Abstract
In recent years, research in molecular genetics has been instrumental in deciphering the molecular pathogenesis of acute myeloid leukemia (AML). With the advent of the novel genomics technologies such as next-generation sequencing, it is expected that virtually all genetic lesions in AML will soon be identified. Gene mutations or deregulated expression of genes or sets of genes now allow us to explore the enormous diversity among cytogenetically defined subsets of AML, in particular the large subset of cytogenetically normal AML. Nonetheless, there are several challenges, such as discriminating driver from passenger mutations, evaluating the prognostic and predictive value of a specific mutation in the concert of the various concurrent mutations, or translating findings from molecular disease pathogenesis into novel therapies. Progress is unlikely to be fast in developing molecular targeted therapies. Contrary to the initial assumption, the development of molecular targeted therapies is slow and the various reports of promising new compounds will need to be put into perspective because many of these drugs did not show the expected effects.
Introduction
Acute myeloid leukemia (AML) is a genetically heterogeneous disorder characterized by the somatic acquisition of genetic and epigenetic alterations in hematopoietic progenitor cells that perturb normal mechanisms of self-renewal, proliferation, and differentiation. In the last years, an increasing number of gene mutations, deregulated expression of genes and noncoding RNAs (miRNAs), and epigenetic changes have been identified deciphering the enormous molecular heterogeneity of the disease.1 The discovery of some of these genetic changes has been largely facilitated by the development of genomics technologies such as global gene-expression analysis,1 next-generation sequencing,2,3 and single nucleotide polymorphism (SNP) array analysis.4
In recent years, there has been increasing translation of genetic diagnostics into the clinical setting. In the current World Health Organization (WHO) classification, more than half of AML cases are categorized on the basis of their underlying genetic defect, in part defining distinct clinicopathologic entities.5 Furthermore, cytogenetic and molecular genetic changes have been shown to be among the most powerful prognostic markers.1 Finally, novel therapies are being developed that target some of these genetic and epigenetic changes, such as the use of tyrosine kinase inhibitors (TKIs) and demethylating agents.6
There are still limitations with respect to the use of these new biomarkers in clinical practice. The prognostic impact of some of the markers was mostly evaluated in retrospective studies, often with relatively low patient numbers and not taking into account interactions with other molecular markers. Furthermore, for clinical decision making, predictive markers that are attributed to the clinical benefit of a specific treatment are needed. Table 1 summarizes selected molecular markers in adult AML with their prognostic value and their impact on treatment decisions.
Prognostic value and impact on treatment decision of selected molecular markers in adult AML
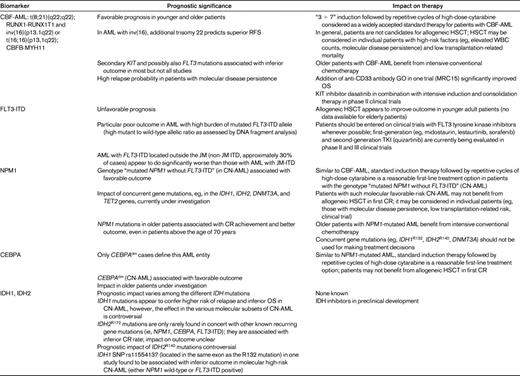
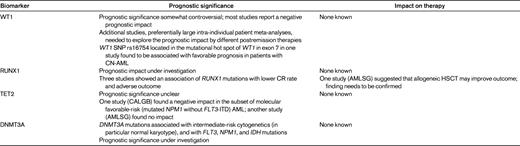
The first part of this review is devoted to biomarkers that have entered clinical practice and affect diagnosis and guidance for standard or investigational therapy. In the second part, selected markers that remain investigational are discussed. The deregulated expression of genes is not the focus of this review.
