Key Points
Haplotype-mismatched FVIII exposure does not result in differential antibody binding to recombinant FVIII proteins.
Antibodies from individuals with no inhibitor bound more strongly to B-domain–deleted than full-length FVIII proteins.
Abstract
The most common complication in hemophilia A (HA) treatment, affecting 25% to 30% of patients with severe HA, is the development of alloimmune inhibitors that foreclose the ability of infused factor VIII (FVIII) to participate in coagulation. Inhibitors confer significant pathology on affected individuals and present major complexities in their management. Inhibitors are more common in African American patients, and it has been hypothesized that this is a consequence of haplotype (H)-treatment product mismatch. F8 haplotypes H1 to H5 are defined by nonsynonymous single-nucleotide polymorphisms encoding sequence variations at FVIII residues 1241, 2238, and 484. Haplotypes H2 to H5 are more prevalent in individuals with Black African ancestry, whereas 80% to 90% of the White population has the H1 haplotype. This study used an established multiplex fluorescence immunoassay to determine anti-FVIII antibody titers in plasma from 394 individuals with HA (188 Black, 206 White), measuring their binding to recombinant full-length H1 and H2 and B-domain–deleted (BDD) H1/H2, H3/H5, and H4 FVIII proteins. Inhibitor titers were determined using a chromogenic assay and linear B-cell epitopes characterized using peptide microarrays. FVIII-reactive antibodies were readily detected in most individuals with HA, with higher titers in those with a current inhibitor, as expected. Neither total nor inhibitory antibody titers correlated with F8 haplotype mismatches, and peptides with D1241E and M2238V polymorphisms did not comprise linear B-cell epitopes. Interestingly, compared with the full-length FVIII products, the BDD-FVIII proteins were markedly more reactive with plasma antibodies. The stronger immunoreactivity of BDD-FVIII suggests that B-domain removal might expose novel B-cell epitopes, perhaps through conformational rearrangements of FVIII domains.
Introduction
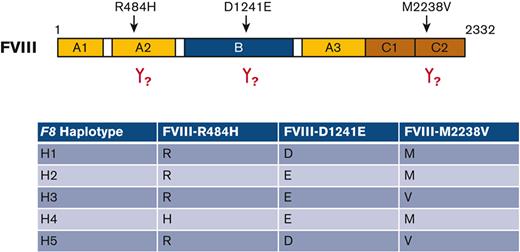
Several studies have indicated that African Americans with hemophilia A (HA) have an elevated risk of developing an alloimmune response to infused factor VIII (FVIII), compared with White non-Hispanic American patients with HA (referred to hereafter as White).1-3 One hypothesis put forward to explain this disparity is that significant subsets of the Black HA population mount an immune response to specific neoepitopes corresponding to mismatches between their endogenous (mutated) F8 gene and the infused FVIII product.4F8 gene haplotypes H1 to H5 are defined by nonpathogenic nonsynonymous single-nucleotide polymorphisms (ns-SNPs) encoding sequence variations at amino acid residues 1241, 2238, and 484 (“legacy” FVIII numbering, corresponding to the circulating protein after proteolytic removal of its 19-residue leader sequence, Table 1).5 Haplotypes H2 to H5 are more prevalent in individuals with Black African ancestry, whereas >90% of the White population has the H1 haplotype. Recombinant FVIII products correspond to H1 or H2 haplotypes, and plasma-derived FVIII concentrates are expected to contain predominantly FVIII-H1 in areas where the majority of the blood donor population is White. The Personalized Approaches to Therapies for Hemophilia (PATH) study collected blood samples from 394 individuals with HA in the United States, 188 Black and 206 White, recording their inhibitor history and self-identified race. F8 haplotypes were determined by F8 gene sequencing, polymerase chain reaction to amplify the relevant ns-SNPs, a DNase digestion assay, and high-resolution melting experiments. Statistical analyses revealed no significant correlations between inhibitor history and F8 haplotype or the individual ns-SNPs,3,6 in agreement with independent studies of smaller European7 and South African8 cohorts. CD4+ T-cell responses to the putative neoepitopes at FVIII residues 1241 and 2238 were investigated by tetramer-guided epitope mapping9 using HLA Class II tetramer reagents loaded with FVIII peptides, and these sensitive assays revealed no high-avidity binding of these peptide-HLA complexes by T cells from individuals with HA.3 Measurements of peptide-HLA affinities utilizing synthetic FVIII peptides and recombinant HLA Class II proteins indicated limited HLA binding of these polymorphic sequence variants, consistent with the observed lack of T-cell reactivity.3
This study aimed to look for evidence of B-cell responses correlating with exposure to haplotype-mismatched FVIII products. Aims were to analyze plasma samples from Black and White individuals with HA with known F8 haplotypes, testing antibody binding to recombinant proteins with the sequence variants R484H, D1241E, and M2238V, and to FVIII 20-mer peptides to determine whether these sequence variants comprise distinct linear B-cell epitopes.
