Abstract
Since the approval of horse antithymocyte globulin (ATG) decades ago, there was a long hiatus in therapies with activity in severe aplastic anemia (SAA). This scenario changed in 2014 when eltrombopag, a thrombopoietin receptor agonist, was approved for SAA after an insufficient response to initial immunosuppressive therapy (IST). The basis for this approval was the observation of single-agent activity of eltrombopag in this patient population, where 40% to 50% recovered blood counts at times involving >1 lineage. The achievement of transfusion independence confirmed the clinical benefit of this approach. Increase in marrow cellularity and CD34+ cells suggested a recovery to a more functioning bone marrow. Further in its development, eltrombopag was associated with standard horse ATG plus cyclosporine in first line, producing increases in overall (at about 90%) and complete response rates (at about 40%) and leading to transfusion independence and excellent survival. Interestingly, best results were observed when all drugs were started simultaneously. The cumulative incidence of clonal cytogenetic abnormalities to date has compared favorably with the vast experience with IST alone in SAA. Longer follow-up will help in define these long-term risks. In this review, the development of eltrombopag in SAA will be discussed.
Introduction
For many years, the focus in the clinical development of novel nontransplant therapies for severe aplastic anemia (SAA) has been on intensifying immunosuppressive therapy (IST). The accumulation of data supporting an immune pathogenesis along with large prospective trials defining the success of IST in SAA formed the rationale for this development.1 Earlier efforts in which immunosuppression was increased led to higher hematologic response rates. Although hematologic recovery with antithymocyte globulin (ATG) was observed in 40% to 50%, the addition of cyclosporine (CsA) increased this rate to 60% to 70%.2-4 The ATG formulation most studied was that of horse serum, which is only a modest immunosuppressant.1 This opened the possibility of intensifying immunosuppression further by adding a third drug to the horse ATG/CsA or substituting horse ATG for more lymphocytotoxic agents, such as cyclophosphamide, rabbit ATG, or alemtuzumab.
Indeed, this hypothesis was investigated in prospective studies, yielding, surprisingly, a series of disappointing results. The principal end point in these studies was an increase in the hematologic response rate, which is a powerful surrogate for survival in SAA.5 The additions of mycophenolate and later, sirolimus to horse ATG/CsA were “negative” (that is, there was no increase in the response rates).6,7 A CsA taper course beyond 6 months did not increase the response or ultimately prevent relapses from occurring.8 The substitution of horse ATG for cyclophosphamide, rabbit ATG, and alemtuzumab was equally disappointing in prospective comparative studies due to increased toxicity and/or a lower hematologic response rate.9-15 In particular, results with rabbit ATG/CsA were unexpected and unanticipated given the activity of this regimen in relapsed and refractory SAA.16,17 This difference in efficacy does not seem to be related to rabbit ATG dosing.18,19 These studies led to the notion that a “ceiling” had been reached in regard to exploring more intense immunosuppressive regimens in SAA.20 Therefore, the standard immunosuppressive regimen still remains horse ATG/CsA in SAA.21
The reasons for the lack of response to IST in SAA are not clearly understood, but prevailing notions included autoreactive T cells that may survive IST and/or significant destruction of the more primitive hematopoietic compartment, hindering the sprout of progenitor cells after the autoimmune insult was controlled. In a minority of cases, a cryptic underlying genetic defect could contribute to unresponsiveness to IST, and other approaches may be better suited in this selected group.22 The observation that the hematologic response rate did not improve despite more intense IST regimens argued against the existence of autoreactive cells not amenable to immunosuppression. Thus, the notion of an insufficient marrow unable to recover from a severe stem cell deficit became more preponderant. Unfortunately, efforts to stimulate this primitive compartment with growth factors, such as erythropoietin, granulocyte colony-stimulating factor (G-CSF), stem cell factor, and interleukins among others, have been to no avail.23-25 Approximately 10 years ago, agonists of the thrombopoietin (Tpo) receptor, which stimulated megakaryocytes to produce platelets, were approved for immune thrombocytopenia. These agents led to platelet count recovery in the majority of refractory cases of immune thrombocytopenia.26
