Abstract
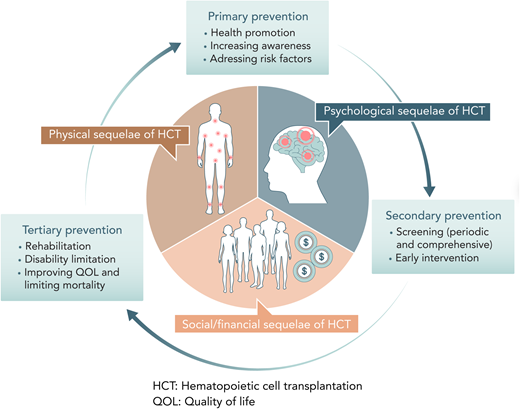
With improvement in survival after hematopoietic cell transplantation (HCT), it has become important to focus on survivors' psychosocial issues in order to provide patient-centered care across the transplant continuum. The goals of this article are to describe updates in the literature on certain psychosocial domains (emotional/mental health and social/financial) in HCT survivors, offer a brief overview of the status of the screening and management of these complications, and identify opportunities for future practice and research. An evidence-based approach to psychosocial care can be broken down as primary (promoting health, raising awareness, and addressing risk factors), secondary (screening and directing early pharmacological and nonpharmacological interventions), and tertiary (rehabilitating, limiting disability, and improving quality of life) prevention. Implementing such an approach requires close coordination between multiple stakeholders, including transplant center staff, referring hematologist/oncologists, and other subspecialists in areas such as palliative medicine or psychiatry. Innovative models of care that leverage technology can bring these stakeholders together to fulfill unmet needs in this area by addressing barriers in the delivery of psychosocial care.
Learning Objectives
Understand the burden of psychosocial complications after hematopoietic cell transplantation
Describe the approach to screening and managing these complications
Recognize barriers in the delivery of psychosocial care
CLINICAL CASES
J. B. is a 47-year-old non-Hispanic White female who is 6 years post C antigen mismatched unrelated-donor peripheral blood hematopoietic cell transplant (HCT) for acute myeloid leukemia. She had chronic graft-versus-host disease (GVHD) of the skin, fascia, and joints and is currently on treatment with prednisone, sirolimus, and extracorporeal photopheresis. She also had multiple other complications, including a chronic nonhealing ulcer of the left shin, left-lower-extremity deep vein thrombosis, chronic renal insufficiency, and a fracture of the left femur due to osteoporosis, which then ended up as a mycobacterial infection of the hip joint after surgery. She got divorced 1 year after hematopoietic cell transplantation (HCT) and lost her job 3 years after the HCT due to missing work frequently. She is extremely depressed due to the ongoing medical and financial issues and was recently hospitalized for expressing suicidal intent.
A. R. is a 14-year-old Hispanic male who received a matched unrelated-donor bone marrow transplant for Wiskott-Aldrich syndrome at 10 months of age. His parents emigrated from Mexico without extended family just before his transplant. Medicaid coverage was adequate, with minimal out-of-pocket expenses or deductibles, but the stress of having barely enough money for food and necessities was high, especially during the early posttransplant period. Soon after the HCT, the father ran out of paid time off and was forced to take unpaid time off work. The parents shared duties during and after transplant, often neglecting their own health care needs. A. R. did well from a medical standpoint but has lasting cognitive and academic deficits and behavioral problems that make it difficult for him to manage school. This has led to a great deal of stress for his parents, especially since they have little social support.
