed in the form of key questions, comparing the history of existing evidence over the years and the gaps that remain in both conditions (Figure 1).
Timeline of important milestones related to application of exercise science and medicine in SCT and SCA. 6-MWD, 6-minute walk distance; ACSM, American College of Sports Medicine; CHAMP, Consortium for Health and Military Performance; NATA, National Athletic Trainers’ Association; NCAA, National Collegiate Athletic Association.
Timeline of important milestones related to application of exercise science and medicine in SCT and SCA. 6-MWD, 6-minute walk distance; ACSM, American College of Sports Medicine; CHAMP, Consortium for Health and Military Performance; NATA, National Athletic Trainers’ Association; NCAA, National Collegiate Athletic Association.
What are the epidemiological data that SCT and SCA impact cardiopulmonary fitness and what is the evidence that high-intensity exercise is associated with harm?
Given the prevalence of SCT is estimated at ∼8% of the general population in the United States, with the highest predominance among persons of African ancestry, the implications for the current discussion about the impact of SCT on exercise safety and fitness are tremendous. The current debate about exertion-related adverse events in SCT goes back several decades and stems from early case reports and epidemiological data describing high rates of exertional collapse and sudden death during high-intensity physical training in athletes and military fighters with SCT.6-8 In an early study of basic training in the US Armed Forces, rates of unexplained deaths per 100 000 were 32.2 and 0.7 for black recruits with and without SCT, respectively. The relative risk of sudden unexplained death among black recruits with SCT in this study was 27.6 (95% confidence interval, 9-100; P < .001).6 Additional efforts aimed at trying to understand the prevalence and risk factors associated with this phenomenon were initially limited. More recent spikes in interest have been spurred on by high-profile cases in the lay press involving athletes as well as the National Collegiate Athletic Association (NCAA) policy (instituted in 2010 for Division I and 2013 for all Divisions) mandating SCT testing in all student athletes (https://www.ncaa.org/sites/default/files/SCT%20testing%20brief%202014.pdf). This policy has led to controversy and ethical debates about the nonintended consequences of widespread SCT screening for this purpose among various organizations and professional societies that represent stakeholders, including athletic associations, military personnel, and physician societies like the American Academy of Pediatrics and the American Society of Hematology.9-13 However, an important benefit of these debates has been the organization of concerted efforts to better study and define exertion-related sudden death in SCT, develop consensus guidelines for mitigating this risk, and frame a future research agenda. For example, it is recognized now that exertional rhabdomyolysis underlies the phenomenon of potential sudden death during high-intensity exercise under extreme conditions in SCT. In support of this, a 2016 retrospective study of nearly 48 000 active military, black soldiers demonstrated that soldiers with SCT had a significantly higher risk of exertional rhabdomyolysis (hazard ratio, 1.54; 95% confidence interval, 1.12-2.12), but not death, when compared with those without SCT.14 Among student athletes, Harmon et al found that the relative risk of exertional death (though not known if always due to rhabdomyolysis) in those students with vs without SCT ranged from 15 to 37, with the highest reported among Division I football players, in a retrospective study of NCAA athletes from 2004 to 2008.15 Although the data are sparse, SCT status in and of itself does not appear to impact fitness levels. Among young black adults followed longitudinally in the Coronary Artery Risk Development in Young Adults study, SCT was not associated with baseline or longitudinal changes in fitness as measured by exercise duration by treadmill testing (535 vs 540 seconds; P = .62).16 Similarly, small prospective studies using maximal cardiopulmonary exercise testing demonstrate no differences in direct measurements of maximal oxygen consumption (VO2 max), considered the standard reference for fitness, or ventilatory responses to exercise testing, in individuals with or without SCT.17,18 For example, Marlin et al found no significant difference in VO2 max between subjects with (42.7 ± 2.5 mL/kg per minute) or without (42.5 ± 3.4 mL/kg per minute) SCT in their study.18
