Abstract
The many comorbidities in the severely ill patient also make thrombocytopenia very common (∼ 40%) in intensive care unit patients. The risk of bleeding is high with severe thrombocytopenia and is enhanced in intensive care patients with mild or moderately low platelet counts when additional factors are present that interfere with normal hemostatic mechanisms (eg, platelet function defects, hyperfibrinolysis, invasive procedures, or catheters). Even if not associated with bleeding, low platelet counts often influence patient management and may prompt physicians to withhold or delay necessary invasive interventions, reduce the intensity of anticoagulation, order prophylactic platelet transfusion, or change anticoagulants due to fear of heparin-induced thrombocytopenia. One approach to identify potential causes of thrombocytopenia that require specific interventions is to consider the dynamics of platelet count changes. The relative decrease in platelet counts within the first 3 to 4 days after major surgery is informative about the magnitude of the trauma or blood loss, whereas the dynamic of the platelet count course thereafter shows whether or not the physiologic compensatory mechanisms are working. A slow and gradual fall in platelet counts developing over 5 to 7 days is more likely to be caused by consumptive coagulopathy or bone marrow failure, whereas any abrupt decrease (within 1–2 days) in platelet counts manifesting after an initial increase in platelet counts approximately 1 to 2 weeks after surgery strongly suggests immunologic causes, including heparin-induced thrombocytopenia, other drug-induced immune thrombocytopenia, and posttransfusion purpura.
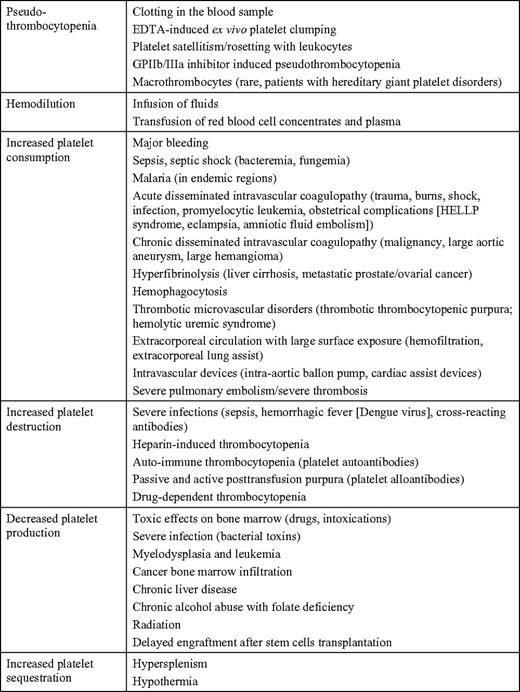
The many comorbidities in the severely ill patient also affect platelet homeostasis, and, consequently, thrombocytopenia is very common in critically ill patients treated in the intensive care unit (ICU). Thrombocytopenia is usually defined as a platelet count of < 150 × 109/L, whereas severe thrombocytopenia is considered as platelet counts < 50 × 109/L. Thrombocytopenia has six major mechanisms, and it can be induced by (1) hemodilution, (2) increased platelet consumption (both are very common in the ICU after tissue trauma, bleeding, and disseminated intravascular coagulopathy [DIC]), (3) increased platelet destruction (ie, immune mechanisms), (4) decreased platelet production, (5) increased platelet sequestration, or (6) by the laboratory artefact of pseudothrombocytopenia (Table 1).
Frequency of Thrombocytopenia in ICU Patients
Various studies found thrombocytopenia in 35% to 45% of ICU patients, with a somewhat greater variability of 5% to 20% for severe thrombocytopenia (Table 2). Surgical ICU patients seem to have a higher incidence of severe thrombocytopenia, compared with medical ICU patients. However, most studies have been performed in mixed surgical/medical ICUs, making definitive conclusions difficult. The prevalence of thrombocytopenia at admission to ICU is around 20% to 30% of patients, and a similar percentage of patients develops thrombocytopenia (from a normal platelet count) while being treated in the ICU.
