Abstract
Leukemia in infants is rare but generates tremendous interest due to its aggressive clinical presentation in a uniquely vulnerable host, its poor response to current therapies, and its unique biology that is increasingly pointing the way toward novel therapeutic approaches. This review highlights the key clinical, pathologic, and epidemiologic features of infant leukemia, including the high frequency of mixed lineage leukemia (MLL) gene rearrangements. The state of the art with regard to current approaches to risk stratified treatment of infant leukemia in the major international cooperative groups is discussed. Finally, exciting recent discoveries elucidating the molecular biology of infant leukemia are reviewed and novel targeted therapeutic strategies, including FLT3 inhibition and modulation of aberrant epigenetic programs, are suggested.
Introduction
Leukemia in infants is among the most vexing clinical problems in pediatric hematology/oncology. It is so rare that even the largest pediatric leukemia centers may see only a handful of cases per year and most centers will go a year or more between cases, precluding the widespread acquisition of expertise that occurs with more common diagnoses. Infants with leukemia tend to present with aggressive clinical features that make initial management particularly challenging, and this difficulty is amplified by the vulnerability of infants to complications and toxicity of the necessary procedures and treatments. Perhaps most importantly, the eventual outcomes for infants with leukemia in terms of relapse-free survival are poor compared with leukemia in older children despite the use of maximally intensified standard therapies (chemotherapy with or without hematopoietic stem cell transplantation [HSCT]). As daunting as these challenges are, there is real promise that better days lie ahead for infants with leukemia. The fascinating and ever-expanding discoveries regarding the unique molecular biology of infant leukemia are leading to novel therapeutic strategies that have generated exciting preclinical results and are advancing to clinical trials. There is a palpable sense of hope among caregivers for infants with leukemia that the emerging era of molecularly targeted therapy will be especially beneficial for these patients. Turning this hope into reality will require close collaboration between molecular biologists and clinical trialists and among the international cooperative groups that have painstakingly established the infrastructure for the systematic treatment of these patients.
Characteristics of infant leukemia
The term “infant leukemia” generally refers to acute lymphoblastic leukemia (ALL) or acute myeloid leukemia (AML) diagnosed in a child before 1 year of age. The estimated incidence of acute leukemia in infants is 41 cases per million in the United States, which equates to ∼ 160 cases of infant leukemia per year, with ∼ 90 of the cases being ALL and 70 AML. Neuroblastoma and brain tumors occur with similar frequency as acute leukemia in the infant population. The incidence of ALL in infants is significantly lower than in children aged 1 to 14 years old and approximately the same as adolescents. In contrast, the incidence of AML in infants is approximately twice that of older children and adolescents. Interestingly, females have a higher risk of developing infant leukemia than males but a lower risk of developing leukemia beyond the first birthday.1
Compared with older children, infants with acute leukemia tend to present with more aggressive features, including high WBC counts, hepatosplenomegaly, CNS involvement, and leukemia cutis (skin infiltration).2,3 The prognostic significance of infant age differs between ALL and AML. In ALL, infants fare far worse than older children. The 4-year event free survival (EFS) in Interfant-99, the largest trial of infant ALL to date, was 47%.4 Recent trials for childhood ALL report long-term EFS rates exceeding 85%.5,6 Conversely, outcomes for infants with AML are similar to those for older children.2
A high proportion of acute leukemias occurring in infants are characterized cytogenetically by balanced chromosomal translocations involving the mixed lineage leukemia (MLL) gene at chromosome 11q23. MLL rearrangements (MLL-r) occur in ∼ 5% of childhood ALL cases overall,7 but in 70% to 80% of ALL in infants.3,4 In childhood AML, MLL-r is more common overall (15%-20%), but is also particularly common in the infant age group (∼ 50%).8
MLL-r results in the fusion of the N-terminus of the MLL gene with the C-terminus of a partner gene. Remarkably, 79 different MLL partner genes have now been identified.9 In infant ALL, 4 partner genes account for 93% of cases: AF4 (49%), ENL (22%), AF9 (17%), and AF10 (5%). In infant AML, 3 partner genes account for 66% of cases: AF9 (22%), AF10 (27%), and ELL (17%).