In contrast to what is known in SCT, less is known about the actual adverse events associated with high-intensity physical exertion and exercise in SCA. Formal studies to evaluate adverse events in these settings may be lacking due to assumptions that individuals with SCA do not participate in high-intensity physical activity and exercise because of self- or provider-imposed restrictions or that physical and physiological limitations stemming from disease-related complications preclude participation. In the absence of direct data, much of the former stems from unsubstantiated concerns that high-intensity physical exertion may increase sickling and predispose to complications such as vaso-occlusive pain. Although data from sustained high-intensity exercise are not available, safety data from several studies in both adults and children with SCA that use maximal cardiopulmonary exercise testing to measure fitness suggest that exercising with increasing intensity until exhaustion appears to be safe and does not result in adverse events. What we do know is that in contrast to what has been observed in SCT, SCA is associated with markedly decreased cardiopulmonary fitness in both children and adults using this gold-standard test.19-21 In their study of 60 children with SCA and 30 matched controls, Liem et al found that peak VO2 was ∼30% lower in children with SCA when compared with controls (26.9 ± 6.9 mL/kg per minute vs 37.0 ± 9.2 mL/kg per minute; P < .001).19 In another study, 83% of adults with sickle cell disease (all genotypes) had evidence for decreased maximal exercise capacity.20 Besides maximal cardiopulmonary exercise testing, other approaches have been used to evaluate fitness in SCA patients, including submaximal exercise testing or 6-minute walk distance, which have commonly been used in adults with SCA to measure impact of disease and its complications, such as cardiopulmonary disease, on physical functioning.22-24 Despite challenges in comparing data in these studies due to variability in testing modality, the data in aggregate demonstrate a major impact of disease on fitness and physical functioning. Even less data are available to help us understand actual physical activity levels in this population; however, at least 1 study using a Physical Activity Questionnaire adapted from the National Health and Nutrition Examination Survey (NHANES) has suggested that compared with matched peers, fewer children with SCA reported spending at least 60 minutes per day in either moderate to vigorous (17% vs 23%; P < .01) or vigorous intensity (24% vs 43%; P = .01) physical activity.25
What are the pathophysiologic processes that could predispose to adverse events and what factors impact fitness in SCT and SCA?
The potential pathophysiologic mechanisms that trigger concern for adverse events with high-intensity exercise in SCT and SCA are not well characterized and, importantly, despite some overlap, are not necessarily interchangeable between the 2 populations. RBC sickling is minimal among individuals with SCT at baseline or under normal conditions. Early studies, however, have demonstrated that sickling in individuals with SCT may increase under conditions associated with extraordinary exercise intensity, including severe dehydration, metabolic acidosis, and hypoxemia.26,27 How these factors converge to create the “perfect storm” and interact with other considerations such as extreme heat or genetic predisposition to result in ECAST in some individuals and not others is not clear. Moreover, another challenge to our understanding of the risk conferred by these interactions is that from a pathophysiologic standpoint, ECAST most reflects signs and symptoms of exertional rhabdomyolysis (eg, muscle weakness or pain, dark urine, renal injury, hyperkalemia, arrhythmias), yet there is overlap with symptoms of exertional heat injury or heat stroke (Table 1). Studies that have tried to evaluate the pathophysiologic factors during exercise challenge that could predispose to ECAST have been limited, small in scope, and confounded by variability in exercise testing conditions and protocol (ie, intensity, duration). The potential pathophysiologic contributors that have been considered can be divided into factors related to whole-blood viscosity, the proinflammatory response to exercise, oxidative stress, and hemorheological properties (Table 2). Blood viscosity appears to be higher at baseline and increases during exercise in individuals with SCT, although increases in viscosity are similar to that measured in controls and the effect can be blunted or normalized with hydration.28,29 In SCT carriers participating in a soccer game, for example, blood viscosity decreased