AML with RUNX1-RUNX1T1 and CBFB-MYH11
Core-binding-factor AML (CBF-AML) characterized by t(8;21)(q22;q22); RUNX1-RUNX1T1 and inv(16)(p13.1q22) or t(16;16)(p13.1;q22); and CBFB-MYH11 belong to the genetic favorable-risk category.6,7 In younger adult patients, response rates are approximately 90%, and consolidation therapy with repetitive cycles of high-dose cytarabine (3 g/m2 every 12 hours on days 1, 3, and 5), a widely accepted standard therapy for patients with CBF-AML, results in 60%-70% long-term survival probabilities. Older patients also appear to significantly benefit from dose intensification of standard chemotherapy.6
In the British Medical Research Council (MRC) AML15 trial, 1113 patients, predominantly younger than 60 years of age, were randomly assigned to receive a single dose of the anti-CD33 immunoconjugate gemtuzumab ozogamicin (GO) (3 mg/m2) in induction course 1 and the first consolidation course.8 Although there was no difference in response and survival in the overall trial population, a predefined analysis by cytogenetic risk groups showed a significant survival benefit for patients with CBF-AML. Market withdrawal of GO for the moment prevents the conduction of a confirmatory trial in patients with CBF-AML.
In recent years, molecular analyses have identified secondary genetic changes in CBF-AML, most commonly mutations in the genes encoding KIT, FMS-like tyrosine kinase 3 (FLT3), and RAS.7 Activating KIT mutations are found in approximately one-third of CBF-AML, and have been associated with a significantly inferior outcome in most but not all studies. Furthermore, the KIT receptor is expressed at significantly higher levels compared with other AML subgroups. Activating tyrosine kinases are potential targets for the use of TKIs. Both the German-Austrian AML Study Group (AMLSG; www.ClinicalTrials.gov identifier NCT00850382) and Cancer and Leukemia Group B (CALGB) (www.ClinicalTrials.gov identifier NCT01238211) are conducting a trial combining dasatinib, a potent inhibitor of mutated and wild-type KIT, with conventional induction and consolidation therapy, followed by a 1-year dasatinib maintenance therapy in patients with CBF-AML.
Finally, molecular disease persistence has been shown to be a highly predictive factor for relapse-free survival (RFS) and overall survival (OS).9 Future studies should incorporate monitoring of fusion transcript copy ratios to evaluate whether early intervention, for example by allogeneic hematopoietic stem cell transplantation (HSCT) or using an investigational agent, will improve outcome.
AML with FLT3 mutations
FLT3 is a member of the class III receptor tyrosine kinase family that plays an important role in proliferation, survival, and differentiation of hematopoietic progenitor cells. FLT3 mutations are among the most common genetic changes in AML. They are primarily located in 2 functional domains of the receptor: the juxtamembrane (JM) domain and the activation loop of the tyrosine kinase domain (TKD). FLT3 internal tandem duplications (ITDs) are found in approximately 20% of all AML (cytogenetically normal [CN]–AML: 28%-34%) and cluster in the JM domain.1 However, more recently, it was shown that approximately 1/3 of ITDs insert in the TK1 rather than in the JM domain.10,11 The activation loop in the carboxyterminal lobe of the TKD is affected by point mutations, small insertions, or deletions mainly involving codon 835 and 836 in 11%-14% of CN-AML.1
When treated with conventional chemotherapy, prognosis of AML with FLT3-ITDs is significantly worse compared with AML without the mutation. Several studies have shown that the allelic ratio affects outcome in that AML with a high mutant–to–wild-type ratio do significantly worse compared with AML with lower ratios.1 A common mechanism for loss of the FLT3 wild-type allele in cases with high allelic ratios is mitotic recombination leading to partial uniparental disomy. Furthermore, one study showed that non-JM FLT3-ITDs are associated with a particularly poor outcome.11 The prognostic relevance of the FLT3-TKD mutation has remained controversial.
