Abstract
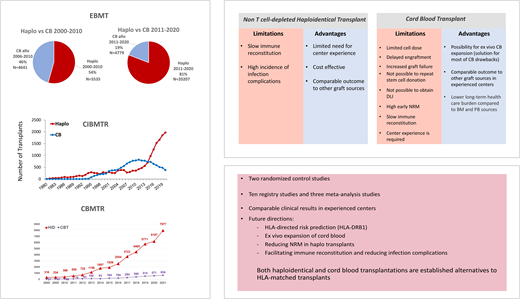
Allogeneic hematopoietic stem cell transplantation is the treatment of choice for high-risk hematological malignancies such as acute myeloid and lymphocytic leukemia, myelodysplastic syndrome, and myeloproliferative disorders. Alternative donor transplantation from either haploidentical (haplo-SCT) or cord blood donor (CBT) is an established therapeutic alternative for patients who need transplants but lack a human leukocyte antigen–matched donor. Although haplo-SCT (mainly non–T-cell-depleted haplo-SCT with posttransplant cyclophosphamide) is increasing while CBT is decreasing worldwide (Figure 1), recent developments in CBT, especially cord blood expansion and other strategies to improve engraftment and immune reconstitution post-CBT, make CBT still a valuable option. This article discusses the 2 options based on the currently available data, focusing on adults, and tries to give some clues to help the transplant physician choose a haploidentical vs a cord blood donor. Given the limited numbers of published or ongoing well-designed randomized controlled trials comparing haplo-SCT to CBT and the overall similar clinical results in the available, mostly registry-based, and single-center studies, with substantial heterogeneity and variability, the decision to perform haplo-SCT or CBT in a given patient depends not only on the patient, disease, and donor characteristics and donor availability (although most if not all patients should have in principle an alternative donor) but also on the transplant physician's discretion and, most importantly, the center's experience and preference and ongoing protocols and strategies.
Learning Objectives
Review the available published literature on haploidentical vs cord blood transplantation
Discuss the available literature that should guide decisions regarding haploidentical vs cord blood transplantation for an adult patient with a high-risk hematological malignancy in need of allogeneic transplantation
CLINICAL CASE 1
A 50-year-old man hospitalized because of acute myeloid leukemia (AML) presented with subfebrile fever, flu-like symptoms, bleeding tendency and leukocytosis, neutropenia, anemia, and thrombocytopenia. Bone marrow (BM) aspiration revealed 70% myeloblasts. Cytogenetic and mutational analysis disclosed monosomy 7 and fms-like tyrosine kinase 3 internal tandem duplication positivity while nucleophosmin 1 was negative. Conventional induction chemotherapy with cytarabine and daunorubicin (7 + 3) in combination with midostaurin yielded the first complete remission (CR1; by morphology and cytogenetics), but molecular remission was achieved only post high-dose cytarabine-midostaurin consolidation. The patient had no human leukocyte antigen (HLA)-matched brothers or sisters, and a search for an unrelated donor that began at the time of diagnosis failed to allocate a 10 of 10 HLA-matched donor. The patient had 4 brothers and sisters (2 of them haploidentical [haplo] and 1 with an HLA DRB1 mismatch), 3 children, and parents with no comorbidities. In parallel, the search for unrelated donors yielded few potential cord blood units (CBUs) with a 6 out of 8 HLA match (considering HLA loci A, B, C, and DRB1). Two of the potential CBUs contained a class II mismatch on HLA DRB1. The total nucleated cell dose of the units ranged between 1 to 2 × 107/kg with 1 to 1.2 × 105 CD34+/kg. Screening by Luminex assay for anti-HLA donor-specific antibodies (DSAs) was positive for 2 of the potential CBUs, with a mean fluorescence intensity level greater than 1000. The patient had no DSAs to the potential haplo donors. The patient was referred by his primary hematologist to a transplant expert for a consultation about allogeneic transplantation, which is strongly indicated for high-risk AML. As no HLA-matched sibling or unrelated donor was available, the potential relevant donors included a haplo donor,1,2 CB with 2 CBUs or ex vivo expanded CB in a clinical trial, or a combination of a graft from a haplo donor and a cord (haplo-cord).3-5 The theoretical considerations, advantages, and disadvantages of haplo transplants (haplo-SCT) vs CB transplants (CBT) were discussed (Table 1).
Haploidentical and cord blood transplantation activities in Europe, the US, and China. (A) Haplo-SCT and CBT for AML and ALL in Europe (Acute Leukemia Working Party of the EBMT). Data include non–T-cell- depleted and T-cell depleted haplo-SCT, single CTB, and double CBT in 2000-2020. (B) Haplo-SCT and CBT in Europe in adult and pediatric populations in 2000-2020. Data include haplo-SCT and CBT for various hematological malignancies (AML, ALL, MDS, MPN [myeloproliferative neoplasms], NHL) in 2020. (C) Haplo-SCT and CBT in the US (CIBMTR) in 2000-2020 for various hematological malignancies (AML, ALL, MDS/MPN, NHL, HL) and nonmalignant diseases, excluding SAA, modified from CIBMTR 2021 summary slides. Data include adults (>18 years) and children and adolescents (<18 years) and BM and PB (peripheral blood) grafts, with MAC or RIC/NMA (nonmyeloablative conditioning). (D) Haplo- SCT (HID) and CBT in China (Chinese Blood and Marrow Transplantation Registry Group) in 2008-2021. Data are for haplo-SCT and CBT in various hematological malignancies (AML, ALL, MDS, NHL) in 2021. peds, pediatric patients; SCBT; single cord blood transplantation; URD, unrelated donor transplant.
