Abstract
Telomeres, repeat sequences at the ends of chromosomes, are protective chromosomal structures highly conserved from primitive organisms to humans. Telomeres inevitably shorten with every cell cycle, and telomere attrition has been hypothesized to be fundamental to normal senescence of cells, tissues, and organisms. Molecular mechanisms have evolved to maintain their length and protective function; telomerase (TERT) is a reverse transcriptase enzyme that uses an RNA molecule (TERC) as the template to elongate the 3′ ends of telomeres. Shelterin is a collection of DNA-binding proteins that cover and protect telomeres. The recent discovery of inherited mutations in genes that function to repair telomeres as etiologic in a range of human diseases, which have clinical manifestations in diverse tissues, including the hematopoietic tissue, suggests that defects in telomere repair and protection can cause organ failure. Dyskeratosis congenita is the prototype of telomere diseases; it is characterized by bone marrow failure, mucocutaneous abnormalities, pulmonary fibrosis, liver cirrhosis, and increased susceptibility to cancer, including acute myeloid leukemia. Aplastic anemia, acute myeloid leukemia, and idiopathic pulmonary fibrosis also are associated with inherited mutations in telomere repair or protection genes. Additionally, telomere defects associate with predisposition to hematologic malignancy and epithelial tumors. Telomere erosion is abnormally rapid in patients with mutations in telomerase genes but also after hematopoietic stem cell transplant, and telomeres are naturally shorter in older individuals—all conditions associated with higher rates of malignant diseases. In human tissue culture, short telomeres produce end-to-end chromosome fusion, nonreciprocal translocations, and aneuploidy.
Telomeres were first measured to be short in approximately one third of patients with acquired aplastic anemia more than a decade ago; those with the shortest telomeres appeared to have longer disease duration and to be more likely to develop late malignant clonal complications.1,2 Granulocytes were subsequently found to be mainly affected by telomere erosion in acquired marrow failure and that patients with short telomeres were mainly those who did not respond to immunosuppression.2 Telomere shortening also is common in congenital aplastic anemias; dyskeratosis congenita is the prototypical telomere disease in which telomeres are most severely eroded,3 but patients with Fanconi anemia and Shwachman-Diamond syndrome also have some degree of telomere attrition mainly in granulocytes.4,5
At first, telomere shortening was thought to be the result of a “stressed” hematopoietic stem cell, which over-proliferates in response to marrow destruction. However, the findings that X-linked dyskeratosis congenita was caused by mutations in a gene called DKC1,6 and that this gene product, dyskerin, physically associated with the telomerase complex7 provided a crucial connection between marrow failure and telomere shortening. Subsequently, mutations in similar genes related to telomere maintenance were described in autosomally inherited forms of dyskeratosis congenita. Mutations in the telomerase complex genes or in the telomere-protecting complex (shelterin) cause telomere erosion and disease. However, gene penetrance, the onset of symptoms and signs early or late in life, disease anticipation, the ultimate severity of clinical manifestations, and the organs affected must be influenced by incompletely defined added environmental, epigenetic, or genetic modifiers.
Telomere Biology
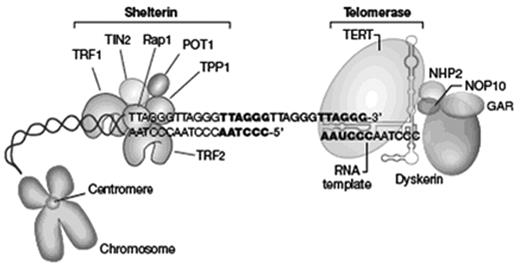
In humans, telomeres are hexameric repetitive DNA sequences (TTAGGG in the leading strand and CCCTAA in the lagging strand)8 capped by specific proteins at the extremities of linear chromosomes (Figure 1 ).9 The leading strand (G-rich) ends in a single-stranded 3′ overhang, which is generated by processing of the lagging (C-rich) strand. The single-stranded 3′ overhang folds back into the telomeric DNA, invades the double-helix, and anneals with the C-rich strand, forming a loop known as T-loop, thus hiding the very ends of chromosomal DNA. Telomeres are coated by a group of at least six proteins, collectively called shelterin.9 Three proteins, TRF1, TRF2, and POT1, directly recognize and bind to TTAGGG repeats (POT1 binds to single-stranded repeats), whereas the other shelterin proteins, TIN2, TPP1, and Rap1, interconnect the telomere-binding proteins to form the entire complex. Shelterin serves as a signal that allows the cellular DNA-repair machinery to distinguish telomeres from DNA double-stranded breaks. Telomeres also bind to nucleosomes, which are rich in modified histones. Major histone modifications found in telomeres are H3K9 and H4K20 trimethylation and low abundance of acetylated H3 and H4.10
Telomeres cannot be fully duplicated during cell division, and this insufficiency—the “end-replication problem”—causes telomere shortening after every cell division. This problem is caused by the DNA polymerase’s characteristic of requiring an RNA (or DNA) primer to initiate duplication.11 When the RNA primer binds to the very last nucleotides (ending in 3′-OH) of the leading strand, polymerase binds to the heteroduplex DNA-RNA double strand and starts polymerization, moving along the DNA strand; as DNA polymerase moves away, the RNA primer dissociates, leaving a gap (a non-duplicated DNA strand) behind; the newly synthesized strand is therefore shorter than the template strand correspondent to the size of the RNA primer. Telomeres are additionally shortened by post-replicative DNA processing or by direct damage caused by, for instance, reactive oxygen species.
