Key Points
Demographic changes have a direct impact on the blood supply, and demography can be used to predict blood donation rates in the future.
The transfusion demand cannot be predicted from demography.
Abstract
Transfusion safety includes the risk of transmission of pathogens, appropriate transfusion thresholds, and sufficient blood supply. All industrialized countries experience major ongoing demographic changes resulting from low birth rates and aging of the baby boom generation. Little evidence exists about whether future blood supply and demand correlate with these demographic changes. The ≥50% decline in birth rate in the eastern part of Germany after 1990 facilitates systematic study of the effects of pronounced demographic changes on blood donation and demand. In this prospective, 10-year longitudinal study, we enrolled all whole blood donors and all patients receiving red blood cell transfusions in the state of Mecklenburg-West Pomerania. We compared projections made in 2005 based on the projected demographic changes with: (1) number and age distribution of blood donors and transfusion recipients in 2015 and (2) blood demand within specific age and patient groups. Blood donation rates closely followed the demographic changes, showing a decrease of −18% (vs projected −23%). In contrast, 2015 transfusion rates were −21.3% lower than projected. We conclude that although changes in demography are highly predictive for the blood supply, transfusion demand is strongly influenced by changes in medical practice. Given ongoing pronounced demographic change, regular monitoring of the donor/recipient age distributions and associated impact on blood demand/supply relationships is required to allow strategic planning to prevent blood shortages or overproduction.
Introduction
A safe and adequate blood supply is an integral part of every country’s national health care policy and infrastructure.1 Enormous progress has been made to prevent transmission of pathogens by blood products,2-4 to establish lower transfusion thresholds for red blood cell (RBC) concentrates in various indications and patient populations,5-12 and to solve issues related to the age of stored blood.13-16
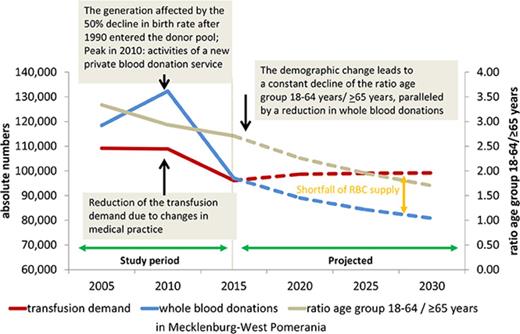
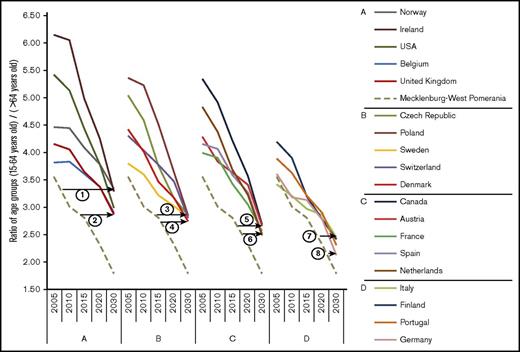
Another important aspect of transfusion safety, an adequate blood supply, has not been a major issue in industrialized countries during the past decades; however, this may change in times of major demographic alterations. The population structure in most countries in Europe and North America is shifting from younger to older age groups because of an increase in life expectancy and aging of previous high birth rate cohorts, aggravated by a sustained decrease in birth rates. Because most blood donors belong to the age group of 18 (or 16 years in some countries) to 65 years and the majority of blood recipients are in the age group >65 years, the ratio between these 2 population groups is relevant for the blood supply/demand relationship. This ratio will change substantially in all European and North American countries during the next decade17 (Figure 1; supplemental Table 1).
Changes in the ratio of the age groups 15 to 64 years and >64 years in different countries. In all countries shown, the demographic change will cause a major shift in the ratio of the age groups between 15 to 64 years and >64 years, which reflects the ratio of the main blood donor population vs the main blood recipient population. The demographic change is most pronounced in the eastern German state of Mecklenburg-West Pomerania, which can be seen as a model region where the effects of the demographic change on the blood supply manifest 10 to 15 years earlier than in other regions. The figure is grouped into 4 panels that summarize countries with similar changes in demography. The countries are listed according to the ratio between age groups in 2030 from the highest to the lowest ratio. The hatched line shows the change in the population ratio in Mecklenburg-West Pomerania; the numbered horizontal lines show at which year the population ratio of Mecklenburg-West Pomerania exemplifies the population ratio reached in 2030 for the extremes in each group. The other countries of each panel show effects in between. Supplemental Table 1 provides the respective data.