Various lines of evidence (eg, retrospective analyses of neonatal samples and twin concordance studies) have shown that MLL rearrangements are acquired in hematopoietic precursors in utero, and this initiates rapid progression to full blown leukemia. One intriguing aspect of leukemia epidemiology is that MLL-r leukemias occur with high frequency in 2 very different clinical situations: infants with de novo acute leukemia and patients with treatment-related secondary myelodysplastic syndrome/AML after exposure to potent DNA topoisomerase II (DNAt2) inhibitors (eg, etoposide). This has led to a hypothesis, with supporting evidence from case-control studies10,11 and laboratory studies,12 that maternal exposure to environmental DNAt2 inhibitors (eg, dietary flavonoids) during pregnancy may contribute to the risk of MLL-r infant leukemia. Germline genetic susceptibility may also play a role, because candidate gene studies13,14 and genome-wide association studies15 have identified several single nucleotide polymorphisms that are correlated with risk of infant leukemia.
In ALL, MLL-r is associated with CD10 negativity and coexpression of one or more myeloid antigens, suggesting that these leukemias arise from very immature lymphoid progenitors.16 In AML, MLL-r is associated with monocytic differentiation.2
The presence of MLL-r in infant acute leukemia has different prognostic implications in ALL than in AML. In infant ALL, MLL-r is clearly associated with poorer outcome. In the Children's Cancer Group protocol CCG-1953, the 5-year EFS for MLL-r infants was 34% compared with 60% with germline (wild-type) MLL (MLL-g).3 In Interfant-99, the 4-year EFS in MLL-r and MLL-g infants was 37% and 74%, respectively.4 Conversely, in infant AML, MLL-r is not a significant risk factor. In a combined analysis of AML-BFM-98 and AML-BFM-2004, the 5-year EFS was 43% and 52% for MLL-r and MLL-g infants, respectively (P = .59).2
Among infants with MLL-r ALL, several additional independent prognostic factors have been identified. The most important of these are age and WBC at diagnosis, with the younger infants and those with the higher WBC having poorer outcomes.3,4,17 In the context of a 7-day “prophase” of single-agent prednisone given before intensive induction chemotherapy in the Interfant-99 protocol, a poor response (≥ 1000 blasts/μL in the peripheral blood on day 8) was also an independent negative prognostic factor.4
Poor response to prednisone is significantly more common in infants than in older children with ALL, which has raised the question of whether the poor outcome for infants with leukemia may be partly due to enhanced chemoresistance. Indeed, infant MLL-r ALL cells demonstrate enhanced in vitro resistance to corticosteroids and asparaginase in assays using short-term exposure of bulk leukemia populations. Conversely, infant MLL-r AML cells do not demonstrate a more resistant phenotype.18-20 It is somewhat counterintuitive, then, that the typical pattern of failure for infant MLL-r ALL is to achieve rapid complete remission with induction chemotherapy, but then relapse during the first year of therapy. This would suggest that the poor outcomes are due primarily to the emergence of a chemoresistant population over time. The low rates of second remission reported by the Japanese Pediatric Leukemia Study Group (JPLSG) in patients relapsing after treatment for infant ALL are consistent with this hypothesis.21
Another challenging aspect of the treatment of infants with acute leukemia is the infant patient's unique vulnerability to complications and toxicities. There are several complex physiologic processes that undergo rapid changes during the first year of life and there are very limited data to guide how the distinct physiology of infants (in terms of body composition, binding of drugs by plasma proteins, cytochrome p450 activity, renal function, immunocompetence, etc) should be considered in designing chemotherapy treatment protocols. It is perhaps not surprising, then, that infant leukemia protocols have encountered problems with excessive toxicity. In the Children's Oncology Group (COG) infant ALL protocol P9407, for example, death from toxicity (primarily infectious) within the first 90 days of enrollment occurred in 25% of the first 68 patients. After the study was amended to substitute prednisone for dexamethasone, reduce the dose of daunorubicin, and enhance supportive care, the early death rate dropped to 6% for the next 141 patients.22 Remarkably, the early death rate increased again on the successor COG trial AALL0631, with 4 of the first 26 patients (15%) dying from infections, although the only change to induction therapy was to substitute a single dose of PEG asparaginase for native E coli asparaginase.23 Similar issues have been reported in infants with AML. Induction mortality on the Medical Research Council (MRC) protocols AML10 and AML12 was 12% and 3% for infants and older children, respectively.24 Survivors of infant leukemia also demonstrate an increased risk of late effects, particularly in cases in which treatment included cranial radiation or HSCT.25
Current “state of the art” for treatment of infant leukemia
Given the similar prognosis and response to therapy of infants with AML compared with older children, infants are generally treated on the same clinical trial protocols as older children, which typically include intensive multiagent chemotherapy to induce remission, followed by consolidation with either additional chemotherapy courses (for patients with favorable prognostic features) or allogeneic HSCT (for patients with unfavorable prognostic features). Cases of AML in infants are relatively unlikely to harbor cytogenetic or molecular abnormalities that confer unfavorable risk or favorable risk. Therefore, infants usually fall into the intermediate cytogenetic/molecular risk group, for which current stratification into favorable or unfavorable prognostic groups is dictated by end-induction minimal residual disease testing.