Thrombocytopenia as a Prognostic Marker
Thrombocytopenia in critically ill patients is often multifactorial (Table 1) and likely a marker of illness severity.1,2 This is supported by the observation that critically ill patients with thrombocytopenia have higher Multiple Organ Dysfunction Scores (MODS), Simplified Acute Physiology Scores (SAPS), and Acute Physiology and Chronic Health Evaluation (APACHE) scores compared with patients admitted with normal platelet counts at the time of ICU admission.3,4 Nearly all studies analyzing thrombocytopenia as a prognostic marker in ICU patients found an inverse correlation of the platelet count with the risks for a prolonged ICU stay and mortality (mortality rate 31%–46% in thrombocytopenic patients vs 16%–20% nonthrombocytopenic patients).3–10 Furthermore, the magnitude of the platelet count decrease correlates more highly with adverse outcomes than the absolute platelet count nadir. Notably, the platelet count pattern over time provides important information about the likely underlying reason(s) for thrombocytopenia (Figure 1a-c). Differentiation of the causes of thrombocytopenia is essential for efficient and appropriate treatment.
Typical platelet count courses in ICU patients show how the dynamic of the platelet count can be used to differentiate between different causes of thrombocytopenia in the critically ill patient. The grey background area shows the platelet count course of 553 patients after cardiopulmonary bypass surgery obtained from a prospective study,13 excluding patients with persistent thrombocytopenia or later onset thrombocytopenia. (a) The normal platelet count patterns observed in patients undergoing major surgical interventions. The platelet count nadir is typically reached by days 3 and 4 for major surgery (inserted graph). A platelet count of 50 to 100 × 109/L during this time period is nearly always related to postoperative consumption and dilution. Different types of surgery show slightly different patterns in regard to the postsurgery platelet count decrease (time and nadir), the time to reach the presurgery platelet count level, and the dynamics of the postsurgery rebound. The different lines exemplify typical platelet count patterns based on summarized data,12,15 but are not real patients. **Data for the orthopedic surgery patients given in the insert of (a) have been kindly provided by Dr T. E. Warkentin, McMaster University, Canada. (b) Early-onset thrombocytopenia in surgical patients (solid line) and medical patients (dot-dash line) are caused by major platelet consumption (eg, sepsis, multiorgan failure or aggravation of the underlying disease). The second solid line indicates a platelet count pattern typical for late-onset complications in a surgical ICU patient. The first decrease in platelet counts is caused by major surgery (compare with (a)). After initial start of platelet counts recovery, late-onset nonimmune complications cause a gradual decrease of platelet counts. (c) Late-onset rapid decrease of platelet counts is typical for immune-mediated thrombocytopenia, which typically occurs in the second week of treatment (after surgical intervention, heparin, and other drugs). Arrows indicate the typical range of platelet count nadirs. Transfusion-related passive alloimmune thrombocytopenia can occur any time, but is closely related to transfusion of plasma-containing blood products.
Typical platelet count courses in ICU patients show how the dynamic of the platelet count can be used to differentiate between different causes of thrombocytopenia in the critically ill patient. The grey background area shows the platelet count course of 553 patients after cardiopulmonary bypass surgery obtained from a prospective study,13 excluding patients with persistent thrombocytopenia or later onset thrombocytopenia. (a) The normal platelet count patterns observed in patients undergoing major surgical interventions. The platelet count nadir is typically reached by days 3 and 4 for major surgery (inserted graph). A platelet count of 50 to 100 × 109/L during this time period is nearly always related to postoperative consumption and dilution. Different types of surgery show slightly different patterns in regard to the postsurgery platelet count decrease (time and nadir), the time to reach the presurgery platelet count level, and the dynamics of the postsurgery rebound. The different lines exemplify typical platelet count patterns based on summarized data,12,15 but are not real patients. **Data for the orthopedic surgery patients given in the insert of (a) have been kindly provided by Dr T. E. Warkentin, McMaster University, Canada. (b) Early-onset thrombocytopenia in surgical patients (solid line) and medical patients (dot-dash line) are caused by major platelet consumption (eg, sepsis, multiorgan failure or aggravation of the underlying disease). The second solid line indicates a platelet count pattern typical for late-onset complications in a surgical ICU patient. The first decrease in platelet counts is caused by major surgery (compare with (a)). After initial start of platelet counts recovery, late-onset nonimmune complications cause a gradual decrease of platelet counts. (c) Late-onset rapid decrease of platelet counts is typical for immune-mediated thrombocytopenia, which typically occurs in the second week of treatment (after surgical intervention, heparin, and other drugs). Arrows indicate the typical range of platelet count nadirs. Transfusion-related passive alloimmune thrombocytopenia can occur any time, but is closely related to transfusion of plasma-containing blood products.
