Key Points
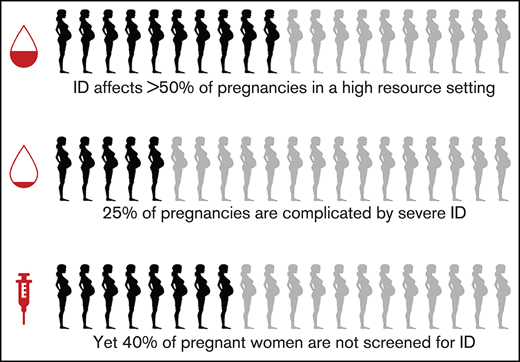
ID affects more than one-half of pregnancies in a high-resource setting, yet screening for ID is missed in 40% of pregnancies.
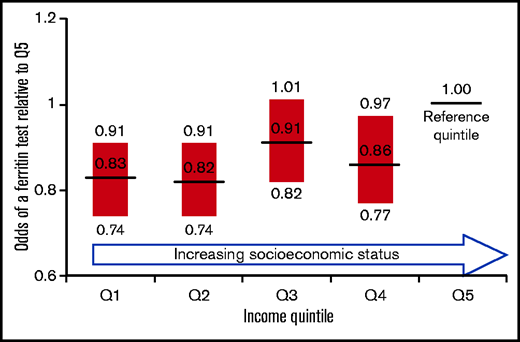
Females of lower socioeconomic status (SES) have a lower odds of ID screening in pregnancy compared with higher SES counterparts.
Abstract
Iron deficiency (ID) anemia in pregnancy is associated with poor maternal and childhood outcomes, yet ferritin testing, the standard test for ID, is not considered part of routine prenatal bloodwork in Canada. We conducted a retrospective cohort study of 44 552 pregnant patients with prenatal testing at community laboratories in Ontario, Canada, to determine the prevalence of ferritin testing over 5 years. Secondary objectives were to determine the prevalence and severity of ID and to identify clinical and demographic variables that influence the likelihood of ID screening. A total of 59.4% of patients had a ferritin checked during pregnancy; 71.4% were ordered in the first trimester, when the risk of ID is lowest. Excluding patients with abnormally elevated ferritins, 25.2% were iron insufficient (30-44 µg/L) and 52.8% were iron deficient (≤29 µg/L) at least once in pregnancy. A total of 8.3% were anemic (hemoglobin <105 g/L). The proportion of anemic patients with a subsequent ferritin test in pregnancy ranged from 22% to 67% in the lowest and highest anemia severity categories, respectively. Lower annual household income was negatively associated with the odds of a ferritin test; compared with those in the fifth (ie, highest) income quintile, the odds of ferritin testing for patients in the first, second, and fourth quintiles were 0.83 (95% confidence interval [CI], 0.74-0.91), 0.82 (95% CI, 0.74-0.91), and 0.86 (95% CI, 0.77-0.97), respectively. These data highlight gaps in prenatal care and issues of health equity that warrant harmonization of obstetrical guidelines to recommend routine ferritin testing in pregnancy.
Introduction
Iron deficiency (ID ) is the most widespread micronutritional deficiency in the world1 and disproportionately affects females because of increased iron requirements during menstruation, pregnancy, and lactation. ID is the most common cause of anemia in pregnancy. ID and ID anemia (IDA) represent a spectrum that begins with depletion of iron stores and progresses to an inability to support proper red blood cell synthesis. Estimates of the prevalence of ID among North American pregnant patients range from 16% to 77%, with rates increasing progressively across trimesters.2-7
IDA has been associated with poor maternal and fetal outcomes including maternal fatigue, cognitive dysfunction, depression, low birth weight, premature delivery, childhood ID, and anemia and poor cognitive development in the child.8-14 In two high-resource countries, maternal anemia early in pregnancy has been associated with severe maternal morbidity and mortality, and with increased risk of intellectual disability, autism spectrum disorder, and attention deficit/hyperactivity disorder in offspring.15,16 Moreover, it has been shown that proper management of ID reduces the risk of maternal postpartum blood transfusions and improves neonatal birth weight.11,17,18
Although most prenatal guidelines recommend screening for anemia in pregnancy, recommendations for ID screening are variable,19 and thus ID screening practices among clinicians are inconsistent.20 A hemoglobin check is often recommended as a screen for IDA; however, hemodilution resulting from increased plasma volume in pregnancy renders hemoglobin concentration an inaccurate indicator of iron stores and response to iron replacement.21,22 Furthermore, identification of ID without anemia allows for early supplementation to prevent progression to overt IDA. Ferritin levels provide an accurate assessment of iron stores and are thus considered the gold standard for diagnosis of IDA in pregnancy.23
The primary objective of this study was to determine the prevalence of ferritin testing over a 5-year period among pregnant patients with prenatal testing at outpatient private laboratories in Ontario. Secondary objectives were to determine the prevalence and severity of ID, and to identify clinical and demographic variables that influence the likelihood of ID screening in this population.
