Abstract
The terminology applied to autoimmune hemolytic anemia (AIHA) seems inconsistent. We aimed to evaluate the consistency of definitions used for diagnosis and treatment. In this systematic review of literature from January 2006 to December 2015, we assessed heterogeneity in the definition of AIHA and its subtypes, refractory disease, disease phase, severity, criteria for treatment response, and response durability. A Medline search for anemia, hemolytic, autoimmune was supplemented with keyword searches. Main exclusions were conference abstracts, animal and non-English studies, and studies with <10 cases. Of 1371 articles retrieved, 1209 were excluded based on titles and abstracts. Two authors independently reviewed 10% and 16% of abstracts and full papers, respectively. After full-paper review, 84 studies were included. AIHA was most frequently (32 [52%] of 61) defined as hemolytic anemia with positive direct antiglobulin test (DAT) and exclusion of alternatives, but 10 of 32 also recognized DAT-negative AIHA. A lower threshold for diagnosis of DAT-negative AIHA was observed in literature on chronic lymphocytic leukemia. Definitions of anemia, hemolysis, and exclusion criteria showed substantial variation. Definitions of primary/secondary cold agglutinin disease/syndrome were not consistent. Forty-three studies provided criteria for treatment response, and other than studies from 1 center, these were almost entirely unique. Other criteria were rarely defined. Only 7, 0, 3, 2, 2, and 3 studies offered definitions of warm AIHA, paroxysmal cold hemoglobinuria, mixed AIHA, AIHA severity, disease phase, and refractory AIHA, respectively. Marked heterogeneity in the time period sampled indicates the need to standardize AIHA terminology.
Introduction
Autoimmune hemolytic anemia (AIHA) is a decompensated acquired hemolysis caused by the host’s immune system acting against its own red cell antigens. AIHA is primary or secondary, depending on the presence of an underlying disease or condition promoting immune dysregulation. However, there are no standard diagnostic criteria for AIHA and its subtypes, with reviews often describing “typical” laboratory and clinical features. As a result, clinical studies have used different criteria for diagnosis and treatment response. These inconsistencies make it difficult to compare studies and determine best clinical practice. This in turn has become a limitation of systematic reviews, meta-analyses, and clinical guidelines1-3 that are based on this data.
A systematic review underpinning recent British guidelines on AIHA searched Medline and Embase for published English-language literature from January 1960 to October 2015.2 No study was found that specifically evaluated variability in the terminology used to define and treat AIHA. In a 2015 meta-analysis of the efficacy and safety of rituximab for AIHA, the variable definitions of treatment response, particularly partial response, were noted as a limitation of the analysis.3 A critical appraisal of terminology is overdue, given the growing number of therapeutic agents being assessed for efficacy in patients with AIHA.4
We have carried out a systematic review of recent literature to assess heterogeneity in AIHA terminology. The terminology under review included: diagnostic criteria for AIHA (including direct antiglobulin test [DAT]–negative AIHA), cold agglutinin (CA) disease (CAD), warm AIHA, paroxysmal cold hemoglobinuria (PCH), mixed AIHA, disease severity, disease phase, refractory disease, treatment response criteria, and assessment of response durability (Table 1). Through this, we aim to promote the development of agreed-on terminology for the definition of AIHA and the evaluation of its response to treatment.
The 10 diagnostic and response criteria reviewed
| Criteria . |
|---|
| AIHA (including DAT-negative AIHA) |
| CAD |
| Warm AIHA |
| PCH |
| Mixed AIHA |
| Disease severity |
| Disease phase |
| Refractory disease |
| Treatment response criteria |
| Assessment of response durability |
| Criteria . |
|---|
| AIHA (including DAT-negative AIHA) |
| CAD |
| Warm AIHA |
| PCH |
| Mixed AIHA |
| Disease severity |
| Disease phase |
| Refractory disease |
| Treatment response criteria |
| Assessment of response durability |
Methods
Search strategy
In May 2016, full-paper articles published from 2006 to 2015 were searched on the Medline database using the medical subjects heading term “anemia, hemolytic, autoimmune,” with explosion function and all subheadings included. The search was supplemented with keyword searches for: Evans syndrome, CAD, cold hemagglutinin disease, and paroxysmal cold hemoglobinuria (supplemental Figure 1).
