Abstract
Less than 5% of patients with a plasma cell dyscrasia present with a single bone (SBP) or extramedullary plasmacytoma (EMP) without evidence of systemic disease (normocalcemia, absence of anemia, preservation of uninvolved immunoglobulins, or renal disease attributable to myeloma). Diagnosis requires biopsy confirmation of a monoclonal plasma cell infiltrate from a single site. The treatment of choice for both entities is radiotherapy given with curative intent (> 4000 cGy) resulting in long term disease-free survival in approximately 30% of patients with SBP and 65% of patients with EMP.
Less than 5% of patients with a plasma cell dyscrasia present with a single bone or extramedullary lesion due to a malignant plasma cell infiltrate, without apparent evidence of systemic myeloma. Most present with a painful lesion, but some patients who are asymptomatic may be diagnosed during radiologic examination for other conditions.
Solitary Plasmacytoma of Bone
Diagnosis
Diagnosis requires a biopsy-proven monoclonal plasma cell infiltration of a single lytic bone lesion; no additional lesions on bone survey; absence of clonal plasma cells on a random marrow sample; and no evidence of systemic myeloma (normocalcemia, absence of anemia or renal disease attributable to myeloma). The role of magnetic resonance imaging (MRI) of the thoracic and lumbosacral spine in the diagnosis of solitary plasmacytoma of bone (SBP) was prospectively evaluated by Moulopoulos et al in 12 consecutive patients with SBP. MRI detected additional abnormalities in 4 patients who, after radiotherapy for the solitary lesion (of curative intent), had persistent paraprotein (> 50% of the pretreatment value), compared with only 1 of 6 similarly treated patients without an abnormality by pretreatment spinal MRI.1 In a follow-up report of 23 patients with thoraco-lumbar spine disease from our center, 7 of 8 patients who had SBP by radiographs alone developed myeloma, compared with only 1 of 7 patients with only 1 lesion confirmed by MRI.2 Thus, most investigators agree that a negative MRI of the thoraco-lumbar spine is a prerequisite for the diagnosis of SBP.
The presence of monoclonal protein (M protein) in the serum or urine has been noted in 24%–72% of patients in various series.3–5 In our experience, among 63 consecutive previously untreated patients with SBP, 62% had a serum M protein, 13% had only Bence Jones protein (BJP), and 25% had non-secretory disease.6 Paraprotein values were usually very low, with only 11 of 37 patients with a serum M protein > l g/dL (high value 2.2 g/dL) and the highest urine BJP was 0.7 g/day. Recently, free light chain assays have provided a measurable parameter to follow in approximately 65% of patients previously diagnosed with “non-secretory” multiple myeloma by standard electrophoretic studies.7 It is likely that these assays will also be useful in a similar percentage of patients with SBP. Like MRI, this would improve the precision of monitoring SBP and provide more sensitive identification of patients who achieve complete disappearance of paraprotein after radiation therapy and are most likely to be cured. Levels of uninvolved immunoglobulins are usually preserved, and in our series of 63 patients, only 3 had suppressed levels. These 3 patients had disease progression at 12, 18 and 74 months, indicating, in our opinion, the presence of systemic disease.6
Treatment
Radiotherapy with curative intent is the treatment of choice, resulting in local control in > 80% of patients and prolonged cause-specific disease-free survival in approximately 35% of patients with SBP. Strict dosing guidelines are difficult to recommend due to the limited number of patients and the absence of prospective phase I-II and randomized studies. Despite this, some recommendations are reasonable based on multiple single institution studies (Table 1 ). Tsang et al report no dose-response above 35 Gy in 32 patients; however, a retrospective review by Mendenhall et al noted that among 81 patients treated with ≥ 40 Gy of radiation, there was only 6% local progression of disease, which was superior to 31% for those who received < 40 Gy.8,9 Similarly, Frassica et al saw no local failure for doses > 50 Gy.10 While no dose-response was noted by Tsang et al, size of the tumor appeared predictive for local recurrence. That report indicated that SBP < 5 cm was 100% controlled for local recurrence, while nearly 40% of patients with bulky disease (≥ 5 cm) had local progression or recurrence of disease.8
Thus, in the absence of a large cooperative group study, our practice has been to recommend 45 Gy in 25 fractions over 5 weeks. Recently, evidence-based guidelines of the United Kingdom Myeloma Forum (UKMF) recommend radiotherapy of at least 40 Gy in 20 fractions and ports that encompass the tumor volume plus a margin of at least 2 cm beyond disease detectable by MRI.5 For bulkier disease (> 5 cm), a higher dose (up to 50 Gy in 25 fractions) was recommended.