Introduction
J. B. and A. R. illustrate some of the issues faced by 100 000 HCT survivors in the United States, a population projected to increase 5-fold by 2030.1 The cost of cure is the physical, psychological, and social sequelae of HCT that have a detrimental impact on the quality of life of these survivors after HCT (Table 1). HCT survivors and their caregivers have identified these concerns as “what matters to them,” and addressing them is an important component for delivery of high-quality care.2 Unmet needs in emotional health and financial burden in HCT survivors have been recently described.3
Physical, psychological, and social sequelae of HCT
| Physical sequelae . | Psychological sequelae . | Social sequelae . |
|---|---|---|
| Poor physical and mental health | Depression/anxiety | Financial distress |
| Fatigue, sleep, pain | Perceived stress | Social reintegration |
| Sexual dysfunction | Adverse coping | Return to work |
| Symptom burden | Cognitive dysfunction | Social support/marital problems |
| Physical sequelae . | Psychological sequelae . | Social sequelae . |
|---|---|---|
| Poor physical and mental health | Depression/anxiety | Financial distress |
| Fatigue, sleep, pain | Perceived stress | Social reintegration |
| Sexual dysfunction | Adverse coping | Return to work |
| Symptom burden | Cognitive dysfunction | Social support/marital problems |
The goal of this article is to describe the updates in the literature for the last 5 years for psychosocial domains (emotional/mental health and social/financial) across the HCT trajectory describing the burden of the problem, with a special focus on the pediatric/adolescent and young adult (AYA) group. Many seminal studies conducted earlier are not included. We also do not include physical and sexual functioning concerns and psychosocial outcomes for HCT caregivers, though they may be highly related to the domains of interest. We conclude by reviewing the current status of screening and management of these complications and opportunities for improvement, including possible incorporation of recently tested psychosocial interventions in practice, and highlight the barriers and models of care to address these complications.
Emotional and mental health and cognitive problems after HCT
Psychological sequelae following allogeneic HCT, the importance of which cannot be underestimated, have been documented (depression, anxiety, perceived stress, adverse coping, and neurocognitive dysfunction). Potential risk factors for psychological sequelae following HCT are numerous; however, female gender, younger age, not living with a partner, and chronic GVHD appear to be salient predictors of impairment. Among allogeneic HCT survivors, the most frequently reported unmet needs are focused on psychological sequelae.4 Despite this, few studies of psychological sequelae have been conducted in long-term HCT survivors in a contemporary cohort. These studies are often subject to a variety of methodological limitations (small or often heterogeneous samples, a lack of longitudinal data with short follow-up, and the use of variable measures).
Depression and anxiety have been reported in 12% to 30% of HCT survivors.4,5 Even at very distal time points as long as >20 years following HCT, depression and anxiety remain a frequent problem.6 While 22% to 43% of HCT survivors suffer from emotional distress, posttraumatic stress disorder is relatively infrequent (3%–13%).7 Importantly, adaptive or maladaptive coping strategies play a crucial role in the occurrence and impact of psychological sequelae.8,9
Estimates suggest that 10% to 40% of HCT survivors experience neurocognitive dysfunction when measured with neuropsychological testing; however, estimates are higher when self- reported (40%–60%).4 A proportion of HCT survivors may experience persistent neurocognitive dysfunction, while other survivors may experience improvements over time. Age, sex, education, income, cognitive reserve, type of HCT, and conditioning intensity are predictive factors for post-HCT cognitive impairment. Specific domains (ie, motor functioning) appear to be disproportionately impaired to a greater extent, whereas others may be spared.10
Social and financial problems after HCT
Medical complications after HCT along with the physical and psychological problems described above can adversely affect the social well-being as well as the employment and financial status of survivors. In turn, financial hardship due to reduced income, loss of employment, and the cost of care for ongoing active medical issues can exacerbate the stress and worsen the psychological problems. Financial toxicity has emerged as an important complication of HCT, as multiple studies have demonstrated patients' poor financial well-being after HCT. A lack of well-validated instruments to measure social and financial outcomes, the use of mostly small institutional studies, and the absence of longitudinal data are some of the gaps in research for this complication of HCT. The prevalence of financial hardship ranges from 20% to 70% of HCT survivors.4,11-15 In addition to the sociodemographic factors, chronic GVHD in allogeneic HCT survivors is a major factor associated with financial stress, as two-thirds of chronic GVHD patients endure financial hardship despite health insurance, and these are likely to be patients with lower household income.16 Denials and delays in care due to insurance and loss of coverage are common stressors faced by HCT survivors. Financial hardship in HCT survivors is known to be associated with poor quality of life, higher perceived stress, nonadherence to treatment, higher symptom burden, and low satisfaction with care but, fortunately, no impact on survival.11,12,16,17