Eligibility criteria, study selection, and data extraction
The titles and abstracts identified were then evaluated. Abstract-only papers and articles not written in English were excluded, as were laboratory studies with no clinical correlation, studies unrelated to AIHA, and animal studies. Reviews or guidelines were included, but case reports or original articles with <10 cases were excluded. The first 10% of titles and abstracts identified by the search strategy, from latest publication date, were reviewed independently by 2 authors (Q.A.H. and S.B.) against the eligibility criteria and the authors’ selections compared. Any differences in inclusion or exclusion of abstracts were reviewed and resolved through discussion. The remaining 90% of abstracts were then reviewed for eligibility by 1 author (Q.A.H.).
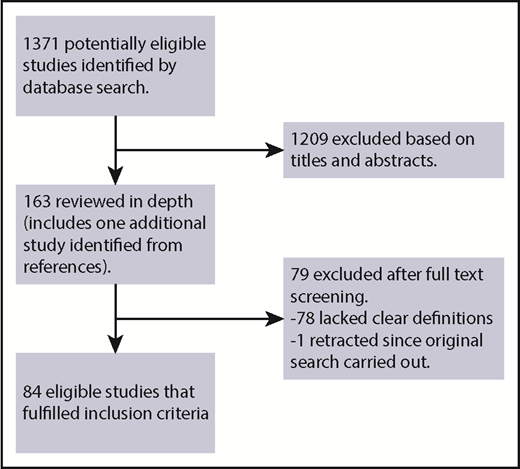
The complete articles meeting these criteria were then retrieved and reviewed. These articles were retained for final analysis if they offered a clear definition of ≥1 of the 10 diagnostic or response criteria listed in Table 1 (Figure 1). Although the definitions of primary vs secondary AIHA were not part of the search criteria, these are listed in supplemental Table 11 if present. For this review, the definition of AIHA as hemolysis caused by the host’s immune system acting against its own red cell antigens was considered descriptive and not accepted as a clinically applicable definition. The first 16% of complete articles were independently reviewed by 2 authors (Q.A.H. and S.B.). Data were extracted if a clear definition was provided, and differences in data extraction were compared and again resolved by review and discussion. The remaining 84% of articles were then reviewed by 1 author (Q.A.H.).
The definitions used for each of these criteria were extracted into supplemental Tables 1 to 10 and summarized as a narrative synthesis. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses checklist was used for the preparation of this review.5 The review methodology was agreed on before conducting the study, but a review protocol was not published. Because the review does not evaluate methodological quality, a risk-of-bias tool was not required.
Results
A total of 1371 abstracts and titles were initially retrieved. The first 137 (10%) of 1371 were reviewed independently by both authors and the authors’ selections compared. There was 91% agreement, with a κ statistic of 0.7, indicating substantial agreement.6 On the basis of their titles and abstracts, 1209 articles were excluded. The remaining 162 articles were retrieved for review and data extraction. The first 26 (16%) of 162 were independently reviewed by both authors. Comparison identified differences in data extraction from 6 of 26, resolved by discussion (missed data fields, n = 3; erroneous inclusion when definition unclear, n = 3). Seventy-eight articles were finally excluded based on a lack of clear definitions, and 1 paper had been retracted since the original search.7 One additional article8 meeting inclusion criteria was identified from an article reference; it was not detected in the original search. A total of 84 articles were therefore eligible for inclusion in this study (Figure 1). These consisted of 1 meta-analysis, 4 clinical trials, 60 case-control, case series, or cohort studies, 3 laboratory studies, and 16 reviews.
Definitions of disease, disease severity, and disease phase
AIHA was defined in 61 papers (supplemental Table 1). The most commonly used definition (n = 32) was hemolytic anemia with positive DAT and exclusion of alternatives, although 10 of 32 also provided criteria for DAT-negative AIHA. The second most common definition (n = 16) was hemolytic anemia with positive DAT, although 3 of these papers also provided criteria for DAT-negative AIHA. Four used hemolysis and positive DAT with or without exclusion of alternatives, 2 used symptomatic anemia and positive DAT, 2 used hemolysis and positive red cell antibody serology, and the remaining 5 all differed from one another and the definitions used in the others (Table 2). There was considerable variation in how anemia, hemolysis, and exclusion criteria were defined. For example, anemia was either undefined, defined as a fall of at least 20 or 30 g/L, or defined as hemoglobin (Hb) <90, 100, 110, 120, or (in men) 130 g/L.