Surgical resection of SBP is rarely necessary, but occasional patients may require decompressive laminectomy in the presence of cord compression. When possible, an anterior approach is preferred and radiotherapy is generally delayed, but ports may be somewhat compromised due to hardware.11
Adjuvant chemotherapy has been administered with inconclusive results. Although some studies have found that adjuvant therapy may prevent or delay progression to myeloma, most have noted no benefit with the early administration of chemotherapy.3–5 More recently, even myeloablative therapy with stem cell support has been evaluated in high-risk patients with solitary bone plasmacytoma, but results are too premature to draw any conclusions given the long natural history of this disease.12 It is unclear whether the risk of early therapy for SBP may predispose to development of either resistant plasma cell clones or to secondary leukemia. Thus, given the lack of consistent data proving benefit from chemotherapy, we and others believe that there is no current role for adjuvant chemotherapy in the initial treatment of SBP.
Natural history and prognosis
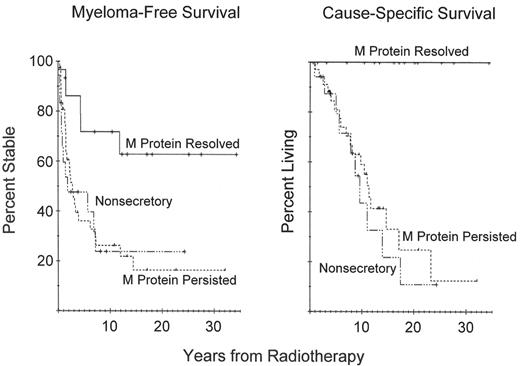
While the majority of patients with solitary plasmacytoma of bone develop myeloma after a median of 2–3 years, the overall median survival of 7–12 years is longer than for patients in early phases of symptomatic myeloma. Approximately 15%–45% of patients remain disease free at 10 years, and although the majority of these appear to be cured, rare late recurrences have been reported. In our experience, prolonged stability ensued only in patients with complete disappearance of paraprotein by one year, indicating the absence of occult disease outside the radiotherapy port, in contrast to patients with either persistence of paraprotein (after one year) or non-secretory disease in whom myeloma usually evolved (Figure 1 ).6 Others have reported that neurologic problems associated with SBP, spinal disease, soft tissue masses, bulky disease (≥ 5 cm), age > 55 years, radio-therapy dose, and M protein level were important prognostic factors.2–6,8,10,13–16 In our series of 63 patients we were unable to confirm any of these factors, although no patient with a serum M protein ≥ l.0 g/dL had complete disappearance of paraprotein.
As further advances in diagnostic testing are evaluated (PET scans, free light chains) occult disease should be more easily recognizable. Consequently, SBP will be diagnosed less, complete disappearance of paraprotein should occur more frequently and the fraction of cured patients should rise.
Extramedullary Plasmacytoma
Diagnosis
Solitary extramedullary plasmacytoma (EMP) is less common than SBP and occurs when there is soft tissue infiltration of clonal plasma cells. There should be no evidence of bone destruction or occult disease elsewhere. EMP must be distinguished from reactive plasmacytoma, plasma cell granuloma and lymphoma (MALT, marginal zone, and immunoblastic).3,5 This is probably best accomplished by phenotypic studies positive for CD38 and monoclonal cytoplasmic light chain expression of malignant plasma cells obtained by biopsy or fine needle aspiration of the solitary lesion. Similar to SBP, there should be no evidence of clonal marrow plasmacytosis. Approximately 85% of lesions occur in the head and neck mucosa, and underlying bone involvement, particularly in the sinuses, may be noted. Gastrointestinal involvement, although significantly less common, is the next most frequent site and other areas of involvement reported infrequently include lung, bladder, thyroid, testis, ovary, and tonsil among others.3,6,17
There are limited data regarding the diagnosis and staging of this disorder, and while CT or MRI is required to document the extent of the solitary lesion, no prospective data exist regarding the role of spinal MRI in staging this entity, but similar to SBP, we find it useful for the accurate staging of EMP.