Materials and methods
Participants’ demographics are summarized in Table 2, supplemental Table 1, and supplemental Data. Family members (n = 23), including 21 carrier mothers of the participants with HA, donated blood for control assays; these are referred to as family controls. Black participants are also described as African American in some cases hereafter, because this was an entirely American cohort; some results and conclusions may not apply to other Black populations or cohorts.
Antibody assays
Plasma samples were analyzed using a multiplex fluorescence immunoassay10-12 in which Luminex microsphere beads were coupled to the following rFVIII proteins: full-length (FL) rFVIII (H1, Kogenate, produced in baby hamster kidney [BHK] cells by Bayer), FL rFVIII (H2, Recombinate, produced in Chinese hamster ovary [CHO] cells by Baxter), and 3 B-domain–deleted (BDD)-FVIII proteins corresponding to H1/H2 FVIII (R484, M2238), H3/H5 FVIII (R484, V2238), and H4 FVIII (H484, M2238), all produced in human embryonic kidney (HEK) cells at Biogen (Table 3). Inhibitor titers were determined using a Chromogenic Nijmegen Bethesda assay (CNBA). Microarrays with imprinted 20-mer peptides spanning the FVIII A1, A2, C1, and C2 domain sequences, plus B-domain peptides spanning the FVIII-D1241E variant (supplemental Table 2) were utilized to map linear B-cell epitopes. Details of the study participants, multiplex fluorescence immunoassay, CNBA, and peptide array assays are provided in supplemental Data.
Plasma samples from 150 non-HA blood donors were evaluated in an earlier study using this same multiplex fluorescence assay, in which Luminex beads were coated with rFVIII-H2 (produced in CHO cells by Baxter).10 The anti-FVIII antibody levels in these individuals ranged from 1.4 ± 5 to 6.2 ± 5 nM. As in our analysis of 46 individuals with HA using this same assay,12 a 7 nM cutoff was chosen to indicate anti-FVIII antibody levels exceeding those expected for controls without HA.
Statistical analysis
Individuals with HA exposed to haplotype-mismatched FVIII were defined as follows: (1) all individuals with haplotype H3, H4, or H5 that had been treated with recombinant or plasma-derived FVIII or with any blood product (FVIII will be haplotype-mismatched at 1-2 of the polymorphic sites); (2) individuals with haplotype H1 that had been treated with recombinant FL-FVIII-H2 (FVIII will be haplotype-mismatched at 1 ns-SNP encoding D1241E); and (3) individuals with haplotype H2 that had been treated with recombinant FL-FVIII-H1 or plasma-derived FVIII or with any blood product (FVIII will be haplotype-mismatched at 1 ns-SNP encoding D1241E). For the purpose of this study, plasma-derived FVIII and other blood products are presumed to contain primarily FL-FVIII-H1, as many pooled plasma products are derived from a primarily White population that circulates predominantly FVIII-H1.5
Data were examined for normality using normal probability plots and log-transformed for analysis. Multiplex fluorescence immunoassay results measuring binding of antibodies from various subgroups of participants (eg, severe HA, mild + moderate HA, HA with intron-22 inversion, etc) to the 5 recombinant FVIII proteins were evaluated using the paired t test with step-down Bonferroni correction for multiple pairwise comparisons. The binding ratios were then calculated and compared for the following subgroups: those with a current inhibitor, no inhibitor history, an inhibitor history but no current inhibitor, and no current inhibitor regardless of inhibitor history using paired t tests with stepdown Bonferroni correction.
Separate linear regression analyses were run for individuals with and without a current inhibitor, adjusting for age and whether the individuals were related. For those with no current inhibitor, models were run adjusting or not adjusting for inhibitor history. All models were adjusted for age, relatedness, and race if the primary comparison did not involve race.
