Abstract
Although there have been significant insights into the biology of diffuse large B-cell lymphoma (DLBCL) over recent years, progress in our therapeutic approach has been disappointing over the same timeframe. This is not for want of trying. In 2017, R-CHOP (rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone) remains the “gold standard,” despite all of our insights into cell-of-origin and other subgroups. We have traditionally used clinical risk factors to tailor our therapies and have tested intensification of chemotherapy with little success. We are now in an era of testing therapies according to the molecular phenotype of the individual’s tumor. Many phase 1/2 studies have looked at adding targeted agents to conventional R-CHOP with some promise. The phase 3 data are now starting to emerge. Are we ready yet to modify our standard of care and have we reached an era of precision medicine in DLBCL? The answer to this is “not yet.” The exception is perhaps patients with the newly defined World Health Organization category of high-grade B-cell lymphoma with rearrangements of MYC and BCL2 and/or BCL6, the so-called double- and triple-hit lymphomas. In these tumors there has been a move away from R-CHOP to more intensified regimens, however, has not been based upon rigorous prospective evaluation but review of retrospective datasets. This article will review the molecular subgroups of DLBCL, interventional strategies, and the outcomes of these interventions to date.
Learning Objectives
To review controversies in the front-line therapy of diffuse large B-cell lymphoma and discuss which, if any, patients should receive tailored therapy
To understand the role of cell of origin in the prognosis of newly diagnosed patients and to examine if knowledge of this should impact upon selection of optimal therapy
To define double- and triple-hit lymphomas and the dual-expresser population of diffuse large B-cell lymphoma, and to examine optimal therapeutic approaches
Introduction
The 2016 revision of the World Health Organization classification of lymphoid neoplasms firmly recognizes the molecular heterogeneity of diffuse large B-cell lymphoma (DLBCL) that has been revealed over recent years and stresses the need to clearly identify subgroups in pathology reporting.1 The cell-of-origin (COO) classification is now formally embedded and identification of either germinal center B-cell–like (GCB) and activated B-cell–like (ABC) is required as therapeutic strategies to target subtypes are investigated. In addition, the greater understanding of c-MYC alterations in DLBCL, along with frequently associated translocations of BCL2, and to a lesser extent BCL6, has led to a new diagnostic category of high-grade B-cell lymphoma (HGBL) with rearrangements of MYC and BCL2 and/or BCL6: “the double- and triple-hit lymphomas.” Coupled with these new categorizations is the recognition of a group of DLBCLs that have dual positivity for MYC and BCL2 protein expression by immunohistochemistry (IHC), the “dual-expressers,” which lack identifiable translocations of MYC and BCL2 by fluorescence in situ hybridization (FISH). These may carry a worse prognosis and should be considered a prognostic indicator, but not a distinct entity. Furthermore, through next-generation sequencing, recurrent somatic mutations have been identified in all groups of DLBCL, some of which may carry prognostic value. Knowledge of the presence of these are likely to play a role in tailoring therapy in the future.
Despite this biological heterogeneity, R-CHOP (rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone) chemotherapy has remained the “gold standard” in the management of DLBCL for the last 15 years.2-4 Is it time for a paradigm shift from the one combination to fix all? Are we now ready to use these new biological tools and panoply of novel agents to “individualize” therapy in the first-line management of DLBCL?
This review examines how biological factors may modify our treatment approaches, rather than focusing on clinical factors, such as age, comorbidity, and extranodal sites where DLBCL may occur, such as testes, breast, bone, and the central nervous system (CNS). In these circumstances, specifically tailored approaches may be required. These have been expertly reviewed elsewhere.4-6
DLBCL biology: insights from the transcriptome
We have become familiar with the ABC/GCB COO classification of DLBCL derived from transcriptome analysis.7 Each phenotype has a set of distinct oncogenic aberrations and patterns of gene expression that are reminiscent of their COO. This is not only of biological interest, but of clinical relevance as the ABC group—in retrospective analysis—has an inferior prognosis compared with the GCB DLBCL.8 The distinct biology may be exploited as we develop new therapeutic approaches. There is a third group of DLBCL, defined by gene-expression profiling (GEP), which lack sufficient probability to classify into either the ABC or GCB group: the “unclassifiable.” This group represents 10% to 15% of cases; the underlying biology behind this group is poorly understood.
ABC DLBCLs are characterized by chronic active B-cell receptor (BCR) signaling with constitutive activation of the nuclear factor-κB (NF-κB) signaling pathway appearing central to cell survival in ABC-like lymphomas.9 These tumors rely upon the CARD11/MALT1/BCL10 signaling complex to activate the central kinase in the NF-κB pathway, IκB kinase.10,11 More than half of ABC DLBCL carry somatic mutations in multiple genes, including negative (A20) and positive (CARD11, TRAF2, TRAF5, MAP3K7, and TNFRSF11A) regulators of NF-κB.12 Of these, the A20 gene, which encodes a ubiquitin-modifying enzyme involved in termination of NF-κB responses, is most commonly affected, with one-third of patients displaying biallelic inactivation by mutations or deletions. In addition, 29% of ABC DLBCL tumors, harbor activating mutations in the MYD88 adaptor protein, which mediates Toll and Interleukin-1 (IL-1) receptor signaling.13 The mutation promotes cell survival by spontaneously assembling a protein complex containing IL-1 receptor-associated kinase 1 (IRAK1) and IRAK4, leading to IRAK4 kinase activity, IRAK1 phosphorylation, NF-κB signaling, JAK kinase activation of STAT3, and secretion of IL-6, IL-10, and interferon-β.