significantly under hydrated conditions but increased 16.3% under dehydrated conditions.28 Similarly, RBC rigidity has been shown to be greater at baseline in SCT and may increase after high-intensity, supramaximal exercise.30-32 In a small study of 8 adults with SCT and 8 controls, Connes et al showed that 2 measures of RBC rigidity (Tk and k) did not significantly change during a short supramaximal exercise challenge despite being higher in adults with SCT at every point of exercise.30 However, these studies in general have been largely inconclusive regarding their direct causative relationship to ECAST. Other studies generally demonstrate no major or consistent between-group differences in the proinflammatory responses to exercise, coagulation profiles, as well as lactate metabolism or responses during exercise at moderate to high intensities in individuals with and without SCT.18,33-35 Importantly, Sara et al found no significant difference in the occurrence of the first and second lactate thresholds during incremental exercise testing in SCT carriers (38% ± 4.7% and 72.9% ± 3.4% of VO2 max) vs controls without SCT (37.3% ± 3% and 76.8% ± 5.4% of VO2 max).34
Signs and symptoms of exertional rhabdomyolysis, heat injury, and heat stroke
| Sign or symptom . | Exertional rhabdomyolysis . | Exertional heat injury . | Exertional heat stroke . |
|---|---|---|---|
| Fatigue/weakness | • | • | • |
| Dizziness/lightheadedness | • | • | |
| Vision changes | • | • | |
| Headache | • | • | |
| Nausea/vomiting | • | • | |
| Confusion/altered mental status | • | ||
| Muscle weakness | • | ||
| High core body temperature | • | • | |
| Tachycardia | • | ||
| Hypotension | • | ||
| Dark urine or decreased urine output | • | • | • |
| Seizures | • | ||
| Hyperkalemia | • | ||
| Disseminated intravascular coagulation | • | ||
| Collapse or cardiac arrest | • |
| Sign or symptom . | Exertional rhabdomyolysis . | Exertional heat injury . | Exertional heat stroke . |
|---|---|---|---|
| Fatigue/weakness | • | • | • |
| Dizziness/lightheadedness | • | • | |
| Vision changes | • | • | |
| Headache | • | • | |
| Nausea/vomiting | • | • | |
| Confusion/altered mental status | • | ||
| Muscle weakness | • | ||
| High core body temperature | • | • | |
| Tachycardia | • | ||
| Hypotension | • | ||
| Dark urine or decreased urine output | • | • | • |
| Seizures | • | ||
| Hyperkalemia | • | ||
| Disseminated intravascular coagulation | • | ||
| Collapse or cardiac arrest | • |
Potential pathophysiologic mechanisms underlying adverse events during high-intensity exercise in SCT and SCA
| Potential factors during exercise . | SCT . | SCA . |
|---|---|---|
| Plasma or whole blood viscosity and dense sickle RBCs | • Higher at baseline compared with controls | • No difference in viscosity at baseline or after exercise compared with controls |
| • Increases with exercise but no difference in increase compared with controls | • Increase in dense cells after exercise | |
| • Remained elevated at end of recovery compared with controls | ||
| • No effect of α-thalassemia trait on results | ||
| RBC rigidity and deformability | • Higher at baseline and during exercise compared with controls | • No data in the literature |
| • Unchanged with exercise | ||
| Oxidative stress markers | • No difference in baseline levels compared with controls | • No difference in response after acute exercise compared with controls |
| • Increased after exercise with postexercise levels higher compared with controls | • May remain elevated after prolonged exercise compared with controls | |
| Inflammatory response markers | • No difference in baseline levels of most cytokines and adhesion molecules | • No difference in response of IL-6 and other inflammatory markers after exercise compared with controls |
| • Variability in sVCAM and sP-selectin response to exercise | • No difference in sVCAM response to exercise compared with controls | |
| • No change in sE- or sP-selectin response to exercise | ||
| Coagulation markers | • No difference in baseline levels of coagulation profile, fibrinogen, and antithrombin activity compared with controls | • No data in the literature |
| • Unchanged with exercise | ||
| Lactate metabolism | • No difference in lactate thresholds or clearance compared with controls | • Increases with exercise with lower lactate thresholds during exercise compared with controls |
| • Variability in lactate levels throughout exercise and recovery compared with controls | ||
| • Faster RBC uptake of lactate in SCT |
| Potential factors during exercise . | SCT . | SCA . |
|---|---|---|