Diagnostic criteria for AIHA
| Criteria* . | Studies (N = 61) . |
|---|---|
| Hemolytic anemia with positive DAT and exclusion of alternatives | 32 |
| Hemolytic anemia with positive DAT | 16 |
| Hemolysis and positive DAT (± exclusion of alternatives) | 4 |
| Symptomatic anemia and positive DAT | 2 |
| Hemolysis and positive red cell serology | 2 |
| Unique/unrelated definitions | 5 |
| Criteria* . | Studies (N = 61) . |
|---|---|
| Hemolytic anemia with positive DAT and exclusion of alternatives | 32 |
| Hemolytic anemia with positive DAT | 16 |
| Hemolysis and positive DAT (± exclusion of alternatives) | 4 |
| Symptomatic anemia and positive DAT | 2 |
| Hemolysis and positive red cell serology | 2 |
| Unique/unrelated definitions | 5 |
17 of 61 papers also had criteria for DAT-negative AIHA.
DAT-negative AIHA was defined in 17 (28%) of 61 papers overall. Chronic lymphocytic leukemia (CLL)–associated AIHA was considered in 13 of 61 papers overall. Of the 13 papers concerning CLL, 7 (54%) defined DAT-negative AIHA, and none of these required evidence of red cell antibodies or steroid response to diagnose DAT-negative AIHA. In contrast, of 10 of 17 papers defining DAT-negative AIHA and not specifically considering CLL, 7 of 10 required evidence of red cell directed antibodies by another method9-13 and/or evidence of steroid responsiveness.9,14,15
Thirty-seven papers distinguished primary and secondary AIHAs (supplemental Table 11). AIHA was considered primary in the absence of an associated disorder and secondary when an associated disorder was present. Studies listed common associations such as lymphoproliferative disorders and autoimmune and infectious diseases with varying degrees of detail. Some authors noted that the strength of evidence was variable for an association between AIHA and some conditions within these broad categories.16,17 Drug-induced immune hemolysis was sometimes categorized as secondary AIHA10,11,18-21 but also as a distinct AIHA subgroup22 or distinct category of immune hemolysis.14,16 Eleven papers defined primary CAD vs secondary CAD or secondary CA syndrome (CAS). All 8 Nordic papers defined primary CAD as the absence of associated disorders with the exception of a B-cell clonal lymphoproliferative disorder but without overt (eg, clinical or radiological) evidence of malignancy. Secondary disease (associated with malignancy or infection) was defined as CAS in 2 papers23,24 but as secondary CAD in the remaining 6.25-30 Other authors defined primary CAS (idiopathic16 or idiopathic but in most cases with evidence of a lymphoproliferative disorder22 ) or primary CAD (idiopathic)31 and secondary CAS (infection or malignancy)16,22 or secondary CAD (associated with a B-cell lymphoproliferative disorder).31
Thirteen papers offered a definition of CAD (supplemental Table 2). Eight of these were from 1 group and defined CAD as: chronic hemolysis, positive polyspecific DAT, monospecific DAT strongly positive for C3d (and negative or weakly positive with immunoglobulin G [IgG] in 3 of 8 papers), and CA titer of ≥64 at 4°C. In the remaining 5 articles, clinical significance was attached to a CA titer of >64 (n = 2), 258, or 500 or titer not specified. One definition required CA to have an anti-I specificity,32 and another required it to have a thermal amplitude up to at least 30°C.16
Of 7 of 84 papers that offered criteria for warm AIHA (supplemental Table 3), 4 based these solely on the presence of DAT positive for IgG with or without C3d9,32-34 ; a fifth article was the same but also stated that CAD was an exclusion criterion.18 The sixth included patients with DAT positive for IgG with or without C3d but also included those with DAT positive for C3d if CAS had been excluded.35 The seventh required 2 of 3 of the following: DAT positive for IgG with or without IgA or IgM, positive eluate indirect antiglobulin test (IAT; with warmed washed red cells at 37-40°C), and positive serum IAT (warmed to 37-40°C).36