The return to work (RTW) is an indicator of functional recovery for transplant survivors, and the inability to RTW may be associated with financial burden. Only about half of the patients who previously contributed to household earnings may be able to RTW by 2 years after HCT.18 Chronic GVHD is a major factor influencing RTW/sick leave, with one-quarter of patients with chronic GVHD reporting being “disabled/unable to work” at a median of 2 years post HCT.16,19 Lower physical functioning, multimorbidity, being female, and the receipt of peripheral blood stem cells for an unrelated HCT are associated with a lower likelihood of RTW post HCT.20-22 A lack of standard guidelines for RTW leading to poor communication between providers, patients, and employers can be a barrier to successful reintegration of patients in the workplace after HCT.23
While a majority of HCT survivors show reasonable levels of social adjustment, those with fatigue may be at risk for maladjustment and may need effective rehabilitation strategies.24 Social reintegration and social support, including emotional, informational, and logistical support, can help mitigate the effects of psychosocial problems, as illustrated by studies in cancer patients. One of the positive sequelae of overcoming traumatic stressors caused by life-threatening disease and intensive treatment reported in HCT survivors is the phenomenon of “posttraumatic growth.” The roles of emotional and instrumental social support, social constraints, and support from health care professionals in promoting posttraumatic growth have been elucidated further in the last few years.14,25
Specific considerations for pediatric/AYA populations
Pediatric patients are vulnerable to psychosocial sequelae after HCT. Among pediatric HCT survivors, estimates of physical, psychological, and social dysfunction vary due to heterogeneity in methodological aspects. Longitudinal evaluation of pediatric HCT survivors is vital because the ability to assess specific constructs in children changes over time; however, prospective longitudinal data in pediatric HCT survivorship care are infrequent. Symptom burden is greater and health-related quality of life is poorer when compared to healthy peers, though comparable with conventionally treated cancer survivors.26 Health problems may prevent 16% of survivors from attending school; however, the need for special education services at school was similar between pediatric HCT survivors and conventionally treated survivors.27 Depression as well as anxiety is often noted among pediatric HCT survivors as compared to healthy peers. A recent study found that 16% of pediatric HCT survivors endorsed depression, whereas 10% of survivors endorsed anxiety.28 Neurocognitive dysfunction is prevalent in about 50% of pediatric HCT survivors.28 The domain of motor development was affected to the greatest extent; however, language, social, and emotional development was also impaired compared to healthy peers.
AYA survivors of HCT are a unique population that require special care considerations. HCT and its sequelae may undermine the ability of AYA survivors to achieve milestones such as graduating from college, selecting a career, and establishing employment as well as achieving socioeconomic independence from parents, serving as a risk factor for adverse psychosocial outcomes.29,30 Despite the importance of developing a greater understanding of the AYA experience within the context of HCT survivorship, few studies have focused on psychosocial sequelae among AYA survivors of HCT. When we compare AYA survivors to healthy peers, decrements in physical and social functioning and health become apparent.31,32 AYA survivors of HCT report feeling left behind their peers, which sometimes leads them to rush back to work and school and take on too many responsibilities too quickly, resulting in overwhelming demands.33 RTW and employment issues continue to be major psychosocial challenges for AYA survivors of HCT.34
Risk factors for adverse psychosocial outcomes among AYA survivors of HCT include sociodemographic (age, education level, etc), transplant-related (conditioning regimens with total body irradiation), and posttransplant factors such as chronic health conditions and chronic GVHD. AYA survivors of HCT have a myriad of unmet psychosocial needs that differ from other HCT survivors, indicating a necessity to develop interventions specifically tailored to them.35
