Key Points
COVID-19 occurs commonly in working-age patients with CML under treatment with different generations of TKIs, especially in older males.
Patients without hematological response experienced an unfavorable evolution of both diseases: CML and SARS-CoV-2 infection.
Visual Abstract
An increasing number of publications suggested a higher susceptibility to COVID-19 infection among patients with leukemias than the allegedly healthy population. The aim of the study was to assess the epidemiological, clinico-biological features and management outcomes of chronic myeloid leukemia (CML) in association with COVID-19. This analytical study included 20 patients with CML with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, who were treated at the Institute of Oncology in Moldova between 2020 and 2023. These patients with CML with COVID-19 represented 13.2% of 151 patients being followed up under tyrosine kinase inhibitor (TKI) treatment. According to the World Health Organization classification of COVID-19, mild forms were recorded in 5 patients (25%), moderate in 10 (50%), and severe in 5 (25%). No correlation was found between the duration of CML and severity of COVID-19. SARS-CoV-2 infection occurred during treatment with imatinib in 12 (60%), nilotinib in 5 (25%), and ponatinib in 3 (15%). All 5 patients (25%) with severe and 7 (35%) with moderate forms were hospitalized for COVID-19 treatment. Viral pneumonia emerged in 9 (45%). SARS-CoV-2 infection developed commonly in older males with advanced CML phases. There was no significant difference in morbidity by COVID-19 in patients aged <75 years treated with various generations of TKIs.
Introduction
Chronic myeloid leukemia (CML) represents 15% to 20% of all leukemia cases in adults and is the most common chronic myeloproliferative neoplasm, with significant global disease burden and rate of disability-adjusted life years in its advanced phases.1-8 During the last 2 decades, the advent of coronavirus-associated diseases (severe acute respiratory syndrome and Middle East respiratory syndrome [MERS]) entailed global challenges to public health systems in a lot of countries. The World Health Organization (WHO) proclaimed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection a public health emergency of international concern on 30 January and a pandemic on 11 March 2020.9,10 Recent publications suggested a higher susceptibility of patients with leukemia to COVID-19 infection and its superior incidence (1%) compared to the allegedly healthy population (0.1%). Nevertheless, these appraisals remain controversial. The risk of occurrence of SARS-CoV-2 infection persists, not being comprehensively evaluated in different types of hematological malignancies (HMs) at the global level.11-13
The aim of the study was to outline and assess the epidemiological, clinico-biological features and management outcomes of CML in association with COVID-19.
Study design
We reported on the analytical, prospective study of 20 patients with CML and COVID-19 infection, who were treated at the Institute of Oncology in Moldova between 2020 and 2023. SARS-CoV-2 infection was diagnosed only in these 20 patients from the total number of CML cases treated with tyrosine kinase inhibitors (TKIs) during this period. All CML cases were diagnosed in chronic phase (CP) by molecular genetic testing of the bone marrow and peripheral blood. The expression of BCR-ABL p210 and p190 transcripts was determined by quantitative reverse transcription polymerase chain reaction.7 Nucleic acid amplification with an reverse transcription polymerase chain reaction assay was performed to identify SARS-CoV-2 RNA from the upper respiratory tract as a preferential initial diagnostic test for COVID-19 detection.14 The severity degree of infection was identified according to WHO guidelines for the certification and classification (coding) of COVID-19.14-16
The research protocol was approved by the research ethics board of Nicolae Testemitanu State University of Medicine and Pharmacy.