Apart from erythropoietin and G-CSF, Tpo has distinct properties that could be effective in stimulating hematopoietic stem cells (HSCs). This hormone, first cloned in 1994, was initially associated with megakaryocyte stimulation and platelet production.27-30 However, in vitro and experimental data implicated that Tpo also had an important role in stem cell proliferation and maintenance. First, unlike erythropoietin and G-CSF, the Tpo receptor is expressed in stem cells.31 Second, in Tpo receptor knockout models, aside from megakaryocytopenia and thrombocytopenia, significant reductions in HSCs were observed.32-35 Third, Tpo is commonly used along with other growth factors and interleukins in culture to stimulate stem cells in vitro.31 Fourth, in a rare form of marrow failure, amegakaryocytic thrombocytopenia, mutations in the Tpo receptor (c-MPL) resulted in multilineage cytopenias and significant HSC deficit in humans.36-39 Thus, a Tpo mimetic could in theory be active in ameliorating marrow function in aplastic anemia and associated disorders. The very elevated endogenous Tpo serum levels in SAA patients raised concerns of the ineffectiveness of this approach.40,41 Notwithstanding, a prospective dose escalation study was developed with eltrombopag in SAA patients with an insufficient response to initial IST. Later, due to the single-agent activity observed in these earlier studies, eltrombopag was combined with IST in front line.
Clinical development
Eltrombopag in refractory SAA
To overcome the high endogenous Tpo serum level and possible resistance to this approach, single-agent eltrombopag was developed in a phase 1/2 study, where 25 SAA patients unresponsive to initial IST received escalating doses starting at 50 mg up to 150 mg in 25-mg dose increment every 2 weeks (ramp-up study).42 The primary end point was hematologic response at 3 to 4 months. Overall, 11 (44%) achieved a hematologic response, of which 9 were in platelets, 9 were in neutrophil, and 6 were in the erythroid lineages (some patients had response in >1 lineage). In some responders, there was a corresponding increase in marrow cellularity, which along with the multilineage recoveries, suggested an HSC stimulation of eltrombopag. In an extension cohort of the ramp-up study (totaling 43 patients), the response rate remained at about 40%, and multilineage improvements continued to be seen.43 Clonal evolution was observed in 8 patients, including 5 with chromosome 7 loss or partial deletion. The cumulative incidence of clonal evolution in this refractory cohort was about 15% to 20%, which was similar to what has been reported historically.43 Of interest, most of the karyotype abnormalities occurred early—usually with the first 6 months of starting therapy. Eltrombopag was well tolerated, with principal toxicities being upper respiratory infection, fever, and musculoskeletal pain.42,43 There were no cases of significant increase in marrow reticulin deposition or thrombosis. In some patients who experienced a more robust hematologic response, drug discontinuation was possible after a quick taper, with most not relapsing.43 These studies led to the approval of eltrombopag as a single agent in SAA in patients with an insufficient response to initial IST.
In a follow-up phase 2 study by Winkler et al,44 39 patients with refractory SAA received a starting dose of eltrombopag of 150 mg (without the ramp up) for 6 months (fixed dose study). This design was chosen, because most responses in the ramp-up study occurred at 150 mg, suggesting it to be the more active dose. The duration of therapy was extended from 3 or 4 months (original ramp-up study) to 6 months (fixed dose study) to capture responses that may occur up to 6 months.44 These data were only presented in abstract form at the time of this writing. In total, 19 of 39 (49%) met criteria for hematologic response at 6 months. Compared with the ramp-up study, responses involving >1 lineage were more frequent in the fixed dose study by 6 months; they were observed in most responders and almost always equated to achieving transfusion independence. Of the 18 patients who met criteria for a robust response after a median follow-up of 12 months on drug, 13 had eltrombopag discontinued without a significant drop in blood counts. Of the remaining who relapsed, eltrombopag was successfully reinstituted with recovery of blood counts.