Screening for and interventions to help improve psychosocial health in HCT survivors
Most transplant centers perform some form of psychosocial evaluation, including financial assessment of HCT candidates prior to HCT. Table 2 provides examples of some of the screening instruments used in clinical practice, though these may not necessarily be limited to the HCT population. However, there is a lot of variability in terms of frequency and types of these assessments before and after HCT at various transplant centers. Also, the approach when addressing these issues is usually reactive rather than proactive. Increasing awareness is vital to identify survivors and their family members who may benefit from additional in-depth assessment and referral for resources for these issues. Guidelines for post-HCT care recommend periodic screening for psychosocial difficulties, especially depression, after transplant, at 6 and 12 months, and annually thereafter.36 They also recommend mental health professional counseling for those with recognized deficits and regular assessments of spousal/caregiver psychological adjustment and family functioning while encouraging robust support networks. Universal screening for financial distress should be added to the usual assessments since it is prevalent and affects patient outcomes.37
Examples of psychosocial and financial screening tools
| Scale . | Description . |
|---|---|
| Psychosocial Assessment of Candidates for Transplant41 | Describes psychosocial functioning before organ and HCT |
| Transplant Evaluation Rating Scale42 | Describes psychosocial functioning before organ and HCT |
| Psychosocial Assessment Tool—Hematopoietic Cell Transplantation43 | Describes the family psychosocial risk for families of a child undergoing HCT |
| Stanford Integrated Psychosocial Assessment for Transplantation44 | Measures psychosocial readiness for transplant |
| Comprehensive Score for Financial Toxicity45 | Describes the financial distress experienced by cancer patients 18 years of age and older during the past 7 days |
| InCharge Financial Distress/Financial Well-Being Scale46 | Measures responses to one's financial state on a continuum ranging from overwhelming financial distress to no financial distress |
| Scale . | Description . |
|---|---|
| Psychosocial Assessment of Candidates for Transplant41 | Describes psychosocial functioning before organ and HCT |
| Transplant Evaluation Rating Scale42 | Describes psychosocial functioning before organ and HCT |
| Psychosocial Assessment Tool—Hematopoietic Cell Transplantation43 | Describes the family psychosocial risk for families of a child undergoing HCT |
| Stanford Integrated Psychosocial Assessment for Transplantation44 | Measures psychosocial readiness for transplant |
| Comprehensive Score for Financial Toxicity45 | Describes the financial distress experienced by cancer patients 18 years of age and older during the past 7 days |
| InCharge Financial Distress/Financial Well-Being Scale46 | Measures responses to one's financial state on a continuum ranging from overwhelming financial distress to no financial distress |
Developing a set of standard patient-reported outcome measures to be collected at periodic time points and to address the domains most relevant to survivors is crucial. Such measures can help understand the population-based prevalence of these psychosocial issues and screen for problems that would need intervention in real time. Electronic medical records can be leveraged to routinely collect a standardized set of social, psychological, and behavioral determinants of health to integrate this process with routine clinical care. Screening recommendations and possible management options may also be incorporated into survivorship care summaries to facilitate the delivery of psychosocial care across the trajectory of HCT care.38 It is interesting to note that these individualized care plans as educational tools can lead to reduced distress and improvement in the mental domain of health-related quality of life, as shown by a recent randomized clinical trial.39
There is a need for interventions specific to HCT survivors that are evidence based and leverage novel platforms to improve accessibility, with the goal of mitigating risks and improving outcomes following HCT. Table 3 summarizes some of the interventions that have attempted to address the psychosocial domains in HCT survivors. These interventions were largely aimed at depression, anxiety, stress, and coping, with only one intervention focused on cognitive dysfunction. To our knowledge, in the last 5 years no interventions have been published focusing on financial hardship or social health among HCT survivors specifically, suggesting a concerning gap in the care of HCT survivors and their families. Most intervention studies have been by single institutions employing small sample sizes to assess acceptability as well as feasibility. Most studies were not appropriately powered to assess efficacy and require future evaluation within the context of larger randomized controlled trials.