No study defined PCH (supplemental Table 4), but 3 papers defined mixed AIHA (supplemental Table 5). All required AIHA with DAT positive for C3d and IgG. Two required the detection of both warm autoantibodies (method was not defined) and high-titer CAs.9,32 The third required evidence of a cold antibody, defined as an agglutinin strongest at 0 to 10°C and reactive at ≥30°C, and a warm antibody, again defined as 2 of 3 of the following: IgG-positive DAT, positive eluate IAT, or positive serum IAT.36
Two papers provided differing definitions of severity (supplemental Table 6). In 1 paper, severe was Hb ≤60 g/L not maintained by daily transfusion, and extremely severe was Hb <30 g/L.19 In the other, very severe was Hb ≤60 g/L; severe, Hb 61 to 80 g/L; moderate, Hb 81 to 100 g/L; and mild, Hb >100 g/L.32
Only 2 papers provided criteria for disease phase (supplemental Table 7). One defined chronic as persisting >6 months37 ; the other, by analogy to current criteria for immune thrombocytopenia, described newly diagnosed (within 3 months from diagnosis), persistent (3-12 months from diagnosis), and chronic (lasting >12 months) phases.20
Criteria for refractory disease, treatment response, and response duration
Three papers defined refractory AIHA (supplemental Table 8): 1 by steroid nonresponse or dependence,3 1 by failure to respond after ≥4 treatment modalities,38 and a third by the need for treatment after ≥2 prior treatment lines or dependence on treatment to maintain a response after ≥3 lines.39
Forty-three studies provided criteria for treatment response (supplemental Table 9). Five categorized response uniquely as: recovery,40 remission,41 initial response/complete response/no response,12 complete response only,20 or improvement/stable/ineffective.19 Seven reported on a single category of response, but definitions ranged from the nonspecific “improvement in clinical symptoms”17(p1116) to the more detailed “hemoglobin levels reached 100 g/L in the absence of hemolysis (normal corrected reticulocyte count, normal lactate dehydrogenase [LDH] and haptoglobin levels).”42(p3059) All 7 differed from one another except for 2 papers from the same group, which defined response as transfusion independence and Hb >20 g/L above baseline and an absolute value >80 g/L.15,43 The remaining 31 papers divided response assessment into partial (PR) and complete response (CR), with 2 of these also defining a maintained39 or sustained44 response and 14 also defining no response. In all 14, no response was when patients did not meet criteria for PR or CR. Of the 31 defining CR/PR, 7 were for patients with CAD. In all 7, response criteria included a reduction in clonal disease and cold-associated symptoms as well as anemia and hemolysis. One group, responsible for defining response in 6 of 7 studies, used the same criteria. CR (primary CAD) was the absence of anemia, no signs of hemolysis, and disappearance of clinical symptoms of CAD. Additional requirements were no detectable monoclonal serum protein and no signs of clonal lymphoproliferation as assessed by bone marrow histology, immunohistochemistry, and flow cytometry. PR was a stable increase in Hb level by at least 20 g/L or to the normal range, along with a reduction of serum IgM level by at least 50% of the initial level or to the normal range, improvement of clinical symptoms, and transfusion independence. Definitions of CR and PR in the remaining 24 studies are summarized in Table 3.