There are 2 important aspects in the decision-making process in AML with FLT3-ITDs. First, several FLT3 inhibitors are in various stages of clinical development; for example, midostaurin (PKC412), lestaurtinib (CEP-701), sunitinib (SU-11248), sorafenib (BAY-43-9006), and the second-generation compound quizartinib (AC220).12 When used as single agents, the first-generation TKIs have limited clinical activity in patients with FLT3 mutations, with at most transient reduction in blood blast counts and, less frequently, bone marrow (BM) blast counts. The large randomized trial with midostaurin in combination with chemotherapy for first-line treatment of younger adult patients will reach its accrual goal at the end of 2011 (www.ClinicalTrials.gov identifier NCT00651261). Quizartinib is a novel compound expressly optimized as a FLT3 inhibitor for the treatment of AML. In a first-in-humans phase I study, quizartinib given as a single agent has proven to be highly efficacious, leading to high response rates in relapsed and refractory AML exhibiting FLT3-ITDs.13 A pivotal phase II trial for relapsed patients with FLT3-ITDs is nearly completed (www.ClinicalTrials.gov identifier NCT00989261). Second, there is increasing evidence showing that allogeneic HSCT may be of benefit for patients with FLT3-ITDs.14,15 A beneficial effect was shown for patients with CN-AML and unfavorable genotypes that include the FLT3-ITD–positive patients.14
AML with the NPM1 mutation
NPM1 mutations are the most frequent known mutations in AML. They are found in 25%-35% of adult AML and are particularly frequent in CN-AML (45%-64%).1 NPM1 mutations lead to abnormal cytoplasmic localization of the protein that is caused by disruption of the N-terminal nucleolar localization signal of nucleophosmin and by the generation of a new nuclear export signal. The role of NPM1 mutations in leukemogenesis has largely remained elusive. In a recent knock-in mouse model of the most common type A NPM1 mutation, it was shown that such mutant Npm1 knock-in alleles are AML-initiating lesions leading to Hox gene overexpression, increased self-renewal, and expanded myelopoiesis.16 One-third of mice develop delayed-onset AML by activation of a set of proliferative molecules and pathways, often in combination with transcriptional regulators. In human AML, NPM1 mutations have been shown to be associated with FLT3-ITDs and, more recently, also with IDH and DNMT3A mutations.3,17–22
NPM1 mutations are associated with several presenting clinical and laboratory features, such as predominance of female sex and higher BM blast percentages, lactate dehydrogenase serum levels, and white blood cell counts; blast cells typically show high CD33- but low or absent CD34-antigen expression. NPM1 mutations, in particular those without concurrent FLT3-ITDs, have consistently been shown to confer a superior outcome.1,14 As a consequence, in the recently published AML recommendations, the genotype “mutated NPM1 without FLT3-ITD” (CN-AML only) has been incorporated into the genetic favorable-risk category, together with CBF-AML.6 The prognostic value of the NPM1/FLT3-ITD genotypes will need to be revisited in the context of the newly discovered mutations, in particular IDH and DNMT3A mutations. First studies suggest that IDH1 mutations may confer inferior outcome in CN-AML (see “IDH1 and IDH2 mutations”).
After conventional induction and consolidation chemotherapy, younger adult patients with mutated NPM1 without FLT3-ITDs have survival probabilities of approximately 60%. A study by AMLSG suggested that these patients may not benefit from allogeneic HSCT in first complete remission (CR).14 In general, patients with genetically favorable risk profiles, such as CBF-AML, AML with mutated NPM1 without FLT3-ITDs, and possibly also AML with double-mutated CEBPA (see “AML with CEBPA mutations”), may not be candidates for allogeneic HSCT in first CR. Nonetheless, allogeneic HSCT may be considered in patients with molecular disease persistence,23 in those with a very low transplantation-related risk, or if new transplantation strategies are investigated with a clinical trial. The favorable prognostic impact of NPM1 is not restricted to younger adults, but also extends to older patients, even to those above the age of 70 years.24,25 Therefore, screening for a NPM1 mutation has become clinically relevant in selecting those older patients who are likely to benefit from intensive conventional chemotherapy.