The Dynamics of Platelet Counts in ICU Patients
Although the absolute lowest platelet count is a risk marker for adverse outcomes, assessing only the platelet count nadir during the ICU stay is an oversimplification. The platelet count is very dynamic, reflecting the bone marrow production of about 150 billion platelets daily and their circulating survival time of approximately 10 days under normal conditions.11
Many ICU patients show a significant decrease in platelet counts during their first days in the ICU.5,12 A typical cause for a decrease in platelet counts is major surgery (eg, cardiopulmonary bypass surgery). In a prospective study including 581 ICU patients who underwent cardiac surgery with use of the heart-lung machine,13 platelet counts fell below 150 × 109/L in 56.3% of patients and below 50 × 109/L in 2.9% of patients within 10 days after surgery (unpublished data). The platelet count nadir typically occurs between days 1 to 4 after surgery (Figure 1a). In the vast majority of patients, platelet counts will increase thereafter, reaching the presurgery level at about postoperative days 5 to 7. In the recovering patient, platelet counts then increase further to levels significantly higher (∼ 2–3 times) than the baseline platelet count (Figure 1a) and peaking at about day 14.14 In the postcardiac surgery study, only 5% of patients reached the platelet nadir later than day 4, and only 1.2% of patients developed severe thrombocytopenia with platelet counts < 50 × 109/L after day 4.13 Very similar patterns of platelet count courses were described by Nijsten et al12 in ICU patients after surgery for major trauma, vascular surgery, and abdominal surgery. In the Nijsten study, the magnitude of the platelet count decrease was less pronounced after abdominal surgery, compared with cardiac surgery. Also the nadir (days 1–2) and platelet count recovery (days 3–4) occurred earlier. The largest reactive platelet count increase was observed in trauma patients with values of more than 300 × 109/L reached already on day 7.12 Also Akca et al5 found in 1449 ICU patients an initial decrease in platelet counts, reaching their mean nadir at day 4, followed by an increase above the baseline value. Such a dynamic platelet count course with an initial decrease of platelet counts (nadir days 1–3 after surgery) followed by an overshooting increase in platelet count is also typical for non-ICU patients undergoing major orthopedic surgery (inserted graph in Figure 1a).15 This “rebound” in platelet count to supra-baseline levels indicates an intact physiologic response to platelet consumption. Conditions associated with an acute decrease in platelet numbers lead to an increase in circulating thrombopoietin levels with consequent stimulation of megakaryocytopoiesis.16 The physiology of platelet production by the megakaryocytes explains why it is the normal course of platelet counts to reach a nadir 1 to 4 days after major surgery (Figure 1a). Even after intravenous application of thrombopoietin receptor agonists, the subsequent platelet count increase begins earliest after 3 days,17 indicating that this is the minimum time for megakaryocytes to begin to release increased numbers of platelets following the thrombopoietic stimulus. Prior to this release of new platelets, acute consumption of platelets cannot be compensated by increased platelet production. Thus, the relative decrease in platelet counts within the first 3 to 4 days after major surgery is informative about the magnitude of the trauma or blood loss, whereas the dynamic of the platelet count course shows whether the physiologic compensation mechanisms work.
