Key Points
Low early childhood antimicrobial use supports the late infection hypothesis in young adult nodular sclerosis HL.
High childhood antimicrobial use suggests immune dysfunction to be important in young adult mixed cellularity HL etiology.
Abstract
The peculiar bimodal age distribution of Hodgkin lymphoma (HL), together with other epidemiological findings, inspired the so-called “late infection hypothesis” in the 1970s. Under this model, HL in young adults is caused by delayed infection with a relatively common agent, with HL risk increasing with age at infection. We time-dependently tallied prescriptions filled, for a broad spectrum of antimicrobials, at age 0 to 9 years for all Danish HL patients diagnosed in 1997 to 2015 at age 10 to 25 years (n = 296) and up to 10 controls for each of these, individually matched for sex and birthdate (n = 2688). Antimicrobial use was taken as a proxy for general infectious disease pressure. Analyses were also stratified by the 2 main histological subtypes: nodular sclerosis HL (NSHL) (n = 206) and mixed cellularity HL (MCHL) (n = 47). We compared antimicrobial use at ages 0 to 9 years between cases and comparators using stratified Cox regressions with repeated follow-up for a next prescription, to produce hazard ratios (HRs) of antimicrobial use according to (future) HL status. Reverse causation was mitigated by disregarding risk time <2 years before HL (pseudo)diagnosis. Analyses were adjusted for number of older and younger siblings. NSHL patients had received statistically significantly fewer antimicrobials than comparators early in life (HR0-2 years, 0.79; 95% confidence interval, 0.66-0.95), whereas patients with MCHL had received statistically significantly more antimicrobials than comparators throughout the first 10 years of life (HR0-9 years, 1.53; 95% confidence interval, 1.33-1.76). The late infection hypothesis was supported in NSHL, whereas immune dysfunction seemed more prominent in MCHL etiology.
Introduction
It has long been recognized that Hodgkin lymphoma (HL) incidence among adolescents and younger adults (AYAs) varies with the level of socioeconomic development in the underlying population.1 Specifically, whereas an AYA nodular sclerosis HL (NSHL) incidence peak is characteristic of affluent Western populations, absence of the peak is equally characteristic of socioeconomically deprived populations.2
The presumed background for the AYA HL incidence variation is captured in the so-called “late infection model,” which has dominated epidemiological HL research for decades.1,3-6 The model posits that AYA HL is caused by delayed infection with a relatively common agent, with age at infection as an important risk modifier.6 Accordingly, under this model, the higher AYA incidence in affluent populations compared with deprived populations reflects corresponding differences in infectious disease pressure in early childhood in general and, by implication, in timing of the infection critical for AYA HL risk.
Studies have mostly supported the late infection model only indirectly by relating AYA HL risk with correlates of childhood infectious disease pressure, such as number of siblings, birth order, and history of infectious mononucleosis caused by Epstein-Barr virus (EBV) infection in adolescence.2 Accordingly, direct support for the model has largely been limited to interview-based case-control studies with ample risk for participation, recall, and exposure misclassification biases.7-10 In addition to providing only indirect or questionable evidence for the late infection model for AYA HL, the studies are also uninformative about age intervals during which infections may modulate AYA HL susceptibility. Rare exceptions to this malaise of biases are a twin study by Cozen et al11 and, especially, a register-based cohort study by Mack et al,12 even if these investigations were still restricted to the aforementioned indirect measures of infectious disease pressure and recall of a few common childhood infections. These studies both supported the delayed infection hypothesis, as well.11,12
Methods
To advance our understanding of AYA HL epidemiology, we used Danish health registers to test the late infection model by comparing childhood antimicrobial use between AYA HL patients and comparators. We identified all patients registered with classical HL (ICD10 C81) at ages 10 to 25 years between 1997 and 2015 in the Danish Cancer Register,13 when possible stratifying cases by histological subtype: NSHL (ICD-O-3 96633) and mixed cellularity HL (MCHL; ICD-O-3 96523). In the Danish Civil Registration System, we matched each HL patient by sex and birthdate with up to 10 individuals, who were alive and free of HL at index patient diagnosis.14 Sibship structure for the study participants was also obtained from the Danish Civil Registration System. For all participants, we obtained information on antimicrobial prescriptions (ATC codes J01A, J01C-J01G, J01M, J01X, J02A, J04A, J05A, P01A, P02C) from the Danish Prescription Register, which covers the period since 1996.15,16 The prescriptions included antibacterials, antimycobacterials, antifungals, antivirals, antiprotozoals, and anthelmintics.17
We compared antimicrobial use at ages 0 to 9 years between cases and comparators using the Andersen-Gill model to allow repeated follow-up for a next prescription after antimicrobial-specific treatment periods.17,18 We used stratified Cox regression, taking the matched design into account to produce hazard ratios (HRs) of antimicrobial use according to (future) HL status and modeling the age-specific effect of case status by fractional polynomials.19 Reverse causation was mitigated by disregarding risk time <2 years before HL (pseudo)diagnosis.20 Analyses were performed for HL overall, as well as for NSHL and MCHL. Sociodemographic confounding was addressed by adjusting time-dependently for number of older and younger siblings. The study was approved by the Danish Data Protection Agency (2015-57-0102).
