Abstract
Given the commonality of bleeding symptoms in the general population and the diagnostic limitations of available laboratory testing for mild bleeding disorders, there has been increasing interest in a more precise quantification of bleeding symptoms. The Vicenza bleeding score (and its successor, Molecular and Clinical Markers for the Diagnosis and Management of Type 1 von Willebrand disease [MCMDM-1 VWD]) and its pediatric counterpart, the Pediatric Bleeding Questionnaire, are validated research tools that have demonstrated their ability to discriminate between healthy subjects and those with VWD. These instruments collect data regarding both the presence and severity of a variety of bleeding symptoms and generate a bleeding score by summing the severity of all symptoms reported by a subject. More recent work demonstrates the promise of these tools as a diagnostic aid in the evaluation of patients with a suspected inherited mild bleeding disorder, as well as the development of a condensed score with increased clinical applicability. This review focuses on the development of these bleeding assessment tools, recent publications applying and refining these instruments, and current limitations of bleeding scores. Needed research studies and potential clinical applications of bleeding scores are also discussed. The ultimate goal would be for bleeding scores to be integrated with the results of standardized laboratory testing to allow for a universal diagnostic approach to patients with suspected bleeding disorders.
Introduction
The diagnostic evaluation of a patient presenting with symptoms of easy bruising or bleeding remains a challenge for the consulting hematologist. Whereas symptoms such as spontaneous joint bleeding or excessively prolonged umbilical stump bleeding are suggestive of specific severe bleeding disorders, the majority of patients seen are much more likely to have mild underlying defects such as type 1 VWD or platelet function defects. In these cases, it is the lifelong “hemorrhagic picture” of the patient who informs the evaluation,1 and drawing this picture requires obtaining a detailed and objective bleeding history.
The primary difficulty lies in the fact that mild bleeding events are commonly reported by patients both with and without inherited bleeding disorders, making it difficult for hematologists to define a “significant bleeding history.” Mauer et al have recently verified the high frequency of bleeding in healthy adults through the development of a comprehensive, ontology-backed, Web-based questionnaire (http://ds9.rockefeller.edu/RUBHPSR/; accessed May 1, 2012).2 In that study, 500 healthy adults were recruited through online and print advertisements or in primary care clinic waiting rooms, and a trained physician or nurse conducted a bleeding interview. In this healthy population, 25% of subjects reported epistaxis, 18% easy bruising, 18% prolonged bleeding after a tooth extraction, and 47% of women reported heavy menstrual bleeding. A similar study has not yet been performed in pediatric populations, but symptoms such as easy bruising and epistaxis are also commonly reported in children. Nosek-Cenkowska et al administered a bleeding questionnaire to 251 otherwise healthy children undergoing tonsillectomy and/or adenoidectomy.3 In the 228 “nonbleeders” (those patients without excessive bleeding during or after the procedure), 24% reported easy bruising and 39% reported epistaxis. Not only is bleeding common in patients with and without bleeding disorders, but hematologists need to be aware that the number and perceived severity of symptoms reported by a patient can be influenced by a variety of factors. A patient or parent's education level, personality, experience with bleeding in other family members, as well as the manner in which symptoms are reported (ie, a self-administered survey compared with a guided interview), may lead to under- or overreporting of bleeding symptoms.1 As a result of these challenges, there has been increasing interest among researchers and clinicians in efforts to precisely and objectively quantify bleeding symptoms.
The development of the Vicenza bleeding score
The majority of investigations in this arena over the past decade have included or stemmed from a bleeding questionnaire and score developed by Rodeghiero, Tosetto, and their collaborators at the Vicenza General Hospital in Vicenza, Italy.4 These investigators first sought to establish minimal clinical criteria for the identification of patients affected by VWD, and in 2005, published the validation of a physician-administered standardized questionnaire and bleeding score. The study population included 42 type 1 VWD obligatory carriers and 215 control subjects. Participants were asked about a multitude of bleeding symptoms, such as epistaxis, ecchymoses, menstrual bleeding, and postsurgical bleeding, and the severity of each symptom was graded using a score ranging from 0 (absence of symptom) to 3. Grade 1 is given when a patient reports the presence of bleeding, grade 2 if the symptom required evaluation by a physician but no active intervention, and grade 3 if there was some type of intervention. The final bleeding score is generated by summing the severity of all bleeding symptoms reported by the patient. A threshold below which a specific bleeding episode should be reported as trivial (grade 0) rather than a true symptom is also described. For example, bleeding after tooth extraction is described as a symptom only if bleeding occurs after the patient leaves the dental office or prolonged bleeding at the office caused a delay in the procedure.
