Abstract
From an evolutionary perspective, the immune system developed primarily to protect the host from pathogens. In the continuous balance between killing pathogens and protecting host tissues, selective pressures have shaped the discriminatory functions of the immune system. In addition to protection against microbial pathogens, the immune system also plays a critical role in antitumor immunity. Immune dysfunction, either under- or overactivity, is found in a wide range of hematologic disorders. Here we review the fundamental features of the immune system and the key concepts critical to understanding the impact of immune dysfunction on hematologic disorders.
Learning Objectives
Describe the cardinal features of the innate vs adaptive arms of the immune system
Define the mechanisms that result in an inadequate immune response
Understand the immunotherapeutic approaches to overcome immune dysfunction
CLINICAL CASE
A 70-year-old man in previously good health presents with 6 weeks of fatigue and drenching night sweats. The physical exam is notable for cervical, axillary, and inguinal lymphadenopathy. Laboratory studies are significant for mild anemia and an elevated lactate dehydrogenase level. Lymph node biopsy reveals CD20+CD10+Bcl6+ large B cells consistent with a diffuse large B-cell lymphoma, germinal center subtype. He is treated with rituximab, cyclophosphamide, doxorubicin hydrochloride, vincristine sulfate, and prednisone, also known as R-CHOP, immunochemotherapy for 6 cycles and obtains a complete remission. However, his lymphoma relapses within 6 months, and he has progressive disease despite salvage immunochemotherapy. He then discusses chimeric antigen receptor T cells (CAR-T) therapy vs a bispecific T-cell engager (BiTE) clinical trial with his hematologist.
Introduction
Innate immune system
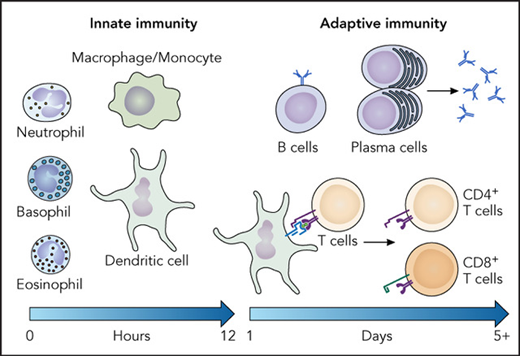
The immune system is classically divided into 2 primary arms—the innate and the adaptive (Table 1). The cardinal feature of the innate immune system is the rapid but nonspecific response to a broad repertoire of pathogens and tissue damage. This response is mediated by germ line-encoded pattern recognition receptors (PRRs) that can recognize conserved features of pathogens or damaged cells, termed pathogen- associated molecular patterns or damage-associated molecular patterns. Cells of the innate immune system include granulocytes, monocytes/macrophages, dendritic cells (DCs), and natural killer (NK) cells. Through PRRs, innate immune cells recognize broadly conserved structures present in a large group of micro-organisms, such as bacterial lipopolysaccharide, a component of gram-negative bacteria, or pathogen-associated nucleic acids such as double-stranded RNA. There are 4 main classes of PRRs: toll-like receptors, C-type lectin receptors, NOD-like receptors, and RIG-I-like receptors.