Results
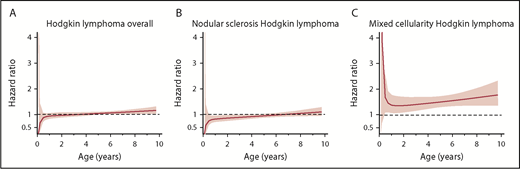
Overall, we identified 296 HL patients, of whom 206 had NSHL and 47 had MCHL, and 2688 comparators. Analyses for HL overall suggested that future AYA HL patients had received fewer antimicrobials than their peers early in childhood and had received more antimicrobials than their peers late in childhood (Figure 1A). However, analyses stratified by subtype revealed that this pattern reflected different trajectories for NSHL and MCHL. Specifically, NSHL patients had received statistically significantly fewer antimicrobials than comparators early in life (HR0-2 years, 0.79; 95% confidence interval, 0.66-0.95) (Figure 1B), whereas patients with MCHL had received statistically significantly more antimicrobials than comparators throughout the first 10 years of life (HR0-9 years, 1.53; 95% confidence interval, 1.33-1.76) (Figure 1C). Number of older siblings was a statistically significant predictor of antimicrobial use, but the adjustment for number of younger and older siblings had minimal impact of the effect of future case status (data not shown).
Use of antimicrobials in childhood by AYA HL patients relative to comparators. Age-specific HRs (lines) with 95% confidence intervals (shaded areas) for use of antimicrobials by patients with classical HL of any type (A) and by NSHL (B) and MCHL (C) patients relative to comparators. Inspection of graphs of antimicrobial use for cases and comparators revealed that our results were not driven by only few individuals (data not shown).
Use of antimicrobials in childhood by AYA HL patients relative to comparators. Age-specific HRs (lines) with 95% confidence intervals (shaded areas) for use of antimicrobials by patients with classical HL of any type (A) and by NSHL (B) and MCHL (C) patients relative to comparators. Inspection of graphs of antimicrobial use for cases and comparators revealed that our results were not driven by only few individuals (data not shown).
Discussion
Because of the limited information available about the myriad infections affecting persons during childhood, we chose antimicrobial prescriptions during childhood as a simple and operational proxy for age-specific infectious disease load. The examined list of antimicrobials pertained to bacterial, viral, fungal, and parasitic infections, whether transmissible or not, to optimize it as an approximation of the burden of infections experienced in early life.