At least four studies have assessed the dynamic of the platelet count course in ICU patients as a risk factor for adverse outcomes.5,9,12,13 They all found a blunted or absent rise in platelet counts after the initial decrease within the first 4 days strongly associated with mortality and prolonged ICU admission, with either thrombocytopenia present on day 14 or an absence of a relative increase in platelet counts over baseline being a stronger predictor for mortality than the platelet count nadir either at admission or during early ICU stay. The mortality rate in patients with thrombocytopenia at day 4 was 33%, whereas the mortality rate of those with thrombocytopenia at day 14 was 66%.5 Nijsten et al12 calculated the median increase of platelet counts to be approximately 30 × 109/L × day in ICU survivors, compared with 6 × 109/L × day in nonsurvivors (P < .001). Also Selleng et al13 found that the 30-day mortality of postcardiac surgery ICU patients was 1.3% in those with an increase in platelet counts after day 4, compared with 12% in patients with persistent thrombocytopenia < 100 × 109/L after day 4.
There is less information on the dynamics of the platelet count in medical ICU patients. In two studies enrolling 243 medical ICU patients and 198 patients with nosocomial bloodstream infections, respectively, platelet counts dropped below 150 × 109/L in 90% of patients within 5 days, and this occurred within the first 3 days in > 40% of the patients. Thereafter, platelet counts normalized again within 3 to 7 days to values above 150 × 109/L.4,9
Onset and Dynamics of Thrombocytopenia—As a Diagnostic Approach in ICU Patients
Given the high frequency (Table 2) and various causes of thrombocytopenia in the ICU (Table 1), it is important to identify those patients in whom thrombocytopenia requires a specific treatment in addition to treating the underlying disease (eg, heparin-induced thrombocytopenia [HIT] requires alternative anticoagulation and thrombotic thrombocytopenic purpura [TTP] requires plasma exchange). As a general rule, a slow and gradual fall in platelet counts developing over 5 to 7 days is more likely to be caused by consumptive coagulopathy or bone marrow failure, whereas any abrupt decrease in platelet counts manifesting within 1 to 2 days, after an initial increase in platelet counts, and beginning in the second week after surgery, is the domain of immunologic causes and adverse transfusion reactions (posttransfusion purpura or drug-induced immune thrombocytopenia). If the transfusion of blood products is associated with an abrupt platelet count fall within hours, thrombocytopenia can be caused by bacterial contamination or passive alloimmunization. Because patients are often referred from other hospitals or from other wards to the ICU, information about preceding platelet counts is important for interpreting a low platelet count in an ICU patient.
Thrombocytopenia in Patients Admitted to the ICU With a Low Platelet Count (Table 3)
Platelet counts between 50 and 100 × 109/L after major surgery with no overt ongoing bleeding at admission to the ICU are rather “normal” and do only require further monitoring unless there is overt bleeding.
Platelet counts between 50 and 100 × 109/L at admission with gastrointestinal or retroperitoneal hemorrhage, or bleeding due to acute trauma or surgery, are most likely caused by loss or consumption of platelets. Management requires interventions—such as surgery, endoscopic vessel occlusion, interventional radiologic coiling of the bleeding vessel until the bleeding stops—or rapid reversal of any anticoagulant effects. The platelet count should be frequently monitored and maintained above 80 to 100 × 109/L with platelet transfusions18 to avoid consumptive coagulopathy. Because a low hematocrit can enhance the bleeding tendency, the hematocrit should be maintained above 30% in patients with microvascular bleeding.19 In trauma patients, tranexamic acid (loading dose 1 g intravenous bolus followed by infusion of 1 g over 8 hours) reduced mortality and risk of death due to bleeding.20
In medical patients who are not bleeding, the most common reason for an acute, moderately decreased platelet count is severe infection (eg, sepsis and endocarditis). Moderate thrombocytopenia can be caused by sepsis alone, but when the platelets fall below 50,000/μL, DIC is frequently present.21 Chronic moderately decreased platelet counts are more often caused by bone marrow dysplasia (eg, myelodysplastic syndrome and leukemia), toxic drug effects, or chronic liver disease, including chronic alcohol abuse with cirrhosis and hypersplenism. Platelet consumption associated with cardiovascular disease, autoimmune thrombocytopenia (ITP), and thrombotic microangiopathic disorders (see below; TTP, hemolytic uremic syndrome [HUS], and preeclampsia) are less common causes. In endemic areas, malaria is by far the most likely cause of acute thrombocytopenia in a severely ill medical patient. Also, viral infections (eg, infection with the human immunodeficiency virus, hepatitis C virus, or Epstein Barr virus) are often associated with thrombocytopenia.