Key characteristics of innate vs adaptive immune cells
| . | Innate . | Adaptive . |
|---|---|---|
| Timing of response | Minutes to hours | Days |
| Self vs nonself | No | Yes |
| Diversity | Limited | Extensive |
| Receptors | Broad, germ line encoded | Highly specific, somatically rearranged |
| Cell types | Granulocytes, macrophages, DCs, NK cells | B cells, T cells |
| . | Innate . | Adaptive . |
|---|---|---|
| Timing of response | Minutes to hours | Days |
| Self vs nonself | No | Yes |
| Diversity | Limited | Extensive |
| Receptors | Broad, germ line encoded | Highly specific, somatically rearranged |
| Cell types | Granulocytes, macrophages, DCs, NK cells | B cells, T cells |
Innate immune cells exert their effector functions through the phagocytosis of infected cells and/or extracellular organisms, the production of inflammatory cytokines, and the release of soluble mediators, such as cytokines and chemokines. Different pathogens trigger distinctive innate immune responses as distinct effector functions are needed for effective clearance. For instance, neutrophils are required to protect against certain fungal pathogens, such as Aspergillus fumigatus and Candida albicans,1 the putative underlying mechanism for the increased risk of invasive fungal infections in patients with prolonged neutropenia following high-dose chemotherapy or allogeneic hematopoietic stem cell (HSC) transplant.2 Furthermore, some innate immune cells such as DCs and macrophages function as antigen presenting cells (APCs). Antigen presentation is a process through which small peptides are incorporated into the binding groove of the major histocompatibility complex (MHC; also known as human leukocyte antigen) proteins. During an infection, small peptides derived from pathogen proteins are presented in the context of self-MHC on the surface of APCs to help activate T lymphocytes and thus the adaptive immune response.
More recently, immune cells termed “innate lymphoid cells” (ILCs), which have features of both the innate and adaptive immune cells, have been recognized. ILCs respond quickly to infection and do not express antigen receptors like innate immune cells but produce similar inflammatory cytokines as T lymphocytes.3
Adaptive immune system
In contrast to the innate immune response, the cardinal features of the adaptive immune response include antigen specificity and the formation of immunological memory, which is the ability of lymphocytes to respond to a previously encountered antigen rapidly and more efficiently upon reexposure. B and T lymphocytes are the primary cells of the adaptive immune system. Both lineages express antigen receptors, the B-cell receptor (BCR) and T-cell receptor (TCR), respectively, which undergo somatic rearrangement to allow B and T cells to recognize and respond to specific antigens. B cells are the primary mediators of the humoral (ie, antibody-mediated) immune response, which functions to protect the host from extracellular micro-organisms and prevent the spread of intracellular pathogens. T cells mediate the cellular immune response, which both supports the humoral immunity and acts as the primary effector cell to kill virally infected or transformed host cells.
Lymphocytes of the adaptive immune system share common features of antigen specificity and the formation of long-lived immune memory. Specificity is achieved by each lymphocyte bearing an antigen receptor that recognizes a single epitope, which is attained by the somatic rearrangement of several sets of gene segments encoding the BCR, which is also a membrane-bound form of antibodies or immunoglobulins (Ig), and TCRs to generate receptor diversity. During B- and T-cell development, the variable (V), diversity (D), and joining (J) gene segments are somatically rearranged through DNA recombination mediated by the recombination-activating genes (RAG1/2) in a relatively analogous process occurring at the light and heavy chains of the immunoglobin loci or the α and β chains of the TCR locus.4-7 The combinatorial diversity of V(D)J recombination is further enhanced with an additional layer of junctional diversity when nucleotides are added or subtracted between different gene segments during the recombination process. Each resultant B or T cell expresses an antigen receptor with unique specificity. Estimates suggest that such diversity could lead to 1015 to 1018 unique BCR combinations and 1015 to 1020 distinct TCRs; however, unique functional populations are significantly smaller due to developmental selection events. Exploiting this fact, polymerase chain reactions to detect somatically rearranged immunoglobulin or TCR loci are a commonly used molecular hematopathology technique to evaluate for clonality in pathology specimens.
B cells: B cells develop in the bone marrow from HSCs, where they undergo several progressive stages of lineage specification and commitment. B-cell commitment and development are regulated by a coordinated network of transcription factors as well as accompanying epigenetic changes. In the bone marrow, developing B cells rearrange the heavy-chain and then the light-chain immunoglobulin loci. Following the generation of an antigen receptor, developing B cells must pass several checkpoints to prevent the production of self-reactive lymphocytes.8 Once each chain is successfully rearranged, a process called allelic exclusion occurs to prevent rearrangement of the other allele, which allows each individual cell to produce only a receptor of single-antigen specificity. Light-chain loci also undergo isotypic exclusion, in which only 1 type of light chain (κ or λ) is expressed by each individual B cell. Once a functional BCR forms (as a surface IgM), the antigen receptor is tested for self-reactivity in a process known as central tolerance to eliminate autoreactive cells. Immature B cells then migrate out of the bone marrow to the spleen, where they undergo further maturation. In the periphery, B cells that encounter and recognize self-antigen in the absence of infection will be deleted or become anergic in a process known as peripheral tolerance. Failure of these tolerance mechanisms can result in B-cell-mediated autoimmunity.