In this cohort, 6 of 39 developed cytogenetic abnormalities. Interestingly, all occurred early—within the first 6 months after the drug was initiated. These earlier cytogenetic abnormalities suggest that eltrombopag might be stimulating marrow preexistent clones, leading to their apparition in earlier evaluations within the first 6 months. Although the cumulative incidence of clonal evolution has not differed to date from historical experience, the earlier kinetics suggest a causal relation. Whole-exome sequencing performed at baseline has not correlated with important outcomes of hematologic response or clonal evolution.44-46 Full reporting of these data will provide additional insights into the activity of eltrombopag in refractory SAA.
In all, the hematologic response rate with eltrombopag in second-line SAA patients with an insufficient response to initial IST is about 40% to 50%. A starting dose of 150 mg for 6 months seems optimal given the quicker and more robust hematologic recovery, which has allowed successful discontinuation of eltrombopag in most responders. Abnormal cytogenetics identified in ∼15% to 20% to date is in accordance to date with the vast historical experience of IST regimens without eltrombopag in SAA.1 Notwithstanding, cytogenetic abnormalities have been observed in the historical cohort up to 10 years; thus, a longer follow-up in eltrombopag-treated patients will be important in defining this risk.
Eltrombopag combined with IST in first line
The next steps in development combined eltrombopag with the most active IST regimen in SAA, horse ATG/CsA, in patients not suitable for hematopoietic stem cell transplantation (HSCT) upfront (lack of donor, advanced age, comorbidities, and/or patient preference).47 This 3-drug regimen, which combined 2 immunosuppressants and a marrow stimulatory agent, was developed at the National Institutes of Health (NIH) to investigate its feasibility in terms of safety as well as address the limitations of horse ATG/CsA alone, which are namely a “ceiling” response rate of 60% to 70%, with only a minority being complete (about 10% historically); rates of relapse (in about 1/3 of responders); and clonal evolution (∼15%) long term.1 Thus, a primary end point of a complete response at 6 months of 30% or higher was chosen given its correlation with a better survival and fewer late events.1,5 Given the optimal dosing of the pilot trials, a starting dose of 150 mg was chosen to be combined with IST for a total of 6 months.47 Liver enzyme abnormalities are common with horse ATG/CsA, which is one of the toxicities with eltrombopag observed in 10% of patients.48 Thus, the initiation of eltrombopag was delayed by 2 weeks after IST until the liver enzymes had normalized or near normalized in the initial cohort of 30 patients (cohort 1). In this group, the overall hematologic response was 80%, of which 33% were complete. In a subsequent cohort of 31 patients (cohort 2), eltrombopag was also started on day 14, and duration was abbreviated to 3 months given concerns for clonal evolution with longer-term use of this agent. In this cohort 2, the response rates at 6 months were 87% overall and 26% complete. The small decline in the complete response and some loss of responses between 3 and 6 months led to the resumption of the 6-month course in a subsequent cohort of 31 patients (cohort 3). In this group, eltrombopag was started on day 1 along with the IST given the lightening of the concern for increase hepatotoxicity with the combination based on the experience of the prior 2 cohorts. In this group, the overall hematologic response rate was 95%, being complete in 58% at 6 months. The results of this latest cohort 3 represented a nearly 6 times increase in historical complete response rates (of about 10%) and a near doubling of the complete response rate compared with cohorts 1 and 2. The simultaneous initiation of all drugs on day 1 seemed to be optimal. In this study across all cohorts, there was a quality of life gain from the more rapid recovery of blood counts and the decreases in transfusion burden and hospital visits.47 Ancillary laboratory assays showed an increase in marrow progenitor cells in vitro after therapy compared with baseline samples, indicating recovery to a more normal functioning bone marrow.47 The overall hematologic response rate at 6 months for all cohorts (n = 92) was 87%, with 39% being complete, which achieved the primary end point of the protocol of a complete response rate of 30% or higher at 6 months.