| Plasma or whole blood viscosity and dense sickle RBCs | • Higher at baseline compared with controls | • No difference in viscosity at baseline or after exercise compared with controls |
| • Increases with exercise but no difference in increase compared with controls | • Increase in dense cells after exercise | |
| • Remained elevated at end of recovery compared with controls | ||
| • No effect of α-thalassemia trait on results | ||
| RBC rigidity and deformability | • Higher at baseline and during exercise compared with controls | • No data in the literature |
| • Unchanged with exercise | ||
| Oxidative stress markers | • No difference in baseline levels compared with controls | • No difference in response after acute exercise compared with controls |
| • Increased after exercise with postexercise levels higher compared with controls | • May remain elevated after prolonged exercise compared with controls | |
| Inflammatory response markers | • No difference in baseline levels of most cytokines and adhesion molecules | • No difference in response of IL-6 and other inflammatory markers after exercise compared with controls |
| • Variability in sVCAM and sP-selectin response to exercise | • No difference in sVCAM response to exercise compared with controls | |
| • No change in sE- or sP-selectin response to exercise | ||
| Coagulation markers | • No difference in baseline levels of coagulation profile, fibrinogen, and antithrombin activity compared with controls | • No data in the literature |
| • Unchanged with exercise | ||
| Lactate metabolism | • No difference in lactate thresholds or clearance compared with controls | • Increases with exercise with lower lactate thresholds during exercise compared with controls |
| • Variability in lactate levels throughout exercise and recovery compared with controls | ||
| • Faster RBC uptake of lactate in SCT |
IL-6, interleukin 6; RBC, red blood cell; SCT, stem cell transplantation; sE-selectin, soluble E-selectin; sP-selectin, soluble P-selectin.
Such factors of concern in SCT have been less well studied in SCA in part due to hesitation in using submaximal or maximal exercise testing to simulate the conditions under which these factors may be examined in individuals with SCA. Limited data from a small study suggest that although the percentage of dense red blood cells was increased to a greater degree in adults with SCA (29% vs 12%; P < .001) at rest when compared with that seen in controls, no consistent between-group differences in plasma or blood viscosity were observed. Moreover, exercise significantly increased plasma viscosity (1.2 ± 0.07 mPa per second to 1.28 ± 0.1 mPa per second; P < .01) but not whole-blood viscosity or percentage of dense cells in adults with SCA.36 Recently, there has been greater focus on the potential concern for an exaggerated inflammatory response to exercise in SCA that might predispose to adverse events such as vaso-occlusive pain. SCA is characterized by a proinflammatory state, as evidenced by baseline elevation in inflammatory markers that worsen during complications like pain and acute chest syndrome. Acute exercise itself is also associated with a well-described proinflammatory response in the general population marked by the immediate and delayed elevation of various inflammatory biomarkers. Limited data suggest that the inflammatory response to acute exercise is observed in both adults and children with SCA. In the only study that compared data to that observed in matched controls without SCA, the magnitude of the acute inflammatory response to maximal exercise testing, defined by change in soluble vascular cell adhesion molecule (sVCAM) and other biomarkers, was not any greater in children with SCA.37 In this study, the increase in sVCAM immediately after exercise was not significantly different in subjects with SCA vs controls (87 vs 48 ng/mL; P = .15). However, a small study of women with SCA exposed to 3 consecutive days of exercise suggests that oxidative stress associated with exercise may remain elevated compared with that observed in controls.38 Acute exercise is associated in general with other physiologic consequences that could constitute “danger” signals for precipitating sickling in individuals with SCA but studies in humans or mouse models are limited. Small studies in a mouse model of SCA suggest acute exercise can increase the risk of intramuscular metabolic acidosis and other metabolic derangements.39,40 For example, Chatel et al demonstrated that reduction in intramuscular pH was greater for SS mice undergoing electrostimulation simulating exercise when compared with AA mice (−0.28 ± 0.06 vs −0.15 ± 0.05; P < .01).40 Although these factors represent the same pathophysiologic mechanisms that