In contrast, treatment for infant ALL is quite different from that for childhood ALL generally. Currently, there are 3 major cooperative groups conducting specific clinical trials for infant ALL: Interfant (Interfant-06), COG (AALL0631), and JPLSG (MLL-10). All have adopted an identical induction strategy based on Interfant-99.4 All are using a prospective risk-stratified approach that incorporates MLL rearrangement status. Table 1 summarizes the key features of the 3 trials.
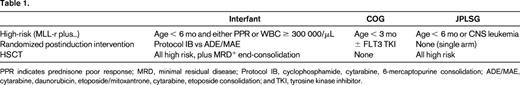
PPR indicates prednisone poor response; MRD, minimal residual disease; Protocol IB, cyclophosphamide, cytarabine, 6-mercaptopurine consolidation; ADE/MAE, cytarabine, daunorubicin, etoposide/mitoxantrone, cytarabine, etoposide consolidation; and TKI, tyrosine kinase inhibitor.
Interfant-06 is testing whether consolidation with “myeloid”-style chemotherapy with cytarabine, daunorubicin/mitoxantrone, and etoposide will prove superior to “lymphoid”-style consolidation with cyclophosphamide, cytarabine, and 6-mercaptopurine in MLL-r infants. This stems from the hypothesis that these leukemias derive from an early hematopoietic precursor with myeloid differentiation potential and may therefore respond better to chemotherapy regimens developed for AML. AALL0631 is testing whether the addition of a FLT3 tyrosine kinase inhibitor to postinduction chemotherapy will enhance the effectiveness of chemotherapy based on data showing aberrant activation of the FLT3 pathway in MLL-r ALL (detailed below). The use of HSCT varies between the groups on these trials, reflecting the controversy that exists regarding the risk/benefit ratio of HSCT in this population. Sison reviews this important topic in the accompanying evidence-based review elsewhere in this publication.
Given the similarities in treatment approach and outcomes between the groups and the rarity of infant ALL, the 3 groups are currently developing a joint collaborative protocol to standardize treatment and enhance the ability to test novel treatment approaches based on recent discoveries regarding the unique molecular biology of MLL-r leukemias detailed in the following section.
Recent biological discoveries with novel therapeutic implications
MLL-r infant ALL is characterized by a distinct global gene expression profile.26,27 A notable component of this profile is striking overexpression of FLT3.28 FLT3 signaling is constitutively activated in these cases either by activating mutations29,30 or, more commonly, by autocrine activation by coexpressed FLT3 ligand.31 Moreover, FLT3 tyrosine kinase inhibition results in selective killing of these samples and synergizes with chemotherapy in a sequence-dependent manner.30-33 FLT3 overexpression has been shown to confer especially poor prognosis in MLL-r infant ALL.34,35 As discussed above, the ongoing COG trial AALL0631 is the first to incorporate a novel, molecularly targeted agent into frontline treatment of MLL-r infant ALL. A dose that is safe in combination with intensive chemotherapy and results in sustained pharmacodynamic FLT3 inhibition has been successfully determined,36 and a randomized evaluation of efficacy is ongoing. This trial serves as proof of principle that novel targeted therapeutics can feasibly be tested in this high-risk group and has laid the groundwork for the international collaborative trial in development by Interfant, COG, and JPLSG.
Genomic single nucleotide polymorphism and sequencing studies have revealed a striking paucity of cooperating genetic alterations in infant MLL-r ALL compared with all other subsets of childhood ALL.37 Accordingly, MLL-r infant leukemia is increasingly recognized to be driven by aberrant epigenetic programs. As this complex network of interdependent epigenetic processes is elucidated, novel therapeutic strategies are emerging.