Changes in the ratio of the age groups 15 to 64 years and >64 years in different countries. In all countries shown, the demographic change will cause a major shift in the ratio of the age groups between 15 to 64 years and >64 years, which reflects the ratio of the main blood donor population vs the main blood recipient population. The demographic change is most pronounced in the eastern German state of Mecklenburg-West Pomerania, which can be seen as a model region where the effects of the demographic change on the blood supply manifest 10 to 15 years earlier than in other regions. The figure is grouped into 4 panels that summarize countries with similar changes in demography. The countries are listed according to the ratio between age groups in 2030 from the highest to the lowest ratio. The hatched line shows the change in the population ratio in Mecklenburg-West Pomerania; the numbered horizontal lines show at which year the population ratio of Mecklenburg-West Pomerania exemplifies the population ratio reached in 2030 for the extremes in each group. The other countries of each panel show effects in between. Supplemental Table 1 provides the respective data.
The eastern part of Germany, especially the federal state of Mecklenburg-West Pomerania, has encountered particularly pronounced demographic changes.18 This is the result of the rapid and pronounced decline in birth rate (∼50%) after the German reunification in 1989 and ensuing migration of younger people to the western German federal states. The ratio of age groups 18 to 64 years to those ≥65 years was 3.71 in Mecklenburg-West Pomerania in 2005, declined to 2.5 in 2015, and is projected to be 2.4 in 2020 (calculated based on Statistisches Amt Mecklenburg-Vorpommern19 ). Importantly, 10 years later, in 2030, this ratio will be 2.2 in Germany as a whole (calculated based on Statistisches Bundesamt20 ), where the most pronounced changes in population distribution will occur between 2020 and 2030 (Figure 1).
In Germany, blood donations are voluntary and nonpaid, although some donation services provide an allowance of €20 (∼US$22) to cover travel expenses to the blood center. Because blood donors must be at least 18 years old, individuals born after 1989 became eligible for blood donation beginning in 2008. In parallel to these demographic changes, in 2010, the “patient blood management initiative” was started21 with the aim to optimize patients' hemoglobin levels before elective surgery, to introduce measures to reduce perioperative blood loss, and to apply more stringent criteria for transfusion. These developments provided the unique chance to perform a longitudinal study of the effects of unprecedented major demographic changes on blood donation rates and of changes in medical practice on transfusion demand. We began this study in 2005, enrolling all in-hospital recipients of RBC concentrates and all whole blood donors in the entire federal state Mecklenburg-West Pomerania, with 5-year follow-up.18,22 The study's longitudinal design allowed us to compare the projections that were made in 2005 with: (1) the current age distribution of the blood donor and transfusion recipient populations and (2) the impact of demographic changes as well as changes in medical practice on blood donation numbers and transfusion demand within specific age groups. We demonstrate that blood donation numbers closely follow demographic changes, whereas the transfusion demand is strongly influenced by changes in medical practice.
Methods
During the study period, the age restriction for blood donors became more liberal, and now allows more elderly donors to donate blood. On the other hand, West Nile virus infections in Southern Europe and the Zika virus outbreak in South America resulted in exclusion of some donors who had traveled to these regions. The health care infrastructure did not show major changes in the state; thus, the conditions in regard to blood donation and health care provision remained relatively stable during the study period.
We identified for each allogeneic RBC concentrate transfused in the 40 hospitals in the Federal State Mecklenburg-West Pomerania for the years 2005, 2010, and 2015 the following characteristics of the blood donors and blood recipients: age (or date of birth) and sex; date of donation or transfusion; and patient classification (medical, surgical, critically ill/emergency room, pediatrics) from all hospitals and the 4 blood donation services in the state as described18 (Red Cross blood donation service; blood donation service of the University Hospital Rostock; blood donation service of the University Hospital Greifswald; Haema Blutbank [private blood donation service]). Each donated and each transfused RBC was counted as 1 event, respectively. Although the blood supply in Germany is based on regional self-sufficiency, there are exchanges with other blood services; however, this does not affect analysis of the current study because we assessed the donor and recipient populations independently. Even if some RBCs were exported to other regions or imported from other regions for transfusion in Mecklenburg-West Pomerania, this would not change the ratio between donated and transfused RBCs in the state.