In a retrospective analysis, the Vicenza score was found to be very specific, although less sensitive, for identifying individuals with VWD.4 Using a definition of more than 2 bleeding symptoms had a sensitivity of 50% and a specificity of 99.5% for identifying type 1 VWD obligatory carriers. When using the bleeding score rather than just the number of symptoms, a score of 3 in male subjects and 5 in female subjects was 98.6% specific and 69.1% sensitive for the identification of individuals with type 1 VWD. In a classification and regression tree (CART) analysis, the 2 most predictive symptoms for the identification of VWD were bleeding after tooth extraction or surgery and cutaneous bleeding (ecchymoses or hematomas).
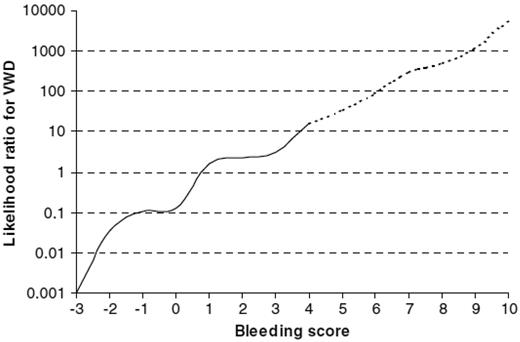
A subsequent refinement of the bleeding score was used in the European MCMDM-1VWD study.5 In this version, the number of possible grades for each bleeding symptom was increased, ranging from −1 to 4. Grade 4 accounts for the most dramatic presentations (requiring blood transfusion or surgery to control bleeding), whereas the −1 grade highlights the importance of the absence of bleeding despite a hemostatic challenge such as dental extraction or surgery. In the MCMDM-1VWD study, which included 154 families with at least 2 family members affected by type 1 VWD, as well as unaffected family members and controls, a higher bleeding score was found to be associated with an increased likelihood of bleeding after surgery or tooth extraction in patients with known VWD.5 The likelihood of VWD increased exponentially with each unit increase in the bleeding score (Figure 1). The bleeding score also correlated with VWF Ag and ristocetin cofactor levels in an apparently linear relationship. A more recent study also demonstrated a relationship between increasing PFA-100 ADP closure times and higher bleeding scores.6
Likelihood ratios for VWD based on the Vicenza bleeding assessment tool (−1 version) and on data from the MCMDM-1 study. (Reprinted with permission from Tosetto et al.15 Copyright 2007, Elsevier.)
Likelihood ratios for VWD based on the Vicenza bleeding assessment tool (−1 version) and on data from the MCMDM-1 study. (Reprinted with permission from Tosetto et al.15 Copyright 2007, Elsevier.)
Recent applications of the bleeding score
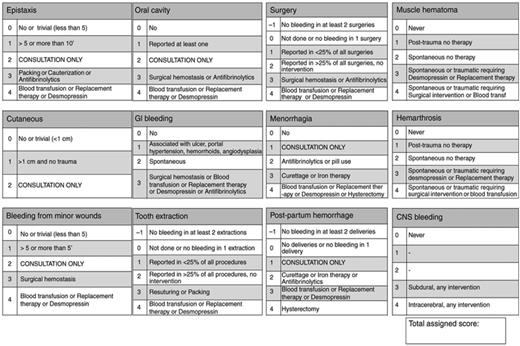
Although they have shown great promise as research tools, both versions of the Vicenza score are detailed questionnaires (12-17 pages) that take approximately 40 minutes to administer, making them impractical for clinical use. Bowman et al developed a condensed version of the MCMDM-1VWD bleeding assessment tool by maintaining only the details that affect the bleeding score directly, resulting in a 6-page questionnaire that requires 5-10 minutes to administer (Figure 2).7 In 100 healthy subjects, the range of normal bleeding scores was found to be −3.2 to +3.6 (mean of 0.16 ± 2 SD), therefore an abnormal bleeding score was considered to be ≥ 4. In comparison, the median bleeding score in 42 patients with known VWD was 14 (range, 4-29). In a separate analysis of 217 subjects undergoing a prospective evaluation for VWD, the condensed bleeding score demonstrated 100% sensitivity, 87% specificity, 20% positive predictive value, and 100% negative predictive value for the diagnosis of VWD.7 The correlation between the full MCMDM-1VWD instrument and the condensed version (calculated on a subset of 17 patients) was excellent, with a Spearman rho of 0.97. Inter-observer reliability of the condensed version (calculated on a subset of 24 patients) was reasonable, with a Spearman rho of 0.72.