Long-term events of relapse and clonal evolution have been reported in the upfront 3-drug regimen study; however, follow-up has been relatively short (median of 18 months). In cohort 1 and part of cohort 2, the CsA was discontinued at 6 months; this resulted in a relapse rate of 54%, which was higher than historically observed with IST alone.49 Thus, the protocol was amended in the latter part of cohort 2 to allow for a continued fixed low-dose CsA (2 mg/kg) after 6 months (for a total of 2 years), resulting in a decrease in the relapse rate to about 15%.47 The dose of 2 mg/kg was chosen based on prior experience that associated this dose with a decrease in relapse rate.8 To date, the 2-year cumulative incidence of clonal evolution rate is about 8%, which compares favorably with the historical data of IST without eltrombopag of ∼8% at this time point.47 Of note, most cytogenetic abnormalities have been detected early in the first 6 months (5 of 7), such as was observed in the initial pilot studies of eltrombopag in refractory SAA. In some cases, karyotype abnormalities did not correlate with poor counts or marrow dysplasia, at times being transient. Ancillary molecular analysis of marrow cells before treatment did not associate with hematologic response or risk of clonal evolution. This observation is in accordance with prior reports in which pretreatment mutational status was not universally associated with outcomes.45,50 After a median follow-up of 18 months, the overall survival was 97% (95% confidence interval, 94-100) in all cohorts and 99% (95% confidence interval, 97-100) when data were censored for stem cell transplantation.47
The results with the use of eltrombopag in association with horse ATG/CsA are very encouraging, although some questions remain. First, the durability of response with the 3-drug regimen (without relapse and clonal evolution) will be of great relevance, and it will be defined with longer-term follow-up.51 Formal presentation of these results in the ∼150 patients treated with the 3-drug regimen by 2018 from the original NIH study is anticipated, which will better define the activity and safety of this regimen. Conversely, the role of the 3-drug regimen in pediatrics is yet unclear given the already higher overall and complete response rates with IST alone in this group and the small number of children included in the original reporting. Thus, a pediatric subset analysis of the NIH trial and dedicated studies in children will be important to establish its role in this patient population. Second, the duration of CsA beyond 2 years has not yet been defined. Currently in the NIH trial, CsA is administered up to 2 years, and its interruption at this time point is being investigated in a protocol comparing a CsA taper with its substitution for a tolerizing immunosuppressant (sirolimus; NCT02979873). Third, confirmation of these results in separate prospective cohorts will further strengthen the evidence and allow for incorporation of these novel regimens in routine clinical practice. The European Group for Blood and Marrow Transplantation (EBMT) is conducting a prospective, randomized, multicenter trial comparing horse ATG/CsA with and without eltrombopag (RACE study; NCT02099747), which will provide important confirmatory and comparative data on horse ATG/CsA alone. Of note, in the RACE study, eltrombopag is initiated on day 14 after IST, which was based on the initial cohorts of the American NIH experience. Given the substantial increase in complete responders when all 3 drugs were administered simultaneously on day 1 (cohort 3 of the NIH study), the European data may not reproduce the best results seen in the American trial. Nevertheless, preliminary results of the RACE study are anticipated in the next 1 to 2 years, as accrual completion of the 200-patient study is anticipated by the end of 2018. Importantly, this trial, given its direct comparison design, will more definitively define the clonal evolution risk between eltrombopag- and noneltrombopag-containing IST regimens as initial therapy in SAA.
How eltrombopag is acting in SAA
The initial goal in using eltrombopag in SAA was to stimulate residual stem cells to proliferate and improve hematopoiesis and blood counts. Originally, a platelet response was sought given that frequent platelet transfusions (once or twice a week) tend to be more limiting for patients with persistent cytopenias and impact quality of life. The multilineage blood count recoveries, increase in marrow cellularity, and increase in CD34+ marrow cells in exploratory experiments indeed indicated that such an effect was taking place. The very high endogenous Tpo levels did not seem to hinder patient’s ability to recover, unlike what is observed in other marrow failure settings, such as in myelodysplastic syndrome, where exogenous erythropoietin therapy is largely ineffective when endogenous levels of erythropoietin are >200 to 500 mU/mL.52 Thus, other effects of eltrombopag could be at play in SAA, contributing to its activity.