Definitions of CR and PR in patients treated for AIHA
| Response . | Definition . | |
|---|---|---|
| CR (n = 24) | ||
| Hb > or ≥120 g/L (n = 10) | ||
| >120 | Plus Hb increase of at least 20 g/L above pretreatment Hb without transfusion or concomitant therapy (n = 1) | |
| > or ≥120 | Plus no laboratory features of hemolysis* (n = 4)† | |
| > or ≥120 | Plus no laboratory features of hemolysis | Plus independent from transfusion (n = 4)‡ |
| ≥120 | Plus no laboratory features of hemolysis and independent from transfusion | Plus on no medication except steroids at stable or reducing dose (n = 1) |
| Normalization of Hb (n = 9) | ||
| Normalization of Hb only (n = 1) | ||
| Normalization of Hb | Plus no laboratory features of hemolysis (n = 1) | |
| Plus no laboratory features of hemolysis | Plus no detectable antibodies in serum or eluate or on red cells (n = 2) | |
| Plus no laboratory features of hemolysis | Plus sustained for at least 6 mo (n = 1) | |
| Plus no laboratory features of hemolysis | Plus without ongoing immunosuppresion (n = 2) | |
| Plus no laboratory features of hemolysis | Plus no transfusion (n = 1) | |
| Plus no laboratory features of hemolysis | Plus independent from additional treatment (n = 1) | |
| Hb > or ≥110 g/L (n = 5) | ||
| >110 (n = 2) | ||
| ≥110 | Plus reticulocytes <120 × 109/L (irrespective of treatment or DAT) (n = 1) | |
| >110 | Plus reticulocytes <120 × 109/L for 4 wk | Plus no rescue or supportive regimens during that time (n = 1) |
| >110 (women) or 120 (men) | Plus no laboratory features of hemolysis | Plus not on treatment (n = 1) |
| PR (n = 24) | ||
| Minimum Hb 100 g/L (n = 9) | ||
| ≥100 or 100-120 or rise of at least 20 | Plus no transfusion (n = 2) | |
| ≥100 or rise of at least 20 | Plus absence of any treatment (n = 1) | |
| >100 or rise of at least 20 | Plus maintained for at least 6 mo posttreatment (n = 1) | |
| ≥100 and rise of at least 20 | Plus persistent hemolysis (n = 2) | |
| ≥100 and rise of at least 20 | Plus no transfusion (n = 1) | |
| ≥100 and rise of at least 20 | Plus without hemolysis or with hemolysis if Hb stable | Plus no medication except steroid at stable or reducing dose (n = 1) |
| ≥100 and rise of at least 20 | Plus persistent hemolysis | Plus no transfusion in last 2 wk and off treatment or stable dose of prednisolone at ≤10 mg (n = 1) |
| Minimum Hb 70-90 g/L (n = 5) | ||
| 90-110 (n = 1) | ||
| >80 but below normal (n = 1) | ||
| 80-110 or if baseline >80, then rise >15 (n = 1) | ||
| 70-110 ± reticulocytosis (>120 × 109/L) or >110 with reticulocytosis (n = 1) | ||
| 70-110 or >110 with reticulocytosis (>120 × 109/L) | Plus sustained during 4 consecutive wk without rescue or supportive care regimens (n = 1) | |
| No absolute minimum Hb (g/L) threshold (n = 10) | ||
| Increase of at least 20 and/or transfusion independence if previously dependent (n = 1) | ||
| Increase of at least 20 | Plus Hb <120 g/L ± persistent hemolysis (n = 1) | |
| Increase of at least 20 | Plus improved markers of hemolysis but Hb <120 g/L | Plus reduced transfusion (n = 1) |
| Hb increase of at least 20 g/L | Plus improved clinical and laboratory signs of hemolysis | Plus transfusion free or reduced requirements (n = 2) |
| Improvement in hemolysis markers but need for maintenance treatment (n = 1) | ||
| Improvement in laboratory markers or decrease in transfusion requirements but persistence of detectable antibodies (n = 2) | ||
| Improved clinical and laboratory analysis and/or steroid dependence despite presence of autoantibodies (n = 1) | ||
| CR except requiring maintenance prednisolone <10 mg/d or stable hemolysis with acceptable Hb without treatment except prednisolone <10 mg/d (n = 1) | ||
| Response . | Definition . | |
|---|---|---|
| CR (n = 24) | ||
| Hb > or ≥120 g/L (n = 10) | ||
| >120 | Plus Hb increase of at least 20 g/L above pretreatment Hb without transfusion or concomitant therapy (n = 1) | |
| > or ≥120 | Plus no laboratory features of hemolysis* (n = 4)† | |
| > or ≥120 | Plus no laboratory features of hemolysis | Plus independent from transfusion (n = 4)‡ |
| ≥120 | Plus no laboratory features of hemolysis and independent from transfusion | Plus on no medication except steroids at stable or reducing dose (n = 1) |
| Normalization of Hb (n = 9) | ||
| Normalization of Hb only (n = 1) | ||
| Normalization of Hb | Plus no laboratory features of hemolysis (n = 1) | |
| Plus no laboratory features of hemolysis | Plus no detectable antibodies in serum or eluate or on red cells (n = 2) | |