Results and discussion
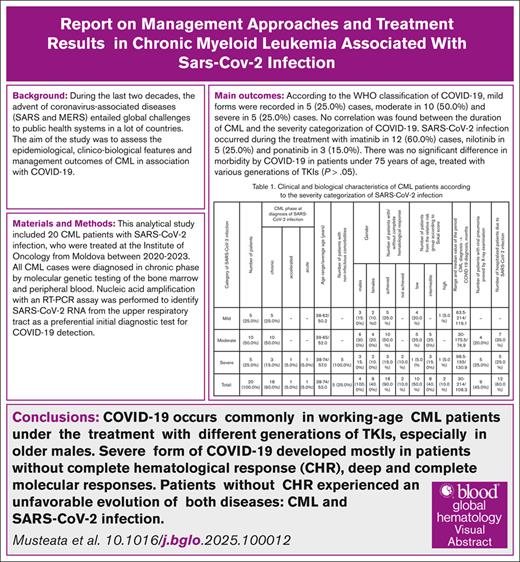
The 20 analyzed patients with CML with SARS-CoV-2 infection represented 13.2% of 151 unvaccinated patients diagnosed with CML and followed up under TKI treatment between 2020 and 2023. Of these 20 patients, COVID-19 appeared in only 2 (5.9%) of 34 newly diagnosed patients with CML (22.5%) who were initially treated with TKIs during COVID-19 pandemic. Patients diagnosed with CML before the onset of the COVID-19 pandemic had a higher morbidity rate of SARS-CoV-2 infection than patients with CML with shorter duration (12% vs 5.9%; P < .05). There were 12 males (60%) and 8 females (40%), with a male-to-female ratio of 1.5:1 (Table 1), whereas the male-to-female ratio in patients with CML without infection was 1.1:1. The age at diagnosis of COVID-19 ranged from 38 to 74 years (average age, 53 years). Nine patients (45%) were aged <50 years, 11 patients (55%) were aged ≥50 years, and 7 (35%) were aged >60 years. The average age of patients with CML without infection was lower at 47.7 years (P < .05). These data suggested that older patients with CML were more susceptible to COVID-19, consistent with studies of patients in the same age category with other HMs treated at the Institute of Oncology or published at the international arena.11-13
According to the WHO classification of COVID-19 severity,14-16 mild form (MdF) was recorded in 5 (25%), moderate form (MF) in 10 (50%), and severe form (SF) in 5 patients (25%). Three of 5 patients with SF and 3 patients (30%) with MF were aged between 60 and 70 years. CML lasted from 30 to 214 months (average period, 108.3 months) before the diagnosis of SARS-CoV-2 infection. No correlation was found between CML span and the severity of COVID-19 (r = 0). Comorbidities were recorded in patients with SF of SARS-CoV-2 infection: cardiovascular diseases in 3 patients (15%) and type 2 diabetes in other 2 (10%).
This study evaluated the impact of Sokal score at CML diagnosis on morbidity due to COVID-19. SARS-CoV-2 affected 10 low-risk (50%), 8 intermediate-risk (40%), and 2 high-risk group patients (10%). MF emerged in 5 low-risk (25%) and in 5 intermediate-risk patients (25%). SF developed in 3 intermediate-risk group patients (15%) and in 1 patient (5%) each from low- and high-risk groups. Therefore, the intermediate- and high-risk Sokal scores at CML diagnosis did not influence the rate and clinical course of COVID-19 infection (P > .05).
COVID-19 developed in 18 patients (90%) with complete hematological response (CHR) and in 2 (10%) without stable hematological response. Sixteen patients (80%) achieved complete or deep molecular response (MR) before COVID-19 diagnosis. MdF of COVID-19 occurred in 1 patient (5%) with partial MR. Three patients (15%) without MR, including those lacking CHR, experienced SF. Molecular relapse developed after SARS-CoV-2 infection in 4 patients (20%) with previously obtained complete MR. There were no significant differences in morbidity due to COVID-19 between patients treated with different generations of TKIs (P > .05).
All 5 patients (25%) with SF and 7 (35%) with MF were hospitalized for treatment of SARS-CoV-2 infection. Viral pneumonia was diagnosed by radiological examinations in 5 patients (25%) with SF and in 4 (20%) with MF. An oral antiviral medication with umifenovir was administered at onset in 4 patients (20%) with MF and in 5 (25%) with SF. Oral medication was followed by remdesivir in 2 patients (10%) with SF and without CHR. All hospitalized patients received steroid therapy with dexamethasone. TKIs were discontinued for the period of hospitalization in patients with CHR. The duration of hospitalization ranged from 9 to 17 days (average duration, 13.5 days). Ten patients (83.4%) were discharged from the hospital with a negative diagnostic test result for COVID-19. Two patients (16.6%) with SF died due to the viral pneumonia, acute cardio-respiratory failure, and CML progression into accelerated and acute phases. Patients without CHR experienced unfavorable evolution of both diseases.
