Key Points
Time to POD after 1L rituximab-based chemotherapy is strongly associated with PFS and OS from the point of 2L BTKi initiation.
The 2L BTKi MIPI identifies patients expected to have limited disease control with 2L BTKis and who may benefit from other therapies.
Abstract
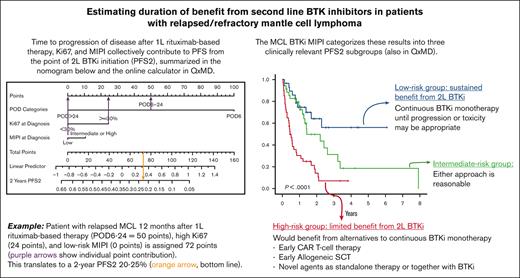
Time to progression of disease (POD) after first-line (1L) therapy is prognostic in mantle cell lymphoma (MCL), although studies have included a broad range of 1L, second-line (2L), and subsequent lines of therapy. The purpose of this study was to evaluate the factors predicting outcomes in patients with relapsed/refractory (R/R) MCL exclusively initiating 2L Bruton’s tyrosine kinase inhibitors (BTKis) after 1L rituximab-containing therapy. Patients were accrued from 8 international centers (7 main, 1 validation cohort). Multivariable models evaluating the association between time to POD and clinical/pathologic factors were constructed and converted into nomograms and prognostic indexes predicting outcomes in this population. A total of 360 patients were included, including 160 in the main cohort and 200 in the validation cohort. Time to POD, Ki67 ≥ 30%, and MCL International Prognostic Index (MIPI) were associated with progression-free survival (PFS2) and overall survival (OS2) from the start of 2L BTKis. C-indexes were consistently ≥0.68 in both cohorts. Web/application-based calculators based on nomograms and prognostic indexes to estimate PFS2 and OS2 were constructed. The 2L BTKi MIPI identifies 3 groups with distinct 2-year PFS2, including high risk (14%), intermediate risk (50%), and low risk (64%). Time to POD, Ki67, and MIPI are associated with survival outcomes in patients with R/R MCL receiving 2L BTKis. Simple clinical models incorporating these variables may assist in planning for alternative therapies such as chimeric antigen receptor T-cell therapy, allogeneic stem cell transplantation, or novel agents with alternative mechanisms of action.
Introduction
Time to progression of disease (POD) after first-line (1L) treatment is a robust prognostic factor in mantle cell lymphoma (MCL). In particular, POD within 24 months (early POD) of 1L therapy is associated with poor outcomes across broad ranges of age, fitness, and prior therapies.1-6 Studies of outcomes according to timing of POD have included heterogeneous 1L, second-line (2L), and subsequent lines of therapy, which limit the prognostic performance of this variable in the assessment of outcomes from the point of initiation of individual 2L therapies.
The covalent Bruton tyrosine kinase inhibitors (BTKis) ibrutinib, acalabrutinib, and zanubrutinib are standard treatment options for patients with relapsed/refractory (R/R) MCL.7-9 Randomized and observational data have demonstrated improved outcomes with ibrutinib compared with other therapies for R/R MCL such as temsirolimus or chemoimmunotherapy,10,11 and the use of ibrutinib as 2L rather than later lines of therapy is associated with more favorable outcomes.12,13
Although most patients with R/R MCL respond to BTKis, eventual progressive disease (PD) is inevitable, and outcomes after BTKi discontinuation are poor.14,15 Cellular therapies such as allogeneic stem cell transplantation (alloSCT)16-19 and chimeric antigen receptor T-cell (CAR-T) therapy20 are associated with favorable response rates and outcomes in R/R MCL, even in patients previously treated with BTKis, and are currently considered a standard of care in this setting.9 However, these therapies are complex and require advance planning; practically, it is challenging to set them up in patients with rapid progression of R/R MCL. Other emerging novel therapies such as noncovalent BTKi, antibody-drug conjugates, and bispecific antibodies could be reasonable alternatives in this setting.9
Therefore, a refined estimator of treatment duration at the point of 2L BTKi initiation may better identify patients who will likely require a rapid switch to other therapies while their disease remains relatively controlled with 2L BTKi monotherapy, the inclusion of additional novel therapies together with 2L BTKis to maximize response duration, or potentially an alternative 2L therapy without BTKi. The purpose of this study is to analyze the association between prognostic factors, including time to POD, and outcomes in patients with R/R MCL starting 2L BTKi therapy.