The acquisition of a reciprocal MLL translocation initiates transformation in utero by the aberrant recruitment of multiprotein complexes with chromatin-modifying activity to MLL target genes via myriad translocation partner genes, inducing dysregulated transcription of multiple genes and a highly characteristic global gene expression profile. Several studies have now established that a required component of this aberrant epigenetic state and MLL-r leukemogenesis is the H3K79 methyltransferase DOT1L.38-41 It is of particular interest, then, that potent and highly selective small-molecule inhibitors of DOT1L are in clinical development after having shown promising activity in preclinical models of MLL-r leukemia.42,43
BRD4 is one of several epigenetic “reader” proteins that binds acetylated histones and facilitates transcription downstream of MYC and other validated oncogenes. A nonbiased RNA interference screen of 243 chromatin-modifying genes identified BRD4 to be required for the maintenance of leukemia in an MLL-AF9 murine model.44 Potent and selective small-molecule inhibitors of BRD4 binding down-regulated characteristic MLL-r and MYC target genes and demonstrated in vitro and in vivo antileukemic activity by inducing apoptosis and differentiation in murine models, leukemia cell lines, and, most importantly, in a cohort of primary MLL-r infant ALL cells.44,45 A phase 1 clinical trial in adults with hematologic malignancies with a BRD2/3/4 inhibitor (OTX015) is under way and others are in development.
Complementing the widespread gene activation in MLL-r ALL is the epigenetic silencing of a specific set of genes with tumor suppressor function via promoter region CpG island hypermethylation and associated repressive histone modifications.46,47 A high level of promoter hypermethylation was correlated with inferior survival in Interfant-99.47 Demethylating agents such as decitabine and zebularine preferentially kill MLL-r lymphoblastic leukemia cells and this is correlated with the up-regulation of several of the identified silenced genes.46,47 Promoter hypermethylation and transcriptional silencing of certain microRNAs with likely tumor suppressor function also characterize infant MLL-r ALL cases.48,49 Of particular interest is hypermethylation of miR-152, which correlates with a poor prognosis in MLL-AF4+ infant ALL.48
Synergistic reexpression of epigenetically silenced genes has been demonstrated by combining CpG demethylation with reversal of repressive chromatin states. Deacetylation of histone marks such as H3K9/14 is associated with gene silencing and can be modulated with histone deacetylase (HDAC) inhibitors. Two recent applications of the connectivity map concept have identified HDAC inhibitors as capable of reversing epigenetically determined global gene expression profiles associated with chemotherapy resistance, one in relapsed childhood ALL50 and one in infant MLL-r ALL.51 These findings support the testing of demethylating agents and HDAC inhibitors as a strategy to reverse the inherent chemoresistance of MLL-r infant ALL. A pilot study of decitabine and vorinostat in combination with reinduction chemotherapy in children with relapsed ALL is under way in the Therapeutic Advances in Childhood Leukemia (TACL) consortium and will hopefully lay the groundwork for subsequent frontline trials in infant ALL.
As noted above, although the majority of infants with ALL can achieve remission, most will suffer disease recurrence with a short latency to relapse. This suggests that chemotherapy-resistant leukemia stem cells survive and can recapitulate the leukemia. Interactions between infant MLL-r ALL leukemia stem cells and the BM stromal microenvironment via the CXCR4/SDF-1 axis have been shown to mediate survival and therapeutic resistance in MLL-r ALL.52 Moreover, in xenograft models of MLL-r infant ALL, CXCR4 inhibition with plerixafor led to markedly enhanced in vivo efficacy of FLT3 inhibitors, suggesting that targeting leukemia-stroma interactions with CXCR4 inhibitors may represent a promising adjunctive therapy. Dynamic up-regulation of CXCR4 expression on the surface of acute leukemias (including MLL-r) in response to cytotoxic chemotherapy may enhance this stroma-mediated resistance and serve as a biomarker that can identify subsets of infants with leukemia for whom CXCR4 inhibition may be particularly effective.53
It is notable that most of the therapeutically relevant biological insights described above are specific to infant ALL. This reflects a relative paucity of published data suggesting that AML in infants represents a biologic entity distinct from AML in older children.
Conclusions and future directions
Infant leukemia is one of most difficult clinical situations encountered in pediatric hematology/oncology. Standard approaches with maximally intensive and toxic regimens of chemotherapy and HSCT are curative in a minority of patients. Although most treatment failures are due to relapse, treatment-related mortality and life-limiting late effects in survivors are also problematic. Recent discoveries regarding the unique biology of these leukemias are fueling the development of a pipeline of exciting novel treatment strategies that are increasingly being incorporated into clinical trials and have the potential to reduce both relapse rates and treatment-related toxicities. Increasing collaboration among the major international cooperative groups will accelerate the translation of biological understanding into better outcomes.
Disclosures
Conflict-of-interest disclosure: The author has consulted for Epizyme. Off-label drug use: decitabine and vorinostat.
Correspondence
Patrick Brown, MD, Johns Hopkins Oncology, 1650 Orleans Street, CRB1 Room 2M49, Baltimore, MD 21231; Phone: 410-955-8817; Fax: 410-955-8897; e-mail: pbrown2@jhmi.edu.