Haploidentical and cord blood transplantation activities in Europe, the US, and China. (A) Haplo-SCT and CBT for AML and ALL in Europe (Acute Leukemia Working Party of the EBMT). Data include non–T-cell- depleted and T-cell depleted haplo-SCT, single CTB, and double CBT in 2000-2020. (B) Haplo-SCT and CBT in Europe in adult and pediatric populations in 2000-2020. Data include haplo-SCT and CBT for various hematological malignancies (AML, ALL, MDS, MPN [myeloproliferative neoplasms], NHL) in 2020. (C) Haplo-SCT and CBT in the US (CIBMTR) in 2000-2020 for various hematological malignancies (AML, ALL, MDS/MPN, NHL, HL) and nonmalignant diseases, excluding SAA, modified from CIBMTR 2021 summary slides. Data include adults (>18 years) and children and adolescents (<18 years) and BM and PB (peripheral blood) grafts, with MAC or RIC/NMA (nonmyeloablative conditioning). (D) Haplo- SCT (HID) and CBT in China (Chinese Blood and Marrow Transplantation Registry Group) in 2008-2021. Data are for haplo-SCT and CBT in various hematological malignancies (AML, ALL, MDS, NHL) in 2021. peds, pediatric patients; SCBT; single cord blood transplantation; URD, unrelated donor transplant.
Haplo-SCT vs CBT: advantages and disadvantages
| Donor . | CBT . | HAPLO-transplant . | ||
|---|---|---|---|---|
| SCBT . | DCBT . | TCD . | TCR . | |
| Indications | Nonmalignant and malignant | Nonmalignant and malignant | Mainly malignant | Mainly malignant |
| Age | Mainly pediatric | Adult and pediatric | Adult and pediatric | Adult and pediatric |
| Donor availability | High | High | High | High |
| Degree of HLA mismatch | 1-2 mismatches | 1-2 mismatches | 2-3 mismatches | 2-3 mismatches |
| DSA | Important | Important | Important | Important |
| Time for donor identification | Slower <1 month | Slower compared to SCBT | Faster (immediate) | Faster (immediate) |
| Time of graft acquisition | 15-30 days | 15-30 days | 15-30 days | 15-30 days |
| Type of graft | Cryopreserved CBU | 2 cryopreserved CBUs | Mobilized PB | Mobilized PB and/or BM |
| Limitation of graft acquisition | Cell dose | Improved compared to SCBT | Poor mobilization | Improved compared to TCD haplo |
| Graft manipulation | Ex vivo expansion | None | In vivo TCD | None |
| Donor safety (risk to the donor) | No risk | No risk | Very low | Very low |
| Easy to repeat stem cell donation | Not possible | Not possible | Possible | Possible |
| Conditioning | MAC and RIC | MAC and RIC | MAC | MAC and RIC |
| Engraftment | Delayed | Improvement compared to SCBT | Comparable to MRD or MUD | Comparable to MRD or MUD |
| Use of ATG | Determinantal omitted | Determinantal omitted | Indicated (can be replaced by PTCy) | Indicated (can be replaced by PTCy) |
| GVHD | Lower incidence with less stringent HLA matching needed | Incidence increased compared to SCBT | Low incidence | Low incidence with BM and PTCy; higher incidence with PB |
| NRM | High due to graft failure and infections | Improved compared to SCBT | High | Improved compared to TCD-haplo |
| RI | Comparable to MSD or MUD | Low compared to SCBT | High | Comparable to MSD or MUD (higher in initial report) with BM and RIC |
| DLI | Not possible | Not possible | Possible | Possible |
| Immune reconstitution | Slow | Improved compared to SCBT | Slow | Improved compared to TCD-haplo |
| Infections incidence | High | Improved compared to SCBT | High | Improved compared to TCD-Haplo |
| OS | Lower than other stem cell sources | Improved compared to SCBT | Lower than other stem cell sources | Improved compared to TCD-Haplo |
| Cost associated with donor search and graft procurement | High | Very high | Lower | Lower |
| Donor . | CBT . | HAPLO-transplant . | ||
|---|---|---|---|---|
| SCBT . | DCBT . | TCD . | TCR . | |
| Indications | Nonmalignant and malignant | Nonmalignant and malignant | Mainly malignant | Mainly malignant |
| Age | Mainly pediatric | Adult and pediatric | Adult and pediatric | Adult and pediatric |
| Donor availability | High | High | High | High |
| Degree of HLA mismatch | 1-2 mismatches | 1-2 mismatches | 2-3 mismatches | 2-3 mismatches |
| DSA | Important | Important | Important | Important |
| Time for donor identification | Slower <1 month | Slower compared to SCBT | Faster (immediate) | Faster (immediate) |
| Time of graft acquisition | 15-30 days | 15-30 days | 15-30 days | 15-30 days |
| Type of graft | Cryopreserved CBU | 2 cryopreserved CBUs | Mobilized PB | Mobilized PB and/or BM |
| Limitation of graft acquisition | Cell dose | Improved compared to SCBT | Poor mobilization | Improved compared to TCD haplo |
| Graft manipulation | Ex vivo expansion | None | In vivo TCD | None |
| Donor safety (risk to the donor) | No risk | No risk | Very low | Very low |
| Easy to repeat stem cell donation | Not possible | Not possible | Possible | Possible |
| Conditioning | MAC and RIC | MAC and RIC | MAC | MAC and RIC |
| Engraftment | Delayed | Improvement compared to SCBT | Comparable to MRD or MUD | Comparable to MRD or MUD |
| Use of ATG | Determinantal omitted | Determinantal omitted | Indicated (can be replaced by PTCy) | Indicated (can be replaced by PTCy) |
| GVHD | Lower incidence with less stringent HLA matching needed | Incidence increased compared to SCBT | Low incidence | Low incidence with BM and PTCy; higher incidence with PB |
| NRM | High due to graft failure and infections | Improved compared to SCBT | High | Improved compared to TCD-haplo |
| RI | Comparable to MSD or MUD | Low compared to SCBT | High | Comparable to MSD or MUD (higher in initial report) with BM and RIC |
| DLI | Not possible | Not possible | Possible | Possible |
| Immune reconstitution | Slow | Improved compared to SCBT | Slow | Improved compared to TCD-haplo |
| Infections incidence | High | Improved compared to SCBT | High | Improved compared to TCD-Haplo |
| OS | Lower than other stem cell sources | Improved compared to SCBT | Lower than other stem cell sources | Improved compared to TCD-Haplo |
| Cost associated with donor search and graft procurement | High | Very high | Lower | Lower |
SCBT, single cord blood transplantation; TCD, T-cell depletion; TCR, T-cell repletion.