Methods
Study design
This was an international, multicenter, retrospective, observational study. Patients meeting the following eligibility criteria were identified at each participating center: (1) age ≥ 18 years at diagnosis of MCL, (2) 1L treatment with any rituximab-containing chemotherapy regimen, with or without consolidative autologous SCT (with or without maintenance rituximab [MR]), and (3) 2L treatment with single-agent covalent BTKi for first relapse/progression. Patients could have been diagnosed with MCL at any time in the past, but they had to have initiated 2L BTKi before December 2020.
Consecutive patients were identified through single-center and/or population-based registries depending on resources available at each participating institution. Each site performed systematic queries of available databases (clinical, pathology, pharmacy, administrative, and billing) or used software to abstract specific terms (eg, MCL, ibrutinib, acalabrutinib, zanubrutinib) from electronic health records. Individual medical records were reviewed to confirm eligibility and abstract additional data.
The diagnosis of MCL was determined locally at the time of MCL diagnosis and treatment. Deidentified or fully anonymized patient, disease, treatment, and follow-up data were collected in a common case report form and were centrally pooled and analyzed at British Columbia Cancer in Vancouver, British Columbia, Canada. Because this is a retrospective study in which individual patient informed consent would be impossible or impractical to obtain, research ethics approvals were obtained at each institution according to their own policies.
The primary end point of the study was second progression-free survival (PFS2), defined as the time from initiation of 2L BTKis until disease progression or death from any cause. Patients who discontinued BTKi therapy to proceed with consolidative alloSCT (while responding to BTKis) were censored on the date of alloSCT. Patients who discontinued BTKi therapy for toxicity but developed subsequent disease progression were coded as having a PFS2 event on the date of PD. The secondary end point was second overall survival (OS2), defined as the time from initiation of 2L BTKis until death from any cause. PFS2 and OS2 were estimated using the Kaplan-Meier method.
Statistical analysis
The association between time to POD and other prognostic factors with PFS2 and OS2 was analyzed using Cox proportional hazards models. Initially an 8-variable model was constructed using the following variables known to have a prognostic association in MCL: time to POD (categorical variable: 3 risk groups), blastoid/pleomorphic morphology at diagnosis (dichotomous variable: present vs absent), Ki67 at diagnosis (dichotomous variable: ≥30% vs <30%), MCL International Prognostic Index (MIPI) at diagnosis (categorical variable: 3 risk groups), age at POD (continuous variable), performance status at diagnosis (dichotomous variable: >1 vs 0-1), type of 1L chemotherapy (dichotomous variable: high-dose cytarabine vs not), receipt of MR (dichotomous variable: yes vs no), and individual treatment center (categorical variable: each center included as a single cluster). Stepwise backward selection was applied to identify significant variables in the final models.
Time to POD was defined as the time from the date of initiation of 1L rituximab-based therapy to the date of POD before initiation of 2L BTKi therapy. Time to POD was categorized into 3 prognostic subgroups as previously described: POD6 (POD within 6 months of 1L therapy), POD6-24 (POD within 6-24 months of 1L therapy), and POD >24 (POD after 24 months of 1L therapy).2 POD6, also labeled as refractory disease, was defined as progression during induction or within 6 months of diagnosis or stable disease/PD at the end of induction. The primary reason for this definition was to account for patients who did not have a response assessment recorded in the database but clearly did not achieve disease control with initial treatment. POD6 and POD6-24 were collectively labeled as early POD, whereas POD > 24 was labeled as late POD, as previously described.1
The following regimens were defined as containing high-dose cytarabine: rituximab in combination with cyclophosphamide, doxorubicin, vincristine, and prednisone alternating with dexamethasone, cytarabine, and cisplatin (R-CHOP/R-DHAP) (MCL Younger), R-CHOP/high-dose cytarabine (Nordic), R-DHAP alone, and R-HyperCVAD. TP53 mutation status results were not included because of incomplete data. p53 protein overexpression results by immunohistochemistry were not collected. Other factors at first relapse were not included in the models because of incomplete data: (1) MIPI at relapse because results were only available in about half of the cohort and (2) blastoid/pleomorphic morphology or Ki67 at relapse because repeat biopsies were not performed consistently at first relapse, thus generating a potential bias.