Results
BDD-FVIII proteins
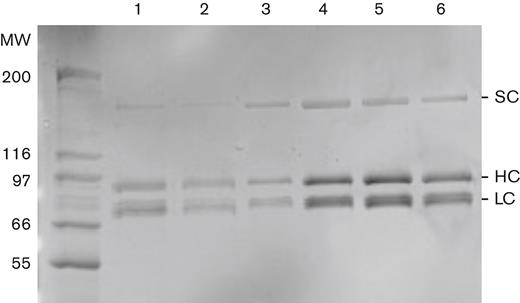
Yields of BDD-FVIII proteins (H1/H2, H3/H5, and H4) were 0.4 to 3.0 mg protein per preparation. Specific activities were in ranges expected for properly folded FVIII proteins (data not shown). Figure 1 is a representative sodium dodecyl sulfate polyacrylamide gel electrophoresis gel showing the purified proteins.
Purified BDD-FVIII proteins. BDD-FVIII H1/H2, H3/H5, and H4 proteins analyzed by sodium dodecyl sulfate polyacrylamide gel electrophoresis plus Coomassie brilliant blue staining showed high purity and the expected molecular weights. Molecular weights of protein standards are indicated in kDa. Refacto (Pfizer) was run as a BDD-FVIII standard. Lane 1: Refacto (10 μL, 300 IU/mL). Lane 2: Refacto (10 μL, 100 IU/mL). Lanes 3, 4, 5, 6: BDD-FVIII-H3/H5 (∼0.2 μg), BDD-FVIII-H1/H2 (0.56 μg), BDD-FVIII-H3/H5 (0.37 μg), and BDD-FVIII-H4 (0.46 μg), respectively, purified from representative clones, 1 μL/lane.
Purified BDD-FVIII proteins. BDD-FVIII H1/H2, H3/H5, and H4 proteins analyzed by sodium dodecyl sulfate polyacrylamide gel electrophoresis plus Coomassie brilliant blue staining showed high purity and the expected molecular weights. Molecular weights of protein standards are indicated in kDa. Refacto (Pfizer) was run as a BDD-FVIII standard. Lane 1: Refacto (10 μL, 300 IU/mL). Lane 2: Refacto (10 μL, 100 IU/mL). Lanes 3, 4, 5, 6: BDD-FVIII-H3/H5 (∼0.2 μg), BDD-FVIII-H1/H2 (0.56 μg), BDD-FVIII-H3/H5 (0.37 μg), and BDD-FVIII-H4 (0.46 μg), respectively, purified from representative clones, 1 μL/lane.
Chromogenic Nijmegen Bethesda assay
Because of limited plasma volumes, CNBA assays could be carried out for only 315 of the 394 participants with HA. Results are reported in Chromogenic Nijmegen Bethesda units (CNBU)/mL. Inhibitors (≥0.6 CNBU/mL) were detected in 24 of 274 individuals with severe HA (13 Black, 11 White) and 4 of 41 individuals with nonsevere HA (3 Black, 1 White). The 4 inhibitor-positive samples from participants with nonsevere HA showed detectable antibody binding to all 5 FVIII proteins. Among the severe HA inhibitor-positive samples, 3 of 24 had detectable antibodies against BDD-FVIII but not the FL H1 and H2 FVIII proteins; these inhibitors were between 0.9 to 6.4 CNBU/mL. The remaining 21 participants had total antibody titers ≥7 nM to all 5 rFVIII proteins. The CNBA assays detected inhibitors with titers ranging from 0.8 to 3.8 CNBU/mL in 4 participants who had no clinical history of an inhibitor. Of these participants, 2 (1-18 and 4-6) had mild or moderate HA and 2 (11-37 and 12-1) had severe HA.
Peptide microarray assays
Of the 152 FVIII 20-mer peptides, 18 showed substantial binding to antibodies in the plasma samples, notably including 3 overlapping peptides spanning FVIII residues 2194 to 2229, which include 1 of the 2 C2 domain hydrophobic beta turns that interact with both von Willebrand factor (VWF) and negatively charged phospholipid membranes. Peptides spanning residues 2297 to 2324 and 469 to 504, both of which are known antigenic sites in FVIII, were also highly reactive with plasma antibodies. However, the peptide-binding patterns were similar for individuals with HA with and without a current inhibitor and regardless of total anti-FVIII antibody titers. Peptides spanning the D1241E and M2238V polymorphic sites (corresponding to F8 haplotypes more common in African Americans) showed low reactivity with plasma antibodies, clearly indicating that these sites do not comprise immunodominant linear B-cell epitopes.