In contrast, the GCB group are somewhat more heterogeneous and are characterized by evidence of ongoing somatic hypermutation, expression of CD10, and recurrent mutations in the epigenetic regulator EZH2.14 The latter is an emerging target for therapeutic intervention.15 EZH2 encodes the H3K27 methyltransferase gene and is mutated in 24% of GCB DLBCL cases, and may drive GCB DLBCL by proliferation and by impeding plasmacytic differentiation. Translocations of BCL2, amplifications of REL, and loss of phosphatase and tensin homolog deleted on chromosome 10 (PTEN), resulting in activation of the phosphatidylinositol 3-kinase (PIK3)/AKT/mammalian target of rapamycin (mTOR) pathway,16 are more common in the GCB group.17
As technologies have evolved, simplified platforms for determination of COO classification of DLBCL from formalin-fixed paraffin-embedded tissue have been validated. These include the Lymph2Cx assay18 and HTG EdgeSeq DLBCL COO assay.19 As yet, clinical access to these tools remains limited, but it is likely that in the not too distant future these will be more widely accessible to diagnostic laboratories providing rapid turnaround COO classification.
Attempts have been made to simplify molecular subclassification of DLBCL by IHC methodologies.20,21 Although these have the attraction of being readily applied to routine diagnostic material, there is a major problem of poor reproducibility between laboratories and pathologists, even when expert hematopathologists are reporting, with a lack of concordance using semiquantitative techniques.22 The Hans algorithm,23 based upon CD10, interferon regulatory factor 4 (IRF4), and BCL6 expression is most commonly employed. This results in dichotomous categorization into GCB and non-GCB subgroups, although it fails to identify those “unclassifiable” tumors that represent 10% to 15% of DLBCL by transcriptome analysis. When surveying the literature, the reader needs to be cognizant of the limitations of this IHC binary classification.
Beyond COO, transcriptome analysis has revealed other subgroups of DLBCL. These include clusters of DLBCLs that have dominant expression of oxidative phosphorylation genes, BCR/proliferation genes, and host-response genes.23 These subgroups have yet to be best exploited clinically to define groups of patients for investigation of novel agents; however, they appear to be increasingly relevant as we explore novel agents in DLBCL.
Are we likely to see improvements from refinement of conventional chemotherapy?
Probably no. In the pre-rituximab era, intensified second- and third-generation CHOP-like chemotherapy regimens, which were promising in the phase 2 setting, showed no advantage over conventional CHOP.24 Attempts at increasing dose-density by delivering R-CHOP on a 14-day schedule, compared with the usual 21-day schedule, demonstrated no difference in outcomes in 2 large phase 3 studies.25,26 There were no clinical or biological subgroups identified in which the accelerated schedule provided benefit, although R-CHOP-14 may provide an option for patients who may wish to have therapy completed over a shorter period.
We have seen from a number of studies and a meta-analysis that high-dose chemotherapy with peripheral blood stem cell rescue does not have clear value in the consolidation of first remission of DLCBL.27 These studies were largely conducted in the pre-rituximab era. The South West Oncology Group study, in which half the patients had R-CHOP induction, did demonstrate a progression-free survival (PFS) advantage in favor of high-dose chemotherapy consolidation for those patients with a high or high-intermediate International Prognostic Index (IPI), although this did not translate into an overall survival (OS) advantage and so has not widely changed practice.28
The French Groupe d’Etude des Lymphomes de l’Adulte have championed the use of the R-ACVBP (rituximab, doxorubicin, cyclophosphamide, vindesine, bleomycin, and prednisone) regimen in younger patients (age <59 years) with an age-adjusted IPI of 1. This approach, which also included the intensified delivery of intravenous methotrexate, ifosfamide, etoposide, and cytarabine, showed superiority to R-CHOP with a 3-year OS of 92% compared with 84%.29 Although it has been encouraging to see a positive study, acceptance of the regimen has been limited because of increased hematological toxicity and hospital inpatient stays, along with the limited wider availability of vindesine. Additionally, some have argued that the R-CHOP control arm performed less well in the same IPI risk groups than has been observed in other studies.30 In a retrospective analysis, tumors were evaluated by the Hans algorithm. Non-GCB tumors predicted a worse PFS [hazard ratio (HR), 3.21; 95% confidence interval (CI), 1.29 to 8.00; P = .01] and OS (HR, 6.09; 95% CI, 1.37 to 27.03; P = .02) among patients treated with R-CHOP compared with patients who received R-ACVBP, whereas there were no significant survival differences between these regimens among patients with GCB tumor. This finding indicates that much of the OS benefit associated with the R-ACVBP regimen was associated with improved outcomes in the non-GCB subgroup.
What about DA-EPOCH-R? Should we switch?
No. Impressive results in the phase 2 setting have been achieved with the DA-EPOCH-R (etoposide + prednisone + vincristine + cyclophosphamide + doxorubicin + rituximab) infusonal chemotherapy regimen.31 Etoposide, vincristine, and doxorubicin are given as a 96-hour infusion with bolus cyclophosphamide, along with usual rituximab and oral prednisolone. Dosing in each successive cycle is up- or down-titrated based upon the pharmacodynamic endpoint of nadir blood counts. The Cancer and Leukemia Group B (CALGB) conducted a study to determine reproducibility in a multi-institutional setting.32 With a median follow up of 62 months, time to progression and OS were 81% and 84%, respectively, and time to progression was 87%, 92%, and 54% for low/low-intermediate, high-intermediate, and high IPI risk groups, respectively, at 5 years and beyond. The time to progression and event-free survival (EFS) of GCB were 100% and 94%, respectively, and non-GCB were 67% and 58%, respectively, at 62 months.