The remainder of this article focuses mainly on a comparison of non–T-cell-depleted haplo-SCT with posttransplant cyclophosphamide (PTCy) and CBT.
Theoretical considerations for haplo vs CB grafts
As depicted in Table 1, CB and haplo donors as alternative hematopoietic stem cell sources have potential strengths as well as limitations.1-4 Some of these historical advantages and disadvantages have subsequently been overcome with recent developments in the field, including double-unit CBT (DCBT) and the ex vivo expansion of CBUs, overcoming the cell-dose limitation that resulted in slow and low engraftment as well as slow immune reconstitution and lead to the high infection rates and early transplant-related mortality rate associated with CBT.3,4 In parallel, the non–T-cell-depleted haplo platform, especially with PTCy, improves engraftment rates and immune reconstitution posttransplant, significantly reducing the historical limitations of T-cell-depleted haplo-SCT, which are mainly nonengraftment, high infection rates, high transplant-related complications and mortality, and high relapse incidence (RI).1,2 Still, haplo grafts possess some advantages in comparison to CBU grafts, including a shorter time for donor identification, the possibility for a repeat stem cell donation, donor lymphocyte infusion (DLI), and lower cost (Table 1).
Haplo-STC vs CBT: registry-based studies
Several registry-based studies have compared alternative donor transplants, including haplo-SCT, to CBT (Supplemental Table 1). Ruggeri et al,6 on behalf of the European Society for Blood and Marrow Transplantation (EBMT), compared non–T-cell-depleted haplo-SCT to CBT in 1446 patients with AML (n = 918) and lymphocytic leukemia (ALL; n = 528). CBT was associated with delayed engraftment and higher graft failures in both AML and ALL. CBT resulted in a lower incidence of chronic graft-versus-host disease (cGVHD) in both AML and ALL. The main take-home message of this large-cohort registry-based analysis was that there were no statistical differences in main outcomes after haplo-SCT and CBT. Specifically, RI did not differ between the two graft sources. Nonrelapse mortality (NRM) and leukemia-free survival (LFS) were comparable as well (Supplemental Table 1).6 A subsequent analysis, by Versluis et al,7 assessed the outcomes of poor-risk AML in CR1 from various donor categories. The study included 193 patients who underwent haplo-SCT and 333 undergoing CBT. The 2-year OS was significantly lower for umbilical cord blood (UCB) grafts compared to haplo-SCT, with no differences in 2-year NRM. The results were confirmed by multivariable analysis (MVA). The author concludes that especially haplo but also CB donors are alternative graft sources for high-risk AML patients who need hematopoietic stem cell transplantation (HSCT) and do not have an HLA-matched donor. However, sufficient numbers and follow-up to define a hierarchy are lacking.7 In a more recent EBMT analysis that included 106 188 patients with different hematological malignancies and assessed longitudinal outcomes of HSCT from various graft sources comparing the results of transplants performed in 2006-2010 to those performed in 2011-2015, the authors demonstrated improved 3-year OS for both haplo-SCT and CBT. Interestingly, the improvement in OS was mostly driven by a reduction in NRM, including for haplo-SCT, with the exception of CBT recipients, who had a lower RI.8 Both haplo-SCT and CBT demonstrated a greater hazard for NRM, with overlapping risk between the 2 donor types. The leading cause of NRM in both haplo-SCT and CBT was infections.8 A combined EBMT-Eurocord study focused on patients with AML receiving thiotepa, busulfan, and fludarabine (TBF) conditioning before both non–T-cell-depleted haplo-SCT and single CBT. It demonstrated increased NRM, delayed engraftment, and higher graft failure in the CBT vs haplo-SCT, which translated into reduced OS and GVHD-free, relapse-free survival (GRFS) in the CBT group compared to the haplo group.9 The Adult AML and the Donor/Source Working Group of the Japan Society for Hematopoietic Cell Transplantation also performed a registry-based study retrospectively comparing the results of haplo-SCT to CBT in 1313 adult patients with intermediate- or poor-risk AML in CR (Supplemental Table 1).10 Between 2007 and 2018 in Japan, 211 patients received haplo-SCT and 1102, single CBT. The cumulative incidences of neutrophil and platelet recovery were significantly lower in CBT when compared with haplo-SCT. Grade 2 to 4 acute GVHD (aGVHD) was significantly higher in CBT, while extensive cGVHD and cytomegalovirus antigenemia were higher in haplo-SCT. In the MVA and propensity scores matching grade 3 to 4, aGVHD as well as RI, NRM, LFS, OS, and GRFS did not differ between the two graft sources.10 The Kyoto Stem Cell Transplantation Group retrospectively compared 57 non–T-cell-depleted haplo-SCT patients to 460 patients receiving single CBT between 2013 and 2019 and demonstrated similar results: significantly delayed neutrophil and platelet engraftment for CBT recipients but similar OS, NRM, GVHD, and RI. Interestingly, in the AML subgroup RI was lower with CBT in comparison to the haplo-SCT group (Supplemental Table 1).11 The Center for International Blood and Marrow Transplant Research (CIBMTR) has also recently compared 375 non–T-cell-depleted haplo-SCT with PTCy to 333 CBT performed between 2012 and 2017 with myeloablative conditioning (MAC) in patients (adults and pediatric) with different hematological malignancies. Three-year OS and LFS were similar. RI was lower and NRM was higher in fewer than or equal to 5 out of 8 HLA-matched CBT patients vs 6 to 8 out of 8 HLA-matched CBT and haplo-SCT patients. The engraftment of both neutrophils and platelets was delayed with CBT vs haplo-SCT. aGVHD was higher with CBT, while cGVHD did not differ between the 2 graft sources. Of note, the