No molecular therapy is currently available in AML with NPM1 mutations. Based on the high CD33 expression, the use of the anti-CD33 antibody GO appeared to be an attractive approach. However, in a subset analysis within the MRC15 trial, GO failed to have a significant survival benefit in AML with a NPM1 mutation.26 In a retrospective predictive marker analysis, AMLSG reported on the potential benefit of all-trans retinoic acid in AML with mutated NPM1 without FLT3-ITDs.24 This effect could not be confirmed in a study by the British MRC.26
AML with CEBPA mutation
Similar to NPM1 mutations, CEBPA mutations are primarily found in CN-AML (10%-18%).1 AML with CEBPA mutations can be divided into 2 subgroups: those with a single mutation (CEBPAsm; one-third of cases) and those with double mutations (CEBPAdm; two-thirds of cases). In the majority of CEBPAdm AML, both alleles are mutated, typically consisting of one N-terminal mutation on one allele and a C-terminal mutation on the second allele.
In previous studies that considered CEBPAsm and CEBPAdm as one group, mutated CEBPA was associated with a favorable outcome. Recent studies, however, suggest that AML with CEBPAdm should be clearly distinguished from AML with CEBPAsm.27,28 This conclusion is based on: (1) clinical outcome analysis (only CEBPAdm is an independent prognostic factor for favorable outcome); (2) the pattern of concurrent gene mutations (significant higher frequency of NPM1 mutations and FLT3-ITDs in AML with CEBPAsm); and (3) global gene-expression studies (only CEBPAdm AML, but not CEBPAsm AML, expresses a unique signature). As a consequence, only AML with CEBPAdm should be considered as a distinct entity within the WHO classification and as a prognostic category in the current risk classification.
Therapeutic recommendations are similar to those of AML with mutated NPM1 without FLT3-ITDs.6 These patients also may not benefit from allogeneic HSCT. This statement, however, is not based on data but on the assumption that, in general, favorable-risk AML may not benefit from this approach. Large meta-analyses and intergroup clinical trials are warranted to achieve progress in this relatively small subgroup of AML.
Investigational molecular markers
There is a myriad of novel gene mutations that have been discovered in part by the application of genomics technologies such as SNP array analysis followed by sequence analysis of candidate genes in regions of recurrent copy number alterations and by next-generation sequence studies. These biomarkers include mutations in the RUNX1, IDH1, IDH2, DNMT3A, WT1, TET2, MLL, ASXL1, CBL, NRAS, KRAS, and TP53 genes.1 All of these markers remain investigational and have so far had no impact on treatment decisions. For some of the markers, there is still a paucity of studies evaluating their prognostic and predictive impact. A brief review of selected markers is given in the following sections.
RUNX1 mutations
The gene encoding runt-related transcription factor 1 (RUNX1) is targeted by chromosomal rearrangements such as t(8;21)(q22;q22) and intragenic mutations in AML. The few studies evaluating the clinical impact of intragenic RUNX1 mutations suggest that these lesions may be associated with inferior outcome.29–31 The various frequencies of RUNX1 mutations reported in these studies may be due to patient selection and ethnic differences. In a Taiwanese study, RUNX1 mutations were detected in 13.2% of AML; mutations predicted for lower CR rate and shorter disease-free survival (DFS) and OS; in a multivariate analysis, RUNX1 mutations were an independent prognostic factor for OS.29 In another study of 449 AML cases that was selected for AML with specific karyotypes (ie, normal and noncomplex karyotypes), RUNX1 mutations were found in 32.7%; mutations predominantly clustered in AML FAB M0 (65.2%) and in AML with trisomy 13 (90%), but were also found in a relatively high frequency (26.3%) in CN-AML. Patients with RUNX1 mutations had a shorter OS and event-free survival (EFS) compared with patients without RUNX1 mutations.30 In a study by AMLSG of 945 unselected younger adult patients, RUNX1 mutations were found in only 5.6%.31 RUNX1 mutations clustered in the intermediate-risk cytogenetic group (CN-AML 6.3%). RUNX1 mutations were significantly associated with MLL partial tandem duplications and with IDH1/IDH2 mutations. Mutations predicted for resistance to chemotherapy as well as inferior EFS, RFS, and OS. In multivariable analysis, RUNX1 mutations were an independent prognostic marker for shorter EFS. Explorative subgroup analysis revealed that allogeneic HSCT had a favorable impact on RFS in patients with RUNX1 mutations.