| Plus no laboratory features of hemolysis | Plus sustained for at least 6 mo (n = 1) | |
| Plus no laboratory features of hemolysis | Plus without ongoing immunosuppresion (n = 2) | |
| Plus no laboratory features of hemolysis | Plus no transfusion (n = 1) | |
| Plus no laboratory features of hemolysis | Plus independent from additional treatment (n = 1) | |
| Hb > or ≥110 g/L (n = 5) | ||
| >110 (n = 2) | ||
| ≥110 | Plus reticulocytes <120 × 109/L (irrespective of treatment or DAT) (n = 1) | |
| >110 | Plus reticulocytes <120 × 109/L for 4 wk | Plus no rescue or supportive regimens during that time (n = 1) |
| >110 (women) or 120 (men) | Plus no laboratory features of hemolysis | Plus not on treatment (n = 1) |
| PR (n = 24) | ||
| Minimum Hb 100 g/L (n = 9) | ||
| ≥100 or 100-120 or rise of at least 20 | Plus no transfusion (n = 2) | |
| ≥100 or rise of at least 20 | Plus absence of any treatment (n = 1) | |
| >100 or rise of at least 20 | Plus maintained for at least 6 mo posttreatment (n = 1) | |
| ≥100 and rise of at least 20 | Plus persistent hemolysis (n = 2) | |
| ≥100 and rise of at least 20 | Plus no transfusion (n = 1) | |
| ≥100 and rise of at least 20 | Plus without hemolysis or with hemolysis if Hb stable | Plus no medication except steroid at stable or reducing dose (n = 1) |
| ≥100 and rise of at least 20 | Plus persistent hemolysis | Plus no transfusion in last 2 wk and off treatment or stable dose of prednisolone at ≤10 mg (n = 1) |
| Minimum Hb 70-90 g/L (n = 5) | ||
| 90-110 (n = 1) | ||
| >80 but below normal (n = 1) | ||
| 80-110 or if baseline >80, then rise >15 (n = 1) | ||
| 70-110 ± reticulocytosis (>120 × 109/L) or >110 with reticulocytosis (n = 1) | ||
| 70-110 or >110 with reticulocytosis (>120 × 109/L) | Plus sustained during 4 consecutive wk without rescue or supportive care regimens (n = 1) | |
| No absolute minimum Hb (g/L) threshold (n = 10) | ||
| Increase of at least 20 and/or transfusion independence if previously dependent (n = 1) | ||
| Increase of at least 20 | Plus Hb <120 g/L ± persistent hemolysis (n = 1) | |
| Increase of at least 20 | Plus improved markers of hemolysis but Hb <120 g/L | Plus reduced transfusion (n = 1) |
| Hb increase of at least 20 g/L | Plus improved clinical and laboratory signs of hemolysis | Plus transfusion free or reduced requirements (n = 2) |
| Improvement in hemolysis markers but need for maintenance treatment (n = 1) | ||
| Improvement in laboratory markers or decrease in transfusion requirements but persistence of detectable antibodies (n = 2) | ||
| Improved clinical and laboratory analysis and/or steroid dependence despite presence of autoantibodies (n = 1) | ||
| CR except requiring maintenance prednisolone <10 mg/d or stable hemolysis with acceptable Hb without treatment except prednisolone <10 mg/d (n = 1) | ||
Laboratory assessment of hemolysis varied.
Irrespective of the DAT result (n = 1).
Irrespective of the DAT result (n = 1).
In assessing response duration (supplemental Table 10), we examined how relapse was defined and duration reported. Thirty-three papers reported on 1 or both of these. Three did not report on or define relapse, despite reporting response duration. Eighteen reported relapse without defining it, and 12 reported and defined relapse. Of the remaining 12, 4 defined it as loss of response31,32,42,45 and 2 as recurrence of AIHA as defined in their study.46,47 In 3, relapse required the need for additional treatment.12,18,34 Duration was most frequently presented as relapse-free survival or median duration of response. Response duration was calculated as starting from treatment47 or response17,28 and lasted until relapse28,47 or next treatment.17,46 Other analyses included recurrence rate per 100 person-years48 and incidence of relapse (episodes per person per year).41
Discussion
This systematic review found enormous variation in how terminology is used to describe AIHA and its response to treatment. Although DAT is a key test, it is not completely sensitive or specific, and therefore, DAT-positive and -negative AIHA are described. The most frequently applied definition of AIHA, used in just more than half the studies, was DAT-positive hemolytic anemia after exclusion of alternatives. Exclusion is necessary, because DAT-positive hemolysis can occur in other circumstances, such as a delayed hemolytic transfusion reaction. Only a quarter of papers defining AIHA included DAT-negative AIHA. This likely reflects the deliberate exclusion of a smaller less well-defined category from clinical studies rather than disagreement over its validity.