Based upon these promising results, the CALGB/Alliance Group conducted a phase 3 study comparing DA-EPOCH-R to R-CHOP, each for 6 cycles.33 In this study, 524 patients were enrolled, of which 465 were eligible. There was no difference in overall-response rates or complete-response rates, and no difference in the primary endpoint of EFS [HR = 1.14 (0.82-1.61) P = .4386] at a median follow-up of 5 years. Three-year EFS was 81% for R-CHOP vs 79% for DA-EPOCH-R. OS was not significantly different [HR = 1.18 (0.79-1.77) P = .42] between regimens (R-CHOP 85% vs DA-EPOCH-R 85% at 3 years). There was no clinical subgroup identified based on age or IPI that appeared to benefit from DA-EPOCH-R; hematological toxicity was not unsurprisingly greater, as this was the pharmacodynamics endpoint for dose adjustment. The study undertook multiple correlative translational research; however, none has been presented to date. From this, we must conclude there is no advantage to be had from the use of DA-EPOCH-R in DLBCL over conventional R-CHOP.
Is there a role for next-generation anti-CD20 antibodies in front-line therapy?
No. Obinutuzumab (GA101; G) is a glycoengineered type II humanized anti-CD20 monoclonal antibody with a different mechanism of action to rituximab. It exhibits lower complement-dependent cytotoxicity, but greater antibody-dependent cellular cytotoxicity, phagocytosis, and greater direct B-cell killing. The antitumor activity of obinutuzumab combined with chemotherapy has been demonstrated in patients with chronic lymphocytic leukemia and follicular lymphoma, in both cases demonstrating superior outcomes to rituximab-based therapy.34,35 In DLBCL, the GATHER phase 2 study of G-CHOP demonstrated the safety and high response rates for the combination.36 Results from the phase 4 GOYA study has, however, shown no benefit from the use of G-CHOP over R-CHOP in front-line DLBCL.37 The study was a 1:1 randomization of 6 or 8 cycles of each regimen, recruiting 1400 patients with an IPI ≥ 2, or an IPI of 1 not due to age alone, or an IPI of 0 with bulky disease (1 lesion >7.5 cm). There was no difference in complete or overall response rates (ORR) determined by either conventional computed tomography criteria or positron emission tomography (PET) and no difference in the primary endpoint of PFS. With a median follow-up of 29 months at the time of reporting, 3-year PFS was 66.9% for R-CHOP and 68.6% for G-CHOP [HR (95% CI) = 0.92 (0.76-1.11 P =.3888]. There was no difference in OS.
Despite there being no overall benefit from the use of obinutuzumab with CHOP, this study has provided one of the largest prospective evaluations of the COO model (employing the Nanostring Lymph2Cx technology), demonstrating the inferior outcomes of the ABC phenotype, with 3-year PFS in the ABC, GCB, and unclassified groups of 59.3%, 75.0%, and 63.2%, respectively. None of the molecular subgroups demonstrated any significant benefit from the use of G-CHOP over R-CHOP, although there is a perhaps a hint that in the GCB patients there may be a trend toward benefit from the use of obinutuzumab with 3-year PFS of 71% in the R-CHOP arm and 79% in the G-CHOP arm [HR (95% CI) = 0.72 (0.50-1.01)]. This is of course an underpowered subgroup analysis, but it appears that in further exploratory work, those with the strongest confidence of GCB phenotype have the greatest benefit from obinutuzumab. Toxicity was greater in the G-CHOP–treated patients, particularly in infections and infusion-related reactions, leaving R-CHOP as the standard of care.
Ofatumumab is a human IgG1k anti-CD20 monoclonal antibody targeting a distinct epitope to rituximab. The ORCHARRD study (Ofatumumab versus Rituximab salvage Chemoimmunotherapy in Relapsed or Refractory Diffuse large B-cell lymphoma) examined ofatumumab in combination with second-line chemotherapy in transplant-eligible patients with relapsed or refractory DLBCL.38 There was no difference in response rates, number of patients proceeding to high-dose therapy, PFS, or OS compared with rituximab-based salvage regimens. Although not tested in the front-line setting in a randomized study, extrapolation of the data from the ORCHARRD study would indicate no role ofatumumab up-front in the management of DLBCL.
Can we improve outcomes by targeting the NF-κB pathway? This might help our ABC patients
No, not yet. As stated above, the ABC phenotype of DLBCL demonstrates constitutive activation of the NF-κB pathway, through a number of mechanisms. Proteosome inhibitors, such as bortezomib, may prevent the degradation of IκB kinase and maintain NF-κB in its inactive state. Results from a small proof-of-concept study in relapsed DLBCL showed that when bortezomib was added to DA-EPOCH-R, a differential benefit between ABC and GCB could be documented.39 In the front-line setting, a phase 2 study showed that it could safely be administered with R-CHOP, with acceptable levels of peripheral neuropathy, and that it might improve the outcome of the non-GCB patients, compared with historical controls.40 In prospective evaluation, this promise has not been fulfilled. In the randomized phase 2 Personalized Lymphoma Therapy: Randomized Study of Proteasome Inhibition in Non-GCB DLBCL (PYRAMID) study, patients were confirmed by a central laboratory to have non-GCB DLBCL and then randomized between R-CHOP and R-CHOP with bortezomib.41 The primary endpoint was PFS; there was no demonstrated efficacy advantage with the addition of bortezomib. Interestingly, the R-CHOP–treated arm had a lower event rate than expected for non-GCB patients. In this, it may not have just been that bortezomib lacked efficacy or that the use of IHC may have misclassified the COO, but because central review was required, and the less sick patients may not have been recruited because they required immediate initiation of therapy.