Complete case analysis without imputation was performed. Deviance residuals were used to evaluate extreme values when generating the models. Model performance was assessed using time-dependent concordance indexes (C-index) and calibration curves. The final models were validated using C-index and calibration curves in an independent cohort of 200 patients with R/R MCL uniformly treated with 2L ibrutinib in a national audit database from the UK National Health System.21
The final models were used to construct nomograms and web-based calculators predicting PFS2 and OS2. A prognostic model, the 2L BTKi MIPI, predicting 2-year PFS2 was constructed. The linear predictor of the final model for PFS2 was broken down into 3 risk categories (high, intermediate, low). Optimal cutoffs were identified within the probability distribution of 2-year PFS2 under the assumption that it satisfied a mixed model.
Data were analyzed with the Statistical Package for the Social Sciences version 14 and The R Project for Statistical Computing version 4.0.3. Models were constructed using the cph (rms) and coxph (survival) functions in R.
Results
Patient characteristics
The main cohort included 160 patients identified from 7 academic centers. Median age at diagnosis was 67 years (range, 38-90 years), and 73% were male. The most common 1L regimens were bendamustine and rituximab (50%) and alternating R-CHOP with high-dose cytarabine (MCL Younger and Nordic regimens, 19%).22,23 In addition, 31% received autologous stem cell transplantation and 37% received MR (Table 1).
The median time to POD after 1L therapy was 24 months (range, <1-161 months), and 19% had refractory disease (POD6). High-risk MIPI was associated with refractory disease (supplemental Table 1). About half of the patients (51%) had early POD; older age at diagnosis, blastoid/pleomorphic morphology, Ki67 ≥ 30%, and high-risk MIPI were associated with early POD (supplemental Tables 1 and 2).
Repeat biopsy at progression, performed in 96 patients (60%), identified additional individuals who developed blastoid/pleomorphic morphology and/or high Ki67. The median time to 2L BTKi was 25 months (range, <1-162 months), and ibrutinib was the most frequent 2L BTKi (84%). At data cutoff, 50 patients (31%) remained on BTKi. The other 110 patients (69%) discontinued BTKi for a variety of reasons including PD (n = 82), BTKi toxicity (n = 18), and planned consolidative alloSCT (n = 4). Third-line therapies were heterogeneous (Table 1).
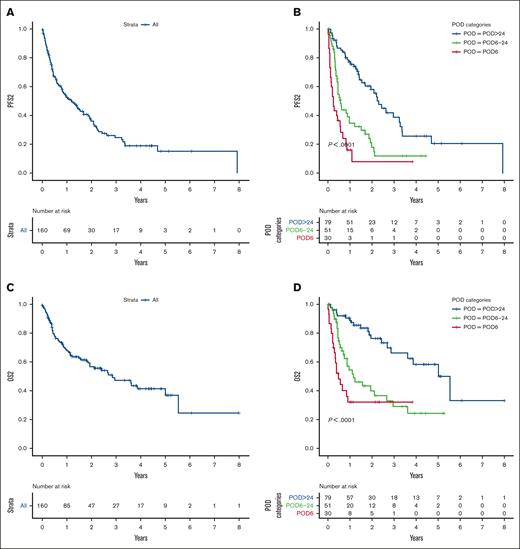
PFS2
With a median follow-up after 2L BTKi in living patients of 1.5 years (range, <1 month to 9.5 years), the median PFS2 was 1.2 years (95% confidence interval [CI], 0.8-1.6) and the 2-year PFS2 was 36% (95% CI, 22-50) (Figure 1A). The median PFS2 was 0.3 years (95% CI, 0.2-0.4) in patients with POD6/refractory disease (n = 33, 21%) and 1.7 years (95% CI, 1.2-2.2; P < .001) in patients without refractory disease (n = 127, 79%) (Figure 1B; supplemental Figure 1A). The median PFS2 was 0.45 years (95% CI, 0.3-0.6) in patients with early POD (n = 81, 51%) and 2.3 years (95% CI, 1.7-2.8; P < .001) in patients with late POD (n = 79, 49%) (Figure 1B; supplemental Figure 1B).
Outcomes in the main cohort. (A) PFS2, (B) PFS2 according to POD categories, (C) OS2, and (D) OS2 according to POD categories.
Outcomes in the main cohort. (A) PFS2, (B) PFS2 according to POD categories, (C) OS2, and (D) OS2 according to POD categories.