Multiplex fluorescence immunoassay to quantify anti-FVIII antibodies
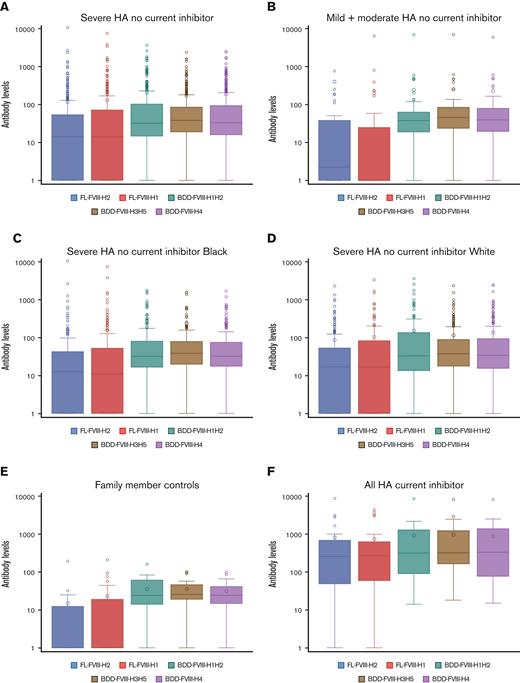
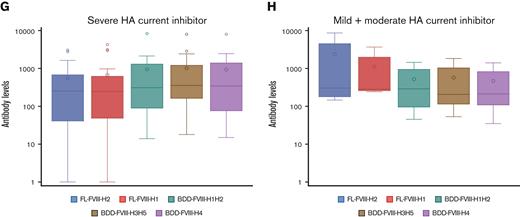
Samples from 160 of 162 Black and 177 of 185 White participants with severe HA, and samples from 24 of 26 Black individuals and from all 23 White individuals with mild/moderate HA showed ≥7 nM antibodies binding to at least 1 of the rFVIII proteins (supplemental Excel file). Blood from ∼30% (48/162) of Black and 25% (46/185) of White participants with severe HA, and 31% (8/26) of Black and 52% (11/21) of White participants with mild/moderate HA had no detectable antibodies against the 2 FL rFVIII proteins (H1 and H2) but showed binding to at least 1 of the 3 BDD-FVIII (H1H2, H3, or H4) proteins at ≥7 nM. Antibody binding of ≥7 nM to the FL FVIII proteins was detected in 31% to 39% of the 23 family controls, and to the BDD-FVIII proteins in 87% to 91% of these samples. Antibody binding to FL FVIII proteins above this cutoff was detected in 57% to 62% of the 366 HA–no current inhibitor samples, and to the BDD-FVIII proteins in 70% to 78% of these samples. Antibody binding of ≥7 nM to the FL FVIII proteins was detected in 89% of samples from 28 HA–current inhibitor samples, and to the BDD-FVIII proteins in 100% of these individuals.
As summarized in Tables 4, 5 and supplemental Tables 3-7 and Figure 2 and supplemental Figure 1, paired t tests for all subgroups of participants with HA showed higher antibody binding to the 4 BDD-FVIII proteins (∼2-6× higher) compared with the 2 FL-FVIII proteins, whereas binding to rFVIII-H1 (Kogenate) was virtually indistinguishable from binding to rFVIII-H2 (Recombinate). Anti-FVIII antibody levels in the 23 family controls were lower, as expected, but they also showed stronger binding (∼6× higher) to the BDD-FVIII proteins compared with the FL-FVIII proteins. Samples from individuals with a current inhibitor (supplemental Table 4) showed ∼2 to 4× higher binding to the 4 BDD-FVIII proteins.
Regression analyses
Distributions of all the variables for regression analyses were right-skewed, therefore, analyses were carried out for log-transformed data. Thus, each regression coefficient represents a log ratio between the 2 groups rather than the difference between the 2 groups. The log ratios were converted to simple ratios. Tables 6-9 show adjusted ratios of mean antibody binding to the 5 rFVIII proteins for various groups being compared after accounting for covariates.