Naive (ie, antigen-inexperienced) B cells are activated by soluble antigen through their BCR, which then initiates an intracellular signaling cascade. The BCR can also deliver the antigen intracellularly for antigen processing to allow B cells to present antigenic peptides to T cells. Some antigens can activate B cells without T cell help (T independent) or require T cell help (T dependent). In T-dependent responses, B cells receive additional activation signals from CD4+ T follicular helper cells that recognizes the antigenic peptide. Activated B cells can differentiate into several different mature subsets,9 including plasmablasts and longer-lived plasma cells, as well as migrate to the germinal center to undergo further maturation, including somatic hypermutation of the V regions of the immunoglobulin genes to generate higher-affinity antibodies (affinity maturation) and class switching to allow B cells to produce antibodies with different effector functions (IgG, IgE, IgA). Molecular subtypes of different lymphomas have similar gene expression signatures as normal B-cell subsets, such as the germinal center B-cell subtype and the activated B-cell subtype (or non-germinal center B cell) of diffuse large B-cell lymphoma,10 which can predict response to certain targeted therapies.11
T cells: T lymphocytes are one of the few cells of the immune system that develop outside the bone marrow. T cell precursors migrate from the bone marrow to the thymus, where they mature into functional T cells. Collectively, mature T cells must possess a diverse TCR repertoire capable of recognizing the immense number of foreign antigens that will be encountered over the host's lifetime. In contrast to B cells that respond to soluble antigen, T cells are stimulated by small antigenic peptides presented on the surface of other cells by MHC molecules. Since the TCR binds antigenic peptides plus some amino acid residues of self-MHC protein, it is critical that only T cells with a TCR able to recognize self-MHC, albeit with limited affinity, be exported to the periphery. In addition, it is essential that T cells possess TCRs that only respond to foreign antigen and that those that possess TCRs recognizing self-peptide in the context of self-MHC are eliminated during development to prevent autoimmunity. Similar to B-cell development, developing T cells undergo several key checkpoints to ensure the development of functional, non-self-reactive T cells.12 In the thymus, developing αβT cells undergo 2 further checkpoints, known as positive and negative selection, to determine TCR fitness. Positive selection occurs when thymocytes interact with self-antigens presented in the context of class I or class II MHC on cortical thymic epithelial cells. The thymocytes that engage antigen/MHC with intermediate affinity are protected from apoptosis, whereas those cells that cannot interact with self-antigen/MHC die by apoptosis. The remaining cells then undergo negative selection, during which cells that react too strongly to self-antigen/MHC undergo apoptosis. This process helps protect the host from T cells that possess TCRs with high reactivity against self-peptides presented by self-MHC, which would lead to autoimmunity. Following positive and negative selection, only remaining thymocytes with moderate affinity for peptide/MHC undergo lineage commitment to become CD4+ or CD8+ T cells, which then migrate to the periphery. Within this continuum of permitted reactivity, the developing CD4+ thymocytes that possess the highest affinity for self-peptide/MHC develop into regulatory T cells (Tregs), characterized by the expression of the transcription factor FoxP3 and the surface expression of CD25. Tregs are a specialized subset of CD4+ T cells that suppress activated CD4+ and CD8+ T cells as well as other immune cells.