In the models for PFS2, blastoid/pleomorphic morphology, age at POD, performance status, type of 1L chemotherapy, and receipt of MR were not statistically significant and were removed. Time to POD, Ki67 ≥ 30%, and MIPI were the 3 statistically significant variables in the final models (Figure 2A). MIPI dichotomized as intermediate/high vs low provided the most robust hazard ratio compared with other combinations of MIPI categories. The deviance residual plot showed that the deviance range was from –2.6 to 2.8 with few outliers (supplemental Figure 2). Separate models using Ki67 ≥ 50% as a cutoff did not yield significantly different PFS2 results (data not shown), and therefore, the 30% cutoff was retained.24
Forest plots of the final models. (A) Forest plot of the final model for PFS2. (B) Forest plot of the final model for OS2.
Forest plots of the final models. (A) Forest plot of the final model for PFS2. (B) Forest plot of the final model for OS2.
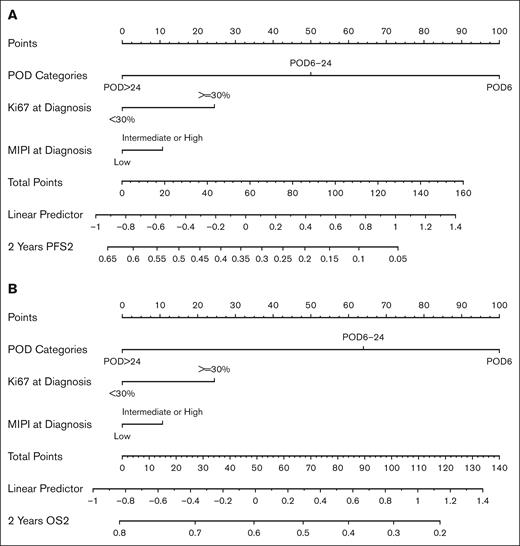
A nomogram predicting 2-year PFS2 based on time to POD, Ki67, and MIPI was constructed (Figure 3A). The C-index at 2 years was 0.71 (supplemental Figure 3). A calculator for 2-year PFS2 based on the nomogram is available online (https://qxmd.com/calculate/calculator_868/estimate-survival-in-relapsed-refractory-mcl).
Nomograms. (A) Nomogram predicting PFS2 based on the final model with categories of time to POD, Ki67, and MIPI. (B) Nomogram predicting OS2 based on the final model with the same variables. To use the nomograms, first calculate the individual number of points in the first row for each of the 3 variables. Locate the sum of the individual points in the “Total Points” row. Draw a vertical line inferiorly to identify the hazard and point estimate of a 2-year PFS2/OS2 event. For example, in Figure 3A, POD6 (100 points) + elevated Ki67 (24 points) + low-risk MIPI (0 points) = 124 points, which translates to a 2-year PFS2 of <10%.
Nomograms. (A) Nomogram predicting PFS2 based on the final model with categories of time to POD, Ki67, and MIPI. (B) Nomogram predicting OS2 based on the final model with the same variables. To use the nomograms, first calculate the individual number of points in the first row for each of the 3 variables. Locate the sum of the individual points in the “Total Points” row. Draw a vertical line inferiorly to identify the hazard and point estimate of a 2-year PFS2/OS2 event. For example, in Figure 3A, POD6 (100 points) + elevated Ki67 (24 points) + low-risk MIPI (0 points) = 124 points, which translates to a 2-year PFS2 of <10%.
OS2
The median OS2 was 2.9 years (95% CI, 1.6-4.1), and the 2-year OS2 was 60% (95% CI, 44-70) (Figure 1C). The median OS2 was 0.6 years (95% CI, 0.2-1) in patients with POD6/refractory disease and 3.6 years (95% CI, 1.9-5.3; P < .001) in patients without refractory disease (Figure 1D; supplemental Figure 4A). The median OS2 was 0.9 years (95% CI, 0.5-1.3) in patients with early POD and 5.5 years (95% CI, 3.5-7.5; P < .001) in patients with late POD (Figure 1D; supplemental Figure 4B).
Time to POD, Ki67 ≥ 30%, and MIPI were also evaluated in the models for OS2 (Figure 2B). The deviance residual plot showed that the deviance range was from –1.9 to 2.7 with few outliers (supplemental Figure 5). A nomogram predicting 2-year OS2 based on these variables was constructed (Figure 3B). The C-index at 2 years was 0.69 (supplemental Figure 6).