Population data in 1-year age groups for males and females were obtained from the population registry for Mecklenburg-West Pomerania for 2005, 2010, and 2015, as was the population projection for 2030.19,23 We then compared the projections that were made in 2005 for the year 2015 with the actual whole blood donation numbers for each age group and the actual transfusion rates per age group in 2015. Assuming constant age-related blood donor frequencies and constant transfusion recipient frequencies equal to 2015 levels, the population data were used to build age- and sex-specific projections of blood demand and supply for each year until 2030.
For comparison with results from other countries, we further calculated age and sex standardized transfusion rates using the World Health Organization (WHO) world standard population.24
Ethics
Exclusively anonymous data were used in the study. The institutional ethics review board of the Universitätsmedizin Greifswald approved the study. The study was performed according to the Declaration of Helsinki.
Results
Development of whole blood donations
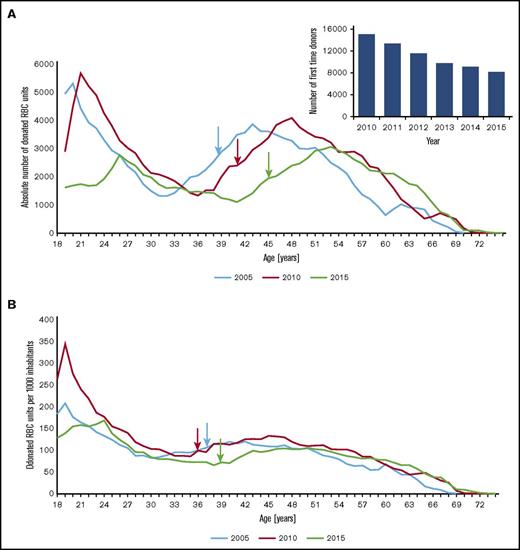
In 2015, the state of Mecklenburg-West Pomerania had 1 081 177 inhabitants in the 18 to 68 year age group, which indicated population decline (−11.6% compared with 2005: 1 223 124; −4.5% compared with 2010: 1 132 628). In 2015, this age group represented 67.1% of the total population (2005: 71.6%). Whole blood donations increased between 2005 (118 418 units) and 2010 (132 291 units) as a result of the activities of a new private blood donation service, and then declined to 97 045 in 2015 (−18% between 2005 and 2015; −26.6% between 2010 to 2015; Figure 2A), rather close to the decrease of −23% predicted in 2005 (91 676 [error 5%]). Between 2005 and 2015, changes in regulation on donor age allowing for more donations from elderly blood donors accounted for 40% of the error in prediction (RBCs donated by blood donors >65 years: 2015, 2150 vs 606 in 2005). Even more pronounced than the total decrease in blood donations is the decrease in first-time donors by 45.6% since 2010 (Figure 2A, inset), despite major efforts to increase donor recruitment by all blood services in the state. Compared with 2005, the decrease in first-time donors was 38%, although the start of the new blood donation service resulted in a strong increase of first-time donors between 2008 and 2010.
Absolute numbers of whole blood donations in 2005, 2010, and 2015. (A) Total whole blood donations by age group in 2005 (blue line), 2010 (red line), and 2015 (green line) per age group. The total numbers strongly decreased in the age groups 18 to 25 years and 36 to 48 years. In addition, the peak age groups of blood donors shifted by 10 years between 2005 and 2015. The inset shows the numbers of first time donors, which decreased between 2010 and 2015 by 45.6%. Arrows correspond to the median age of the donor population in 2005 (39 years), 2010 (41 years), and 2015 (45 years). (B) The rate of blood donations per 1000 subjects per age group showed only minor changes between 2005 and 2015. The substantial increase in blood donations over nearly all age groups between 2005 and 2010 were due to the start of a new blood service, but this effect was transient and no longer present in 2015. Arrows correspond to the median age of the donor population per 1000 inhabitants in 2005 (38 years), 2010 (36 years), and 2015 (39 years). Supplemental Table 2 provides characteristics of the recipient and donor population by type of hospital and type of blood service.