The concept of DAT-negative AIHA arises from patients with hemolysis and no alternative cause identified after extensive investigation, who destroy transfused compatible red cells at a similar rate to their own, indicating an extrinsic mechanism for red cell destruction.49 Patients often respond to steroids,50 have red cell bound antibodies detectable by sensitive methods,9,51 and make up ∼2% to 6% of all AIHA cases.32,52,53
We found a greater tendency to define and include patients with DAT-negative AIHA in studies of AIHA secondary to CLL. In these studies, positive DAT could be replaced by reticulocytosis and another laboratory marker of hemolysis54-57 or by 2 markers of hemolysis.8,58,59 The extent to which alternative causes were excluded varied, including: no evidence of bleeding,58 no bleeding or hypersplenism,8 no alternative cause,54,57,59 no chemotherapy in the preceding month, and supportive bone marrow findings.55 Hemolytic markers such as lactate dehydrogenase and reticulocyte count are not specific for hemolysis and can be influenced by the underlying disease and its treatment.60 Despite this, these less specific criteria did not seem to have increased the overall number of CLL patients who were diagnosed with AIHA: 10% to 11% in series requiring positive DAT61,62 vs 2% to 12% in those that also included DAT-negative AIHA.54,55,57,59 However, DAT-negative cases made up 7%,55 14%,59 52% (based on DAT at study entry),54 and 82%58 of the total AIHA cases in CLL series using these criteria, much higher than the anticipated 2% to 6%. The lowest value (7%) came from a series that required no chemotherapy in the previous month, whereas in the highest (82%), 12 of 14 cases were diagnosed during chemotherapy, suggesting that variation in exclusion criteria influenced the frequency of diagnosis.
There was consensus that primary (idiopathic) AIHA occurred when there was no associated condition, with less certainty about the strength of association for some conditions and whether drug-induced immune hemolytic anemia should be classified as secondary AIHA. Terminology for primary and secondary cold antibody–mediated AIHAs was inconsistent, with the use of various combinations of primary/secondary CAD/CAS. The alternative term cold hemagglutinin disease was also employed,2 avoiding potential confusion with the human blood group antigen Cad.63
For the diagnosis of CAD, most studies required CA to be identified at 4°C, although the minimum titer considered significant varied from 64 to 500. One study required CA to have a thermal range up to 30°C, and some investigators found thermal range to be a better indicator of clinical significance.49 The reason for testing for CA in patients with AIHA and DAT positive for C3d is that C3d may be found in both cold and warm AIHA,64 and patients with CAD do not always have cold-associated symptoms.17 The reason for testing the titer or thermal range is that clinically insignificant CAs occur naturally. At 4°C, an insignificant CA is typically positive with a dilution <64 and rarely exceeds 256, whereas in CAD, the titer is usually ≥512.24,65 However, exceptions occur, and variations in diagnostic criteria reflect the absence of a cutoff titer or thermal amplitude with a proven high sensitivity and specificity. It is also important to recognize that CA activity and severity of hemolysis may show considerable interindividual variation, even among patients with the same titer.66 To some extent, therefore, any sharp cutoff will be arbitrary, and the thermal amplitude will reflect the immunologic activity better than the titer. Furthermore, the titer is susceptible to variations resulting from suboptimal handling of blood samples as well as laboratory procedures for titration.67
Four studies diagnosed warm AIHA in the presence of DAT positive for IgG with or without C3d. However in the presence of C3d, DAT in isolation cannot distinguish cold from warm AIHA, and in another study, patients with DAT positive for C3d only were included after exclusion of CAS.35 Because of the lack of studies in this rare disorder, PCH was not defined in the period under review, but it is usually diagnosed in patients with AIHA and a positive Donath-Landsteiner test.2,68 Disease severity, disease phase, and refractory disease were not concepts that were frequently or consistently applied in patients with AIHA.