After 2L BTKis, 62 patients received 3L therapy, with 30 (48%) receiving chemotherapy-based treatment and 32 (52%) targeted therapy–based treatment (Table 1). Overall survival calculated from the date of 2L BTKi discontinuation to death from any cause (OS3) was not statistically significant between 3L treatment categories: median OS3 23-month chemotherapy (95% CI, 3-43 months) vs 10-month targeted therapy (95% CI, 0.2-25 months), P = .53.
Validation cohort
The final models were validated in an independent cohort of 200 patients with R/R MCL uniformly treated with 2L ibrutinib from the United Kingdom, which has been previously described.21 Briefly, the median age at 2L BTKi was 71 years (range, 33-94 years), 15% had blastoid/pleomorphic morphology, 58% had Ki67 ≥ 30%, the median time to 2L BTKi was 24 months (range <1-158 months), and 52% had early POD (supplemental Table 3). Older age and use of less-intensive therapies were associated with both refractory disease and early POD. High-risk MIPI was also associated with refractory disease (supplemental Tables 4 and 5).
With a median follow-up after 2L BTKi in living patients of 1.2 years (range, <1 month to 5.3 years), the median PFS2 was 1.6 years (95% CI, 1.1-2.1) and the 2-year PFS2 was 43% (95% CI, 31-56) (supplemental Figure 7A). The median PFS2 was 0.6 years (95% CI, 0.2-1) in patients with refractory disease (n = 55, 28%) and 2.6 years (95% CI, 1.9-3.3; P < .001) in patients without refractory disease (n = 145, 72%) (supplemental Figure 7B-C). The median PFS2 was 0.9 years (95% CI, 0.4-1.4) in patients with early POD (n = 104, 52%) and 2.3 years (95% CI, 1.1-3.5; P < .001) in patients with late POD (n = 96, 48%) (supplemental Figure 7B,D). Applying the model developed in the training cohort, the C-index for PFS2 at 2 years in the validation cohort was 0.68. (supplemental Figure 8)
The median OS2 was 1.8 years (95% CI, 1-2.6), and the 2-year OS2 was 48% (95% CI, 40-57) (supplemental Figure 9A). The median OS2 was 0.9 years (95% CI, 0.5-1.3) in patients with refractory disease and 2.7 years (95% CI, 1.6-3.7; P < .001) in patients without refractory disease (supplemental Figure 9B-C). The median OS2 was 1.2 years (95% CI, 0.6-1.8) in patients with early POD and 3.3 years (95% CI, 1.8-4.8; P < .001) in patients with late POD (supplemental Figure 9B,D). Applying the model developed in the training cohort, the C-index for OS2 at 2 years in the validation cohort was 0.70 (supplemental Figure 10).
Prognostic index: 2L BTKi MIPI
Three modes in the probability distribution of 2-year PFS2 in the model were identified (supplemental Figure 11). Two-year PFS2 of 30% and 60% cutoffs separated 3 distinct subgroups within the 2-year PFS2 distribution, generating a high-risk subgroup (n = 40) with 2-year PFS2 of 14% (95% CI, 6-33), intermediate-risk subgroup (n = 35) with 2-year PFS2 of 50% (95% CI, 34-74), and low-risk subgroup (n = 30) with 2-year PFS2 of 64% (95% CI, 47-87) (P < .001) (Figure 4A). To understand the influence of missing individual patient results in the performance of the 2L BTKi MIPI, missing Ki67 results were recoded as <30% and missing MIPI results as low risk. Two-year PFS2 estimates were not substantially different with this approach, which included high-risk subgroup (n = 76) with 2-year PFS2 of 14% (95% CI, 7-27), intermediate-risk group (n = 64) with 2-year PFS2 of 43% (95% CI, 31-60), and low-risk subgroup (n = 76) with 2-year PFS2 of 94% (95% CI, 44-100) (P < .001) (Figure 4B).
PFS2 according to the 2L BTKi MIPI in the main cohort. (A) High-, intermediate-, and low-risk categories of PFS2 in the main cohort according to the 2L BTKi MIPI in cases with complete data (n = 105). (B) High-, intermediate-, and low-risk categories of PFS2 in the main cohort according to the 2L BTKi MIPI in all cases (n = 160; missing individual Ki67 or MIPI values were coded as low).