drive known complications of SCA such as vaso-occlusion, whether or not they directly contribute to potential adverse effects of exercise in SCA is not clear. Moreover, it is important to note that although these pathophysiologic consequences of acute exercise might indirectly limit exercise or physical exertion in SCA, the actual reasons for reduced fitness in SCA are multifactorial and complex, and studies that have tried to dissect out the causes are limited. Risk factors may include chronic anemia, sedentary lifestyle, physical limitations from stroke or avascular necrosis as well as cardiopulmonary complications such as chronic lung disease, pulmonary vascular disease, or diastolic dysfunction. The assessment of breath-by-breath, gas-exchange data obtained during cardiopulmonary exercise testing has been useful for understanding the pathophysiology associated with reduced fitness. Such studies in children and adults with SCA demonstrate derangements in the actual cardiopulmonary response to exercise, including impaired oxygen uptake, reduced ventilatory efficiency, and lower oxygen pulse during exercise.19,20,41,42 These studies also suggest that exercise limitation cannot adequately be explained by the presence of chronic anemia alone in this patient population. When compared with that measured in matched controls without SCA, fitness levels in children with SCA remained significantly lower even when adjusted for hemoglobin, age, sex, and body mass index (β = 5.93; P = .005).19
What is the potential impact of limiting exercise in SCT and SCA and why do we need to consider the benefits of exercise in this debate?
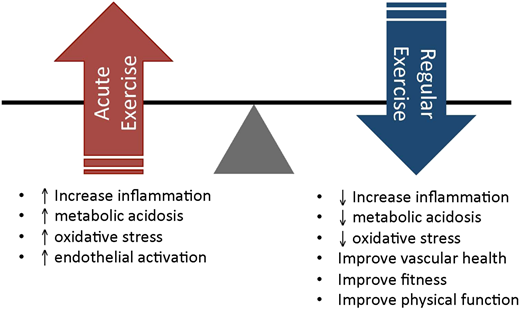
Limiting regular exercise in SCT and SCA without a clear understanding of the balance of its harms vs benefits may have unintended consequences and a long-term impact on fitness in populations who may already be at risk for a sedentary lifestyle and its adverse outcomes.43 Although the potential risks of high-intensity exercise cannot be ignored in SCT and SCA, it may be time to change the current paradigm and shift our attention instead to the benefits of exercise and physical activity in these populations. Landmark epidemiological studies demonstrate that cardiopulmonary fitness remains one of, if not the, most important predictors of all-cause mortality among individuals who are both healthy or have a chronic medical condition.44,45 Long-term gains in fitness, physical activity, and physical functioning are associated with improved cardiovascular outcomes, overall mortality, health-related quality of life and other patient-centered outcomes in adults. For individuals with SCT, in whom the development of cardiovascular risk factors is similar to that observed in the general African American population, reducing cardiovascular disease risk by increasing physical activity and exercise remains important.16 This may hold true even more for individuals affected by chronic conditions such as SCA for whom finding safe approaches to increasing physical activity and promoting regular exercise may not represent a priority. For children affected by SCA, the negative impact of a sedentary lifestyle may be significant given the known benefits of regular exercise and physical activity and their contributions to normal growth and development, including cognitive development, which represent areas negatively affected by disease. Moreover, parent, physician, or school reluctance to allow participation in school- or community-based sports or exercise programs could lead to social isolation and decreased self-esteem among children with SCA. Uncertainty regarding the benefits vs risks of regular exercise in specific disease states is not unique to SCA and has been previously observed in other chronic conditions such as congestive heart failure, chronic obstructive lung disease, asthma, rheumatoid arthritis, and cystic fibrosis.46-52 Despite initial concerns about the inability to tolerate exercise or the harmful effects of acute exercise in affected individuals, ample data demonstrating net benefits now support the prescription of regular exercise in these conditions. SCA in particular may represent an ideal model for studying the benefits of regular exercise or exercise training due to the potential for disease-modifying effects that can be extrapolated from the known physiological benefits ascribed to regular exercise in the general population. Nearly all known pathophysiologic contributors to sickling and vaso-occlusion, most notably inflammation, oxidative stress, endothelial/vascular dysfunction, and cell adhesion, represent mechanisms known potentially to be ameliorated with exercise training.53-58 In the general population, for example, the long-term cardiovascular benefits of regular exercise are in part attributed to the attenuation over time of the acute-phase inflammatory response to acute exercise.59