Mitigating this potential confounder, the United Kingdom National Cancer Research Institute and Swiss SAKK (Swiss Group for Clinical Cancer Research) phase 3 REMoDL-B study took patients with DLBCL in need of 6 cycles of R-CHOP (stage IB or IAX-IV) and commenced a first cycle of R-CHOP chemotherapy42 (Figure 1). At the same time their formalin-fixed paraffin-embedded diagnostic material was sent for central real-time GEP, using the Illumina DASL array technology to determine COO. At the time of the second cycle, patients were randomized between R-CHOP and R-CHOP with the addition of bortezomib for 5 cycles and stratified according to the COO. Whereas proceeding to the first cycle of R-CHOP without additional agents may reduce dose intensity, it allows time for the prospective biomarker work without excluding the sicker patients and may reduce early toxicity of combinations, given that there are typically more adverse events in the first cycle of R-CHOP therapy. REMoDL-B was skeptical about the benefit of bortezomib in any particular COO subgroup, and so all patients with a successful GEP were randomized. Of 1076 patients, a GEP was not obtained in only 158 patients. The vast majority of these results were because there was insufficient material in the submitted blocks and in only 25 cases were there technical problems with the assay. The median turnaround was 10 days from study entry to availability of GEP results; the major factor in this timeline was release of blocks from sites and posting to the central laboratory. Forty-eight percent of patients had a high or high-intermediate IPI, suggesting that the study was not selecting better-risk patients through the use of the immediate first R-CHOP cycle. There was no difference in the primary endpoint of PFS between those patients treated with R-CHOP or R-CHOP + bortezomib (30-month PFS 70.1% and 74.3%, respectively, HR 0.841; P = .252). There was no differential activity of R-CHOP + bortezomib in any of the COO subgroups, although those patients with an ABC phenotype and low IPI derived benefit. Further exploration of the biological basis of these observations is on-going. Although there may be other agents in development that have enhanced activity against dysregulated NF-κB, for the present there is no indication that we should modify our approach.
REMoDL-B.42 (A) Study schema. Patients initiated a first cycle of R-CHOP while the molecular work-up was performed, thus not selecting for patients with less-aggressive phenotypes. The novel agent, bortezomib, was only introduced at the second cycle in randomized patients. (B) PFS by molecular phenotype. Percentages are 30-month PFS. Unc, unclassifiable.
REMoDL-B.42 (A) Study schema. Patients initiated a first cycle of R-CHOP while the molecular work-up was performed, thus not selecting for patients with less-aggressive phenotypes. The novel agent, bortezomib, was only introduced at the second cycle in randomized patients. (B) PFS by molecular phenotype. Percentages are 30-month PFS. Unc, unclassifiable.
If not NF-κB, how about targeting constitutively activated BCR signaling in ABCs?
Not yet! Dysregulation of B-cell signaling is a feature of the ABC phenotype of DLBCL.43 Ibrutinib, a first-generation oral, small-molecule Bruton tyrosine kinase (BTK) inhibitor, binds covalently to a cysteine residue at position 481 in the ATP binding pocket of BTK. Although highly potent in inhibiting BTK, ibrutinib has also shown in vitro activity against other kinases with a cysteine in the same position, and may account for some observed toxicity. A small proof-of-concept study in relapsed and refractory DLBCL has already demonstrated that inhibition of BTK by ibrutinib has clear activity in ABC DLBCL, but little apparent benefit in the GCB subtype.44 Ibrutinib produced complete or partial responses in 37% (14 of 38) of those with ABC DLBCL, but in only 5% (1 of 20) of subjects with GCB DLBCL (P = .0106). ABC tumors with BCR mutations responded to ibrutinib frequently (5 of 9; 55.5%), especially those with MYD88 mutations (4 of 5; 80%); however, the highest number of responses occurred in ABC tumors that lacked BCR mutations (9 of 29; 31%). More recently, a phase 1b trial has shown that ibrutinib may be given safely with R-CHOP.45 Although numbers were small, in those patients subtyped for COO and treated at the recommended phase 2 dose 5 (71%) of 7 patients with the GCB subtype and 2 (100%) patients with the non-GCB subtype had a complete response (CR).
These observations have formed the basis for a randomized phase 3 study, PHOENIX, comparing R-CHOP to R-CHOP with ibrutinib in non-GCB DLBCL (NCT01855750). Recruitment is complete and maturation of the study for the primary endpoint of EFS is awaited. This study requires central review of IHC COO before randomization, and may therefore preclude the sickest of patients. So for the moment, in the absence of phase 3 evidence, there is no role for the addition of ibrutinib to R-CHOP in our ABC patients. Early investigation of a second-generation BTK inhibitor, acalabrutinib, with R-CHOP is ongoing (Eudract 2015-003213-18). Acalabrutinib has increased BTK selectivity and less off-target kinase activity, so toxicity may be reduced and efficacy enhanced.
Other targets in BCR signaling have been investigated in DLBCL. In a study of the SYK inhibitor, fostamatinib, in relapsed or refractory DLBCL, activity was low (ORR: 3%), and no responses were seen in ABC patients.46 However, other SYK inhibitors are currently under investigation in this setting.
What about employing an immunomodulatory agent in combination with R-CHOP?
No…again, not yet. The immunomodulatory lenalidomide has multiple antineoplastic effects, including direct inhibition of tumor proliferation and angiogenesis along with stimulation of cytotoxicity medicated by T and natural killer (NK) cells.47 Cereblon, a ubiquitously expressed E3 ubiquitin ligase, is activated upon lenalidomide binding and appears to be the most-important molecular target. Activated cereblon binds to the B- and T-cell transcriptional regulators Ikaros and Aiolos, resulting in their ubiquitination and degradation. In ABC DLBCL, lenalidomide results in downregulation of IRF4 and subsequently BCR-dependent NF-κB activity. These preclinical observations are supported by the observed differential activity of lenalidomide in relapsed/refractory DLBCL. In a retrospect analysis, the reported response rate in non-GCB tumors was 53%, compared with just 9% in GCB DLBCL (total study size, n = 40).48 Prospectively, lenalidomide has been compared with investigator choice in the relapsed/refractory population, and this observation has been confirmed.49 The former demonstrated superior response rates over investigator choice, with greater improvements in PFS in non-GCB patients (15.1 weeks vs 7.1 weeks, respectively; P = .021) compared with GCB (10.1 weeks vs 9.0 weeks, respectively; P = .550). Of note, exploratory analyses suggest the preferential benefit was more pronounced in the GEP-defined ABC population, rather than by IHC.