PFS2 according to the 2L BTKi MIPI in the main cohort. (A) High-, intermediate-, and low-risk categories of PFS2 in the main cohort according to the 2L BTKi MIPI in cases with complete data (n = 105). (B) High-, intermediate-, and low-risk categories of PFS2 in the main cohort according to the 2L BTKi MIPI in all cases (n = 160; missing individual Ki67 or MIPI values were coded as low).
In the validation cohort, these cutoffs did not identify statistically significant subgroups, although there were substantial missing individual data (66 of 200 patients had complete results for the 3 variables) (supplemental Figure 12A). However, these cutoffs did identify 3 distinct risk subgroups when the analysis was performed in the entire validation cohort after recoding for missing data (supplemental Figure 12B). The online calculator also identifies the individual risk subgroup for a given patient (https://qxmd.com/calculate/calculator_868/estimate-survival-in-relapsed-refractory-mcl).
Discussion
In this study of patients with MCL treated in 6 countries with current standard 1L rituximab-containing chemotherapy and subsequent 2L BTKi monotherapy, outcomes after 2L BTKis were largely driven by time to POD and to a lesser extent by other factors including Ki67 or MIPI at diagnosis. Time to POD informs most, but not all, of the prognosis expected with 2L BTKis. For example, based on the nomograms, the presence of Ki67 ≥ 30%, which is associated with lower response rates and outcomes with both 1L rituximab-based therapy and 2L BTKi-based therapy,4,24-29 significantly influences 2-year PFS2 across the 3 categories of time to POD. Based on the deviance residuals analyses, it is unlikely extreme values are driving some overfitting in the model with reduced calibration in the PFS2/OS2 validation.
Blastoid/pleomorphic morphology was not statistically significant in the models, most likely because of a strong correlation with Ki67. With only a couple of exceptions, all patients with blastoid/pleomorphic morphology had Ki67 ≥30%. Other factors (TP53 mutations, MIPI at relapse, biopsy findings at relapse) could not be included in the models because of missing data, which would have significantly reduced sample size and/or biased results. Biopsy at first relapse, performed in 96 of 160 patients (60%), identified additional cases who developed blastoid/pleomorphic morphology and/or high Ki67. We hypothesize that a model incorporating clinical and biologic factors at first relapse (rather than at diagnosis) may better estimate outcomes from the point of 2L BTKi initiation. However, because of disease, patient, system, and physician factors influencing the decision to perform a biopsy at first relapse, we did not include these variables in our models.
In addition to confirming previous findings that patients with early relapse/progression of MCL experience poor outcomes,1-6 this study highlights the heterogeneity within the early POD group. In our study, the median PFS2 in patients with early POD was 5 months (range, <1 month to 4.4 years). In the pooled analysis of prospective studies of ibrutinib for R/R MCL, the median PFS2 in patients with early POD receiving 2L ibrutinib was 14 months (range, <1 month to ∼7.5 years).3 This suggests that there are outliers with relatively favorable outcomes within the early POD group, particularly those with POD6-24.
Outcomes in our main and validation cohorts were worse than in the pooled analysis of prospective studies of ibrutinib for R/R MCL. In that study, the median PFS2 in patients receiving 2L ibrutinib (n = 99) was 25 months, and the median OS was 62 months.3 These differences are multifactorial and include a higher proportion of adverse prognostic factors (high-risk MIPI, blastoid, and early POD) and very poor outcomes in patients with early POD in our cohorts, other unmeasured differences between real world and clinical trials populations, use of imaging investigations in the assessment of PFS2, and possibly 3L and subsequent therapies.