We see signals in the literature that exercise training may in fact have disease-modifying effects in SCT and SCA. Blood viscosity and biomarkers of oxidative stress have been found to be lower among individuals with SCT who are trained vs untrained.60,61 In their study, for example, Chirico et al found that in response to exercise, trained subjects with SCA had lower levels of oxidative stress markers, including advanced oxidation protein products (174 ± 121 μM vs 224 ± 130 μM; P = .012), nitrotyrosine (70.6 ± 46.6 nM vs 127 ± 29.1 nM; P = .003), and protein carbonyl (86.9 ± 26.8 nm/mL vs 114 ± 34 nm/mL; P = .006), as well as higher levels of some antioxidant markers, including superoxide dismutase activity (8.5 ± 6.2 U/mL vs 4.3 ± 2.5 U/mL; P = .002) and nitrite and nitrate (28.8 ± 11.4 μM/L per minute vs 4.7 ± 7 μM/L per minute; P = .003), when compared with that measured in untrained subjects with SCT.60 In mouse models of SCA, exercise training is associated with a decrease in overall inflammation, oxidative stress, and exercise-related metabolic acidosis.62-64 Investigators have also begun to examine the role of aerobic exercise training in children and adults with SCA. A 12-week pilot study of home aerobic conditioning in 10 children with SCA using cycle ergometry with escalating duration and exercise intensity up to 30 minutes and 100% of ventilatory threshold, respectively, was safe and feasible.65 Additionally, recent data from 40 adults with SCA undergoing 8 weeks of 3 sessions per week of training by cycle ergometer resulted in improved lactate thresholds during exercise as well as increased capillary density on muscle biopsy.66 Given that leg fatigue represents the most common reason for exercise test termination in studies involving individuals with SCA, adaptive changes at the muscle level with training could in part explain improvements in exercise tolerance in this study.
What are the strategies that have been implemented to mitigate risks in SCT and SCA and what do we need to work toward development of guidelines to address this debate?
Evidence-based guidelines for exercise recommendations currently do not exist for individuals with SCT and SCA. The implications for this are tremendous and may affect up to 8% of the black population that carries SCT and nearly 100 000 individuals living with SCA in the United States alone. For SCT, consensus statements and recommendations have been put forth by various groups, including the US military, the NCAA (https://www.ncaa.org/sites/default/files/NCAASickleCellTraitforCoaches.pdf), the American College of Sports Medicine and the National Athletic Trainer’s Association (https://www.nata.org/sites/default/files/sickle-cell-trait-and-the-athlete.pdf) for mitigating the risk of ECAST.4,67 Applying these recommendations to individuals with SCT may depend on training intensity, training conditions, and training status but commonalities include the following general principles: (1) gradual adjustment to training intensity to facilitate acclimation, especially under extreme conditions (heat or altitude); (2) reduction of activity or training intensity after prolonged illness or rest periods; (3) ready access to fluids at regular intervals; (4) prompt recognition of symptoms suggestive of ECAST, exertional rhabdomyolysis, or heat-related illnesses; and (5) rapid termination of training and prompt initiation of treatment in the event of symptoms. Universal precautions have been in place since 1982 for military recruits and soldiers in training and, since their institution, the branches of the US military that have implemented safeguards as part of training have observed no difference in rates of sudden deaths, mild heat injury, or heat stroke in recruits with and without SCT.14,67 Despite their longstanding adoption for military recruits and soldiers in training, universal precautions to prevent ECAST have only recently been introduced for college athletes. However, implementation success and adherence to these policies as well as their impact on outcomes are not clear for college athletes.12 Even less guidance for prevention of exercise-related adverse events exists for individuals with SCA. Anecdotally, the principles adopted by patients and their providers generally focus on avoidance of dehydration, extreme temperatures during exercise, and prolonged physical exertion at moderate to high intensity without adequate rest periods.