The regression models evaluated possible differences related to HA severity, race, F8 haplotype, intron-22 inversion status, and exposure to a haplotype-mismatched FVIII product. Samples from individuals with severe HA with no current inhibitor but not individuals with mild/moderate HA with no current inhibitor, showed ∼1.5 to 2× higher antibody binding to all 5 FVIII proteins, compared with family controls. Among the participants with no current inhibitor, mean anti-FVIII antibody titers did not differ between those with severe HA vs mild or moderate HA; those with severe HA and intron-22 inversions vs no intron-22 inversion; those with severe HA treated with BDD-FVIII vs not treated with BDD-FVIII; Black vs White individuals with severe HA; or Black vs White individuals with mild or moderate HA. Adjusting for inhibitor history had a minimal effect on antibody-binding ratios and P values for all comparisons except the mild + moderate HA subgroup, in which this adjustment revealed higher binding of antibodies from Black participants to the 2 FL FVIII proteins, compared with those from White participants (Table 6). Among individuals with no current inhibitor who were exposed to haplotype-mismatched FVIII, 26 Black participants with severe HA (H3 + H5) showed slightly lower binding to the BDD-FVIII proteins than the 121 Black severe HA individuals with haplotype H1 + H2 (P < .05), but this difference was not significant when the model was adjusted for inhibitor history. Mean inhibitor titers also did not differ between severe HA infused with an H1, H2, or H3 + H5 haplotype–mismatched FVIII product, or between mild + moderate HA infused with an H1 or H2 haplotype–mismatched FVIII product (this group included only 3 individuals with H3 and 1 with H4 ) (Table 7). Samples from individuals with any-severity HA and a current inhibitor showed ∼3 to 11× higher binding to FVIII proteins than those from family controls, and there were no significant differences in antibody levels between any subgroups of participants with a current inhibitor (Table 8). There were also no significant differences in antibody binding among subgroups with a current inhibitor exposed to a haplotype-mismatched FVIII product (Table 9), although the sample size of these participants was too small for meaningful comparisons.
The multiplex fluorescence immunoassay, CNBA, and peptide microarray assay results for individual participants, as well as further descriptions of all participants including race, haplotype, etc, are summarized in the supplemental Data.
Discussion
The development of inhibitors is a serious immunopathologic response to therapeutic FVIII replacement therapy in patients with HA, and autoimmune inhibitors, although rare, often cause severe bleeding that is difficult to manage clinically. Inhibitors are dominated by immunoglobulin G1 (IgG1), IgG2 and/or IgG4 subclasses,13-15 binding to FVIII with high affinity as a consequence of class switching and affinity maturation.16 Known risk factors include the HA-causing mutation, with individuals with severe HA having no detectable FVIII antigen being at higher risk,17 and several studies have documented higher incidences in African Americans and Hispanics.1,3,18 Both genetic and environmental factors contribute to this etiology,19 with inflammation due to trauma, surgery, etc, potentially providing immunologic “danger” signals that can lower the threshold for FVIII immunogenicity.20 Clinical attention has appropriately been focused on patients who develop neutralizing anti-FVIII antibodies. However, several studies have revealed that nonneutralizing anti-FVIII antibodies10,12,13,16,21,22 as well as FVIII-responsive CD4+ T cells23-26 are present in individuals with HA who have with no inhibitor, and even in healthy non-HA human populations. Measurement of the total anti-FVIII antibody titers in individuals with HA provides a more accurate picture of the current immune status than do inhibitor titers, which are based on a clotting assay rather than quantification of the total antigen-specific antibodies.
This study is a natural history profile of anti-FVIII antibodies isolated from Black and White individuals with HA.3 Plasma samples from 347 individuals with severe HA and 47 with mild + moderate HA were evaluated by a multiplex fluorescence immunoassay. Antibody binding to FL rFVIII-H1 (D1241, R484, M2238) and rFVIII-H2 (E1241, R484, M2238) proteins and to BDD-FVIII H1/H2 (R484, M2238), H3/H5 (R484, V2238), and H4 (H484, M2238) proteins, and to synthetic, overlapping FVIII peptides, was measured. The vast majority of participants with HA circulated FVIII-binding antibodies that were above the 7 nM cutoff level representing the upper level found in a previously published cohort of 150 non-HA individuals.10 Although it is possible that some of these antibodies had primary specificity for other antigen(s) in addition to FVIII (eg, glycan-binding antibodies), this result was notable, having potential relevance to FVIII antigenicity as well as antibody-mediated clearance mechanisms.