Psychosocial interventions for HCT survivors
| Author . | Sample . | Study design . | Intervention . | Measures . | Findings . |
|---|---|---|---|---|---|
| Depression/anxiety | |||||
| Copeland et al47 | n = 20, allogeneic HCT, >18 years of age | Single-arm prospective pre-HCT, day 0, +14, +30, +60 | Weekly collaborative care meetings with HCT clinicians and psychiatrist, review case and provide pharmacologic recommendations and psychosocial counseling referrals | Hospital Anxiety and Depression Scale | Anxiety decreased and depression decreased (pre- to day +60). |
| Kim et al48 | n = 40, mean age 59.2 years | Randomized (intervention or information control) pre- and post assessment | Digital storytelling—four 3-minute personal/emotionally rich stories about post-HCT care | POMS subscales for depression and anxiety, PROMIS Social Support scale | Perceived social support increased for intervention and decreased for control. Anxiety and depression improved with time for both. |
| Coping/stress | |||||
| Balck et al49 | n = 91, allogeneic and autologous, >18 years of age | Randomized (intervention or control group) pre-HCT, day +11, +23 | Problem-solving training | HADS, SCL-9, Brief Cope, Social Problem-Solving Inventory-R, Questions of Pain, NCCN Distress Thermometer | Anxiety, distress, pain, stress were lower and active coping better with intervention. Better able to reduce negative orientation and problem-solve with intervention. |
| Somers et al50 | n = 36, allogeneic and autologous (83%), mean age 56 years | Randomized (intervention or usual treatment) pre- and post assessment | Mobile pain-coping skills: website with personalized messages and pain assessment activity. Materials (handouts, videos, audio files) about pain-coping advice from patients and how to apply pain-coping skills | Brief pain inventory, pain disability index, pain subscale of the chronic pain self-efficacy scale, PROMIS Fatigue scale, FACT well-being scale, 2MWT | Intervention with improved pain, self-efficacy, and on the 2MWT, and no improvement in the control group. Changes in pain disability and fatigue in both groups; effect sizes were larger for the intervention group. No changes in pain severity in either group. |
| Majhail et al39 | n = 458, allogeneic (48%) intervention arm, (44%) control arm, median age 59 years for both arms | Randomized (intervention or control) pre- and post assessment (6 months) | Survivorship care plan | CSI, CTXD, Knowledge of Transplant Exposures, Health Care Utilization, SF-12 | Intervention—lower distress scores at 6 months and greater mental health scores |
| Syrjala et al40 Syrjala et al51 Yi et al52 | n = 755, allogeneic and autologous (27%), mean age 51 years | Randomized (intervention or intervention + problem- solving training or control—delayed access to intervention) pre- and post assessment (6 months) | INSPIRE—tailored web page with topics (1) lift mood, reduce fatigue, boost health; (2) self-care tips and tools; (3) tailored care guidelines; (4) forum for posting experiences and for input; (5) resource list problem-solving—focus on problems and goal setting with psychologists (>4 sessions) | CTXD, SCL-90-R Depression Scale, SF-36, FSI | INSPIRE+ problem-solving training more likely to improve in distress than controls. Male, age <40 years, African Americans were less likely to enroll. Engagement did not differ by race, education, income, rural/urban residence, computer experience, donor type, or presence of depression. |
| Cognitive/developmental | |||||
| Ferraro et al53 | n = 110 | Feasibility study of screening at pre-HCT, day +100, 2 years, 5 years post HCT | MoCA, BACH | Neurocognitive screening is feasible to do prior to and post transplant. | |
| Hoodin et al54 | n = 9, allogeneic HCT, mean age 53 years, control cohorts— concurrent longitudinal study | Ancillary study and feasibility of assessing vorinostat, cognitive function, and QOL baseline, day 30, 100, 160 | Vorinostat + Tac + MTX for GVHD prophylaxis | Cogstate, PHQ-9, GAD-7, FACT-General | Neurocognitive function, depression, anxiety, quality of life did not differ across time. Modeling—neurocognitive function in vorinostat patients compared to auto controls was equivalent and better than allo controls. |
| Author . | Sample . | Study design . | Intervention . | Measures . | Findings . |
|---|---|---|---|---|---|
| Depression/anxiety | |||||