When critically short, telomeres signal cell proliferation arrest, senescence, and apoptosis via p53, p21, and PMS2.10 However, if the cell bypasses these inhibitory pathways and continues to proliferate, extremely short telomeres lose their function of chromosomal protection, promoting chromosomal instability.
Telomerase
To counter telomere shortening, highly proliferative cells, such as stem cells (including hematopoietic stem cells) and lymphocytes, express the enzyme telomerase.12 Telomerase is a specialized reverse transcriptase that uses a specific RNA molecule, TERC (telomerase RNA component), as the template to extend the 3′ end of the leading strand by adding TTAGGG repeats (Figure 1 ). The telomerase complex is composed of TERT (the reverse transcriptase enzyme), TERC (the RNA component), and the ribonucleoprotein dyskerin (encoded by the DKC1 gene), which is important for the RNA component folding and stability. NOP10, NHP2, and GAR are other proteins that associate with the telomerase complex; these proteins are important for TERC molecule stabilization and also play a role in ribosome biogenesis and messenger RNA processing.
Most mature cells, however, do not express telomerase and cannot elongate their telomeres. In stem and progenitor cells, telomerase expression is tightly regulated and these cells contain very low levels of telomerase.12 Additionally, c-Myc and estrogen stimulate telomerase expression, and Rb and p21 suppress it. As a result of this low level of telomerase expression even in adult stem and progenitor cells, telomeres eventually shorten with age. In peripheral blood leukocytes, telomeres are long at birth but display rapid erosion in the first two decades of life, continuing to shorten with age at a slower rate. Telomeres also are relatively shorter in lymphocytes in comparison to granulocytes.
Telomere Shortening and Human Disease
Dyskeratosis Congenita
Dyskeratosis congenita is a constitutional aplastic anemia predominantly manifested in the first two decades of life, characterized by bone marrow failure, a triad of mucocutaneous abnormalities (nail dystrophy, leukoplakia, and skin hyperpigmentation), and increased susceptibility to cancer. The most common cancers are head and neck squamous cell carcinomas, skin and anorectal cancer, and acute myeloid leukemia.13 The risk for tongue cancer shows more than 1000-fold increase, and the risk for acute myeloid leukemia is increased almost 200 times. Dyskeratosis congenita patients also are at risk to develop myelodysplasia.
Dyskeratosis congenita is the prototypical disease caused by excessive telomere shortening.14 Mutations in DKC1, which encodes the telomerase component dyskerin, are etiologic in X-linked dyskeratosis congenita. Autosomal forms of dyskeratosis congenita (recessive or dominant) are due to mutations in TERT,15,TERC,16,NHP2,17,NOP1018 (the last two are proteins that associate with the telomerase complex and their mutations are found in autosomal recessive cases only), or TINF2.19 These mutations dramatically reduce the function of the telomerase complex to extend telomeres or, in the case of TINF2, lead to inappropriate capping of telomeres. As telomerase is usually expressed at very low levels in healthy stem cells, heterozygous mutations in either TERT or TERC suffice for telomerase deficiency by haploinsufficiency. All these mutations ultimately result in excessive telomere attrition and replicative senescence of the hematopoietic stem cells, which is clinically translated into marrow failure. In most patients with dyskeratosis congenita, telomeres of both granulocytes and lymphocytes are extremely short (usually varying from 3 to 5 kb long, as opposed to an expected average length of 7 to 8 kb in a 20-year-old healthy subject).12 Since a handful of genes potentially mutate in dyskeratosis congenita and since some of these genes are relatively large, genetic sequencing may be cumbersome and expensive. Additionally, the mutated gene is yet to be identified in a proportion of dyskeratosis congenita patients.