Once in the periphery, naive T cells circulate until the TCR recognition of peptide-MHC complexes induces an intracellular biochemical signaling cascade that activates a program of clonal proliferation and differentiation (with additional input from costimulatory molecules and cytokines), thus transforming the naive T cell into an effector T cell. CD4+ and CD8+ T cells undergo analogous differentiation processes, over the span of several days, to acquire functional maturity but play distinct functional roles in the adaptive immune response to pathogens. Naive cells of both lineages are activated through their TCRs, and their differentiation is influenced by a combination of signals, including TCR signal strength, costimulatory ligands, and the local cytokine milieu. The integration of these signals drives the expression of key transcription factors and effector molecules, which endow the activated T cell with its individualized function. Activated CD8+ T cells function to induce death in host cells following activation, whereas CD4+ T cells function primarily through cytokine production or via direct cell-to-cell contact to activate other immune cells. Depending on the signals during differentiation, naive CD4+ T cells have the potential to develop into 1 of several principal effector (or “helper”) subsets, including TH1, TH2, TH17, and T follicular helper (TFH) cells.13 Different subsets of peripheral T-cell lymphomas have been described that likely arise from these subsets.14,15 In addition to the thymically derived Tregs, naive CD4+ T cells can also be induced to become Tregs and exert immunosuppressive functions in the appropriate context. CD8+ T cells become terminally differentiated effector cells or long-lived memory cells following antigen stimulation.16
What constitutes an effective immune response?
A successful immune response results in the clearance of the pathogen and the formation of immunologic memory while preventing host damage. It requires the careful and integrated orchestration of a multistep process involving diverse cell types, cytokines, and anatomic localization. A prototypical immune response can be broken down into 3 main stages: (1) acute inflammatory response to the invading pathogen by the innate immune system, (2) antigen presentation, and (3) adaptive immune response involving CD4+ and CD8+ T cells and B lymphocytes.
Innate acute inflammatory response: The first line of defense is typically barrier surfaces that seek to prevent pathogen entry into the host, including the epithelial surfaces and mucosal surfaces of the respiratory, gastrointestinal, or urogenital tracts. Following entry through these barriers, most pathogens cause a local infection in the tissues. Innate immune cells recognize pathogen-associated molecular patterns and damage-associated molecular patterns through their germ line-encoded PRRs, which initiates an intracellular signaling cascade to activate their unique effector functions. Cytokine and chemokine production promotes local inflammation, attracting circulating innate effector cells such as neutrophils and monocytes. If the initial innate immune response fails to control the infection, the adaptive immune response is triggered in local lymphoid tissues by the presentation of pathogen-derived antigens by APCs.
Antigen presentation: Following pathogen exposure, APCs process foreign peptides and present them on self-MHC. MHC class I and class II molecules function similarly to deliver and present short peptides on the cell surface to allow these peptides to be recognized by CD8+ or CD4+ T cells, respectively. The peptides presented by the different classes originate from either intracellular proteins for MHC class I or engulfed extracellular proteins for MHC class II. All cells of the body are at risk of malignant transformation or infection by intracellular microbes, which requires a CD8+ T cell response, and thus all nucleated cells express MHC class I. Meanwhile, only professional APCs, such as DCs, macrophages, and B cells, express MHC class II. Additionally, a subset of APCs can present internalized antigens in the context of MHC class I molecules via a mechanism called cross-presentation, thus allowing CD8+ T-cell activation against pathogens or tumors that do not directly infect DCs. Inflammatory cytokines help activate APCs and promote upregulation costimulatory molecules, such as B7.1 (CD80) and B7.2 (CD86) on the APC cell surface. Activated APCs then travel from the site of infection to draining lymph nodes, where they present antigen to naive T cells. T cells that recognize antigen:self-MHC on an activated APC proceed to signal through the multimeric TCR complex. Costimulation by the binding of CD28 on the T-cell surface to a B7 molecule on the APC is required for T cell activation. A failure to receive both the TCR (signal 1) and costimulation (signal 2) typically leads to T-cell anergy and apoptosis. T cell activation can be further modulated by additional costimulatory or coinhibitory signals.17 Activating signals include those provided via 4-1BB (CD37), OX40 (CD134), and CD27.