Progressing these observations forward, lenalidomide has been safely combined with R-CHOP chemotherapy in 2 front-line DLBCL phase 2 studies (R2-CHOP).50,51 In the study reported by Nowakowski et al,51 the results achieved with R2-CHOP were compared with outcomes from R-CHOP–treated historical controls. In R-CHOP patients, 24-month PFS and OS were 28% vs 64% (P < .001) and 46% vs 78% (P < .001) in non-GCB DLBCL vs GCB DLBCL, respectively. In contrast, there was no difference in 24-month PFS or OS for R2-CHOP patients on the basis of non-GCB and GCB subtype [60% vs 59% (P = .83) and 83% vs 75% (P = .61) at 2 years, respectively], concluding that the addition of lenalidomide appears to mitigate the negative impact of non-GCB phenotype on patient outcome. There are now 2 studies further examining differential outcomes, both employing GEP to define true ABC patients. The ROBUST study (NCT02285062) is a randomized, double-blind, global, phase 3 study of oral lenalidomide (15 mg, days 1-14) plus R-CHOP-21 × 6 vs placebo–R-CHOP-21 × 6 in patients with ABC DLBCL, with PFS as the primary endpoint. Molecular subtyping, from formalin-fixed paraffin-embedding, is required prior to randomization and is performed centrally within 3 days of receipt of samples, although, as demonstrated with the REMoDL-B study, the rate-limiting factor may be time-to-delivery of samples and adequate material in the tumor block, once again raising the possibility of bias in patient selection. A United States intergroup randomized phase 2 study is also ongoing, recruiting all patients with stage II-IV DLBCL, but powered to deliver sufficient numbers of ABC-type patients (NCT01856192).
Or an immunodulatory agent as maintenance therapy?
Possibly… if the economics stack up in the nonfit elderly. Attempts at maintenance therapies, upon completion of R-CHOP, have been a story of failure. Enzastaurin, a protein kinase Cβ given for 3 years, showed no benefit over placebo,52 as did a study of 1 year of the mTOR inhibitor everolimus.53 Similarly, rituximab maintenance has shown no benefit.54 Recently, however, positive results from the large REMARC phase 3 study have been reported from The Lymphoma Study Association (LYSA) group demonstrating a benefit from lenalidomide maintenance55 (Figure 2). Older patients, aged 60 to 80 years, with age-adjusted IPI (aaIPI) ≥ 1 and stage II to IV disease, were randomized to either 24 months of lenalidomide 25 mg/day for 21 days on a 28-day cycle or placebo, having a achieved a complete or partial response to R-CHOP. Six hundred fifty patients were randomized and at a median follow-up of 39 months, the HR was 0.708 (95% CI 0.537 to 0.922; P = .0135) in favor of lenalidomide, with a 2-year PFS improving from 75% in the placebo arm to 80% in the lenalidomide arm. This benefit was seen in all subgroups, with particular benefit demonstrated in those who were PET-positive at randomization, compared with those who were PET-negative. There was no difference in overall survival. Many patients did not tolerate therapy well and a large number of patients (36%) discontinued experimental therapy because of treatment toxicity; 72% required a dose reduction. Contrary to perceptions of lenalidomide being an ABC targeted drug, using the Hans criteria, the GCB showed a significant difference from the addition of lenalidomide (median PFS, 61 months vs 53 months in placebo; HR 0.491, P = .04), while no difference was shown in the non-GCB group (HR 1.081, P = .75). When COO was defined in a subset of patients (n = 318) by expression profiling using NanoString technology, there was no differential effect by molecular subgroups. It is unclear why the PFS advantage did not translate into an OS advantage. It was not because of excess toxic deaths in the experimental arm. It may well be that these patients have inferior responses or tolerate subsequent therapies less well at progression.
PFS (A) and OS (B) in elderly patients in first remission of DLBCL randomized to either lenalidomide or placebo maintenance. Results from the REMARC study. Reprinted from Thieblemont et al55 with permission.
PFS (A) and OS (B) in elderly patients in first remission of DLBCL randomized to either lenalidomide or placebo maintenance. Results from the REMARC study. Reprinted from Thieblemont et al55 with permission.
Fifty-five percent of the study population were aged <70 years and approximately 70% of the whole population had a Cumulative Illness Rating Scale score of ≤6. It is likely that many of the younger, fitter patients who were PET-positive at the end of therapy would have been best served by biopsy confirmation of persistent disease and then noncross-resistant chemotherapy consolidated by high-dose chemotherapy, with stem cell rescue. This is readily achievable in many of this patient group, given the increasing fitness of this younger elderly population. Thus, it would seem that the best candidates for this approach are the truly elderly that are PET-positive at the end of induction R-CHOP, and who would not be fit for intensified therapies. The selection of subgroup upon subgroup is unlikely, however, to stack up with funders in many territories.
Nothing so far about the GCB group. Should we be tailoring therapy?
No. There has been much less focus on therapeutic targets in the GCB phenotype. In part, this is because of the better outcomes observed in this group, but also because there is more marked biological heterogeneity compared with the unifying pathways of dysregulation seen in the ABC group. Oncogenic mutations in the epigenetic regulator, EZH2, are observed in 22% of GCB DLBCL and are absent in the ABC phenotype.56 An orally active inhibitor of EZH2, tazemetostat, is in clinical development and has shown some encouraging early results in the relapsed/refractory DLBCL.15,57 The LYSA group is currently preforming a phase 1b/2 Study of tazemetostat in combination with R-CHOP in newly diagnosed patients with DLBCL, and with an aaIPI ≥2 (NCT02889523).