authors did not find a center effect, and no difference was observed between centers that contributed more than 10 vs 6 to 10 cases to the study (Supplemental Table 1).12 In a recent analysis by the CIBMTR focusing on ALL and comparing 393 non–T-cell-deleted haplo-SCT to other graft sources, including 305 CBTs in the years 2013 to 2017, CBT had inferior OS and LFS before 18 months and similar OS and LFS after 18 months. The rates of RI and cGVHD after 18 months were no different between CBT and haplo-SCT, but CBT had increased incidences of NRM and grade 3 to 4 aGVHD (Supplemental Table 1).13 Finally, the health care burden, especially the long-term health care burden, is becoming a very relevant issue with modern, sophisticated, and complex therapies. Recently, the Minnesota group analyzed the 5-year health care burden in 1077 consecutive adults undergoing HSCT from various graft sources, including BM, peripheral blood stem cells (PBSCs), and CBUs. Notably, adults undergoing CBT had a lower long-term health care burden compared with the BM and PBSC graft sources, probably due to a lower incidence of cGVHD, as well as other potential unknown factors, which translated into a better quality of life.14
Haplo-SCT vs CBT: randomized controlled trials
The 2 randomized controlled trials (RCTs) comparing haplo-SCT to CBT are rather limited. The CTN1101 trial (NCT01597778) was performed by the Blood and Marrow Transplant Clinical Trials Network (BMT CTN) and published in Blood in 2021 (Supplemental Table 1 and Table 2).15 This was a phase 3 trial that ran between 2012 to 2018, with a rather long recruiting period, and included 368 patients aged 18 to 70 years with various hematological malignancies in remission (CR; it also included patients beyond the first CR). Of these, 182 patients underwent haplo with BM graft, while 186 underwent CBT with 2 CBUs. Both groups received low-dose TBI/fludarabine/Cy as a conditioning regimen, and haplo recipients received PTCy as GVHD prophylaxis. The trial demonstrated similar 2-year progression-free survival (PFS) (the study primary end point) between haplo-SCT and CBT. However, the 2-year NRM was significantly higher in the CBT group compared to the haplo group (Supplemental Table 1). This resulted in significantly better 2-year overall survival (OS) for haplo-SCT vs CBT (Supplemental Table 1). Both were secondary end points in the study, with the limitation that, usually, studies are not powered on the basis of secondary end points, and rarely are statistical adjustments made for the issue of multiple comparisons. In agreement with the previous literature, neutrophil recovery was lower in the CBT group compared to the haplo group. Platelet recovery was no different between CBT and haplo-SCT. Of note, the incidence of both aGVHD and cGVHD, including the severe and extensive forms, was similar between the 2 study arms. As for the graft-versus-leukemia effect (GVL) initially believed to be somewhat separated from GVHD in CBT, interestingly, the 2-year RI was almost identical post haplo and CBT (Supplemental Table 1). Also, the main cause of death in both study arms was the recurrence of the malignancy. The trial did not assess immunological reconstitution. Notably, mortality from GVHD and infections was comparable in haplo-SCT and CBT. As the most important RTC in the field, even this study faced severe limitations, including a rather long running time and, most importantly, early termination as the trial failed to complete accrual, highlighting the main hurdles in running this type of randomized study. A second analysis of the trial demonstrated that transplant center experience matters and that centers with previous experience in haplo BM transplants (≥10 transplants) had better results, while those with no such experience (≤10 transplants) showed similar results for haplo-SCT and CBT. Therefore, centers with no experience in performing DCBT may do better performing BM haplo with PTCy.16 Moreover, the CIBMTR recently reported on an extended follow-up of trial participants beyond 2 years. A comparison of trial double-unit UCB (dUCB) and nontrial haplo-BM transplantation recipients demonstrated higher PFS and OS at 5 years after haplo-BM transplantation. A comparison to real-world transplants disclosed similar 5-year OS in registry-based and nontrial DCBT and between trial and nontrial haplo-BM transplants, respectively.17 Notably, this additional registry-based study comparing real-world transplantation outcomes in substantially larger numbers of nontrial haplo-BM transplants to trial results with longer follow-up revealed that 5-year survival was significantly higher after nontrial haplo BM transplants compared with trial dUCB, while the longer follow-up of the original trial cohorts failed to demonstrate a difference in 5-year PFS and OS between the treatment groups. Further, the type of graft matters, as nontrial patients who underwent haplo transplants using mobilized PBSC transplants demonstrated significantly higher 5-year survival compared to trial haplo BM and nontrial haplo BM. Similarly, survival was better after haplo-PBSC compared to trial UCB and nontrial UCB.17
Randomized controlled trials of haplo-SCT vs CBT
| Study title . | Clinical trial identifier . | Institution/country . | Patients, N . | Allocation . | Study period . | Primary outcome measures . | Indication . | Status . | Primary investigator . | References . |
|---|---|---|---|---|---|---|---|---|---|---|
| Haplo SCT vs Haplo-cord SCT for Patients With Hematological Disorders | NCT03719534 | First Affiliated Hospital of Soochow University Suzhou, Jiangsu, China | 100 child, adult | Randomized | 1 June 2017- 31 December 2022 | Estimated OS at 3 y post SCT | Hematologic diseases | Recruiting | Jia Chen M. | |