Adaptive immune response: Following activation by APCs, antigen-specific T cells and B cells undergo clonal expansion and differentiation over several days. B cells produce pathogen- specific antibodies that can activate complements to directly kill pathogens, opsonize pathogens to promote phagocytosis, and promote antibody-dependent cell-mediated cytotoxicity. Activated CD4+ T cells release cytokines to enhance other immune cell function, such as macrophage-mediated phagocytosis. Effector CD8+ T cells release proinflammatory cytokines and can directly kill infected cells via cytolysis. Following pathogen clearance, the majority of antigen-specific lymphocytes undergo cell death, resulting in clonal contraction. A small subset remains as long-lived memory lymphocytes that have the capacity to respond to the same pathogen more rapidly upon rechallenge, leading to less severe or subclinical infection.
Importantly, the immune system has several mechanisms to preserve a careful balance between allowing appropriate activation of the immune system and preventing immune overactivation and subsequent tissue damage of the host. For example, in contrast to the costimulatory signals outlined above, coinhibitory signals, such as those mediated by ligands to programmed cell death 1 protein (PD-1), cytotoxic T-lymphocyte antigen 4 (CTLA-4), and lymphocyte-activation gene 3 (LAG3), serve to suppress immune activation and act as a biological rheostat to prevent tissue damage from a hyperactive immune response. In addition, Tregs mediate their immunosuppressive function in trans on other immune cells, including CD4+ and CD8+ T cells, B cells, DCs, NK cells, and macrophages, through CTLA-4 expression; production of the suppressive cytokines IL-10, IL-35, and transforming growth factor β; the conversion of extracellular adenosine triphosphate to adenosine; and the consumption of local IL-2.
Mechanisms that result in an inadequate immune response
The increased risk of malignancies that develop in patients with primary (more recently termed inborn errors of immunity) or secondary (acquired) immunodeficiencies highlights the importance of immune surveillance to prevent cancer.18 The malignant transformation of host cells presents unique challenges to the immune response since the cells are self in origin, and self-tolerance may prevent the development of a full immune response. Multiple mechanisms in the tumor microenvironment dampen effective antitumor responses (Table 2). The selective pressures of an immune response can promote the loss of antigenicity of the tumor itself through several potential mechanisms. Lymphomas, and less commonly leukemias, can lose MHC class I or class II expression.19-23 Additionally, tumor cells can downregulate costimulatory molecules to prevent T cell activation, dysregulation of antigen-processing machinery can lead to the loss of antigen presentation, and selective pressure could lead to the outgrowth of a tumor clone that no longer expresses recognized antigens. Furthermore, the tumor microenvironment in many hematologic malignancies is immunosuppressive, with the upregulation of inhibitory ligands on the malignant cells or other cells. For instance, certain lymphoma cells may overexpress PD-L1/2, which may be driven by viral infection or genetic alterations.24-26 Immunosuppressive cells in the tumor microenvironment, such as Tregs or macrophages, can also dampen the immune response to leukemias and lymphomas.27
Mechanisms that dampen immune response in the tumor microenvironment and corresponding immunotherapeutic approaches
| Mechanisms to evade immune response . | Immunotherapeutic approaches . |
|---|---|
| Loss of antigenicity of tumor cells (ex: loss of MHC, downregulation of costimulatory molecules) | CAR-T, BiTE |
| Increased expression of inhibitory ligands on tumor cells or in microenvironment | Immune checkpoint blockade |
| Suppressive immune populations in tumor microenvironment | CD47 blockade (experimental) |
| Mechanisms to evade immune response . | Immunotherapeutic approaches . |
|---|---|
| Loss of antigenicity of tumor cells (ex: loss of MHC, downregulation of costimulatory molecules) | CAR-T, BiTE |
| Increased expression of inhibitory ligands on tumor cells or in microenvironment | Immune checkpoint blockade |
| Suppressive immune populations in tumor microenvironment | CD47 blockade (experimental) |
Modulating the immune system to overcome immune dysfunction
Immunotherapeutic approaches to overcome or bypass immune dysfunction have had clinical success in many hematologic disorders. The most long-standing example of immunotherapy to treat hematologic malignancies is the allogeneic HSC transplant, first used in humans in 1957.28 Discoveries arising from decades of research have found that the reconstituted donor-derived immune system, particularly donor lymphocytes, mediates a graft-versus-leukemia/lymphoma effect but also leads to graft-versus-host disease, during which activated donor T cells recognize the host tissue as foreign, leading to tissue damage.