| Copeland et al47 | n = 20, allogeneic HCT, >18 years of age | Single-arm prospective pre-HCT, day 0, +14, +30, +60 | Weekly collaborative care meetings with HCT clinicians and psychiatrist, review case and provide pharmacologic recommendations and psychosocial counseling referrals | Hospital Anxiety and Depression Scale | Anxiety decreased and depression decreased (pre- to day +60). |
| Kim et al48 | n = 40, mean age 59.2 years | Randomized (intervention or information control) pre- and post assessment | Digital storytelling—four 3-minute personal/emotionally rich stories about post-HCT care | POMS subscales for depression and anxiety, PROMIS Social Support scale | Perceived social support increased for intervention and decreased for control. Anxiety and depression improved with time for both. |
| Coping/stress | |||||
| Balck et al49 | n = 91, allogeneic and autologous, >18 years of age | Randomized (intervention or control group) pre-HCT, day +11, +23 | Problem-solving training | HADS, SCL-9, Brief Cope, Social Problem-Solving Inventory-R, Questions of Pain, NCCN Distress Thermometer | Anxiety, distress, pain, stress were lower and active coping better with intervention. Better able to reduce negative orientation and problem-solve with intervention. |
| Somers et al50 | n = 36, allogeneic and autologous (83%), mean age 56 years | Randomized (intervention or usual treatment) pre- and post assessment | Mobile pain-coping skills: website with personalized messages and pain assessment activity. Materials (handouts, videos, audio files) about pain-coping advice from patients and how to apply pain-coping skills | Brief pain inventory, pain disability index, pain subscale of the chronic pain self-efficacy scale, PROMIS Fatigue scale, FACT well-being scale, 2MWT | Intervention with improved pain, self-efficacy, and on the 2MWT, and no improvement in the control group. Changes in pain disability and fatigue in both groups; effect sizes were larger for the intervention group. No changes in pain severity in either group. |
| Majhail et al39 | n = 458, allogeneic (48%) intervention arm, (44%) control arm, median age 59 years for both arms | Randomized (intervention or control) pre- and post assessment (6 months) | Survivorship care plan | CSI, CTXD, Knowledge of Transplant Exposures, Health Care Utilization, SF-12 | Intervention—lower distress scores at 6 months and greater mental health scores |
| Syrjala et al40 Syrjala et al51 Yi et al52 | n = 755, allogeneic and autologous (27%), mean age 51 years | Randomized (intervention or intervention + problem- solving training or control—delayed access to intervention) pre- and post assessment (6 months) | INSPIRE—tailored web page with topics (1) lift mood, reduce fatigue, boost health; (2) self-care tips and tools; (3) tailored care guidelines; (4) forum for posting experiences and for input; (5) resource list problem-solving—focus on problems and goal setting with psychologists (>4 sessions) | CTXD, SCL-90-R Depression Scale, SF-36, FSI | INSPIRE+ problem-solving training more likely to improve in distress than controls. Male, age <40 years, African Americans were less likely to enroll. Engagement did not differ by race, education, income, rural/urban residence, computer experience, donor type, or presence of depression. |
| Cognitive/developmental | |||||
| Ferraro et al53 | n = 110 | Feasibility study of screening at pre-HCT, day +100, 2 years, 5 years post HCT | MoCA, BACH | Neurocognitive screening is feasible to do prior to and post transplant. | |
| Hoodin et al54 | n = 9, allogeneic HCT, mean age 53 years, control cohorts— concurrent longitudinal study | Ancillary study and feasibility of assessing vorinostat, cognitive function, and QOL baseline, day 30, 100, 160 | Vorinostat + Tac + MTX for GVHD prophylaxis | Cogstate, PHQ-9, GAD-7, FACT-General | Neurocognitive function, depression, anxiety, quality of life did not differ across time. Modeling—neurocognitive function in vorinostat patients compared to auto controls was equivalent and better than allo controls. |
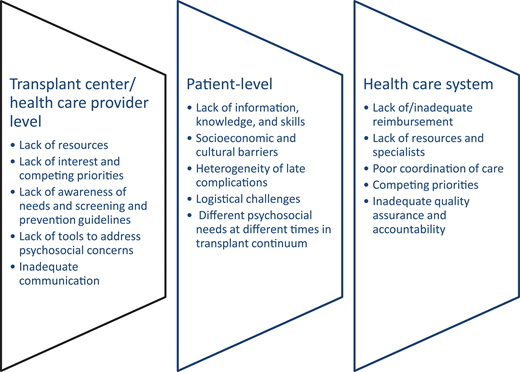
Barriers to psychosocial care delivery and models to address barriers
Many barriers at different levels need to be overcome to recognize and adequately treat the psychosocial concerns of HCT survivors in routine clinical practice (Figure 1). Even if we identify HCT survivors in need of psychosocial support, providing in-depth assessments with connectivity to available resources in a personalized fashion and translating the research in psychosocial interventions to actual clinical practice remains a challenge.