The PFS2 and OS2 models were developed in a broad international population receiving various 1L treatments and with multiple reasons for 2L BTKi discontinuation beyond PD. All patients were systematically identified and were representative of the population seen at each center, without selection for a fit or an unfit group, supporting the external validity of our findings. Although different rituximab-based 1L strategies are associated with variable outcomes, in this study, the use of high-dose cytarabine 1L regimens and/or MR were not significant in the multivariable models, again supporting the broader applicability of the 2L BTKi MIPI.6,28,30-32 Moving forward, these results will not be applicable to patients receiving 1L BTKi together with rituximab-based chemotherapy.33,34
In summary, time to POD, Ki67, and MIPI were strongly associated with outcomes in patients with R/R MCL receiving 2L BTKi therapy. Given the generally aggressive biology of MCL, the identification of such factors could assist in the design of future studies of therapies for R/R MCL. For example, patients could be stratified based on POD status or categories of the 2L BTKi MIPI in studies of novel agents for R/R disease. Practically, the calculators and 2L BTKi MIPI incorporating these variables are clinically useful to anticipate the duration of clinical benefit with 2L BTKis and may assist with treatment decision making, particularly in the subgroup of patients expected to derive limited duration of benefit from 2L BTKi monotherapy. In these patients, options include early planning of consolidative strategies (CAR-T or alloSCT) while 2L BTKi achieves some disease control, the incorporation of other novel agents together with the 2L BTKi, or bringing therapies other than covalent BTKi (including CAR-T) earlier into the 2L treatment setting.
Acknowledgments
The authors thank Emilia Elizbieta Florea for the administrative assistance with the cohort from Italy.
The support for the Ohio State University Lymphoma database, used for this study, was provided by award UL1TR002733 from the National Center for Advancing Translational Sciences and support for the MER database from National Cancer Institute P50 CA097274 University of Iowa/Mayo Clinic Lymphoma SPORE. Medical writers were not involved in the writing of this manuscript.
Authorship
Contribution: D.V. and A.J. designed and performed the research and analyzed data; and all authors contributed to the acquisition, analysis, or interpretation of data for this article and drafts of this article, revised the manuscript critically for important intellectual content, approved the final version for publication, and agreed to be accountable for all aspects of the article.
Conflict-of-interest disclosure: D.V. received honoraria/consulting from Janssen, Roche, Bristol Myers Squibb (BMS), Celgene, Kite/Gilead, AstraZeneca, AbbVie, Kyowa Kirin, and BeiGene, and research funding (to the institution) from Roche and AstraZeneca. D.W.S. reports consulting for AbbVie, AstraZeneca, Incyte, and Janssen, and received research funding from Janssen and Roche. C.V. received honoraria/consulting fees from Janssen, Roche, Incyte, Celgene, Kite/Gilead, AstraZeneca, AbbVie, Kyowa Kirin, BeiGene, and Novartis, and research funding (to the institution) from Janssen. C.Y.C. received consulting/advisory fees/honoraria from Roche, Janssen, MSD, Gilead, AstraZenecca, Lilly, TG Therapeutics, Beigene, Novartis, and BMS, and research funding from BMS, Roche, AbbVie, and MSD. D.A.B. received honoraria/consulting fees from Kite/Gilead and SeaGen, and research funding (to the institution) from Nurix Therapeutics and Novartis. K.L.L. received honoraria/consulting/advisory fees from AstraZeneca, Janssen, Roche, Loxo/Lilly, and IQVIA. A.S.G. received research funding from Roche, AstraZeneca, AbbVie, and Janssen, and honoraria/consulting fees from Sandoz, AstraZeneca, AbbVie, and Janssen. A.K. received consulting/advisory fees/honoraria from Kite Pharma, Janssen, Genentech, and AstraZeneca, and research funding from AbbVie, Adaptive Biotechnologies, Celgene, Pharmacyclics, Seattle Genetics, AstraZeneca, and Loxo Oncology. T.C.E.-G. was previously employed by Roche, and received speakers fees from AbbVie in 2021. J.B. received research funding from Gilead Sciences, Denmark. M.J.M. received research funding from Roche, BMS, GenMab, and is on the advisory board of Adaptive Biotechnologies and GenMab. J.P. received research funding (to the institution) from Karyopharm and Biofourmis. R.M. received research funding/honoraria from Sanofi and honoraria from Janssen. G.T. is on the advisory board of Seattle Genetics with honoraria directed to research funding (to the institution). The remaining authors declare no competing financial interests.
Correspondence: Diego Villa, Division of Medical Oncology, British Columbia Cancer–Vancouver Cancer Centre, 600 West 10th Ave, Vancouver, BC V5Z 4E6, Canada; e-mail: dvilla@bccancer.bc.ca.
References
Author notes
∗D.V. and A.J. contributed equally to this study and share first authorship.
Presented in abstract form at the 16th International Conference on Malignant Lymphoma in Lugano, Switzerland, 18 June 2021 to 21 June 2021.
Data are available on request from the corresponding author, Diego Villa (dvilla@bccancer.bc.ca).
The full-text version of this article contains a data supplement.