| A Randomized Multicenter Study Comparing Unrelated Umbilical-cord Blood Transplant Versus Human Leukocyte Antigen (HLA)-Haploidentical Related Hematopoietic Stem Cell Transplant for Adult Patients With Hematologic Malignancies | NCT02386332 | Instituto de Investigacion Sanitaria La Fe, Valencia, Spain | 206 adults, ≥18 and ≤55 y | 11 March 2015-March 2020 | DFS (time frame: 2 y) | Hematologic malignancies | Unknown | Sanz MA | Sanz et al18 | |
| A Multi-Center, Phase III, Randomized Trial of RIC and Transplantation of (dUCB) Versus HLA-Haplo Related Bone Marrow for Patients With Hematologic Malignancies | NCT01597778 | CIBMTR, Medical College of Wisconsin, US University of Alabama at Birmingham, Birmingham, AL, US Arizona Cancer Center, Phoenix, AZ, US City of Hope National Medical Center, Duarte, CA, US (and 35 more) | 368 adult, older adult (18 y to 70 y) | Randomized | 12 May 2012-11 September 2020 | Percentage of participants with PFS (time frame: 2 y) | AML ALL Burkitt lymphoma Follicular lymphoma Hodgkin lymphoma Mantle cell lymphoma Non-Hodgkin lymphoma | Completed | Horowitz M | Fuchs et al15 Brunstein et al16 |
| An Observational Cohort Study on Transplant-Related Mortality in Patients Receiving Either a Hematopoietic Stem Cell Transplantation Without ATIR or an Umbilical Cord Blood Transplantation | NCT02188290 | Ohio State University Comprehensive Cancer Center, Columbus, OH, US Algemeen Ziekenhuis Sint-Jan, Brugge, Belgium Institut Jules Bordet, Brussels, Belgium Universitair Ziekenhuis Gasthuisberg, Leuven, Belgium Hamilton Niagara Regional Haemophilia Centre, Hamilton, Ontario, Canada (and 5 more) | 178 adult, older adult (18 y to 65 y) | Retrospective | September 2014- 6 October 2015 | Transplant-related mortality (time frame: up to 12 mo after transplantation) | AML ALL MDS | Completed | Rovers J |
| Study title . | Clinical trial identifier . | Institution/country . | Patients, N . | Allocation . | Study period . | Primary outcome measures . | Indication . | Status . | Primary investigator . | References . |
|---|---|---|---|---|---|---|---|---|---|---|
| Haplo SCT vs Haplo-cord SCT for Patients With Hematological Disorders | NCT03719534 | First Affiliated Hospital of Soochow University Suzhou, Jiangsu, China | 100 child, adult | Randomized | 1 June 2017- 31 December 2022 | Estimated OS at 3 y post SCT | Hematologic diseases | Recruiting | Jia Chen M. | |
| A Randomized Multicenter Study Comparing Unrelated Umbilical-cord Blood Transplant Versus Human Leukocyte Antigen (HLA)-Haploidentical Related Hematopoietic Stem Cell Transplant for Adult Patients With Hematologic Malignancies | NCT02386332 | Instituto de Investigacion Sanitaria La Fe, Valencia, Spain | 206 adults, ≥18 and ≤55 y | 11 March 2015-March 2020 | DFS (time frame: 2 y) | Hematologic malignancies | Unknown | Sanz MA | Sanz et al18 | |
| A Multi-Center, Phase III, Randomized Trial of RIC and Transplantation of (dUCB) Versus HLA-Haplo Related Bone Marrow for Patients With Hematologic Malignancies | NCT01597778 | CIBMTR, Medical College of Wisconsin, US University of Alabama at Birmingham, Birmingham, AL, US Arizona Cancer Center, Phoenix, AZ, US City of Hope National Medical Center, Duarte, CA, US (and 35 more) | 368 adult, older adult (18 y to 70 y) | Randomized | 12 May 2012-11 September 2020 | Percentage of participants with PFS (time frame: 2 y) | AML ALL Burkitt lymphoma Follicular lymphoma Hodgkin lymphoma Mantle cell lymphoma Non-Hodgkin lymphoma | Completed | Horowitz M | Fuchs et al15 Brunstein et al16 |
| An Observational Cohort Study on Transplant-Related Mortality in Patients Receiving Either a Hematopoietic Stem Cell Transplantation Without ATIR or an Umbilical Cord Blood Transplantation | NCT02188290 | Ohio State University Comprehensive Cancer Center, Columbus, OH, US Algemeen Ziekenhuis Sint-Jan, Brugge, Belgium Institut Jules Bordet, Brussels, Belgium Universitair Ziekenhuis Gasthuisberg, Leuven, Belgium Hamilton Niagara Regional Haemophilia Centre, Hamilton, Ontario, Canada (and 5 more) | 178 adult, older adult (18 y to 65 y) | Retrospective | September 2014- 6 October 2015 | Transplant-related mortality (time frame: up to 12 mo after transplantation) | AML ALL MDS | Completed | Rovers J |
Data used with permission from ClinicalTrials.gov.
ATIR, haploidentical, naive cell-enriched T-cell product, depleted of recipient-alloreactive T cells.40
The second RCT to randomize haplo-SCT vs CBT was performed by Sanz et al (NCT02386332) (Supplemental Table 1 and Table 2).18 The study prospectively randomized CBT with single CBUs and non–T-cell-depleted haplo with PBSCs, both following MAC consisting of TBF. Of note, single UCB is not a standard of care in North America. Anti-GVHD prophylaxis included antithymocyte globulin (ATG) in the CBT group and PTCy in the haplo-SCT group. The study report includes 22 patients who underwent haplo-SCT and 23 who underwent CBT.18 Interestingly, 4 patients allocated to the haplo arm crossed over to the CBT arm because no haplo donor could be allocated (in the CTN1101 trial, CB was used for 11 of 182 patients randomized to the haplo arm due to donors being ineligible or declining to donate, whereas only 1 of 186 patients randomized to receive CB crossed over to the haplo study arm, due to patient preference). In this rather small study, neutrophil and platelet recovery was slower and lower with CBT compared to the haplo-SCT. Acute and chronic GVHD, as well as RI, was similar between the haplo-SCT and the CBT groups. NRM was higher in CBT in comparison to haplo-SCT. Two-year disease-free survival (DFS), OS, and GRFS were significantly better in haplo-SCT compared to CBT. This study emphasizes once again the technical difficulties of running donor-based RTC studies and also the heterogeneity, even in RTC studies, in comparing haplo-SCT to CBT not just in patients and disease characteristics but also in the transplant platform, including single vs double CB grafts, BM vs PBSC graft, MAC vs reduced-intensity conditioning (RIC), and GVHD prophylaxis.