Less than one-quarter of patients have evidence of a low level of monoclonal protein in serum or urine by electrophoresis and/or immunofixation, and (similar to our experience with SBP) we require normal levels of uninvolved immunoglobulins to confirm the absence of occult disease elsewhere.17 Although current experience is minimal, free-light chain assays should also prove useful in monitoring such patients, particularly those classified with non-secretory features. In addition, patients should have no sign of underlying myeloma by bone survey and chemistries should reveal no abnormalities attributable to plasma cell dyscrasia.
Treatment
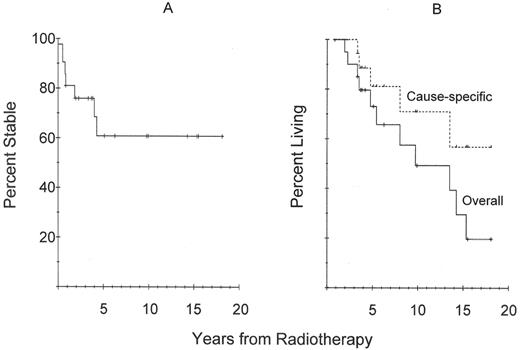
Like SBP, EMP are highly radiosensitive with nearly all patients successfully achieving local control (80%–100%) and approximately the 50%–65% of patients remaining free of disease longer than 10 years (Table 1 , Figure 2 ).8,16–19 Due to small patient numbers and historical retrospective analyses over many decades, no firmly established criteria for treatment exist. Similar to SBP, Tsang et al reported successful local control for nearly all patients (13 of 14) treated with 35 Gy with only 1 failure in a patient with disease > 5 cm; others also confirmed less satisfactory control in sites with bulky disease.8 Median doses of radiation in most studies ranged from 35 to 45 Gy and in our own experience, there appears to be little value for doses beyond 50 Gy (myeloma developed in 1 of 5 patients who received 40–49 Gy versus 4 of 15 patients treated with 50–60 Gy).17 The utility of prophylactic irradiation of local lymph nodes is unclear as there have been excellent results with elective inclusion (but with increased morbidity), as well as similar results with inclusion of draining lymph nodes only when clinically involved (or for Waldeyer’s ring involvement, which is considered at high risk for local recurrence).8,15,18,20 In our own practice we reported 100% local regional control in 5 of 7 patients with tumors in the oral cavity, oral/nasopharynx, larynx, or parotid treated with elective nodal radiotherapy.17 Because of these excellent results, we currently recommend elective radiation of nodal areas, but not for maxillary sinus or nasal cavity involvement. Current evidence-based recommendations by the United Kingdom Myeloma forum are otherwise similar to our own recommendations and those for SBP.5 Their recommendations include a radiotherapy dose of 40 Gy in 20 fractions for tumors < 5 cm and up to 50 Gy in 25 fractions for tumors ≥ 5 cm with at least a 2 cm margin encompassing the primary tumor. If cervical nodes are involved (or in Waldeyer’s ring tumors), these should be included in the radiotherapy field.
Because EMP is a highly radiosensitive tumor, surgical procedures of the head and neck are not recommended, but surgery may be considered for other sites of disease, such as the gastrointestinal tract. This approach is supported by a literature review by Alexiou et al, in which patients with sites other than the head and neck received either surgery, radiation, or a combined-modality treatment.21 There was no difference between the 3 arms, suggesting that either surgery or radiotherapy is reasonable for such patients.
Considering the high cure rate of EMP with radio-therapy and the lack of published data regarding the use of adjuvant chemotherapy, use of adjuvant chemotherapy is not justified outside a clinical trial.
Natural history and prognosis
In most series, < 10% of patients have local recurrence of disease and the 10-year disease free and overall survival ranges from 50–80%, for the 30%–50% of patients who develop disease progression to myeloma. This occurs after a median of 1.5–2.5 years and their clinical course at progression is similar to those of patients diagnosed with de novo symptomatic myeloma. Because of the small number of patients in most series, any statistically significant risk factors for development of myeloma are not clear and are further complicated by the inclusion of patients over many decades during which treatment and diagnostic modalities have become more refined and are likely to impact prognosis. In some series, bulky disease > 5 cm may have prognostic significance.8 In contrast to SBP, because < 25% of patients have a monoclonal protein, any statistically significant analysis of disappearance of paraprotein is precluded for patients with EMP.