Loss of PTEN is detected in 55% of GCB DLBCLs, through a number of mechanisms, including heterozygous deletions of the PTEN locus in 10% of cases, whereas this abnormality is infrequent (14%) in ABCs.16 The result of PTEN loss is activation of the PI3K/AKT/mTOR pathway and oncogenic addiction to the pathway. The clinical activity of PI3K inhibitors in DLBCL has, however, been disappointing, although recently some interesting data have been reported on the activity of copanlisib, a pan-class I PI3K inhibitor in relapsed and refractory DLBCL.58 With molecularly determined cells, the ORR in GCB patients was 14%, and 38% in those of ABC phenotype. The mTOR inhibitor everolimus has been tested in combination with R-CHOP in a phase 1/feasibility study.59 All 24 evaluable patients responded, with 96% demonstrating a complete metabolic response, and all were event free at 12 months. This promising activity contrasts to that seen in the PILLAR2 trial, where everolimus had no benefit in maintenance after R-CHOP53
The checkpoint inhibitors are successful in solid malignancies. What about in DLBCL?
No. The cytotoxic T-lymphocyte coreceptor programmed cell death protein 1 (PD-1) has been extensively studied and is recognized to provide critical inhibitory signals that downregulate T-cell function and provides a mechanism for immune evasion for tumors. This has become a major target for monoclonal antibody therapy in oncology, with durable response observed in a number of solid malignancies. PD-L1, the ligand of PD-1, is expressed on DLBCL tumor cells, along with infiltrating nonmalignant cells, primarily macrophages,60,61 with PD-1 expressed on tumor-infiltrating lymphocytes. The presence of large numbers of PD-1+ tumor-infiltrating lymphocytes has been associated with favorable OS in DLBCL,62,63 while high-levels of circulating PD-L1 in the plasma associated with poor OS in DLBCL.64 The PD-1/PD-L1 axis is thus likely to contribute to DLBCL survival, and manipulation of the interaction would be an appropriate therapeutic target. In a double-staining IHC study of 1253 DLBCL samples, PD-L1 positivity was defined as expression on 30% of malignant cells and was determined as positive in 11% of cases.65 Previous reports have cited PD-L1 expression as between 20% and 75%,61,64,66 but different cut points have been used to define positivity. High PD-L1 expression in the nonmalignant cells (20% cut-off) of the microenvironment (mPD-L1+) was positive in an additional 15% of cases that were PD-L1−.65 There was a significant association with the non-GCB phenotype of DLBCL and the presence of Epstein-Barr virus-positivity. In a subgroup analysis of 273 patients, where all clinical information was available and who had been treated with R-CHOP chemotherapy, PD-L1+ DLBCL was associated with a high IPI, B symptoms, and non-GCB phenotype, as was found in mPD-L1+ patients. PD-L1+ DLBCL patients had an inferior OS compared with PD-L1− patients.
Recently, new molecular insights have arisen in the mechanism of PD-1 expression in DLBCL.67 Using whole-genome sequencing analysis, the PD-L1/PD-L2 locus was been identified as a recurrent translocation partner for IGH in DLBCL. PIM1 and TP63 were also identified as novel translocation partners for PD-L1/PD-L2. Additionally, in this study a subset of samples were found to be affected by gains (12%), amplifications (3%), and translocations (4%) of the PD-L1/PD-L2 locus. Cytogenetic alterations affecting the PD-L1/PD-L2 locus were more frequently observed in the non-GCB subtype of DLBCL. These findings would further support treatments targeting the PD-1/PD-L1 axis in patients with DLBCL and proof-of-principle studies of checkpoint blockade therapy in hematological malignancies, which have included patients with DLBCL. A phase 1 study of nivolumab, a fully humanized IgG4 monoclonal antibody that targets PD-1, included 11 patients with relapsed or refractory DLBCL.68 The ORR was 36%, with 2 patients achieving CR in this population. A pilot study is underway of pembrolizumab, also a humanized Ig4 targeting PD-1, in combination with R-CHOP (NCT02541565), but we are still far from being able to use this combination outside of the trial setting.
How about CD30 then?
No. The expression of CD30 in DLBCL is variable (14%-25%) and depends much upon the cut-off value employed. Objective responses (44%) have been seen when brentuximab vedotin, the antibody-drug conjugate is used as a single agent in the relapsed and refractory setting.69 An ongoing phase 2 study has used brentuximab in combination with R-CHOP, and also with the omission of vincristine to reduce neurotoxicity.70 The study is restricted to high/high-intermediate patients and presents some promising data in a small number of patients. Correlation with the percentage of CD30 expression is ongoing.
HGBL with rearrangements of MYC and BCL2 and/or BCL6 (HGBL-DH). Help!
The inclusion of HGBL with rearrangements of MYC and BCL2 or BCL6, the double- and triple-hits, in the revision of the World Health Organization classification provides us with both some diagnostic and significant clinical challenges. These patients frequently present with high-risk clinical features, including high-stage (stage IV, 65%), B-symptoms (44%), a lactate dehydrogenase >3 [the upper limit of normal (33%)], raised white cell count, and CNS involvement at diagnosis (10%).71 There is little doubt that most of these patients have a poor outcome with R-CHOP,71-73 yet the true value of dose-intensified approaches have yet to be prospectively tested in a randomized fashion. This may be impossible to very clearly answer and we will have to rely, for now, on retrospective data.
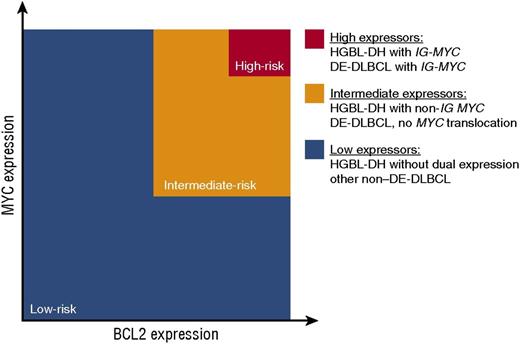
MYC dysregulation leads to promotion of cellular proliferation, genomic instability, and an amplifier of transcription. In HGBL-double hit (DH), MYC is translocated to an immunoglobulin gene (IG) partner or a non-IG partner. In the former, constitutive activity of the IG promoter leads to high levels of expression; in the latter case the mechanism is less clear and the quantity of MYC mRNA may be less.74 A coexistent BCL2 translocation results in overexpression of BCL2, rendering the cell resistant to apoptosis. These cells have a GCB phenotype. Sixty-percent of HGBL will have dual MYC and BCL2 translocations, 20% MYC and BCL6, and an additional 20% will have translocations involving all 3 genes (the triple hits)75 (Figure 3).