If moderate thrombocytopenia is associated with an acute thromboembolic complication, severe pulmonary embolism, diabetic ketoacidosis (arterial), catastrophic antiphospholipid syndrome (venous and arterial), and, if the patient received heparin within the last 10 days, HIT (venous and arterial) has to be considered.
An increasingly frequent clinical challenge is the ICU patient with moderate thrombocytopenia who also requires treatment with antiplatelet drugs (eg, aspirin, clopidogrel, and prasugrel) after recent insertion of a coronary stent. The platelet count is still high enough for arterial thrombotic complications, whereas at the same time the bleeding risk is enhanced. No management guidelines exist other than withholding antiplatelet drugs in case of bleeding symptoms and transfusion of platelet concentrates in case of severe bleeding.
Platelet counts <20 × 109/L at admission can be due to bone marrow failure (eg, due to acute leukemia), severe coagulopathy, or immune-mediated platelet consumption. The most important reasons for severe coagulopathy are sepsis (eg, meningococcemia) and, in endemic areas, malaria and hemorrhagic fever. ITP and TTP need to be differentiated because these patients require specific treatment (intravenous immunoglobulin G [IVIG] and corticosteroids for ITP and plasma exchange for TTP).
In patients with clinically relevant bleeding and a platelet count < 20 × 109/L, intervention is often necessary before laboratory results are available to confirm or exclude a diagnosis. In this situation, transfusion of two therapeutic units of platelet concentrates often controls bleeding and is “diagnostic” at the same time. Platelet count determination within 1 hour after the transfusion may offer the fastest way to decide on further management. In cases of bone marrow failure and increased platelet consumption, platelet counts usually increase measurably, whereas they stay low in cases of immune-mediated thrombocytopenia. Transfusion of one therapeutic unit of platelet concentrate may not be informative because these platelets are often directly “consumed” to cover the multiple endothelial lesions that developed during longer lasting thrombocytopenia. This approach is associated with an increased risk for new thrombosis in case of TTP. Therefore, in patients suspected for TTP, a review of the blood smear to exclude fragmented red cells should be performed before platelet transfusion whenever possible.
Thrombocytopenia Developing During ICU Treatment (Table 3)
A gradual decrease in platelet counts over several days is indicative of worsening of the underlying disease and is often associated with multiorgan failure and consumptive coagulopathy due to bacterial or fungal infection (Figure 1b). Pathogenesis and treatment of DIC are reviewed elsewhere.22,23 Another important cause of a slowly decreasing platelet count reaching levels < 50 × 109/L over 1 to 2 weeks are nonimmune effects on the bone marrow with disturbance of the megakaryocytopoiesis (Figure 1b). If this is associated with pancytopenia, the diagnosis is rather obvious. More difficult is the recognition of toxicity (usually drug-related) primarily or selectively affecting the megakaryocytes.
A major decrease in platelet counts after surgery that persists beyond day 4 with platelet counts between 20 to 50 × 109/L (Figure 1b) is most likely caused by severe consumption of platelets due to early sepsis, circulatory shock, and multiorgan failure. A rare, but important, cause is postsurgery TTP.24,25 In these patients, TTP can manifest as early as days 2 and 3 after surgery. However, the diagnosis is often delayed. Postsurgery TTP is presumably triggered by increased release of von Willebrand factor from endothelial cells as a response to major surgery on the background of low levels of the enzyme ADAMTS13 (see below).