Haplo-SCT vs CBT: meta-analysis
Several meta-analyses have compared haplo to other graft sources, including CBT, as stem cell sources for allogeneic transplantation.19 In 1 such meta-analysis recently reported by Owattanapanich et al comparing haplo-SCT and CBT in patients with ALL in mostly registry-based studies, the pooled odds ratios of OS and LFS in the haplo-SCT and CBT groups were not statistically different. Similarly, the NRM, RI, and aGVHD grade 2 to 4 outcomes of the 2 groups did not statistically differ. Another meta-analysis included 7 studies with 1311 adults undergoing CBT and 915 adults undergoing haplo-SCT and showed no major difference in aGVHD and cGVHD and no difference in 2-year RI, NRM, and DFS (measures of survival could not be pooled because of the different definitions used in the different studies included). The authors concluded that CBTs and haplo-SCT can be considered equally effective options for adult patients without HLA-matched donors.20 A third meta-analysis included 12 studies that compared haplo-SCT to CBT in patients with various hematological malignancies that differed from the above 2 meta-analyses. It reported superior OS and lower NRM and aGVHD with haplo-SCT compared to the CBT group, while RI was similar and cGVHD higher, respectively.21
CLINICAL CASE 1 (Continued)
The patient was informed, after going over the available literature, including RCTs, registry-based studies, and meta-analysis, that both haplo transplantation and CBT were legitimate options. However, the potential CBUs allocated to him were below the recommended cell dose. Additionally, given the patient's DSAs and the referred transplant center's lack of experience in CBT and the lack of an ongoing clinical trial with ex vivo expanded or haplo-cord, the center recommended a non–T-cell-depleted haplo transplant with TBF conditioning and PTCy as anti-GVHD prophylaxis.3,22 The preferred haplo donor was his brother with the HLA-DRB1 mismatch in view of the emerging data demonstrating that HLA-DRB1 mismatches in haplo-SCT may be associated with a lower risk of disease recurrence and that HLA-DRB1 mismatching with HLA-DQB1 matching and HLA-B leader matching in special scenarios correlates with improved DFS and OS.23 Furthermore, the patient was told that due to harboring monosomy 7 and fms-like tyrosine kinase 3 internal tandem duplication mutation defining high-risk leukemia, which has been shown to be a poor prognostic factor in alternative donor transplants,24,25 the risk of posttransplant recurrence was substantial. As per recent publications, HLA-B leader might also have implications for NK immunotherapy,26 which may be important for the GVL effect. For the same reason, posttransplant sorafenib was recommended.27
Haplo-SCT vs CBT: myelodysplastic syndrome and secondary AML
Few studies have compared haplo-SCT and CBT in myelodysplastic syndrome (MDS) and secondary AML. The EBMT performed a registry-based study comparing non–T-cell-depleted haplo-SCT with PTCy to CBT and mismatched unrelated transplants (MMUDs) in patients with MDS (Supplemental Table 1).28 The haplo-SCT group consisted of 222 patients while the CBT group comprised 168 patients. Engraftment was lower with CBT compared to haplo-SCT, while GVHD was lower in haplo-SCT, and 3-year cGVHD and RI did not differ. OS and NRM were better in haplo-SCT compared to CBT (Supplemental Table 1). Additional analysis was performed for 409 secondary AML patients receiving either CBT (n = 163) or haplo-SCT (n = 246). CBT was associated with a higher risk of grade 2 to 4 aGVHD and lower GRFS compared to haplo-SCT. Of note, cGVHD, RI, NRM, LFS, and OS were not statistically different between haplo-SCT and CBT.29 More recently, Childs et al conducted a prospective phase 2 trial of haplo-cord (co-infusing a single UCB unit with CD34+- selected cells from a haplo relative) in 29 patients, including 10 with hypoplastic MDS post severe aplastic anemia (SAA) and 10 SAA patients. Neutrophil recovery occurred with a median of 10 days and platelet recovery, with a median of 32 days. Grade 2 to 4 aGVHD was 21% while cGVHD was 41%. The 7.5-year OS was 83% and GRFS was 69%. The authors concluded that haplo-cord transplants provide an alternative option for patients with hypoplastic MDS and refractory SAA who lack HLA-matched donors.30
CLINICAL CASE 2
A 32-year-old man presented with clinically meaningful lymphadenopathies. A morphological, immunohistochemical, and molecular evaluation of a lymph node biopsy disclosed high-risk lymphoma with MYC translocation and TP53 mutation. The disease was refractory to multiple lines of immune chemotherapy as well as HSCT from an HLA-matched sibling donor (MSD) following MAC. Within 3 weeks of transplant, the disease progressed to a leukemic phase refractory to high-dose cytarabine and mitoxantrone and DLI. The patient was admitted and received chimeric antigen receptor (CAR) CD19 T-cell therapy. One month after cell infusion, positron emission tomography/computed tomography showed significant improvement, with the resolution of previous F-fluorodeoxyglucose-avid lesions consistent with a complete metabolic response. In view of the ultra-high-risk disease and the short persistence of the CAR T cells and the previous relapse 3 weeks post HLA-identical sibling transplant, a second transplant from an alternative donor was considered. As no HLA-compatible unrelated donor was available, the alternatives were haplo-SCT or CBT.