Absolute numbers of whole blood donations in 2005, 2010, and 2015. (A) Total whole blood donations by age group in 2005 (blue line), 2010 (red line), and 2015 (green line) per age group. The total numbers strongly decreased in the age groups 18 to 25 years and 36 to 48 years. In addition, the peak age groups of blood donors shifted by 10 years between 2005 and 2015. The inset shows the numbers of first time donors, which decreased between 2010 and 2015 by 45.6%. Arrows correspond to the median age of the donor population in 2005 (39 years), 2010 (41 years), and 2015 (45 years). (B) The rate of blood donations per 1000 subjects per age group showed only minor changes between 2005 and 2015. The substantial increase in blood donations over nearly all age groups between 2005 and 2010 were due to the start of a new blood service, but this effect was transient and no longer present in 2015. Arrows correspond to the median age of the donor population per 1000 inhabitants in 2005 (38 years), 2010 (36 years), and 2015 (39 years). Supplemental Table 2 provides characteristics of the recipient and donor population by type of hospital and type of blood service.
Median donor age was 45 years (an increase of 5.2 years compared with 2005: 39.8 years), with 45.0% (2005: 48.0%) donations from female donors. In comparison with 2005, the peaks of age groups with the highest numbers of blood donations shifted by approximately 10 years to older age groups with 2 peaks, 1 in the 25 to 30 years age group (13.9% of all donations [2010: 18.1%]) and 1 in 50 to 55 years age group (17.9% [2010: 11.0%] of all donations), respectively (Figure 2A).
Blood donation rates per 1000 inhabitants first increased between 2005 and 2010 in younger age groups as a result of the activities of a new private blood donation service, and then declined in 2015. The less pronounced relative changes in blood donation numbers per 1000 inhabitants of the respective age groups (Figure 2B) (donation rates in the age group 18 to 30: 140.5/1000 population in 2005 vs 125.6/1000 population in 2015; −10.6%, Table 1) further underscores that the decrease in blood donations parallels the demographic change.
In-hospital transfusion of RBCs in 2015
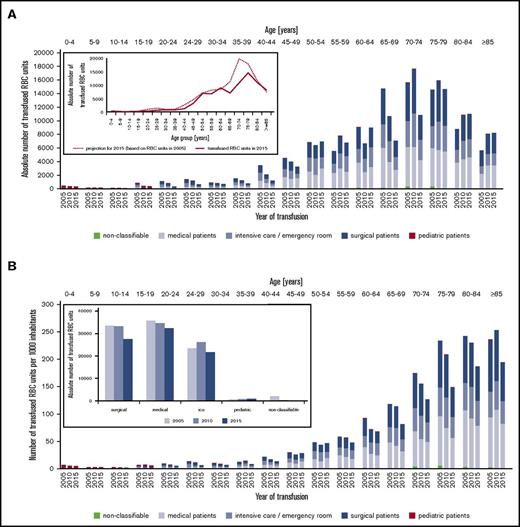
In contrast to the reduction in blood donation numbers, in-hospital transfusion demand remained relatively constant between 2005 (95 455) and 2010 (95 200), and decreased in 2015 (82 591; −13.5% compared with 2005, Figure 3A). The actual transfusion demand in 2015 was 21.3% lower than the transfusion demand projected in 2005 for 2015 (104 880; Figure 3A, inset).
Use of RBC transfusions by age and patient classification for 2015, 2010, and 2005. (A) Use of RBCs by age and patient type shows an increase in the absolute transfusion demand in the age group older than 75 years because of the increase of the population number in this age group (hospital inpatients and outpatients; patients transfused in private praxis are not included because of insufficient information on patient age). Inset: The dotted line shows the number of transfusion demands per age group projected in 2005 based on the transfusion rates in 2005 and the anticipated demographic changes. Although the demographic change followed the prediction, the number of transfused RBCs per age group (solid line) was much lower because of changes in medical practice. The actual transfusion demand in 2015 was 21% lower than projected in 2005. Calculation is based on the age distribution in 2005, transfusion rates in 2005, and the projected age distribution in 2015. (B) The transfusion rates per 1000 subjects of the population decreased in all age groups between 2005 and 2015. Transfusion rates in 2015: 0 to 19 years, 4.2/1000 (2005: 5.7/1000; P < .001); 20 to 39 years, 7.2/1000 (2005: 11.6/1000; P < .001); 40 to 59 years, 37.2/1000 (2005: 37.6/1000; P = .285); 60 to 79 years, 103.4/1000 (2005:144.2/1000; P < .001); ≥80 years, 190.1/1000 (2005: 239.7/1000; P < .001). Inset: The transfusion demand decreased in all patient groups (surgical, medical, and intensive care unit patients), whereas it remained stable at a very low level in pediatric patients.