A new, rapid decrease in platelet counts that begins after day 4 and after the platelet count has already started to increase again is typical for immune-mediated causes (Figure 1c). If the platelet counts are between 20 and 150 × 109/L in a nonseptic, nonbleeding patient, it is very suspicious for HIT. Other drug-dependent immune thrombocytopenias are very unlikely in case of moderately decreased platelet counts. Despite being relatively rare in ICU patients, with an incidence of about 0.5%, HIT is very frequently considered as a potential cause for thrombocytopenia in ICU patients (see below).10,26,27
A rapid decrease in platelet counts < 20 × 109/L after day 4 in the nonseptic, nonbleeding patient is most often immune-mediated: (i) in cardiac patients who had been treated with a glycoprotein (GP) IIb/IIIa inhibitor within the last 10 days; (ii) drug-dependent thrombocytopenia typically induced by drugs that had been started within the last 10 days (see below); (iii) posttransfusion purpura (PTP; rare)28 ; and (iv) transfusion-induced passive alloimmune thrombocytopenia (rare) (see details below). Another cause that should be considered is transfusion of bacteria-contaminated blood products (platelet concentrate > red blood cell concentrate ≫ plasma).
Causes for Thrombocytopenia in the ICU Patient That Require Special Management
Pseudothrombocytopenia (common, platelet count variable) due to clots in the tube or caused by platelet aggregates in ethylenediaminetetraacetic acid (EDTA)-anticoagulated blood should be excluded. This can be done by checking for platelet aggregates in the platelet histogram and reviewing the blood smear. This is especially important in patients treated with GPIIb/IIIa inhibitors, which induce pseudothrombocytopenia almost as frequently as true thrombocytopenia. GPIIb/IIIa inhibitor-induced pseudothrombocytopenia can also be present in citrated blood and the exclusion of platelet clumps by microscopic blood smear assessment is essential.
Posttransfusion purpura (rare, platelet count < 10 × 109/L)29 should be considered if the patient received blood transfusions within the previous two weeks. PTP is most often caused by platelet alloantibodies against the human platelet antigen (HPA)-1a. Typically, females are affected who were immunized against this platelet alloantigen during a previous pregnancy. The recent blood transfusion (red blood cell concentrates or platelets) then triggers a response from memory B cells and antibody levels are boosted. By a not well-understood mechanism, the boosted alloantibodies also destroy autologous (antigen-negative) platelets. Treatment is symptomatic with IVIG 1 g/kg body weight for two consecutive days.
Passive alloimmune thrombocytopenia (platelet count < 20 × 109/L)30 is caused by transmission of platelet anti-HPA-1a alloantibodies through a transfusion of plasma or red blood cells immediately before severe thrombocytopenia occurs. The transfused antiplatelet antibodies bind to the patient′s platelets that are then removed by the reticuloendothelial system.
GPIIb/IIIa inhibitor-induced thrombocytopenia31,32 has been reported in 0.3% to 1.6% of patients treated with abciximab, 0.2% to 0.4% of those treated with tirofiban, and 0% to 0.2% of patients receiving eptifibatide. Thrombocytopenia typically manifests within the first 24 hours of treatment, which indicates that these patients have already circulating (naturally acquired) antibodies in their plasma. The risk for thrombocytopenia is higher during second exposure. Also, severe thrombocytopenia (< 20 × 109/L) is more frequent after reexposure. Usually, platelet counts decrease to values < 50 × 109/L and often < 20 × 109/L. Patients have an increased risk for bleeding, and stopping the offending agent is recommended. Platelet counts normalize after cessation of the GPIIb/IIIa inhibitor within 2 to 3 days, but unusually prolonged thrombocytopenia can occur when these antibodies also affect megakaryocytes.33 It is important to exclude pseudothrombocytopenia in these cases, as withholding of antiplatelet drugs may cause severe complications in acute coronary syndrome. In case of significant bleeding, platelet counts are responsive to platelet transfusion. In case of the reversibly binding inhibitors tirofiban- or eptifibatide-induced thrombocytopenia, platelet transfusions are of little effect, whereas the drug is still circulating (t1/2 = 2 hours for both drugs).
TTP/HUS is characterized by the presentation of severe thrombocytopenia and microangiopathy.