Several complementary techniques have been utilized to quantify neutralizing + nonneutralizing anti-FVIII antibodies. The Reipert group employed a validated enzyme-linked immunosorbent assay to screen HA and non-HA cohorts, with cutoff values based on assays of non-HA plasma samples.13,16 FVIII-reactive antibodies were found in 19% of >600 healthy non-HA individuals, in 34% of 77 individuals with HA with no inhibitor history, in 39% of 23 individuals with HA after successful immune tolerance induction, and in 100% of individuals with an active hemophilic or acquired inhibitor. Apparent affinities were higher in individuals with a current inhibitor, whereas smaller percentages of the other cohorts had titers >1:80 and apparent KDs ranging from ∼2 to 20 nM. More recently, they characterized isotypes and affinities of nonneutralizing antibodies in individuals with HA and in those without HA.27 Boylan et al15 developed a multiplex fluorescence immunoassay with cutoff values set at 2 standard deviations above the mean fluorescence intensity values for 56 non-HA plasma samples. Of these non-HA controls, 5% to 7% had detectable anti-FVIII IgG1, IgG2, or IgM, whereas 23.3% of 369 individuals with inhibitor-negative HA had IgG1 levels above the cutoff and lower percentages of IgG2, IgG3, IgG4, and IgM. This assay was also used to quantify anti-FVIII antibodies in patients with HA undergoing immune tolerance induction or receiving bypass therapy.28 All of these aforementioned assays measured antibody binding to a commercial FL FVIII product. In this study, >50% of the 366 individuals with HA with no current inhibitor, and 89% of the 28 individuals with a current inhibitor, showed antibody levels ≥7 nM specific for 1 or both of the FL FVIII protein(s).
Regarding the varying levels of antibody binding to different FVIII proteins, differences in glycosylation of FL FVIII proteins expressed in different cell lines have been described,29 and both epidemiologic and murine HA model studies29 have suggested that FVIII produced in BHK cells might be more immunogenic than FVIII produced in CHO cells. None of the comparisons presented here, however, revealed notable differences in total antibody binding to Kogenate vs Recombinate, which were expressed in BHK and CHO cells, respectively.
An intriguing result of this study was that antibodies bound to the 3 BDD-FVIII proteins (H1/H2, H3/H5, and H4) with consistently higher mean titers than those against FL recombinant FVIII-H1 and FVIII-H2 proteins. For example, among the tested individuals, all 28 participants with a current inhibitor, 223 of 237 participants with severe HA with no inhibitor history, and all 31 participants with severe HA who cleared a previous high-titer inhibitor, had antibody levels ≥7 nM recognizing at least 1 of the BDD-FVIII proteins, whereas 3 of 28 participants with a current inhibitor, 68 of 237 participants with severe HA with no inhibitor history, and 10 of 31 participants who cleared a previous inhibitor recognized ≥1 BDD-FVIII proteins but neither of the 2 FL FVIII proteins. Of the aforementioned participants, only 4, all with no inhibitor history, had antibodies recognizing both FL FVIII proteins but none of the BDD-FVIII proteins (supplemental Excel file). These observations suggest that protein conformational changes accompanying removal of the B domain expose additional antibody-reactive sites, resulting in higher apparent titers of anti-FVIII antibodies despite the obvious inability of anti–B-domain antibodies to bind to BDD-FVIII proteins. An earlier study employed the same multiplex fluorescence immunoassay to quantify total antibodies from 34 individuals with HA, 16 of whom had a current inhibitor binding to FL rFVIII expressed in BHK cells, FL rFVIII expressed in CHO cells, and BDD-FVIII expressed in CHO cells.11 As in this study, almost all individuals with a current inhibitor also had significantly higher total anti-FVIII antibodies than individuals with no current inhibitor. However, averaged total antibody titers for the BDD-FVIII protein were lower than titers against the FL proteins. This study analyzed plasma from >10× as many participants, thereby providing greater statistical power and leading us to conclude that these BDD-FVIII proteins (produced in HEK cells) were consistently more reactive with anti-FVIII antibodies, compared with the FL rFVIII proteins from CHO or BHK cells.