Use of RBC transfusions by age and patient classification for 2015, 2010, and 2005. (A) Use of RBCs by age and patient type shows an increase in the absolute transfusion demand in the age group older than 75 years because of the increase of the population number in this age group (hospital inpatients and outpatients; patients transfused in private praxis are not included because of insufficient information on patient age). Inset: The dotted line shows the number of transfusion demands per age group projected in 2005 based on the transfusion rates in 2005 and the anticipated demographic changes. Although the demographic change followed the prediction, the number of transfused RBCs per age group (solid line) was much lower because of changes in medical practice. The actual transfusion demand in 2015 was 21% lower than projected in 2005. Calculation is based on the age distribution in 2005, transfusion rates in 2005, and the projected age distribution in 2015. (B) The transfusion rates per 1000 subjects of the population decreased in all age groups between 2005 and 2015. Transfusion rates in 2015: 0 to 19 years, 4.2/1000 (2005: 5.7/1000; P < .001); 20 to 39 years, 7.2/1000 (2005: 11.6/1000; P < .001); 40 to 59 years, 37.2/1000 (2005: 37.6/1000; P = .285); 60 to 79 years, 103.4/1000 (2005:144.2/1000; P < .001); ≥80 years, 190.1/1000 (2005: 239.7/1000; P < .001). Inset: The transfusion demand decreased in all patient groups (surgical, medical, and intensive care unit patients), whereas it remained stable at a very low level in pediatric patients.
In 2015, the Mecklenburg-West Pomerania state had 1 612 362 (as of 31 December 2015) inhabitants. Including the nonhospital outpatient sector (13 521 transfusions), the absolute transfusion rate per 1000 inhabitants in the state was 59.6 RBCs/1000 (in 2005: 62.2/1000). Age distributions vary widely between populations. To allow international comparisons, the WHO has introduced an age-adjusted standard population.24 Normalization of the RBC transfusion rate per 1000 WHO standard population results in an age-normalized transfusion rate of 23.920 RBCs per 1000 population (compared with 31.979 in 2005). Females received 43.24% of RBCs transfused, even though they composed 50.52% of the population. 62.6% of all transfusions were given to patient ≥65 years (2005: 60.3%; Figure 3A). Median patient age was 71.6 years (female: 74.3 years; male: 68.9 years). Only one-third of RBCs were transfused to surgical patients (Table 2; Figure 3B, inset).
The absolute numbers of transfusions (Figure 3A) show a decrease of transfusions in nearly all age groups and in all patient groups (Figure 3B, inset) between 2005 and 2015. When calculated as transfusions per 1000 inhabitants (Figure 3B), it becomes obvious that the absolute decrease occurred primarily in the age group >60 years, although the relative decrease was even more pronounced in the younger age groups.
Projection of the demand for RBC transfusions and whole blood donations in 2030
The potential donor population (18 to 68 years) in Mecklenburg-West Pomerania is projected to decrease further by 12.2% until 2030, with a decrease in total blood donations of 31.7% compared with 2005 resulting in a total donation number of 80 827 RBCs. On the other hand, the overall demand for RBCs is projected to remain rather constant, with ∼99 200 (in-hospital and outpatient transfusions). These 2 combined effects will result by 2030 in a shortfall of 18 373 RBCs (or 22% of the projected available units). This projection, however, will only materialize if there are no major changes in donor population or medical practice (indeed, it is more likely that changes in medical practice will occur). Therefore, monitoring of blood donation rates and transfusion demand per age groups will be increasingly important.
Discussion
This is the first study showing that the future blood supply correlates closely with demographic characteristics of a population. This was possible because our study covered a period with unprecedented changes in the demography of the blood donor population without a parallel catastrophic event worsening living conditions. We could measure the effects of the unique rapid and >50% decline in birth rates in eastern Germany after German reunification on the blood donation rates over 10 years. In 2008 to 2009, children born in 1990 and 1991 became 18 years old, thereby entering the eligible donor population. We found that the blood donation rates closely followed the demographic changes. We also observed that the age distribution of our donors is no longer static but shifts constantly toward older age groups, in parallel with aging of the baby boom generation. This will cause a further reduction in blood donations, when the donors in the age groups 50 to 60 years will no longer be able to donate blood for health reasons.