Model assessing clinical risk according to MYC and BCL2 Status in DLBCL. The risk of treatment failure is proportional to the degree of MYC and BCL2 expression. The 5% of patients with the poorest outcome are shown in red and have the highest level of MYC and BCL expression as a result of translocation immunoglobulin loci. Reprinted from Sesques and Johnson75 with permission.
Model assessing clinical risk according to MYC and BCL2 Status in DLBCL. The risk of treatment failure is proportional to the degree of MYC and BCL2 expression. The 5% of patients with the poorest outcome are shown in red and have the highest level of MYC and BCL expression as a result of translocation immunoglobulin loci. Reprinted from Sesques and Johnson75 with permission.
Given that intensified therapies may play a role in the management of these patients, identification is critical, and thus an increase in FISH testing has become necessary. This comes with economic implications. In the United Kingdom, the cost of FISH analysis is approximately US$480 per case. Applied to all new cases of DLBCL, the annual increase in spending to identify the ∼5% to 10% of cases that will be HGBL is not insignificant. A pragmatic approach is to routinely screen for MYC and BCL2 expression by IHC, and undertake FISH in those patients that have high-expression of both and are of the GCB phenotype. Of course, this approach does miss the HGBL-DH with MYC and BCL6 translocations. It is uncertain how significant is the failure to identify these patients.
Dose-intensification may play role in the management of these patients, although the data we have are based upon retrospective analysis. In a multi-institutional series, DA-EPOCH-R resulted in significantly higher CR rates compared with R-CHOP, or R-CODOX-M/R-IVAC (rituximab, cyclophosphamide, vincristine, doxorubicin, methotrexate/ifosfamide, etoposide cytarabine).71 PFS was greater for those receiving any one of 3 intensified regimens [R-DA-EPOCH, R-HyperCVAD (rituximab, cyclophosphamide, vincristine, doxorubicin, dexamethasone/methotrexate, cytarabine), and R-CODOX-M/R-IVAC] compared with R-CHOP (median PFS 21.6 months compared with 7.8 months; P = .001) and indeed, each regimen alone was superior for PFS against R-CHOP, but none championed the other. There was, however, no difference in OS between the regimens. Stem cell transplant in first remission did not improve OS.
From the MD Andersen Cancer Center, the CR rate was 40% following R-CHOP compared with 68% for DA-EPOCH and R-HyperCVAD, with a significantly improved EFS in the intensified therapies.72 In a meta-analysis of 394 double-hit patients, from 11 studies, first-line therapy with DA-EPOCH-R significantly reduced the risk of progression, but again had no survival advantage.76 There was also a nonsignificant trend toward longer PFS using other dose-intensified regimens. Many have adopted DA-EPOCH-R for these patients, given these finding and relatively modest toxicity compared with the other dose-intensified regimens.
How does this sit with the results of the CALGB/Alliance 50303 study showing no advantage to DA-EPOCH-R in a large phase 3 study?33 We do not as yet have the analysis based on molecular subgroups, but the number of double and triple hits will be low, just a small subgroup of the study, and certainly will not be able to answer this question, so we continue to make our decisions on a relatively poor evidence base.
Given the high-rate of CNS events in this group, attention should be paid to CNS prophylaxis in all patients and indeed attention to CNS prophylaxis has been associated with lower CNS events72 and a trend toward superior OS.71 All patients with double-hit lymphoma should have their CNS examined at baseline, and thereafter CNS-directed prophylaxis should be tailored to risk and the use of intensive regimens that contain agents that penetrated into the CNS.
To consolidate or not with high-dose chemotherapy with stem-cell rescue in CR1? In a landmark analysis of 159 patients achieving CR1, consolidative high-dose chemotherapy with peripheral blood progenitor cell rescue was not associated with improvement in relapse-free or OS77 (Figure 4). Patients treated with R-CHOP and consolidated with high-dose therapy, however, had a similar outcome to those treated with intensified regimens. This finding would support a role for high-dose therapy after R-CHOP, but given that it is an inferior route to induction, it does not present the optimal path to best outcomes. My preference is to use DA-EPOCH-R in these patients, although intensification does rely upon patient fitness and many of the patients are older.
(A) Relapse-free survival by front-line regimen in those patients with double-hit lymphoma who achieve a first CR by induction regimen. (B) Relapse-free survival by front-line regimen and in receipt of an autologous stem-cell transplant. Reprinted from Landsburg et al77 with permission.
(A) Relapse-free survival by front-line regimen in those patients with double-hit lymphoma who achieve a first CR by induction regimen. (B) Relapse-free survival by front-line regimen and in receipt of an autologous stem-cell transplant. Reprinted from Landsburg et al77 with permission.
Dual-expressers. Do I need to do something different?