Condensed version of the bleeding assessment tool. Reprinted with permission from Bowman et al.7
Condensed version of the bleeding assessment tool. Reprinted with permission from Bowman et al.7
The Vicenza group used this condensed version of their bleeding score to prospectively evaluate the clinical usefulness of the score for the diagnosis of mild bleeding disorders in 215 previously undiagnosed patients referred to either the Vicenza General Hospital or Leiden University Medical Center in The Netherlands.8 Study subjects included those referred for evaluation of bleeding symptoms, abnormal laboratory test results, or family history of a known bleeding disorder. Subjects with a bleeding score of > 3 were considered to have an abnormal bleeding history. Final diagnoses in the study population included VWD, mild hemophilia, platelet function defects, and Factor XI deficiency. Assuming the population prevalence of mild bleeding disorders to be 1%, a normal bleeding score showed a 99.2% negative predictive value, essentially ruling out the presence of a mild bleeding disorder in patients with a normal bleeding score from the general population. Conversely, the positive predictive value was acceptable in patients referred for hemostatic evaluation (71%) or family history (77.5%). Adding a measurement of the activated partial thromboplastin time increased the negative predictive value of the bleeding score significantly (to 99.6%).
Most recently, Azzam et al assessed the diagnostic utility of the condensed MCMDM-1VWD bleeding score as a predictor of bleeding disorders in 30 women with unexplained heavy menstrual bleeding.9 The 20 (66.6%) women eventually diagnosed with a bleeding disorder had significantly higher bleeding scores than those without a bleeding disorder, and receiver operator characteristic curve analysis demonstrated that, using a cutoff of 3.5, the bleeding score demonstrated 85% sensitivity, 90% specificity, 89% positive predictive value, and 86% negative predictive value for the presence of an underlying bleeding disorder.
The Pediatric Bleeding Questionnaire
The majority of subjects in the studies thus far reviewed were adults, and obtaining a bleeding history in the pediatric population presents additional challenges to the hematologist. As a result of their shorter life experience, children have fewer or no exposures to bleeding challenges such as dental extractions, surgeries, menarche, and childbirth.10 In 2009, Bowman et al published the Pediatric Bleeding Questionnaire (PBQ), which has an identical format to the MCMDM-1VWD score with the exception of an “other” category, which has pediatric-specific bleeding symptoms such as umbilical stump bleeding, cephalohematoma, postcircumcision bleeding, postvenipuncture bleeding, and macroscopic hematuria. These investigators first administered the PBQ to a naive primary care pediatric population (N = 151), and determined the normal range of scores to be −1.5 to 2.5 (mean ± 2 SD). A “positive” bleeding score was therefore defined as ≥ 2.11 Using this definition, the PBQ had a high negative predictive value (99%) for VWD and could distinguish accurately between children with and without VWD. However, this study was limited by the small number of patients with VWD, resulting in a low positive predictive value (14%). Bleeding symptoms significantly associated with a diagnosis of VWD included epistaxis either of long duration or requiring medical attention to be stopped, bruising brought to medical attention, excessive bleeding from minor wounds, oral cavity bleeding requiring medical attention, gastrointestinal bleeding, and bleeding after dental extraction.
Biss et al evaluated the performance of the PBQ in a cohort of 100 children with known VWD and compared it with a control population of 21 unaffected siblings.12 The median bleeding score in children with VWD was 7.0 (range, 0-29) compared with a median of 0 (range, −1 to 2) in unaffected siblings. Children with more severe forms of VWD tended to have higher bleeding scores, and scores increased with age in patients with definite type 1 and type 3 VWD. However, there was no difference in median scores between female and male subjects. Similar to the original Vicenza score, more studies are needed regarding the use of the PBQ in identifying platelet function defects and other inherited mild bleeding disorders. Biss et al did evaluate the use of the PBQ in a small cohort (N = 23) of children with a wide variety of inherited platelet disorders, and found that whereas there was significant heterogeneity in the scores obtained between diagnostic groups, 96% of patients had an abnormal bleeding score (defined as ≥ 2).13
The high negative predictive value of the PBQ suggests that this tool could be a valuable addition to the evaluation of children with suspected inherited bleeding disorders. However, whereas the PBQ has been validated as a research tool in evaluating bleeding severity in children with known VWD, further validation studies in children prospectively evaluated for an inherited bleeding disorder are required before recommending the use of the PBQ in clinical practice. Marcus et al sought to assess the Vicenza score's predictive power in identifying type 1 VWD, low VWF, and platelet function defects in a prospective cohort of patients referred to a pediatric hematology clinic for evaluation of a possible bleeding disorder.14 In this setting, the Vicenza score demonstrated poor diagnostic utility with the exception of high specificity in ruling out definite type 1 VWD. Whereas the negative predictive value of excluding type 1 VWD was high, simpler qualitative criteria (in which > 2 bleeding symptoms was defined as abnormal) was similarly predictive.