To overcome this challenge, we need to develop and implement effective models for delivering psychosocial care. These models should be based on the 3-step approach to prevention of these complications. The first step or primary prevention would include health promotion activities, including using transplant as a “teachable moment” for promoting health behavior change, increasing awareness, and preemptively trying to address risk factors for these complications. Secondary prevention would include screening that, as reviewed above, should be comprehensive, performed multiple times post HCT, and lead to actionable care pathways possibly incorporating the tested interventions in routine care. Tertiary prevention targeted at decreasing morbidity and mortality from these complications would include rehabilitation strategies and disability limitation.
Implementing the above approach requires integration of all the relevant stakeholders, such as the transplant team, primary care or oncology physician, psychologist or psychiatrist, social workers, and financial counselors (Table 4). With the increased focus on virtual medicine because of the COVID-19 pandemic, there is an opportunity to leverage virtual technologies to deliver well-rounded, risk-stratified survivorship care incorporating psychosocial screening and interventions. This can help encourage health-related self-efficacy in patients, increase health system capacity, and promote adaptive HCT survivorship. Online programs may help address some of the barriers in providing psychosocial care such as distance, varying needs, and lack of standard follow-up care. Recently, the INSPIRE (Internet-Based Survivorship Program with Information and Resources) study found no differences between the study arms in the primary end point of aggregated outcomes of cancer and treatment distress, depressive symptoms, physical dysfunction, and fatigue, though there was significant improvement in distress alone for those in the INSPIRE+ problem-solving treatment arm.40
HCT psychosocial providers and roles
| Category . | Role . |
|---|---|
| Transplant physician | Provide education to patients and families regarding signs of psychosocial distress associated with HCT Recognize signs of psychosocial distress and assess for psychosocial distress associated with HCT |
| Transplant nurse | Provide education to patients and families regarding signs of psychosocial distress associated with HCT Recognize signs of psychosocial distress and assess for psychosocial distress associated with HCT |
| Social worker/case manager | Educate, recognize, and assess for psychosocial distress. Facilitate patient and family adjustment to the process of HCT and its sequelae. Refer patients and families with distress for specialized services and community resources. Address a range of psychosocial and financial needs (eg, insurance benefits, coordination of care, navigating health system, peer support). |
| Psychologist | Provide consultation and management of psychosocial concerns identified among HCT patients and families using various psychotherapeutic techniques. Assist in the control of symptoms (eg, anxiety, depression) that may impact patient and family well-being. |
| Psychiatrist | Diagnose and treat psychologic and psychiatric disorders that arise during HCT using psychopharmacologic interventions. Assist in the control of symptoms (eg, anxiety, depression) that may impact patient and family well-being. |
| Chaplain, clergy, pastoral care | Assist patients and families with coping, spiritual counseling. |
| Patient financial services | Assist patient and families with prior authorization, payment plans to put together an appeal for denials to help with costs of care. |
| Primary care physician/primary hematologist/oncologist | Work closely with transplant team to screen and address psychosocial issues and provide support. |
| Category . | Role . |
|---|---|
| Transplant physician | Provide education to patients and families regarding signs of psychosocial distress associated with HCT Recognize signs of psychosocial distress and assess for psychosocial distress associated with HCT |
| Transplant nurse | Provide education to patients and families regarding signs of psychosocial distress associated with HCT Recognize signs of psychosocial distress and assess for psychosocial distress associated with HCT |
| Social worker/case manager | Educate, recognize, and assess for psychosocial distress. Facilitate patient and family adjustment to the process of HCT and its sequelae. Refer patients and families with distress for specialized services and community resources. Address a range of psychosocial and financial needs (eg, insurance benefits, coordination of care, navigating health system, peer support). |
| Psychologist | Provide consultation and management of psychosocial concerns identified among HCT patients and families using various psychotherapeutic techniques. Assist in the control of symptoms (eg, anxiety, depression) that may impact patient and family well-being. |
| Psychiatrist | Diagnose and treat psychologic and psychiatric disorders that arise during HCT using psychopharmacologic interventions. Assist in the control of symptoms (eg, anxiety, depression) that may impact patient and family well-being. |
| Chaplain, clergy, pastoral care | Assist patients and families with coping, spiritual counseling. |
| Patient financial services | Assist patient and families with prior authorization, payment plans to put together an appeal for denials to help with costs of care. |
| Primary care physician/primary hematologist/oncologist | Work closely with transplant team to screen and address psychosocial issues and provide support. |
CLINICAL CASES (continued)
In addition to the management of J. B.'s medical complications, a multidisciplinary team that included her transplant physician, nurse, and social worker; patient financial services; and providers from palliative medicine and psychiatry/psychology came together to help her manage her various issues and provide coordinated care. Frequent touch points with her using virtual visits made her feel that her team was engaged in her overall care. Participating in a support group for chronic GVHD patients helped her feel emotionally supported.