Haplo-SCT vs CBT: non-Hodgkin, Hodgkin lymphoma, and other lymphatic malignancies
Although the number of HSCTs in malignant lymphomas is decreasing due to the emergence of novel drug-conjugated and bispecific novel monoclonal antibodies and CAR T cells, HSCT still has a potential role in a selected group of young lymphoma patients. Few single-center and registry-based studies have compared haplo-SCT to CBT for non-Hodgkin lymphoma (NHL) and Hodgkin lymphoma (HL). A joint study by the EBMT, Eurocord, and the CIBMTR analyzed 740 patients with NHL and HL who received either haplo-SCT or CBT between 2009 and 2016. Haplo transplants with either BM or PBSCs as a graft source resulted in significantly lower NRM and better PFS and OS (Supplemental Table 1).31 Cornillon et al compared haplo-SCT to CBT in 95 patients with T-cell lymphoma, demonstrating similar PFS and OS and showing that the donor source, whether haplo or CBU, had no major impact on the transplant outcome (Supplemental Table 1).32 Messer et al systematically reviewed some of the early studies on alternative and unrelated donor transplantation in HL. In the 2 or 3 studies that included haplo-SCT and CBT, outcomes did not differ at large; however, the group was very heterogeneous, and some of the outcome parameters were missing.33 Additional studies combined the 2 graft sources in high-risk lymphoma and chronic lymphocytic leukemia with interesting results.34,35 Another addresses haplo-SCT and CBT as well as haplo-cord transplants in pediatric ALL, which is beyond the scope of this review.36-38
CLINICAL CASE 2 (Continued)
Following broad consultation with the patient and his family evaluating the limited therapeutic alternatives in a highly aggressive TP53-positive lymphoma and the course of the patient's disease, haplo-SCT with TBF conditioning and PTCy was performed. The donor was a haplo brother because it was felt that a haplo donor, rather than a CB donor, offered the fast engraftment needed. Unfortunately, the patient died early after the second transplant from transplant-related toxicity.
Future directions
The future optimization of CBT should include a better understanding of the clinical significance of the HLA barrier, hopefully leading to improvements in the current selection of the optimal CBU, increasing CBT cell dose, improving engraftment by ex vivo expansion, and omitting in vivo T-cell depletion (ATG) from the preparative protocols. Some of these strategies have already been implemented, leading to significant improvements in hematopoietic engraftment post CBT and a substantially reduced nonengraftment rate, shortening the length of posttransplant pancytopenia, reducing infection rates, improving immune reconstitution post CBT, impressively reducing day-100 mortality post CBT, and improving outcomes.39 As for haplo transplants, future directions must focus on optimizing conditioning protocols, defining the optimal dose and schedule of PTCy in non–T-cell-depleted transplants, and facilitating posttransplant immune reconstitution.40 Optimizing conditioning protocols with compounds such as treosulfan and especially using pharmacokinetics-based conditioning improves haplo-SCT success rates in the advanced-age patient population.2 The shift from BM grafts, the original stem cell source in non–T-cell-depleted haplo-SCT with PTCy, to PBSC grafts may speed engraftment and immune reconstitution and reduce the relapse rate, with the cost of higher incidences of both GVHD and cytokine release syndrome (CRS).2,41 Notably, patients who developed CRS following a non–T-cell-depleted haplo-SCT with PBSC grafts and PTCy demonstrated a higher incidence of grade 2 to 4 acute GVHD compared to those who did not.41 Finally, the optimal dose and schedule of PTCy are yet to be defined, and it is conceivable that lower doses reduce some of the reported transplant-associated toxicity, including cardiotoxicity and CRS.41,42 Based on the promising results of the ongoing studies aiming to improve engraftment in the setting of CBT and to fasten immune reconstitution post haplo-SCT,39,40 future outcomes with both transplant options look encouraging.
Acknowledgments
The authors thank Annalisa Ruggeri for helpful discussion and critical reading of the manuscript; Jacob Passweg, Helen Baldomero, the Acute Leukemia Working Party (ALWP) office, Xiao Jun Huang, and Marcelo Pasquini for providing transplant activities in the EBMT, Chinese Blood and Marrow Transplantation Registry, and Center for International Blood and Marrow Transplant Research, respectively; Ivetta Danylesko and Katia Beider for helping with the manuscript tables and illustrations, and Myriam Labopin and other colleagues from the ALWP of the EBMT.
Conflict-of-interest disclosure
Arnon Nagler: no competing financial interests to declare.
Mohamad Mohty: no competing financial interests to declare.
Off-label drug use
Arnon Nagler: nothing to disclose.
Mohamad Mohty: nothing to disclose.