Telomere length measurement, especially in lymphocytes, however, appears to be a good screening test to confirm the diagnosis of dyskeratosis congenita and to identify clinically healthy mutation carriers in families.20 Telomere length measurement has important clinical implications in the selection of related donors for hematopoietic stem cell transplant. Several techniques measure telomeres: Southern blot, quantitative PCR (qPCR), and flow-FISH (a combination of flow cytometry and fluorescence in situ hybridization). However, the method that seems more accurate and reliable from the clinical perspective seems to be flow-FISH, in which telomere lengths in different cell types (granulocytes, lymphocytes) can be distinguished.20 ;21
Aplastic Anemia
Most cases of acquired aplastic anemia are the consequence of an immune-mediated destruction of hematopoiesis, and a minority of patients with aplastic anemia has heterozygous mutations in genes encoding the telomerase components TERT or TERC (5%–10% of cases); mutations in shelterin components are very rarely found in patients with aplastic anemia22 and are predominantly found in pediatric cases.23 These patients lack the classical clinical features of dyskeratosis congenita (mucocutaneous anomalies, lung fibrosis, esophageal stricture, short stature, etc), but a proportion of them have a familial history that can suggest the possibility of a telomerase mutation. The clinical history may vary from a relative with some signs of marrow deficiency (isolated thrombocytopenia, anemia unresponsive to B12 or iron therapy), myelodysplasia, aplastic anemia, or acute myeloid leukemia. Other patients may have a family history of severe liver disease or lung fibrosis, and the clinician should be attentive to this.24 Again, in the setting of aplastic anemia, telomere length measurement may be useful to identify suitable sibling donors for stem cell transplant.
Most patients with aplastic anemia with telomerase mutations do not respond adequately to immunosuppressive therapy.22 On the other hand, selection of suitable sibling donors for stem cell transplant must take into account the mutation status and telomere length of potential candidates. The majority of patients respond, at least transiently, to androgen therapy. Androgens activate telomerase activity in hematopoietic cells by its aromatization into estrogens and via the estrogen receptor pathway.25 In a large series of patients undergoing immunosuppressive therapy (n = 183), telomere length of leukocytes at diagnosis did not predict clinical response at six months; however, patients with shorter telomeres (mostly without any telomerase mutation) had a higher possibility of relapse, an increased risk to evolve to myelodysplasia (especially the most feared monosomy 7) and acute myeloid leukemia, and poorer overall survival in comparison to patients with longer telomeres.26 Bone marrow cells of short-telomere aplastic patients also present increased chromosomal instability in vitro. Along with absolute reticulocyte and lymphocyte counts,27 telomere length is likely to be critical in therapy decision making.
Pulmonary Fibrosis
Up to 20% of patients with dyskeratosis congenita eventually develop pulmonary fibrosis.28 In fact, respiratory failure and liver cirrhosis are severe complications and causes of death after hematopoietic stem cell transplant for dyskeratosis congenita. The investigation of patients with familial idiopathic fibrosis led to the identification of telomerase gene mutations in 8% to 10% of familial cases.29 ;30 In these families, most affected subjects present pulmonary fibrosis only, although some individuals also develop aplastic anemia. Of clinical importance, in most of these cases, there is a strong history of cigarette smoking among clinically affected patients. In sporadic pulmonary fibrosis, the frequency of telomerase mutations is much lower (approximately 1%). The age of onset of pulmonary disease usually is after the fifth decade of life in telomerase-mutant patients, as opposed to marrow failure, in which disease also may manifest at younger ages. The mechanism for fibrosis in these patients is elusive, but it has been suggested that short telomeres cause a deficiency in pneumocyte stem cells and loss of alveolar cells, and fibrosis appears as a secondary event.
Short Telomeres and Cancer
Patients with aplastic anemia carrying telomerase mutations have an increased risk of developing cancer, in particular acute myeloid leukemia.13 A strong family history of myelodysplasia and myelodysplasia evolving to acute myeloid leukemia also is observed.31 These observations led us to investigate cases of de novo acute myeloid leukemia. We implicated constitutional telomerase mutations in up to 8% of acute myeloid leukemia cases; telomerase mutations correlated with chromosomal abnormalities, especially trisomy 8 and inv(16).32 Constitutional telomerase deficiency may cause variable degrees of telomere shortening in hematopoietic stem cells; due to short telomeres, these cells become prone to chromosomal instability (aneuploidy, breakage-fusion-bridges, translocations) and eventually, in the presence of other genetic and/or environmental factors, also more vulnerable to “second hits” and malignant transformation. In support of this hypothesis, we also have found that hematopoietic progenitor cells of aplastic anemia patients with short telomeres display increased chromosomal abnormalities in vitro, such as chromosomal breakage, aneuploidy, and end-to-end fusions.26 These cells display chromosomal instability and are probably more likely to evolve to a clonal disorder. Additionally, other healthy hematopoietic stem and progenitor cells with short telomeres that effectively activate cell signaling via p53 and p21 undergo proliferation arrest and senescence. The result is the selection of abnormal, chromosomally unstable stem and progenitor cells in the bone marrow.