In TTP, ultra large von Willebrand factor multimers induce platelet aggregates in the microcirculation. The classic pentad presentation of fever, neurological symptoms, thrombocytopenia, Coombs negative microangiopathic hemolysis, and renal insufficiency is infrequent. Beside thrombocytopenia, laboratory abnormalities include an increase in lactate dehydrogenase, absent to very low levels of haptoglobin, fragmented red blood cells, and reticulocytosis. TTP is often caused by low ADAMTS13 (inherited or acquired due to autoantibodies).34 In a small subset of TTP patients, these antibodies are triggered by drugs. Ticlopidine, clopidogrel (rare), mitomycin C, quinine, cyclosporine, and some chemotherapeutic drugs have been described to induce TTP. In these patients, cessation of the drug is imperative. In HUS, renal failure is the leading symptom. Current management includes plasma exchange as the essential treatment for most adults.35 Patients with autoimmune ADAMTS13 deficiency may also require immunosuppressive treatment. Recurrent acute episodes occur in approximately 40% of patients with acquired ADAMTS13 deficiency, frequently within the first year.
HIT is very frequently considered as a potential cause for thrombocytopenia in ICU patients, although it is relatively rare with an incidence of about 0.3% to 0.5% (ie, the explanation for only about 1 in 100 thrombocytopenic patients in the ICU).10,26,36 In HIT, antibodies of the immunoglobulin G class against platelet factor 4 (PF4)/heparin complexes induce intravascular platelet activation and consequent thrombin generation, resulting in an enhanced risk for venous and/or arterial thrombosis.37 HIT usually features a platelet count fall > 50% (from the highest value after day 4 of heparin treatment), most often to a nadir between 20 to 100 × 109/L and can present with new thrombosis, typically occurring 5 to 14 days after start of prophylactic or therapeutic doses of heparin.37 Timing of onset, the moderate nature of thrombocytopenia, and the common concurrence of thrombosis, are very important factors to differentiate HIT from other explanations for thrombocytopenia in the ICU patient. Patients with early-onset thrombocytopenia or a platelet count < 20 × 109/L usually do not have HIT. Thromboembolic complications predominantly affect the venous system. Other rare complications include skin necrosis, adrenal hemorrhagic necrosis (most often seen in ICU HIT patients and caused by adrenal vein thrombosis), or postintravenous heparin bolus anaphylactoid reactions. A platelet count fall within the first hours after the start of heparin (= rapid onset HIT) can be observed in preimmunized patients who had received heparin usually within the past 30 days.
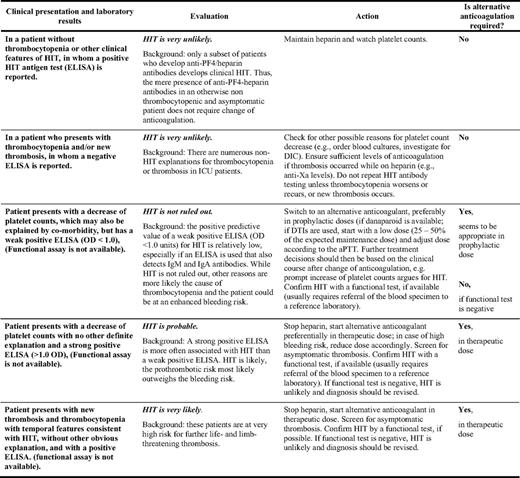
Diagnosis of HIT is especially problematic in critically ill patients, because the two leading symptoms of HIT (thrombocytopenia and thrombosis) are not specific for HIT.10,13 The absence of antibodies against PF4/heparin complexes can rule out HIT (high negative predictive value) (Table 4), but the presence of anti-PF4/heparin antibodies alone cannot confirm a diagnosis. PF4/heparin antibodies are much more frequent than clinical HIT, and HIT is frequently overdiagnosed in the ICU, especially if the diagnosis is based only on a positive antigen test result (PF4/heparin enzyme-linked immunosorbent assay [ELISA] and particle gel immunoassay).36 In case of high clinical suspicion for HIT, stopping heparin alone is insufficient. To prevent new thrombosis, nonheparin anticoagulant therapy is required (Table 4). Three drugs are approved for anticoagulation in HIT: (1) two direct thrombin inhibitors (DTIs), lepirudin and argatroban; and (2) a heparinoid, danaparoid. Also, the DTI bivalirudin and the antifactor Xa inhibitor fondaparinux are rational therapies for HIT. All alternative anticoagulants confer significant risks for major bleeding (0.8%–1.25% per treatment day), if given in therapeutic dose, and no antidote is available for any of them. Therefore, in patients with low/moderate clinical probability for HIT, our practice to reduce the risk of bleeding is to use prophylactic dose alternative anticoagulation, while awaiting the results of laboratory testing (Table 4). Vitamin K antagonists (VKAs) must not be given in acute HIT. They can induce venous limb gangrene in the extreme hypercoagulable milieu of HIT because of VKA-induced protein C depletion.