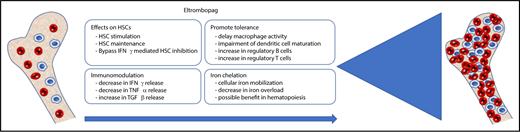
Since its approval for immune thrombocytopenic purpura (ITP) and later SAA, important immunomodulatory properties have been reported with eltrombopag that may contribute to its positive net effect in immunologically mediated cytopenias. In SAA, there are important immune dysregulations that include a deficit of regulatory T cells; increased expression of proinflammatory cytokines and associated proteins (TH1 and TH17); increase in interleukin-2, interferon-γ, and tumor necrosis factor-α (TNFα) secretion; and expansion of oligoclonal CD8+ cytotoxic T cells among others.1,49,53-63 Eltrombopag could be addressing some of these abnormalities directly or indirectly by promoting a more tolerizing environment via an increase in regulatory T and B cells, secretion of transforming growth factor-β, impairment of dendritic cell differentiation, and a decreased release of interferon-γ and TNFα.64-66 These effects have been primarily described in immune thrombocytopenia, although it is plausible that similar actions are also occurring in SAA. Moreover, platelets in themselves may have immunomodulatory properties that contribute to the immune control in aplastic anemia (AA) and overall blood count recovery.66-68 Distinctly, a novel mechanism has been recently presented by Alvarado et al69 (in abstract form only at the time of this writing), showing that eltrombopag can evade the inhibitory effect of interferon-γ on HSCs and signal downstream of c-MPL to net a stimulatory effect. In contrast, in the same experimental design, native Tpo was inhibited by interferon-γ by forming a heterodimer-hindering signaling through c-MPL and subsequent target cell activation.69 The complete report of this observation is anticipated, which will shed additional insights into these mechanisms. Furthermore, eltrombopag has in its structure a chelator backbone that mobilizes intracellular iron, resulting in a decrease in total iron burden.70 Reports in pediatric ITP and AA have shown a progressive decline in ferritin levels with continued use of eltrombopag.71,72 Although there are reports suggesting a benefit of iron chelation in ameliorating cytopenias in AA, its direct benefit has yet to be established.73-76 Nevertheless, reducing total body iron burden in polytransfused patients is desirable to avoid long-term end organ complications and possibly, contribute to marrow recovery. Thus, the mechanisms by which eltrombopag improves marrow function in AA are likely to be multifactorial, and they are still being elucidated (Figure 1). These mechanisms, of course, may also be beneficial in other forms of marrow failure syndromes, myelodysplastic syndromes, poststem cell transplantation, cytopenias related to inflammatory and infectious conditions, and chemotherapy-induced thrombocytopenia among others. Indeed, several reports and clinical protocols are in development exploring this possibility. In AA, studies are ongoing exploring the use of eltrombopag and romiplostim in different forms of marrow failure in various doses either alone or in combination with different immunosuppressants (Table 1). Although data are more limited in SAA, romiplostim at higher weekly doses (10 μg/kg) seems effective, and even higher doses are currently under investigation.77,78
Different proposed mechanisms by which eltrombopag is improving hematopoiesis in aplastic anemia. IFNγ, interferon-γ; TGFβ, transforming growth factor-β.
Different proposed mechanisms by which eltrombopag is improving hematopoiesis in aplastic anemia. IFNγ, interferon-γ; TGFβ, transforming growth factor-β.