The B domain, as well as the a3 acidic peptide N-terminal to the A3 domain, are removed proteolytically upon FVIII activation, releasing activated FVIII from VWF. B-domain removal by protein engineering has long been considered a relatively benign alteration, as this domain is dispensable for FVIII cofactor activity, and the resulting reduction in size offers advantages in FVIII expression, production costs, and packaging into vectors for gene therapy applications. A meta-analysis indicated possible increased immunogenicity of BDD-FVIII products,30,31 whereas several more recent studies have reported that commercial BDD-FVIII products were not associated with increased inhibitor risk.32-34 Discussions continue on how to properly interpret epidemiologic data on the relative immunogenicity of different FVIII products,35-40 and this issue is further complicated by the increasing number of engineered FVIII products available to patients, for example, with modifications to extend its half-life.41,42 The prospective, randomized SIPPET trial evaluated inhibitor incidences in patients treated with recombinant vs plasma-derived FVIII, however, most of the recombinant products utilized by these individuals were FL FVIII proteins,43 thus, the question of relative BDD-FVIII immunogenicity was not evaluated. Systematic epitope mapping using well-characterized monoclonal anti-FVIII antibodies could be employed, similar to earlier mapping of FVIII C2 domain epitopes,44-47 to evaluate conformational variants. It is important to point out that the BDD-FVIII proteins utilized in this study were generated for research purposes only and are not therapeutic products.
The observed different antigenicity of BDD-FVIII vis-à-vis FL FVIII suggests that the FVIII B domain might shield B-cell epitopes on other FVIII domains and/or prevent the development of conformational epitopes owing to altered orientation of FVIII domains in BDD-FVIII. It is also possible that some of the antibody-binding sites on FVIII proteins might be effectively shielded from the immune system when FVIII is bound to VWF. The multiplex fluorescence immunoassay employed here did not utilize a FVIII competition assay to evaluate specificity, as recommended in a recent review and meta-analysis by Abdi et al48; however, the observed differences in the antigenicity of BDD-FVIII and FL FVIII proteins suggest that the choice of FVIII used for such an assay could influence results, and therefore evaluations of sensitivity and specificity. Future studies will be required to elucidate the structural basis of these observed differences.
A primary goal of this study was to test the hypothesis that 3 polymorphic FVIII sequence variations defining F8 haplotypes that are more prevalent in the African American population comprise immunodominant B-cell epitopes. An earlier regression analysis of 362 individuals with severe HA enrolled in the PATH study showed higher inhibitor incidences in Black individuals with an intron-22 inversion mutation, compared with White individuals with the same mutation (P = .02) but showed no correlations of inhibitor history with F8 variants/haplotypes.3 This suggested that genetic differences not localized to the F8 gene play a primary role in these race-associated differences. Inhibitor development is a classic alloimmune response to a foreign antigen driven by CD4+ T cells.49 CD4+ T-cell responses to FVIII peptides were evaluated for a subset of PATH study participants, and tetramer-guided epitope mapping revealed no high-avidity T-cell recognition of peptides containing sequence variants D1241E or M2238V, indicating these polymorphic sequences are unlikely to comprise immunodominant T-cell epitopes.3
This cross-sectional study of plasma samples from these same individuals demonstrates that individuals infused with a haplotype-mismatched FVIII product do not circulate higher titers of total (neutralizing + nonneutralizing) anti-FVIII antibodies than those receiving haplotype-matched FVIII products. Although most participants did circulate FVIII-binding antibodies, these antibodies did not bind differentially to FL rFVIII-H1 vs FL rFVIII-H2 (differing only at D1241E), or to 3 BDD-FVIII proteins with polymorphic sequences differing at R484H and M2238V (haplotypes H1/H2, H4, and H3/H5). Furthermore, synthetic FVIII peptides with either polymorphic sequence at amino acids 1241 (D or E) and 2238 (M or V) did not comprise linear B-cell epitopes recognized by antibodies in the plasma samples. Specifically, the D1241E peptides were remarkably nonantigenic for all individuals, and antibodies from only 4 of the 32 individuals with haplotype H3 + H5 showed detectable but similar reactivity with peptides corresponding to the D2238V variants, suggesting that this binding was not owing to recognition of a haplotype-mismatched sequence motif. Only 3 of the 188 African American participants had the H4 polymorphism (R484H), precluding statistical analysis of this subgroup.