The epidemiological and clinical aspects of COVID-19 in patients with CML are reflected in the literature equivocally and mostly at the national/regional levels.12,17-20
In the updated CANDID study, the average age of patients with CML with COVID-19 (53 years; range, 18-94) was higher than the total patients with CML population.4,17 COVID-19 mostly affected males (59%). In 2021, only 642 cases (0.7%) of COVID-19 were reported among 37 449 patients with CML from 50 countries, which might suggest that the immune status in CP-CML was not a contributing factor to the development of this viral disease.17 MdF (n = 363 [56%]) and MF (n = 119 [18%]) proved to be the most common forms of COVID-19 in patients with CML, with no significant difference compared to the global population.18,21,22 The median time from CML diagnosis confirmation to the onset of COVID-19 was longer, at 8.34 years (range, 0-34), than that of our patients. At the data cutoff, of 606 followed up patients, 48 (8%) died and 558 (92%) recovered. Univariate analysis revealed a higher mortality rate and lower overall survival (OS; P < .001) in patients aged ≥75 years (OS, 80%), as well as in patients with comorbidities (OS, 90%) and those from low- and middle-income countries (OS, 71%), the latter presumably related to the constraints in supportive care. Poor outcomes of COVID-19 management emerged in patients with advanced phases (OS, 71%) and in those who failed to achieve a major MR (OS, 88%). Multivariate analysis revealed a significant association of all these risk factors with OS.
The clinical effects of TKIs on treatment outcomes of patients with COVID-19 were studied via age-, sex-, and comorbidity-matched comparisons with the control group.22 The reported differences did not reach statistical significance and included the following: (1) compared with the control group, the rates of intensive care unit admission and mechanical ventilation support were lower and the length of hospitalization was shorter in patients under TKI therapy; and (2) the rate of fatal cases was 6.3% in patients receiving TKIs and 12.8% in the control group. Patients with therapeutically controllable CP-CML did not experience a greater risk of SARS-CoV-2 infection than the general population.22 This study highlighted the reasonability of randomized trials to evaluate the impact of TKI treatment on COVID-19 evolution on a large scale.22,23
During the SARS-CoV-2 infection pandemic, 530 patients with CML were studied in 29 medical centers of the Hubei Anticancer Association (China).20,24 The prevalence of COVID-19 was 0.9% (95% confidence interval, 0.1-1.8), which was 9 times higher than that of the healthy population (0.1%; 95% confidence interval, 0-0.12) but lower than the 10% (95% confidence interval, 6-17) reported among hospitalized patients with other HMs. Covariates associated with an increased risk of developing COVID-19 among patients with CML were exposure to SARS-CoV-2–infected individuals (P = .037), lack of CHR (P = .003) or complete cytogenetic response (P = .004), and comorbidities (P = .024).
The impact of COVID-19 in patients with CML and carefully matched population controls was reflected by a nationwide population-based cohort study from Sweden.18 The overall risks for developing COVID-19, intensive care unit admissions, and case-related mortality proved to be comparable and relatively low.
The monitoring practice for patients with CML was changed for safety reasons during the pandemic at our comprehensive cancer center. The patients, thus, should present negative results of COVID-19 diagnostic test at each monitoring visit to hematologists. The standard periods between follow-up visits were extended in patients with CHR and deep MR. Patients with CML underwent COVID-19 vaccination at the centers of family medicine.
On 5 May 2023, the International Health Regulations (2005) Emergency Committee, under the auspices of the WHO, downgraded COVID-19 from a global health emergency, although it continued to refer to it as a pandemic.25 The national health care providers are guided by the standing recommendations for COVID-19 issued by the Director-General of the WHO26 and organize the implementation and monitoring of the practical application of the 10th edition of the National Clinical Protocol "Novel Coronavirus Infection (COVID-19)," dated 2025. COVID-19 diagnostic test for monitored patients with CML is required in the presence of specific infection-related clinical signs and fever. The use of personal protective equipment appropriate to the epidemiological situation and risk level remain mandatory. The monitoring practice has returned to the standard periods between follow-up visits for patients with CML.
Authorship
Contribution: The author conceptualized the study, designed and performed research, collected and analyzed data, and drafted the manuscript.
Conflict-of-interest disclosure: The author declares no competing financial interests.
Correspondence: Vasile Musteata, Department of Hematology, Institute of Oncology, Nicolae Testemitanu State University of Medicine and Pharmacy, Stefan cel Mare si Sfant Blvd 165, MD-2004, Chisinau, Republic of Moldova; email: vasile.musteata@usmf.md.
References
Author notes
Original data are available on request from the corresponding author, Vasile Musteata (vasile.musteata@usmf.md; phdschool@usmf.md).
The original data may be available at https://doctorat.usmf.md/ and www.onco.md.