At the same time that TERT mutations were associated with acute myeloid leukemia, the TERT locus also was associated with a variety of other cancers using a radically different technical approach. A large genome-wide association study (3259 cases and 4159 controls) detected two polymorphisms in the TERT gene as risk factors for lung cancer.33 Subsequent studies confirmed the association between the TERT locus and lung cancer.34 Interestingly, an additional very large Icelandic genome-wide association study (over 30,000 cancer cases and 45,000 controls) linked the TERT locus to basal cell carcinoma, bladder cancer, prostate cancer, and lung cancer.35 These association studies did not incriminate specific TERT polymorphisms as causative of cancers, but implicated the TERT locus as a highly significant genetic risk factor for cancer.
Additionally, telomere shortening has been observed in non-dysplastic mucosa surrounding premalignant or malignant lesions in ulcerative colitis.36 Telomere shortening was not seen in the mucosa of patients with ulcerative colitis that did not progress to dysplasia or cancer. Shorter telomeres also have been associated with progression to adenocarcinoma in patients with Barrett’s esophagus.37 Taken together, these studies, driven by different hypotheses, strongly implicate the telomerase locus as an important genetic risk factor in oncogenesis and leukemogenesis. Unfortunately, telomeres were not measured in genome-wide association studies. However, if the theoretical mechanism for telomerase mutations predisposing to acute myeloid leukemia is also applicable to other solid tumors, it is reasonable to speculate that shorter telomeres in different tissues also may contribute to chromosomal instability, which in the presence of other genetic and environmental factors (eg, smoking), may all contribute to tumorigenesis. This is an exciting area of active investigation.
Telomere Shortening and the Environment
Telomere shortening is not determined solely by telomerase mutations; environmental factors may also modulate the rate of telomere erosion in humans. Physiologically, telomeres become shorter with age; iatrogenically, telomeres may be shortened by intensive chemotherapy, such as in the setting of autologous hematopoietic stem cell transplant.38 Patients with accelerated telomere shortening after autologous transplant are at higher risk of developing secondary myelodysplasia. Patients with excessive telomere erosion after allogeneic hematopoietic stem cell transplant also are more likely to develop graft-versus-host disease.39 Cigarette smoking and psychological stress have also been shown to induce accelerated telomere attrition.22 On the other hand, estrogen therapy may abrogate the rate of telomere loss. In one study, women taking hormone replacement therapy have longer telomeres than those not receiving any hormone.40
Conclusion
Adequate telomere length maintenance is pivotal for hematopoiesis, and excessive telomere loss permeates the pathogenesis of bone marrow failure, malignancy, and fibrotic disease. Short telomeres inhibit cell proliferation but also predispose to chromosomal instability. Disease penetrance is variable and dependent on the degree of loss of telomerase enzymatic function, inheritance of short telomeres, telomere length, and unknown genetic, epigenetic, and environmental factors. Aplastic anemia, acute myeloid leukemia, and pulmonary fibrosis are diverse clinical expressions of a mechanism of which dyskeratosis congenita is the prototypical concomitant manifestation. Identification of families with marrow failure, severe liver disease, or pulmonary fibrosis has dramatically changed history-taking for the identification of telomerase mutations in patients with aplastic anemia.
Schematic representation of telomere structure and telomerase complex. Telomeres are at the extremities of chromosomes. The telomeric 3′ end terminates as a single-stranded, G-rich overhang. Telomeres are capped by a protein complex (TRF1, TRF2, TPP1, POT1, TIN2, and Rap1), collectively known as shelterin, that physically shield the DNA. The telomerase complex is composed of telomerase reverse transcriptase (TERT), the RNA component (TERC), and associated proteins (dyskerin, NOP10, NHP2, GAR). TERT enzymatically adds TTAGGG nucleotide repeats to the 3′ end of telomere’s leading strand using TERC as a template. Dyskerin, NOP10, NHP2, and GAR bind to TERC and stabilize the complex.
Schematic representation of telomere structure and telomerase complex. Telomeres are at the extremities of chromosomes. The telomeric 3′ end terminates as a single-stranded, G-rich overhang. Telomeres are capped by a protein complex (TRF1, TRF2, TPP1, POT1, TIN2, and Rap1), collectively known as shelterin, that physically shield the DNA. The telomerase complex is composed of telomerase reverse transcriptase (TERT), the RNA component (TERC), and associated proteins (dyskerin, NOP10, NHP2, GAR). TERT enzymatically adds TTAGGG nucleotide repeats to the 3′ end of telomere’s leading strand using TERC as a template. Dyskerin, NOP10, NHP2, and GAR bind to TERC and stabilize the complex.
Disclosures Conflict-of-interest disclosure: The author declares no competing financial interests. Off-label drug use: None disclosed.
References
Author notes
Hematology Branch, National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, MD