IDH1 and IDH2 mutations
Mutations in the isocitrate dehydrogenase 1 (IDH1) gene were discovered by sequencing of an entire AML genome.2 Subsequent studies found not only IDH1, but also IDH2 mutations as recurrent molecular abnormalities in AML.17–19 Mutations affect typically, but not exclusively, IDH1 at codon R132 and IDH2 at codons R140 or R172. The combined frequency of IDH mutations in unselected cohorts of AML varies between 15% and 22%.18,19,32 Both IDH1 and IDH2 mutations result in a substrate shift to α-ketoglutarate (α-KG) with accumulation of 2-hydroxyglutarate (2-HG) that is a putative oncogenic metabolite. More recently, 2-HG has been characterized as a competitive inhibitor of α-KG-dependent dioxygenases, including histone demethylases and the TET family of 5-methylcytosine hydroxylases, thereby leading to DNA methylation alterations.33
Several recent studies investigated the prognostic impact of IDH1/2 mutations.17–21,32 There is increasing evidence that the prognostic impact varies among the different mutations and also depends on the context of concurrent mutations. IDH1R132 and IDH2R140 are associated with intermediate-risk cytogenetics, in particular with CN-AML, and among CN-AML with NPM1 mutations.18–20,32 In contrast, IDH2R172 mutations are only rarely found together with other known recurrent gene mutations.17–18,32 IDH1 mutations confer inferior outcome in CN-AML, but the prognostic effect in the molecular subsets of CN-AML is controversial. In the studies by CALGB17 and AMLSG,18 IDH1 mutations predicted for inferior outcome in favorable-risk (NPM1-mutated/FLT3-ITD–negative) AML, whereas in the studies by MRC20 and the Dutch-Belgian Hemato-Oncology Cooperative Group (HOVON),19 IDH1 mutations predicted for inferior outcome in FLT3-ITD–negative and FLT3-ITD–negative/NPM1 wild-type AML, respectively. The data on the prognostic significance of IDH2 mutations are also not concordant. AML with IDH2R172 mutations appear to constitute a distinct biological and clinical subset; they display a distinct microarray gene- and miRNA-expression profile,17 and in the studies by CALGB17 and MRC,32 they have been associated with a lower CR rate and with inferior survival. In the study by AMLSG, IDH2R140 mutations predicted for inferior survival in molecular favorable-risk CN-AML,18 whereas in the recent study by the MRC, IDH2R140 mutations were an independent favorable prognostic factor for RFS and OS.32 In the study by the HOVON group,19 no effect was found for IDH2 mutations, although no distinction was made between the 2 different IDH2 mutations. Individual patient data meta-analyses will be needed to resolve these controversies and to identify specific treatment effects.
DNMT3A mutations
Similar to the discovery of IDH mutations, mutations of DNMT3A were identified by next-generation sequencing techniques.3,34 DNMT3A, as well as DNMT3B and DNMT1, encode for methyltransferases catalyzing the addition of a methyl group to the cytosine residue of CpG dinucleotides. Ley et al sequenced DNMT3A in 282 AML samples and detected mutations in 22.1% of cases; mutations predominantly clustered at amino acid R882.3 Clinically, DNMT3A mutations were enriched in intermediate-risk cytogenetics and were associated with FLT3, NPM1, and IDH mutations. No differences were observed in the levels of DNMT3A in global gene-expression profiling or in the methylation content in mass spectrometry independently of DNMT3A mutation status, although 182 genomic regions had significantly different methylation levels (at specific genomic locations) using MeDIP-chip analysis.3 Yan et al identified the mutation by whole-exome sequencing of a case of acute monocytic leukemia.34 They subsequently found mutations in 20.5% of cases, and these mutations were associated with inferior survival. DNMT3A mutants showed reduced enzymatic activity resulting in decreased DNA methylation in several thousand genomic regions. In a recent study of 489 younger adult patients, the mutation frequency was 17.8%; mutations were associated with NPM1, IDH1, and FLT3-ITD mutations.22 DNMT3A mutations predicted for inferior OS. Further studies are needed to evaluate the prognostic effect of DNMT3A mutations.