In addition, we made an interesting and potentially important observation. When we analyzed the first follow-up data in 2010,25 we found an increase in blood donation numbers compared with 2005 rather than the projected decrease. This was primarily because of the new activities of a private blood donation service, which started to operate in the state in 2008. We first interpreted this increase as evidence for the resilience of the blood donation system “responding” to the demographic changes.25 However, this effect was nearly gone in 2015. This strongly indicates that increased activities of blood donation services only transiently increase blood donation numbers and that the resilience of the system is potentially lower than anticipated. Although the transfusion demand decreased in parallel to the decrease in blood donations, these 2 developments happened, coincidently, at the same time. The decrease in blood donations was not intended by our blood services as an attempt to adjust the donation rates to the reduced demand. Indeed, in 2015, the difference between donated and transfused RBCs in the state was 0.96%. This is an unrealistic low wastage rate and indicates already an insufficient self-supply.
Our findings are highly relevant for most Western societies, all of which will be affected by major demographic changes, although to different extents, but in general will occur later than in the region in Mecklenburg-West Pomerania (Figure 1; supplemental Table 1). The effects observed in this study can be seen as a model for what will happen about 10 to 15 years later in many other regions of Europe and North America.
In parallel, the baby boom generation is aging. This will cause a rapid increase in those ≥65 years of age between 2020 and 2030. Because this age group accounted for more than 60% of the demand in RBCs in 2015, an absolute increase in this population will likely result in an absolute increase of RBC demand. Ali et al17 elegantly showed that in many European countries as well as in Canada and the United States the ratio between the population at age eligible for blood donation and the those not eligible for blood donation was most favorable around 2000 through 2010. The authors assume that donor recruitment will become more difficult in the future. Drackley et al26 reported that the baby boom generation is soon leaving the donor pool in Canada, which will cause a decrease in the number of blood donors and an increasing proportion of age groups >65 years, who more likely require blood transfusions. Regarding Ontario, the authors predicted a future mismatch between demand and supply when assuming constant donation and transfusion rates. Volken et al27 analyzed the situation for Switzerland and found decreasing numbers of whole blood donations; however, they identified declining donor retention rates rather than demographic changes as the main cause. This trend is compensated for by changes in clinical practice, but may lead to a supply demand mismatch of RBCs in Switzerland as demographic changes become more pronounced. The decrease in the transfusion demand also influenced blood donation rates in Iceland, where Jóhannsdóttir et al28 found a decreasing number of blood donations, simply because less blood is needed.
In Japan, a country with pronounced demographic changes, Akita et al29 reported an increase in blood donation rates during recent years, which is the opposite of what we found in our study. However, Japan experienced a preceding decline in blood donation rates of nearly 40% between 2003 and 2007.
All Western countries currently experience increased immigration rates. Lattimore et al30 studied the important issue of changes in the population resulting from immigration and its impact on blood donations. The immigrant population is currently underrepresented in the donor pool; therefore, beside demographic factors, changes within the donor population should be monitored to adjust for future recruitment strategies. In the state of Mecklenburg-West Pomerania, immigrants account for <2% of the population and have therefore only a minor impact on the overall blood donation rates.
The transfusion demand depends on the population structure as well as on medical practice. In 2010, Borkent-Raven et al31 showed in the Netherlands that the demand for RBCs does not follow the demographic change, rather it is strongly influenced by changes in medical practice. This resulted in a lower than expected transfusion demand during the past decade. Our study clearly supports that the transfusion demand cannot be reliably calculated based on demographic data. The actual demand in 2015 was more than 20% less than projected based on the transfusion demand in 2005. This is a consequence of a major change in transfusion practice as a response to the “patient blood management” initiative and to several prospective randomized trials showing that a restrictive transfusion regimen is not inferior compared with a liberal transfusion regimen in many patient groups.5 It is, however, unlikely that the trend in reduced red blood cell demand will continue. Most hospitals already follow rather restrictive transfusion guidelines with low pretransfusion hemoglobin thresholds.
Germany has a still relatively high blood use per inhabitant compared with other European countries, Canada, or Australia. However, transfusion rates differ between age groups. Therefore any comparisons should be based on the WHO world standard population24 (ie, calculating the transfusion demand using a standardized age structure, rather than describing blood transfusion per 1000 inhabitants without considering the age group of the recipients). Currently, these data are not available for most countries. Medical practice differs between countries and medical systems. It would be highly desirable to have data on the blood product use adjusted for age groups, which would allow more reliable benchmarking between different health care systems.