Limitations of this study include that the participants with severe HA had multiple FVIII exposures and, therefore, anti-FVIII antibodies generated before class switching and affinity maturation were not analyzed. Antibody subclasses and isotype were not quantified, owing to limited sample volumes. This could be addressed in future studies by prospective analysis of serial plasma samples collected during initial FVIII infusions. Interestingly, 9 of the 23 control samples from family members showed antibody binding ≥7 nM to 1 or both of the FL FVIII proteins, possibly reflecting anti-FVIII immune responses in carrier mothers who had received FVIII infusions or blood transfusions. Cutoff values of 7 nM were based on our analysis of a previously published cohort of 150 healthy non-HA donors.10
The results of this study indicate that anti-FVIII antibodies recognizing 3 minor sequence variations encoded by non–HA-causing ns-SNPs in the F8 gene do not contribute significantly to FVIII antigenicity. Together with our previous statistical analysis and investigation of potential T-cell responses to these polymorphic sequences,3 these data indicate that although immune responses to neoepitopes resulting from F8 haplotype mismatch might occur rarely, they are not a major contributor to inhibitor development in African American patients with HA. Further studies including epitope mapping, structural studies, and glycosylation analyses will be required to determine the basis of the higher antigenicity of BDD-FVIII proteins compared with the 2 FL FVIII proteins observed herein. Finally, the high prevalence of measurable FVIII-reactive antibodies in hemophilic plasma samples described herein adds to growing evidence that mechanisms of peripheral tolerance to FVIII are required to maintain hemostasis owing to the inherent immunogenicity and antigenicity of this essential blood coagulation protein.
Acknowledgments
The authors thank M. Gissel, J. Krudysz-Amblo, V. Zachary, D. Dutta, M. Epstein, R. Hughes, and S. Fletcher for their assistance, and R. Peters for critical reading of the manuscript. The authors thank all blood donors and research nurses, and all of the PATH study clinical investigators: Afshin Ameri, J. Christian Barrett, Rathi Iyer, Neil Josephson, Christine Kempton, Craig Kessler, Nigel Key, Rebecca Kruse-Jarres, Amanda Krause, Cindy A. Leissinger, David Lillicrap, Ronald Louie, Jean Lusher, Johnny Mahlangu, Dana Matthews, Kevin McRedmond, Shannon Meeks, Alexis Thompson, Christopher Walsh, Raymond G. Watts, and Janice Withycombe.
This study was supported by the Personalized Approaches to Hemophilia (PATH) study (National Institutes of Health 1RC2-HL-101851; principal investigators, T. Howard and K.P.P) and R01-HL-130448 (principal investigator, K.P.P.).
The opinions or assertions contained herein are the private ones of the authors and are not to be construed as official or reflecting the views of the Department of Defense or the Uniformed Services University of the Health Sciences.
Authorship
Contribution: D.G., P.V., S.B., S.T., K.P.P., and K.G.M. designed experiments; D.G., P.V., S.B., and S.T. performed experiments and analyzed data; S.T. and G.F.P. produced recombinant BDD-FVIII proteins during their employment at Biogen; C.O. performed biostatistical analysis; K.P.P., C.O., and K.G.M. analyzed data and wrote the manuscript; and all authors reviewed and approved the manuscript.
Conflict-of-interest disclosure: K.G.M. is a shareholder of Haematologic Technologies Inc., and a consultant for Baxalta, Diagnostica Stago, Bayer, CSL Behring, Alnylam, Shire, Takeda, and Novo Nordisk. K.P.P. is an inventor on patents related to FVIII immunogenicity. S.T. and G.F.P. are former employees of Biogen. The remaining authors declare no competing financial interests.
Correspondence: Kathleen P. Pratt, Department of Medicine (MED) A3063, Uniformed Services University of the Health Sciences, 4301 Jones Bridge Rd, Bethesda, MD 20814; e-mail: kathleen.pratt@usuhs.edu; and Kenneth G. Mann, University of Vermont, 72 East Shore Rd, Grand Isle, VT 05458; e-mail: kgmann1@comcast.net.
References
Author notes
Presented in abstract form at the ISTH 2021 Congress in July 2021.
Descriptions of the factor VIII expression plasmids have been deposited in a public database: https://www.addgene.org/Robert_Peters/.
Data are available on request from the corresponding author, Kathleen P. Pratt (kathleen.pratt@usuhs.edu).
The full-text version of this article contains a data supplement.