Our observations for NSHL are entirely consistent with the predictions of the 40-year-old late infection model for AYA HL. Our analyses even refine the model somewhat by suggesting that the first 5 years of life are the most critical for AYA NSHL risk and by demonstrating heterogeneity between the NSHL and MCHL patient subsets, indicating that the model may not apply to AYA MCHL. The assertion that NSHL and MCHL are epidemiologically, if not etiologically, distinct is not new2,21 ; however, it remains uncertain how much of the differences between the 2 can be attributed to variations in tumor EBV-status prevalence.2
At the same time that our study supplements previous investigations, it also highlights their weaknesses. Accordingly, supporting the late infection hypothesis, case-control investigations have reported reduced risks of AYA HL with self-reported history of ≥1 specific childhood infectious disease, such as measles, mumps, and rubella.7-10 Inasmuch as our analyses suggest that the critical window of exposure for AYA NSHL is before age 5 years, such findings could easily be spurious and explained by methodological phenomena, especially recall bias. That said, in the prospective cohort study by Mack et al, mumps were also found to be statistically significantly protective against HL, which cannot be attributed to this type of bias.12
Classical HL can be divided into epidemiologically heterogeneous subgroups based on age at diagnosis, histological subtype, tumor EBV status, or even combinations thereof.2 Although the different epidemiological HL classification criteria overlap with one another, they are not congruent.2 Accordingly, although most MCHLs are EBV+ and most NSHLs are EBV−, NSHLs often make up more than half of all EBV+ HLs in affluent populations. Therefore, our observations for NSHL are compatible with an increased risk for EBV+ HL previously reported among adolescents with EBV-related infectious mononucleosis.22 At the same time, the proportion of AYA HL that is attributable to infectious mononucleosis is too small to fully explain our findings for NSHL, which, therefore, presumably predominantly reflect associations pertaining to EBV− AYA HL.22
The observed trajectory for MCHL differed markedly from that of NSHL. Because most MCHLs are EBV+, the increased childhood antimicrobial use among (future) AYA MCHL patients agrees well with the established association between immune dysfunction and EBV+ HL risk.2 Therefore, the current results for MCHL suggest that a subset of EBV+ AYA HL exists that is not caused by primary EBV infection, but rather by an immunological inability to control latent infection with the virus for reasons related to constitution, comorbidity, or childhood socioeconomic environment.21 Another interpretation of the subtype-specific patterns is that the histological subtype is mainly determined by an immunological host reaction to infectious stimuli, with MCHL being a much more common histology in immunodeficient patients than in other patients.2
The increased risk of infections preceding AYA MCHL also has implications for the interpretation of patterns of AYA HL survivor morbidity. Studies have shown that, among other complications, AYA HL survivors are also at increased risk of being hospitalized for infections.23,24 The present investigation suggests that, to some extent, this increased risk may also reflect infection susceptibility predating AYA HL diagnosis and treatment in some patients.
The use of population-based high-quality registers with independent exposure and outcome registrations is a major strength of the present investigation. Accordingly, by design, the analyses are virtually free of the selection, recall, and exposure misclassification biases that hamper traditional interview-based case-control studies.2 Among the weaknesses in our investigation, we did not have access to information about the indications for the prescription of antimicrobials. Therefore, we can only speculate as to whether other conditions predisposing to infection and MCHL explain the trajectory for this tumor. Also, because we used register data, we had no information on HL EBV status, which is not routinely recorded. Finally, we did not adjust for socioeconomic status beyond number of younger and older siblings, which is believed to mediate, to a large extent, the association between socioeconomic status and AYA HL risk by being associated with infectious disease pressure in the first years of life.25-27 Therefore, we cannot rule out residual bias by socioeconomic status but believe it to be trivial, if present at all, and, therefore, unlikely to explain our findings.
In conclusion, AYA NSHL and MCHL patients differed from healthy comparators with regard to childhood antimicrobial use. Although observations for NSHL strongly supported the late infection model for HL, greater childhood antimicrobial use suggested an alternative model for AYA MCHL, in which immune dysfunction plays an important role.
Acknowledgments
This work was supported by The Danish Cancer Society (grant R40-A2167) (H.H.), by the Ulla and Mogens Folmer Andersen’s Foundation (grant 100041-1) (H.H.), and by the Danish Childhood Cancer Foundation (grant 2014-3464) (H.H.).
Authorship
Contribution: H.H., L.L.H., S.H.S., and K.R. designed the study; H.H. and K.R. analyzed data; H.H. and K.R. drafted the manuscript; and H.H., L.L.H., S.H.S., and K.R. contributed to the final version of the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Henrik Hjalgrim, Department of Epidemiology Research, Statens Serum Institut, 5 Artillerivej, DK-2300 Copenhagen S, Denmark; e-mail: hhj@ssi.dk.