Methods
Study design
This was a retrospective cohort population-based study of pregnant females ages 13 to 54 years in Ontario, Canada, with laboratory testing between January 2013 and June 2018. Anonymized laboratory data were obtained from Dynacare, the second-largest private laboratory enterprise in Ontario, Canada, representing approximately one-third of nonhospital laboratory testing in the province. Data included laboratory test dates and results, patient age, sex, postal code, and ordering provider specialty. Data were obtained from Dynacare at no cost and without restrictions. Dynacare was not involved in study design, data analysis, nor in manuscript preparation. Study approval was granted by the research ethics board at St. Michael’s Hospital. The study was conducted in accordance with the Declaration of Helsinki. Further details on the study population are available in the supplemental Materials.
Pregnancy definitions
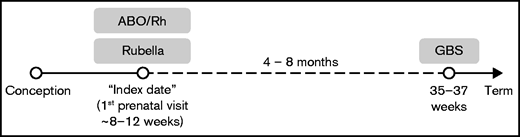
Based on antenatal screening in Ontario, a diagnosis of pregnancy was inferred from the co-occurrence of a Rubella and ABO/Rh test (referred to here as the “index date”), followed by a Group B Streptococcus (GBS) swab at least 4 months and no more than 8 months following the index date (Figure 1). Further details are available in the supplemental Data. Our definition of pregnancy was validated using a cohort of 1000 females who had β-human chorionic gonadotropin (β-HCG) testing at Dynacare between January 2016 and March 2017.
Laboratory definition of pregnancy based on prenatal testing guidelines. The “index date” is the date of the ABO/Rh and the Rubella tests, or if they occur on separate dates but within 28 days of each other, the earlier of the two. The GBS swab must occur at least 4 months and no greater than 8 months following the index date. Weeks refer to gestational age. Timeline is not to scale.
Laboratory definition of pregnancy based on prenatal testing guidelines. The “index date” is the date of the ABO/Rh and the Rubella tests, or if they occur on separate dates but within 28 days of each other, the earlier of the two. The GBS swab must occur at least 4 months and no greater than 8 months following the index date. Weeks refer to gestational age. Timeline is not to scale.
Anemia in pregnancy is generally defined as a hemoglobin of <110 g/L, <105 g/L, and <110 g/L in the first, second, and third trimesters, respectively.24 Without knowing precise trimesters for our population, we used a conservative hemoglobin cutoff of <105 g/L to define anemia at all time points. We defined normal iron stores, iron insufficiency, and iron deficiency as a ferritin 45 to 150 µg/L, 30 to 44 µ/L, and <30 µg/L, respectively.25-27
Income determination
The Environics Analytics DemoStats dataset was used to determine income. Postal codes from laboratory test requisitions were linked to the associated dissemination area using the Statistics Canada Postal Code Conversion File and the average annual household income for that dissemination area was then applied to the patient. If a patient had multiple ferritin tests in pregnancy, each with discrepant postal codes, the mean income across all ferritin testing dates was used. If a patient did not have a ferritin test, the service date closest to the index date was used to determine income. Annual household income quintiles were derived from the Statistics Canada 2016 census tables for Ontario and were applied to the cohort (supplemental Table 1).
Statistical analysis
Counts and percentages or means and standard deviations (SDs) were calculated to characterize the sample according to the different outcomes during specified time periods. The prevalence of ferritin or hemoglobin testing during an interval was calculated by dividing the number of patients who ever had a test for ferritin or hemoglobin by the total number of patients in the study. The 95% confidence intervals (CIs) were estimated using the Wald confidence limits method. To assess the association between dissemination area-derived census income quintile and ferritin testing, we considered each pregnancy separately and determined whether a ferritin had ever been ordered in that pregnancy. Generalized estimating equations with the logit link and unstructured correlation structure were used to estimate odds ratios and 95% CIs. All analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC).