The data of the present study provide strong evidence to suggest that changes in the proportion of donors that donate blood (eg, through improved recruitment) and changes in patient blood use (eg, patient blood management) are the most important drivers of the blood supply, and that economic expediency that requires matching the blood supply with patient demand and minimizing waste, is likely to be the major driving force in the future.
For the next 20 years, the period with the most pronounced changes in the demographic structure of the blood donor population as well as the blood recipient population in Western societies, the age structure of blood recipients and their transfusion demand should be regularly monitored to be able to predict changes in the transfusion demand, whereas the blood donation rate may be calculated based on the demographic changes. This will allow the development of strategies to secure transfusion safety by preventing blood shortages, but also overproduction of blood components.
The full-text version of this article contains a data supplement.
Acknowledgments
The authors thank the following individuals and institutions: S. Scriba, Sozialministerium of Mecklenburg-West Pomerania; A. Crusius, President of the Landesärztekammer (Board of Physicians) Mecklenburg-West Pomerania; the Krankenhausgesellschaft (Hospital Society) Mecklenburg-West Pomerania; the Red Cross blood donation service Mecklenburg-Vorpommern; the blood donation service of the University Hospital Rostock; Haema Blutbank, blood donation service of the University Hospital Greifswald; and all 40 participating hospitals (AMEOS-Klinikum Ueckermünde und Anklam, ASKLEPIOS Klinik Parchim, ASKLEPIOS Klinik Pasewalk GmbH, Bodden-Kliniken Ribnitz-Damgarten GmbH, Dietrich-Bonhoeffer-Klinikum Neubrandenburg, Malchin und Altentreptow, Deutsches Rotes Kreuz [DRK]–Krankenhaus Grevesmühlen gGmbH, DRK-Krankenhaus Grimmen GmbH, DRK-Krankenhaus Mecklenburg-Strelitz gGmbH, DRK-Krankenhaus Teterow gGmbH, Universitätsklinikum Greifswald der Ernst-Moritz-Arndt-Universität Greifswald, Evangelisches Krankenhaus Bethanien gGmbH in Greifswald, HELIOS-Hanseklinikum Stralsund GmbH, HELIOS Kliniken Schwerin, KMG Klinik Boizenburg GmbH, Tagesklinik für Kinder und Jugendpsychiatrie, Psychosomatik und Psychotherapie in Rostock, Klinik Amsee GmbH in Waren an der Müritz, Universitätsklinikum Rostock, Klinikum Karlsburg–Herz und Diabeteszentrum der Klinikgruppe Guth GmbH & Co. KG, Klinikum Südstadt Rostock, KMG Klinikum Güstrow GmbH, MediClin Krankenhaus am Crivitzer See in Crivitz, Krankenhaus Bad Doberan GmbH, MediClin Krankenhaus Plau am See, Kreiskrankenhaus Demmin GmbH, Westmecklenburg Klinikum Helene von Bülow GmbH Hagenow und Ludwigslust, Kreiskrankenhaus Wolgast gGmbH, MediClin Müritz-Klinikum in Waren an der Müritz, BDH-Klinik Greifswald gGmbH–Neurologisches Rehabilitationszentrum und Querschnittgelähmtenzentrum, Sana-Krankenhaus Rügen GmbH in Bergen, Sana HANSE-Klinikum Wismar, Tagesklinik für Psychiatrie/Psychotherapie in Rostock, Warnow-Klinik Bützow gGmbH, Zentrum für medizinische Rehabilitation Fachklinik Waldeck, HELIOS Klinik Leezen GmbH, Fachklinik für Onkologie und Ganzheitsmedizin Graal-Müritz, SHORT CARE Klinik Greifswald).
This study was supported by research funding from the Universitätsmedizin Greifswald.
Authorship
Contribution: W.H. and A.G. conceived and designed the study; K.W., L.S., U.A., V.K., N.G., K.S., D.G., W.S., and A.G. acquired, analyzed, or interpreted the data; K.W., L.S., W.H., and A.G. drafted the article or provided critical revision for important intellectual content; K.W., L.S., U.A., D.G., K.S., W.S., N.G., V.K., W.H., and A.G. provided final approval of the version to be published; and all authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the article are appropriately investigated and resolved.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Andreas Greinacher, Institut für Immunologie und Transfusionsmedizin, Universitätsmedizin Greifswald, Sauerbruchstraße, D-17489 Greifswald, Germany; e-mail: greinach@uni-greifswald.de.
References
Author notes
A.G. and K.W. contributed equally to this work.