WT1 mutations
More than a decade ago, King-Underwood et al reported on Wilms' Tumor 1 (WT1) gene mutations in 10% of acute leukemias.35 Recently, further studies were performed on larger cohorts showing mutations primarily in CN-AML with a frequency of 10%-13%. The prognostic impact of the mutation remains somewhat inconclusive. Whereas in the studies by MRC, CALGB, and Acute Leukemia French Association (ALFA) groups, a negative impact of the mutation on OS was shown, no impact was found in a study of 617 CN-AML by AMLSG.1,35 The latter study only found a possible negative impact in AML with concurrent WT1 and FLT3-ITD mutations.
In one study, another approach was pursued by analyzing the known SNP rs16754 located in the mutational hot spot of WT1 in exon 7.36 The SNP was shown to be associated with favorable outcome in patients with CN-AML, although the mechanisms by which this SNP may alter WT1 function and possibly increase chemosensitivity remain unknown.
TET2 mutations
Recently, the tet oncogene family member 2 (TET2) gene was identified as a candidate tumor suppressor gene in a variety of myeloid disorders using an integrated genomic approach, including comparative genomic hybridization and SNP array analysis.4 Subsequent sequencing analysis revealed heterogeneous TET2 mutations in 12%-27% of patients with AML and in other myeloid diseases.
The TET proteins are involved in epigenetic regulation. Both TET1 and TET2 proteins convert 5-methylcytosine (5mC) to 5-hydroxymethylcytosine (5hmC), a process thought to play an important role in DNA demethylation.32,37 TET2-mutated AML has been shown to display uniformly low levels of 5hmC compared with normal controls, thereby supporting a functional relevance of TET2 mutations in leukemogenesis. Interestingly, low 5hmC levels were also observed in a fraction of TET2-wild-type cases clinically resembling TET2-mutated AML.37 A recent publication by Figueroa et al showed that mutations of IDH1/2 are mutually exclusive with mutations of TET2.38 Moreover, the enzymatic activity of TET2 is impaired by 2-HG produced by mutant IDH1/2.32,38
First studies in small cohorts of AML revealed inconclusive results regarding the prognostic impact of TET2 mutations.1 In a study of 427 patients with CN-AML (18-83 years of age), mutations were found in 23% of cases.39 In multivariable models, TET2 mutations were associated with inferior EFS and DFS only among molecular favorable-risk CN-AML—that is, AML with mutated CEBPA and/or mutated NPM1 without FLT3-ITDs. In contrast, no prognostic impact of TET2 mutations on survival was found in a study of 783 AML cases by AMLSG in the whole cohort, in CN-AML, or in AML with mutated NPM1 without FLT3-ITDs.40
Conclusions
Progress in deciphering the molecular pathogenesis of AML has been impressive, and translation of these findings into the clinical setting has been increasing in recent years. Nonetheless, given the enormous molecular heterogeneity of the disease, large cohorts of patients will need to be analyzed for all of the markers to evaluate their interaction and their precise prognostic value. Furthermore, it will be of prime importance to study these markers in the context of novel therapies to identify biomarkers that allow the definition of patient subgroups that benefit from a particular treatment approach. To accelerate progress, international collaboration of study groups is warranted.
Acknowledgments
Supported in part by a grant from the Bundesministerium für Bildung und Forschung (“IPD-Meta-Analysis: A Model-Based Hierarchical Prognostic System for Adult Patients with Acute Myeloid Leukemia”; grant number 01KG0605).
Disclosures
Conflict-of-interest disclosure: H.D. has consulted for and received honoraria from Celgene, Ambit, Lilly, and Genzyme. V.I.G. declares no completing financial interests. Off-label drug use: None disclosed.
Correspondence
Prof Hartmut Döhner, Department of Internal Medicine III, University Hospital of Ulm, Albert-Einstein-Allee 23, 89081 Ulm, Germany; Phone: 49-731-500-45501; Fax: 49-731-500-45505; e-mail: hartmut.doehner@uniklinik-ulm.de.