Bleeding Risk and Platelet Transfusion in the Thrombocytopenic ICU Patient
Thrombocytopenia usually increases the risk for bleeding complications (Table 3). In one study, 4.1% of patients without thrombocytopenia, compared with 52.6% of patients with nadir platelet counts < 100 × 109/L), had bleeding.3 However, the bleeding risk is not restricted to very low platelet counts and is also enhanced in patients with platelet counts between 50 to 100 × 109/L. This strongly indicates that additional factors contribute to the risk of bleeding, such as DIC, platelet function defects, hyperfibrinolysis, and invasive interventions. In the authors' view, bleeding in ICU patients with platelet counts > 30 × 109/L is more likely an indicator for disturbed hemostasis, whereas thrombocytopenia is not the only or the primary cause. The risk for bleeding in the thrombocytopenic patient is also dependent on the hematocrit, and a low hematocrit increases the bleeding time.19 In a patient with microvascular hemorrhage, transfusion of red blood cells to increase the hematocrit (30%–35%) might be an additional therapeutic option.
Even low platelet counts, which are not associated with bleeding, often influence management and treatment decisions. They often prompt physicians to withhold or delay necessary invasive interventions (eg, surgery), can lead to a reduction in the intensity of anticoagulation, and may also lead to prophylactic platelet transfusion for correction of platelet count numbers. Platelet transfusion triggers in the ICU patient are not very well studied, and the potential adverse effects of platelet transfusions are largely unknown. Retrospective studies indicate that liberal platelet transfusion in the ICU may increase risk for infection, prolonged ICU stay, and even mortality.38 Although there are no data showing a benefit from prophylactic platelet transfusion in the nonbleeding ICU patient, those experiencing active bleeding and or require interventions do require platelet transfusions. Evidence is weak regarding the “safe” cutoff values in ICU patients with thrombocytopenia and when platelet transfusions are indicated. Published consensus guidelines are largely based on expert experience and observational data. The factors that should be considered in deciding whether platelet transfusion is likely beneficial include the absolute platelet count, platelet function, the type of procedure with respect to the risk of bleeding and the site of bleeding, active or history of bleeding, and liver and renal function. In general, platelet transfusion is recommended in the following scenarios18 :
the patient is actively bleeding and has platelet dysfunction (primary or secondary; eg, to antiplatelet drugs), regardless of the platelet count;
the patient requires neurosurgery or invasive procedure with a high risk of bleeding into a critical site (eg, epidural or spinal puncture) with a platelet count of < 100 × 109/L;
the patient requires urgent major surgery or an invasive procedure with a high risk of bleeding (eg, soft-tissue biopsy) with a platelet count of < 50 × 109/L;
the patient requires minor surgery or a low-risk procedure (eg, bronchoscopy and endoscopy) with a platelet count of less than 20 × 109/L;
in patients with hematologic disorders (eg, acute leukemia) following chemotherapy/bone marrow transplantation or bone marrow failure/aplasia when the platelet count is less than 10 × 109/L.
Disclosures
Conflict-of-interest disclosure: A.G. is a consultant for IL Laboratories, Mitsubishi Pharma, and Schering-Plough. K.S. declares no competing financial interests.
Off-label drug use: Use of nonheparin anticoagulants in ICU patients with heparin-induced thrombocytopenia: fondaparinux and bivalirudin.
Correspondence
Professor Dr. Andreas Greinacher, Institut für Immunologie und Transfusionsmedizin, Ernst-Moritz-Arndt-Universität Greifswald, Sauerbruchstrasse, D-17489 Greifswald, Germany; Phone: +49 3834 865482; Fax: +49 3834 865489; e-mail: greinach@uni-greifswald.de