The exact criteria used for treatment response in 43 studies were almost entirely unique, other than studies from the same authors, and there is a clear need for standardized criteria. Nearly three quarters described PR and CR. Most defined CR as normal Hb or Hb ≥110 to 120 g/L, with normalized laboratory markers of hemolysis with or without transfusion independence. PR was more variably defined, but within those definitions, 14 (58%) of 24 authors required a minimum rise in Hb of 20 g/L to indicate response (Table 3). Some response definitions required patients to be on stable or reducing steroids or to be off treatment. However, treatment considerations may be better used to define remission and/or response duration. Treatment response criteria for patients with CAD included assessment of response of the underlying clonal disorder and cold-associated symptoms. Although holistic, these criteria do not allow comparison of hematological response with patients with warm AIHA, in whom response assessment is based only on hematological parameters. Another limitation of holistic criteria will be in the future evaluation of complement inhibitors69 to treat CAD, because it is anticipated that these agents will not influence the clonal disease or IgM-mediated agglutination that leads to cold-associated symptoms.
In assessing response duration, we found that relapse often went undefined. Also, when specified, response duration began at the start of treatment or start of response and ended at relapse or next treatment. These uncertainties and variations will reduce both accuracy and comparability.
Limitations of this systematic review include review of only English-language papers, although all English-language papers meeting eligibility criteria were retrieved and reviewed. Although there was substantial agreement between authors and differences were reviewed and resolved, independent review by 2 authors was only carried out for 10% of the titles/abstracts and 16% of the full papers, increasing the risk that some eligible studies were missed; this is a study limitation. The study assessed a relatively small time period (10 years), and criteria are likely to change further over time as understanding of the condition evolves. Data extraction from the rituximab meta-analysis captured similar variability in response criteria over a more extended period (2001-2014).3 However, it is also possible that evaluation of a longer time period would better describe terminology that was infrequently defined in our study (eg, warm AIHA, PCH, mixed AIHA, AIHA severity, disease phase, and refractory AIHA). A potential for bias arises from frequent publication by centers with a special interest, giving an exaggerated impression of uniformity and consensus on diagnostic and treatment criteria. We have highlighted this effect where needed, particularly in relation to CAD.
In conclusion, this is the first study to systematically assess the terminology applied to AIHA. It has revealed inconsistent use of definitions and no consensus on the criteria used for treatment response. Multiple inhibitory agents that act on different steps in immune response (eg, B cells, plasma cells, complement, spleen tyrosine kinase, and proteasomes) are currently undergoing evaluation in patients with AIHA. Therefore, there is an urgent need to standardize criteria for AIHA. A recent British guideline provides a useful approach to the diagnosis of AIHA and its subtypes2 but does not propose standardized terminology for diagnosis or treatment response. Although available evidence may not allow the formulation of “correct” terminology, achieving a measure of consensus to improve consistency would be a step forward in our understanding of this condition. An international consensus meeting has taken place, and the resulting diagnosis and treatment recommendations are anticipated.
The full-text version of this article contains a data supplement.
Authorship
Contribution: All authors contributed to the writing of the manuscript through critical review, comments, and approval of early drafts of the manuscript, and approved the final draft for publication; Q.A.H. conceived and contributed to study design, contributed to data extraction, analysis, and interpretation, and wrote the paper; A.H. contributed to data analysis and interpretation; and S.B. contributed to study design, data extraction, and data analysis and interpretation.
Conflict-of-interest disclosure: Q.A.H. has received honoraria from Bioverativ and Apellis and research funding from Alexion. A.H. has received honoraria from Bioverativ, Apellis, and Alexion. S.B. has received research funding from Mundipharma and honoraria from Apellis, Bioverativ, Momenta Pharmaceuticals, and True North Therapeutics.
Correspondence: Quentin A. Hill, Department of Haematology, St James’s University Hospital, Beckett St, Leeds LS9 7TF, United Kingdom; e-mail quentinhill@nhs.net.