The development of evidence-based guidelines is critical to implementing safe training and exercise prescription practices among military personnel, athletes, and all individuals with SCT as well as those affected by SCA. Essential questions and remaining knowledge gaps, however, need to be fully addressed before this can be realized, most important of which is finding the right “dose” of exercise that children and adults with SCT and SCA at various levels of fitness need and can tolerate safely. How we strike the right balance between the risks vs benefits of regular exercise, especially at moderate to high intensities, for individuals of different training status remains an important challenge facing these populations (Figure 2). The answer may be different for SCT, which is characterized primarily by an increased risk of exertional rhabdomyolysis under extreme conditions, vs for SCA, which is marked by a proinflammatory state that potentially can be precipitated by the physiologic stress of high-intensity exercise. As such, the potential areas for further investigation probably differ for SCT and SCA as well. For SCT, continued efforts should focus on the following potential areas of impact: (1) mechanisms of exertional rhabdomyolysis and the unique influence/contribution of sickling; (2) genetic basis of exertional rhabdomyolysis and ECAST68 ; (3) environmental and training factors that increase the risk of ECAST; (4) susceptibility of “weekend warriors” to ECAST and the influence of training status on risk of exertional rhabdomyolysis; and (5) development and implementation of evidence-based guidelines for mitigating risk of ECAST. Also worth studying is whether universal SCT screening for individuals at high or higher risk of ECAST remains necessary in the setting of implementing universal precautions around high-intensity exercise and training. For SCA, potential areas of investigation could instead focus on further understanding the following broader themes: (1) evaluating the pathophysiologic consequences of acute exercise, including characterizing the molecular and genetic basis for the inflammatory response to acute exercise; (2) determining the relationship among cardiopulmonary fitness, disease severity, and long-term outcomes, including mortality; (3) exploring the disease-modulating effects of exercise training on inflammation and endothelial and vascular end points on both a physiologic and molecular level; and (4) studying the impact of regular exercise and increased physical activity on pain, quality of life, and other patient-centered outcomes. Systematically addressing these issues has the potential for better understanding the short- and long-term effects of exercise using an ideal model for blood disorders such as SCA with potential application to other blood disorders, both malignant and nonmalignant.
The balance of short-term potential risks of acute exercise vs long-term benefits of regular exercise in individuals with SCT and SCA.
The balance of short-term potential risks of acute exercise vs long-term benefits of regular exercise in individuals with SCT and SCA.
Summary
In summary, SCT and SCA have in common the presence of sickle hemoglobin in erythrocytes that predispose to sickling, generally of minimal consequence in the former but associated with complications throughout the lifespan in the latter. There has been a renewed interest in the risks vs benefits of exercise and high-intensity physical exertion in both SCT and SCA in recent years but for different reasons. In SCT, the mechanisms underlying the evidence for increased risk of exertional rhabdomyolysis and ECAST are poorly understood. In SCA, the field is just starting to understand the risks associated with acute exercise for a disease marked by a baseline proinflammatory state. For both, however, discovering the right “dose” of exercise that optimizes the balance between risks and benefits is key. In working toward the development and implementation of evidence-based guidelines for exercise prescription, SCT and SCA also represent ideal models for applying exercise science and medicine to the field of hematologic disorders.
Correspondence
Robert I. Liem, Ann & Robert H. Lurie Children’s Hospital of Chicago, 225 East Chicago Ave, Box 30, Chicago, IL 60611; e-mail: rliem@luriechildrens.org.
References
Competing Interests
Conflict-of-interest disclosure: The author declares no competing financial interests.
Author notes
Off-label drug use: None disclosed.