For the financial hardship, A. R.'s family was referred to a local charitable organization that provided grant funds for rent assistance. Due to his cognitive and academic challenges, A. R. was referred for formal neuropsychological evaluation. Based upon the detailed evaluation, the HCT clinical team and A. R.'s parents worked closely with the child's school, including his teachers and the administration, to develop an appropriate, individualized education plan for A. R. With additional support in the classroom, A. R. was able to make modest gains in his academic success.
Future directions
Table 5 provides a suggested outline of research priorities and areas of clinical focus when considering potential psychosocial risk and financial distress among HCT survivors. With advances in treatment practices and survival after HCT, there is an increasing recognition of the adverse impact of transplant on psychosocial aspects of survivorship, including the need to proactively collect and intervene in patient-reported outcomes after HCT. Multiple initiatives in the field of HCT are beginning to identify the gaps in practice and research and recognize the importance of integrating patient-centered outcome screening and interventions with the goal of improving long-term health outcomes after HCT.2,4 The role of educational initiatives to empower and engage patients and their caregivers in improving their psychosocial health is extremely valuable. A multipronged approach to address psychosocial concerns utilizing all relevant stakeholders can go a long way in ensuring the long-term success of this medically complicated, resource-intensive procedure.
Recommended areas of focus for future research priorities and clinical practice
| Area . | Focus . |
|---|---|
| Study design and measures | Proactively collect psychosocial and financial health data among HCT patients and families across the entire trajectory of transplant care (longitudinal) using large, representative samples. Increase focus on special populations—children, adolescents, and young adults, older adults, racial/ethnic minority patients. Use well-validated and standard patient-reported outcome measures. |
| Screening and assessment | Develop evidence-based recommendations for universal screening and assessment of HCT patients and families at defined time points across the entire transplant trajectory using a standard set of patient-reported outcome measures focused on psychosocial and financial distress. Leverage technology to ensure robust connectivity to HCT center and community-based resources. |
| Rehabilitation and intervention | Develop and test effective rehabilitation strategies, social support (emotional, informational, and logistical) interventions, and financial support interventions. Employ novel platforms for delivery and developmentally tailored for special populations. |
| Education and awareness | Raise awareness regarding psychosocial and financial health through various means including educational efforts directed at all levels including, but not limited to, patients and families as well as transplant care providers and policy-makers. Develop metrics to examine the effectiveness of these measures. |
| Area . | Focus . |
|---|---|
| Study design and measures | Proactively collect psychosocial and financial health data among HCT patients and families across the entire trajectory of transplant care (longitudinal) using large, representative samples. Increase focus on special populations—children, adolescents, and young adults, older adults, racial/ethnic minority patients. Use well-validated and standard patient-reported outcome measures. |
| Screening and assessment | Develop evidence-based recommendations for universal screening and assessment of HCT patients and families at defined time points across the entire transplant trajectory using a standard set of patient-reported outcome measures focused on psychosocial and financial distress. Leverage technology to ensure robust connectivity to HCT center and community-based resources. |
| Rehabilitation and intervention | Develop and test effective rehabilitation strategies, social support (emotional, informational, and logistical) interventions, and financial support interventions. Employ novel platforms for delivery and developmentally tailored for special populations. |
| Education and awareness | Raise awareness regarding psychosocial and financial health through various means including educational efforts directed at all levels including, but not limited to, patients and families as well as transplant care providers and policy-makers. Develop metrics to examine the effectiveness of these measures. |
Conflict-of-interest disclosure
David Buchbinder: no competing financial interests to declare.
Nandita Khera: no competing financial interests to declare.
Off-label drug use
David Buchbinder: nothing to disclose.
Nandita Khera: nothing to disclose.