![Haploidentical and cord blood transplantation activities in Europe, the US, and China. (A) Haplo-SCT and CBT for AML and ALL in Europe (Acute Leukemia Working Party of the EBMT). Data include non–T-cell- depleted and T-cell depleted haplo-SCT, single CTB, and double CBT in 2000-2020. (B) Haplo-SCT and CBT in Europe in adult and pediatric populations in 2000-2020. Data include haplo-SCT and CBT for various hematological malignancies (AML, ALL, MDS, MPN [myeloproliferative neoplasms], NHL) in 2020. (C) Haplo-SCT and CBT in the US (CIBMTR) in 2000-2020 for various hematological malignancies (AML, ALL, MDS/MPN, NHL, HL) and nonmalignant diseases, excluding SAA, modified from CIBMTR 2021 summary slides. Data include adults (>18 years) and children and adolescents (<18 years) and BM and PB (peripheral blood) grafts, with MAC or RIC/NMA (nonmyeloablative conditioning). (D) Haplo- SCT (HID) and CBT in China (Chinese Blood and Marrow Transplantation Registry Group) in 2008-2021. Data are for haplo-SCT and CBT in various hematological malignancies (AML, ALL, MDS, NHL) in 2021. peds, pediatric patients; SCBT; single cord blood transplantation; URD, unrelated donor transplant.](https://ash.silverchair-cdn.com/ash/content_public/journal/hematology/2022/1/10.1182_hematology.2022000327/7/m_hem2022000327figure1ab.png?Expires=1765897790&Signature=WozAKHOsHHMJVwtQXL~KN5tKWCOQGeFVBbt2BWZ6YOLtoKpwnoQgYk5uDtaRzoj8ouX5nDwME7lr0YNTJzJRPG5t157z6LzNOHEcVclvsVJdnREQ7xmjvH8Of3W2L4ij-hG~kRFEEIXbh47Jx~H0OqatBlXVUS7LsL1lrn69NrFVRJtdkQ5mV57nVAQDvkGd3O3S9QNUcLAgxPkGODHzwnZRcsojELA~4nDiU6kKXZHYUGtTWRAhYsQgQujSMMuUXD10nJUq~sVLF40TDyWaCvkkJhBaFMovDkTzbZgLBMM3ba~dabgY5qTuXXIxjeJAqF4AOH5N22IQJIhL8GhFgA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Haploidentical and cord blood transplantation activities in Europe, the US, and China. (A) Haplo-SCT and CBT for AML and ALL in Europe (Acute Leukemia Working Party of the EBMT). Data include non–T-cell- depleted and T-cell depleted haplo-SCT, single CTB, and double CBT in 2000-2020. (B) Haplo-SCT and CBT in Europe in adult and pediatric populations in 2000-2020. Data include haplo-SCT and CBT for various hematological malignancies (AML, ALL, MDS, MPN [myeloproliferative neoplasms], NHL) in 2020. (C) Haplo-SCT and CBT in the US (CIBMTR) in 2000-2020 for various hematological malignancies (AML, ALL, MDS/MPN, NHL, HL) and nonmalignant diseases, excluding SAA, modified from CIBMTR 2021 summary slides. Data include adults (>18 years) and children and adolescents (<18 years) and BM and PB (peripheral blood) grafts, with MAC or RIC/NMA (nonmyeloablative conditioning). (D) Haplo- SCT (HID) and CBT in China (Chinese Blood and Marrow Transplantation Registry Group) in 2008-2021. Data are for haplo-SCT and CBT in various hematological malignancies (AML, ALL, MDS, NHL) in 2021. peds, pediatric patients; SCBT; single cord blood transplantation; URD, unrelated donor transplant.](https://ash.silverchair-cdn.com/ash/content_public/journal/hematology/2022/1/10.1182_hematology.2022000327/7/m_hem2022000327figure1c.png?Expires=1765897790&Signature=0q8zSujf0Qy0tyR4ZeqqCsHnrBnvhltg2a6fvUx-bniEceeRfDTg~sw6ZxtS0sMYm-jdZbD-ur6Y~38i4dmMpxIaq8Baitk1jqw4G0lLkc4vT0jiL3Vx74Iec--BnS69gDREd3QfBaEutOELGdEjljujz5rWhYZpsHEULjTnz9VAswN~jCM0s2uV0HjosFhC1uJk1jXw1jFPINxgdVlpd~l9m4zFmhJXJqSpUYF6QBVC8BZgYSvIeDkU-wKx06awD0Jyn1wGSTxpzxaKG0AQLeSsMXZUmsSeqUt6U8Hx1t6HI1mZ-UNRC5TFzzJg1CnO5MmgwI-Elh-NcOb0XxONDw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Haploidentical and cord blood transplantation activities in Europe, the US, and China. (A) Haplo-SCT and CBT for AML and ALL in Europe (Acute Leukemia Working Party of the EBMT). Data include non–T-cell- depleted and T-cell depleted haplo-SCT, single CTB, and double CBT in 2000-2020. (B) Haplo-SCT and CBT in Europe in adult and pediatric populations in 2000-2020. Data include haplo-SCT and CBT for various hematological malignancies (AML, ALL, MDS, MPN [myeloproliferative neoplasms], NHL) in 2020. (C) Haplo-SCT and CBT in the US (CIBMTR) in 2000-2020 for various hematological malignancies (AML, ALL, MDS/MPN, NHL, HL) and nonmalignant diseases, excluding SAA, modified from CIBMTR 2021 summary slides. Data include adults (>18 years) and children and adolescents (<18 years) and BM and PB (peripheral blood) grafts, with MAC or RIC/NMA (nonmyeloablative conditioning). (D) Haplo- SCT (HID) and CBT in China (Chinese Blood and Marrow Transplantation Registry Group) in 2008-2021. Data are for haplo-SCT and CBT in various hematological malignancies (AML, ALL, MDS, NHL) in 2021. peds, pediatric patients; SCBT; single cord blood transplantation; URD, unrelated donor transplant.](https://ash.silverchair-cdn.com/ash/content_public/journal/hematology/2022/1/10.1182_hematology.2022000327/7/m_hem2022000327figure1d.png?Expires=1765897790&Signature=sS85MAmiZ4GsQTNU5buK9BCZDHGKGP1Y8McawvsgwrNXq6i4H6OSOuaiH1HTxC4xFfjC-5D8CdzIwljNThqW8t9G80YA93vlwZiSl7RRgQmtoLhkm56O2K-b0A7o7MLvgurC5xbJ1fXys5OJrOBVCi2JasUfzocDuPbdST4m8Fhh49eQOBsYEftDET-AkLwjzOnpP9LlqjOgBBarCuEvJzYnEeJ8IzB1rcaZ9orCrQg-g9Tl7pqzqd1uYn2Lt0uOHRlfoTU~HmcFitIkOcIU6dyf74CDexPrMbcIKKGVL07RQjKG-2bxSzpVBIk46hBb7C7KJ6CU6tDKx61JLdRaqQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)