Summary
The determination of the presence and severity of bleeding symptoms is a key component in the evaluation of a patient with a suspected bleeding disorder. Given the commonality of bleeding symptoms in the general population and the diagnostic limitations of available laboratory testing for mild bleeding disorders, there has been increasing interest in a more precise quantification of bleeding symptoms.1,15 The Vicenza score and its pediatric counterpart, the PBQ, have both demonstrated their ability to discriminate between healthy subjects and those with VWD.4,11 These instruments can also be used to describe symptoms and patterns of bleeding in patients with a variety of inherited bleeding disorders. The similarities between the PBQ and Vicenza score will also improve the quality and standardization of research in this field by allowing for a common method of communicating and comparing results across studies.
In 2010, the ISTH/SSC Joint Working Group agreed to establish a single bleeding assessment tool (the BAT) to standardize the reporting of bleeding symptoms.16 Because data comparing the 2 versions of the Vicenza score (0-3 and −1-4) were not available at the time, the working group elected to develop a new diagnostic bleeding score, albeit one that is heavily based on the 0-3 Vicenza score. The validity, inter-rater and test-retest reliability, and predictive power of this new score all require investigation. Bidlingmaier et al recently compared the ISTH BAT with the PBQ in a cohort of 100 children with a suspected bleeding disorder, and found that both tools were able to discriminate between children with and without defined bleeding disorders.17 The ISTH instrument can be found at http://www.isth.org/default/assets/File/Bleeding_Type1_VWD.pdf (accessed April 30, 2012). Comparing the 0-3 and −1-4 scoring systems is an active area of investigation. When evaluating a subset of patients from prior studies in which all the questions relevant to compute both bleeding scales were available, Tosetto et al reported that both bleeding scores appear equally useful for diagnostic purposes, with similar area under the curve in receiver operator characteristic curve analysis.18
Whereas bleeding scores have demonstrated great promise as valuable research tools, their applicability in clinical practice requires further study. The creation and validation of a condensed bleeding score has been completed, and is one major step toward clinical applicability. However, to be of clinical use, a bleeding assessment tool must also be widely applicable to the full spectrum of mild bleeding disorders. Whereas the tools discussed in this review have never been intended for use in severe bleeding disorders such as hemophilia, more studies of their use for diagnoses of mild bleeding disorders other than VWD are greatly needed. In fairness, however, current variations in the laboratory approach and interpretation of platelet function testing need to be resolved before bleeding scores can be used to their full diagnostic potential. Allowing the patient or parent to complete the bleeding assessment tool on their own would also enhance their clinical applicability, but it is important to note that these instruments were designed to be administered by trained clinicians, and further study is necessary to demonstrate that self-reporting of symptoms is accurate before such tools can be used in settings such as the clinic waiting room. Finally, clinicians would need to know the exact cutoff for an abnormal score, which has varied in previous studies and appears to be somewhat dependent on patient age, patient gender, and the clinical setting.
In the primary care setting, and even in the hematology setting, the greatest clinical utility of bleeding scores lies in their high negative predictive value, and perhaps their greatest value is in the identification of patients for whom testing for VWD is not necessary.7 It is important to note that in very young patients the bleeding history may be completely negative due to lack of hemostatic challenges. Therefore, some laboratory work-up will always be required to exclude a bleeding disorder in a young patient with a positive family history of a bleeding disorder. Conversely, if the bleeding score is elevated and VWF levels are normal, this should be a sign for the hematologist to actively pursue alternate bleeding disorder diagnoses. The study of bleeding assessment tools remains an active and evolving field of research. Future work is anticipated to focus on additional validation of bleeding scores in a variety of mild inherited bleeding disorders. Larger prospective studies of these instruments' diagnostic utility in the evaluation of adult and pediatric patients referred for a possible bleeding disorder are needed. The ultimate goal would be for bleeding scores to be integrated with the results of standardized laboratory testing to allow for a universal diagnostic approach to patients with suspected bleeding disorders.
Disclosures
Conflict-of-interest disclosure: The author is affiliated with an advisory board for GlaxoSmithKline. Off-label drug use: None disclosed.
Correspondence
Sarah H. O'Brien, MD, MSc, The Research Institute at Nationwide Children's Hospital, 700 Children's Dr, Suite J1401, Columbus, OH 43205; Phone: 614-722-3066; Fax: 614-722-3544; e-mail: Sarah.OBrien@nationwidechildrens.org.