More recent immunotherapeutic advances have been built on the recognition that tumor-specific T cells undergo a process termed exhaustion, during which chronic antigen stimulation results in T cells becoming increasingly less responsive, leading to decreased cytokine production and the inability to promote cytolysis.29 Concomitantly, exhausted cells upregulate inhibitory cell surface receptors. The best studied of these inhibitory receptors is PD-1, which binds its ligands, PD-L1 and PD-L2, expressed on activated macrophages and other APCs. The engagement of PD-1 dampens the T-cell response, which normally occurs after initial TCR activation, likely to prevent excessive responses and is subsequently downregulated. Exhausted T cells, however, continue to express this inhibitory receptor.30 Therapeutic targeting of the PD-1 axis has shown efficacy in solid tumors and some lymphomas, including classical Hodgkin lymphoma and primary mediastinal B-cell lymphoma.31-34 However, only a subset of clinical responses is long-lasting, possibly because PD-1/PD-L1 blockade alters signaling pathways within the responding T cells but not the epigenetic landscape.35,36 Current clinical trials are ongoing to examine whether the combination of epigenetic therapy—ie, with hypomethylating agents or histone deacetylase inhibitors—and immune checkpoint blockade improves response rates or durability.
Another recent advance in modulating the immune system to fight hematologic malignancies or viral infection is the use of redirected autologous T cells. The most explored of these approaches is the use of CAR-T to treat relapsed/refractory CD19-expressing B-cell malignancies.37 This approach modifies autologous T cells with the introduction of an engineered antigen receptor to promote an antitumor response. The engineered antigen receptor combines an extracellular domain of a single-chain variable fragment, which is a fusion of the variable regions of the heavy and light chains of an immunoglobulin recognizing the CD19 antigen, with intracellular domains of the CD3ζ chain and the signaling domain of a costimulatory molecule, such as CD28 or 4-1BB. The addition of the costimulatory domain improves the persistence and efficacy of engineered T cells,38 which mirrors the known requirement of costimulation for normal T cell function. Another method of redirecting autologous T cells includes the use of BiTEs, which are fusion proteins containing 2 antibody recognition domains.39 One domain recognizes the CD3 complex on autologous T cells, and a second recognizes a surface receptor present on the tumor cells, such as CD19 or CD20 on B-cell malignancies. BiTEs bring the T cells into the proximity of the tumor cells, and the engagement of both domains promotes the activation of T cells, cytokine production, and cytotoxicity independent of the TCR specificity of the T cell. Currently, only blinatumomab, a CD3xCD19 BiTE, is approved for B-cell precursor acute lymphoblastic leukemia, but many others are currently undergoing clinical trials for B-cell leukemias and lymphomas.
A promising, yet underexplored, approach is that of targeting the immunosuppressive tumor microenvironment in hematologic malignancies to promote a more effective T-cell response. One mechanism to achieve this outcome would be to induce macrophage phagocytosis of transformed cells and thereby enhance tumor antigen presentation to host T lymphocytes. This could be achieved by blockade of CD47 (also known as the “don't eat me signal”) on tumor cells, which enhances tumor antigen presentation to T cells.40 Clinically, CD47 blockade in lymphoma patients has shown some potentially promising early-phase clinical trial results.41,42
Conflict-of-interest disclosure
Shannon A. Carty: no competing financial interests to declare.
Off-label drug use
Shannon A. Carty: nothing to disclose.