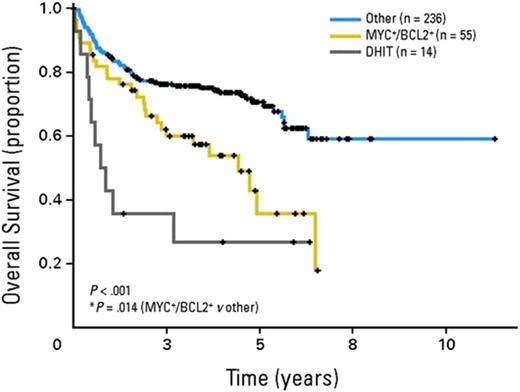
No. Dual-expressers describes a group of DLBCL(NOS) that has high IHC expression of both MYC and BCL2 protein, but lack identifiable translocations. These belong predominantly to the ABC phenotype and the mechanism of increased protein expression is largely through constitutive NF-κB activation.78 Dual expressors may occur in the GCB population and probably results from other genomic lesions, such as amplifications. They represent about 25% of DLBCL patients and in multiple series have been shown to be associated with inferior outcomes to R-CHOP73,79-81 (Figure 5). Unlike HGBL, these tumors do not represent their own diagnostic category, but the presence of double expression of these proteins should be considered a biomarker for poor prognosis. As yet, there are no results from interventional studies focused on this population, but they are a high priority for clinical investigation.
OS of patients with diffuse large B-cell lymphoma treated with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone according to the presence of concurrent expression of MYC and BCL2 proteins (MYC+/BCL2+) or the presence of concurrent MYC and BCL2 translocations. Reprinted from Johnson et al73 with permission.
OS of patients with diffuse large B-cell lymphoma treated with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone according to the presence of concurrent expression of MYC and BCL2 proteins (MYC+/BCL2+) or the presence of concurrent MYC and BCL2 translocations. Reprinted from Johnson et al73 with permission.
Targeting BCL2 in this population is biologically sound. The BH3 mimetic venetoclax may present a potential interventional approach, although data are still very early. As a single agent in relapsed/refractory DLBCL, activity is modest (ORR 18%) and the correlation with BCL2 positivity unknown.82 Venetoclax in combination with either rituximab or obinutuzumab and CHOP is currently being investigated in a phase 1b/2 trial of previously treated patients. This is a dose-finding study, but 6 of 8 dual-expressor patients achieved a PET CR.83 BCL2 abundance is not unique to the GCB phenotype. Approximately 60% of ABC DLBCLs exhibit high levels of BCL2.79 This is typically a result of amplifications or through aberrations in NF-κB signaling.84 The response to inhibition of BCL2 in DLBCL may well therefore turn out to be independent of COO.
Prophylaxis against secondary CNS involvement
A detailed discussion on the risk and treatment approach to the prevention of secondary CNS involvement is beyond the scope of this review. In non-MYC rearranged DLBCL, the CNS-IPI is a useful clinical tool to predict the risk for CNS relapse in patients with DLBCL.85 This tool was developed to identify the components of the traditional IPI score, as well as kidney or adrenal involvement as factors associated with the development of CNS relapse. This 3-risk group model describes a low-risk group (46% of patients) with a 2-year risk of CNS disease of 0.6%, an intermediate-risk group (41% of patients) with a 3.4% risk, and a high-risk group (12%) with a 10.2% CNS event rate at 2 years. Some of the traditional anatomical risk sites did not add to a multivariate model; this may well be because case numbers were small. Patients with testicular DLBCL should receive CNS prophylaxis.
Secondary CNS events may be leptomeningeal or parenchymal. The optimal strategy for prevention of these events is unknown and centers will have different approaches. For high-risk patients and fit patients, after an initial baseline diagnostic lumbar puncture and delivery of intrathecal methotrexate, I employ intravenous methotrexate 3.5 g/m2 at day 10 in cycles of 2, 4, and 6 of R-CHOP. This may be safely delivered, without compromising delivery of systemic R-CHOP. Maintaining a dose density of R-CHOP is imperative, as these patients are at the greatest risk of systemic events rather than those in the CNS. Delivering CNS-directed therapy during induction is important, as events will typically occur early,86 and so should not be delayed until the end of R-CHOP induction. For those in whom intravenous methotrexate cannot be delivered and who are at high-risk, I continue to use at least 4 administrations of intrathecal methotrexate. In asymptomatic individuals, I do not perform any baseline CNS imaging, in the asymptomatic patient.
A molecular precision approach to DLBCL? Not quite yet
With advances in our understanding of disease mechanisms, we have been better able to divide DLBCL into subgroups with distinct biological and clinical features. These provide additional information beyond our traditional prognostication based upon clinical presenting features. We have identified multiple “druggable” targets and in many cases have studied novel agents that may have activity against distinct oncogenic pathways. Some of these have shown much promise, but it is much the story of DLBCL that successful early-phase observations have not translated into benefit in the phase 3 arena. We are starting to see now the reports on phase 3 studies with novel agents in combination with the (R)-CHOP backbone; to date, these have been disappointing and there may be a number of reasons, including patient selection or inadequate efficacy, that may account for this disappointment. It may well be that, because of the time it takes to molecularly classify patients, we are not including patients with the most aggressive disease—who have the most to gain—in our randomized studies. We must work on the evolution of our biomarker identification and provide standardized platforms for their assessment. There are many novel agents in clinical development. Randomized phase 3 studies with time-to-event endpoints require large numbers of patients and take time to mature. This is economically challenging and so we must better design our phase 3 studies with adaptive designs and multiple “pick the winner”-type arms. R-CHOP is no doubt evolving, and there is much promise ahead, but we have yet to change our gold standard.
Correspondence
Andrew Davies, Cancer Research UK Centre, Cancer Sciences Unit, Faculty of Medicine, University of Southampton, Southampton General Hospital, University Rd, Southampton SO17 1BJ, United Kingdom; e-mail: A.davies@southampton.ac.uk.
References
Competing Interests
Conflict-of-interest disclosure: A.D. has received research funding from Janssen, Pfizer, Karyopharma, Acerta Pharma, Bayer, Takeda, Gilead, Roche, Celgene, and GSK; has consulted for Takeda, Gilead, Roche, and CTI; and has received honoraria from Janssen, Pfizer, Karyopharma, Takeda, Gilead, Roche, Celgene, and CTI.
Author notes
Off-label drug use: None disclosed.