Conclusions and Future Directions
SBP and EMP are highly radiosensitive, and appropriate therapy results in long-term stability and potential cure in approximately 50% and 67% of patients, respectively. Spinal MRI and evaluation of uninvolved immunoglobulins have successfully identified occult disease, further refining the diagnosis, which should be reflected in future survival data. New modalities for diagnosis and for monitoring of disease status (PET, free light chain assays, etc.) should help further refine the diagnosis and identify high-risk groups for disease progression. Since prognostic factor analyses have been limited by small patient numbers and retrospective inclusion of patients over many decades, a large cooperative group study to prospectively identify patients who may benefit from novel treatment modalities and adjuvant therapy could help further define treatment and perhaps improve survival for high-risk patients.
Outcome after treatment for solitary plasmacytoma (selected studies).
| Series . | No. of Patients . | Radiotherapy Dose (Gy) . | 10-Year DFS (%) . | OS (Yrs) . | 10-Year OS (%) . |
|---|---|---|---|---|---|
| Abbreviations: DFS, disease-free survival; OS, overall survival. | |||||
| Solitary bone plasmacytoma (SBP) | |||||
| Wilder6 | 60 | 30–70 | 38 | 11 | – |
| Frassica10 | 46 | < 12–70 | 25 | 9.3 | – |
| Tsang8 | 32 | < 30–50 | 36 | 10 | – |
| Bolek15 | 27 | 28.3–60 | 46 | 10 | – |
| Extramedullary plasmacytoma (EMP) | |||||
| Galieni22 | 46 | 40–75 | 78 | – | 80 |
| Liebross17 | 22 | 40–60 | 56 | – | 50 |
| Brinch23 | 18 | 28–60 | 80 | – | 76 |
| Chao16 | 16 | 40–50.4 | 75 | – | 54 |
| Tsang8 | 14 | < 30–50 | 84 | – | 65 |
| Holland14 | 14 | 16.11–62 | 64 | – | NA |
| Series . | No. of Patients . | Radiotherapy Dose (Gy) . | 10-Year DFS (%) . | OS (Yrs) . | 10-Year OS (%) . |
|---|---|---|---|---|---|
| Abbreviations: DFS, disease-free survival; OS, overall survival. | |||||
| Solitary bone plasmacytoma (SBP) | |||||
| Wilder6 | 60 | 30–70 | 38 | 11 | – |
| Frassica10 | 46 | < 12–70 | 25 | 9.3 | – |
| Tsang8 | 32 | < 30–50 | 36 | 10 | – |
| Bolek15 | 27 | 28.3–60 | 46 | 10 | – |
| Extramedullary plasmacytoma (EMP) | |||||
| Galieni22 | 46 | 40–75 | 78 | – | 80 |
| Liebross17 | 22 | 40–60 | 56 | – | 50 |
| Brinch23 | 18 | 28–60 | 80 | – | 76 |
| Chao16 | 16 | 40–50.4 | 75 | – | 54 |
| Tsang8 | 14 | < 30–50 | 84 | – | 65 |
| Holland14 | 14 | 16.11–62 | 64 | – | NA |
Myeloma-free survival (A) and cause-specific survival (B), both in terms of response of myeloma. (M) protein in the blood and/or urine to radiotherapy, for solitary bone plasmacytoma patients.
Myeloma-free survival (A) and cause-specific survival (B), both in terms of response of myeloma. (M) protein in the blood and/or urine to radiotherapy, for solitary bone plasmacytoma patients.
Multiple myeloma-free survival for patients with extramedullary plasmacytoma (EMP) (A) and overall and cause specific survival for all patients (B).
Multiple myeloma-free survival for patients with extramedullary plasmacytoma (EMP) (A) and overall and cause specific survival for all patients (B).
Acknowledgment: Special thanks to Raymond Alexanian, MD, and Meletias Dimopoulos, MD, for their mentorship and collaboration.