Practical considerations
With all eltrombopag-containing regimens (upfront and in refractory settings), continued follow-up will provide safety and efficacy data and define longer-term risks of relapse and clonal evolution.51 “Real world” data thus far have confirmed the results reported in the earlier clinical trials in SAA.77,79,80 Several practical considerations will also emerge from these observations. For example, eltrombopag was developed as a single agent in refractory SAA; however, its combination with CsA is common in the “real world.” Given the good tolerability of this combination reported to date, it is rational to use such a combination with the expectation of complementary or even synergistic mechanisms of action. However, the proven benefit of the combination of eltrombopag plus CsA vs eltrombopag alone in the refractory setting has not yet been established. In East Asian patients, eltrombopag should be administered at lower doses (75–100 mg) given known population pharmacokinetic dynamics. However, some reports recently have proposed that higher doses (up to 300 mg) are tolerated and efficacious in East Asians, requiring additional studies for confirmation.77,80 Liver enzymes should be monitored in all patients, and dosage should adjusted according to published protocols.42,43,47 Mild to moderate indirect bilirubin increase is common and usually of no consequence to the patient.
Frequency of bone marrow sampling in clinical trials included baseline; 3, 6, and 12 months; and yearly thereafter given concerns for clonal evolution. This practice of more frequent sampling early on in therapy permits detection of cytogenetic abnormalities while patients are on therapy during the first 6 months. If no response is observed at 6 months on the optimal dose (150 mg), eltrombopag should be discontinued given risks/benefits and the possible promotion of clonal evolution with its continued use long term. Among responders, attempt to discontinue eltrombopag should be sought especially if blood count recovery is robust and/or counts have been stable for at least 6 months. It is very important to follow dietary restrictions strictly associated with eltrombopag to derive optimal drug activity, because drug levels cannot be monitored.
The adoption of eltrombopag with standard horse ATG/CsA upfront is evolving, and its role should be better defined in ongoing studies (Table 1). The efficacy of combining eltrombopag with rabbit ATG/CsA or CsA alone (ATG-free regimen) is also being elucidated in these trials. Reducing the refractory pool of patients to initial IST and achieving transfusion independence quicker are desirable with the 3-drug combination (horse ATG/CsA/eltrombopag). Its benefit as it relates to standard IST alone and HSCT (in certain age groups; for example, 20-40 years) is of interest, and it is being elucidated with ongoing studies, the results of which are anticipated in coming months and years. Also, the use of the 3-drug combination as a second salvage course of therapy in relapse and refractory patients treated initially with IST alone is intuitive, although it has not yet been defined in this setting. Another question still open is if patients unresponsive to the initial 3-drug regimen benefit from a second course of IST.
Conclusion
Eltrombopag represents an important addition to the armamentarium in AA that, for several decades, lacked approval of new therapies. Eltrombopag is currently approved as a single agent in patients with an insufficient response to initial immunosuppression. Regulatory approval of the combination with horse ATG/CsA is anticipated in the United States given the high overall and complete response rates with this regimen. The immune and nonimmune properties of eltrombopag may be complementary or synergize with those of immunosuppressive therapies, contributing to a more rapid and robust recovery of blood counts when given in combination in SAA. Thus, combining therapies with different modes of action in improving hematopoiesis is proving to be beneficial in SAA. The addition of androgens and possibly, other growth factors (G-CSF and erythropoietin) to the 3-drug regimen may further improve marrow function and blood count recovery, and these possibilities are likely to be investigated in clinical research protocols. In coming years, more will be learned from these trials, and real word evidence (in unselected patients) will further solidify the role of the Tpo receptor agonists in marrow failure syndromes and other cytopenic scenarios.
Authorship
Contribution: P.S. wrote the paper.
Conflict-of-interest disclosure: P.S. is on the Board of Directors or an advisory committee for Novartis and has been affiliated with the Speaker’s Bureau for Pfizer and Novartis. Off-label drug use: Off-label use of eltrombopag in combination with immunosuppressive therapy will be discussed.
Correspondence: Phillip Scheinberg, Division of Hematology, Hospital A Beneficência Portuguesa, Rua Martiniano de Carvalho, 951, Sao Paulo, SP 01321-001, Brazil; e-mail: scheinbp@bp.org.br.
References
Author notes
This article was selected by the Blood Advances and Hematology 2018 American Society of Hematology Education Program editors for concurrent submission to Blood Advances and Hematology 2018. It is reprinted in Hematology Am Soc Hematol Educ Program. 2018;2018:450-456.