Results
Validation of study pregnancy definition
Our definition of pregnancy was validated using a cohort of 1000 female patients who had β-HCG testing at Dynacare between January 2016 and March 2017. Of those, 497 had a positive β-HCG test. As expected, only a minority in our cohort had β-HCG testing; of the 17 840 patients who had an index date within the same time frame, only 128 had a β-HCG ordered. Of these, 119 (93%) were β-HCG positive within 90 days of the index date (supplemental Figure 1); therefore, of those women in our cohort who had a β-HCG test proximal to the index date, 93% were confirmed pregnant by both definitions.
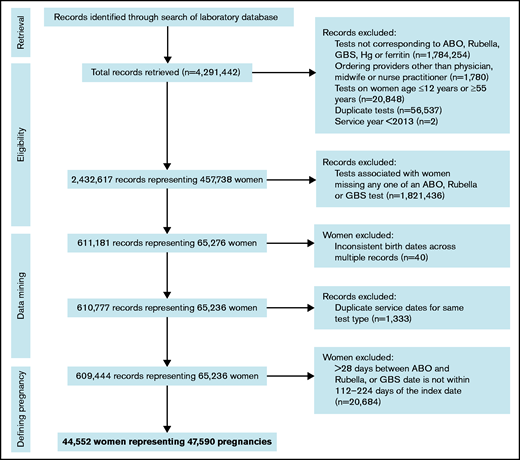
Patients
The Dynacare database was screened for pertinent laboratory test records of female patients performed from January 2013 to June 2018. A total of 4 291 442 records were retrieved. After excluding records based on eligibility criteria or duplication, 609 444 records remained. After excluding all records of individuals who did not meet our definition of pregnancy, 44 552 patients representing 47 590 pregnancies remained in the cohort (Figure 2). A total of 41 549 had 1 pregnancy, 2968 had 2 pregnancies, and 35 had 3 pregnancies within the study period. The median age across all pregnancies was 31 years (interquartile range [IQR] 28, 34 years).
STROBE flow diagram of participants screened for eligibility in the final cohort. “Records” refer to discrete laboratory tests. STROBE, strengthening the reporting of observational studies in epidemiology.
STROBE flow diagram of participants screened for eligibility in the final cohort. “Records” refer to discrete laboratory tests. STROBE, strengthening the reporting of observational studies in epidemiology.
Screening for iron deficiency
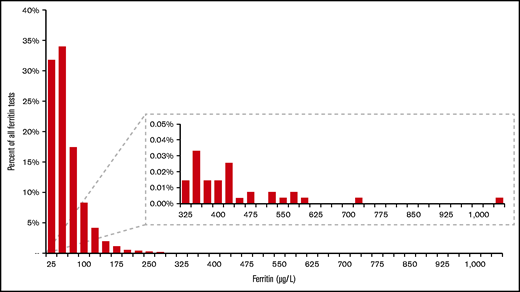
Of the 44 552 patients, 26 469 (59.4%) had a ferritin checked between 4 weeks before and 32 weeks following the index date, with a median ferritin of 36 µg/L (IQR 21, 61 µg/L). A total of 16 525 (62%) of these had a single ferritin test, whereas 9944 (38%) had ≥2 ferritin tests in this period. Nine hundred and eighty-eight patients had a ferritin greater than 150 µg/L (the upper limit of normal for females used by the laboratory) (Figure 3). Most ferritin tests were ordered by general practitioners (48.1%) and obstetricians/gynecologists (32.1%).
Histogram of ferritin values for 26 419 patients with a ferritin test. Of the 26 469 with a ferritin test ordered, 50 were missing results. Mean ferritin was 47 µg/L, median 36 µg/L. Inlay shows the data for higher ferritin values on an amplified y-axis.
Histogram of ferritin values for 26 419 patients with a ferritin test. Of the 26 469 with a ferritin test ordered, 50 were missing results. Mean ferritin was 47 µg/L, median 36 µg/L. Inlay shows the data for higher ferritin values on an amplified y-axis.
We then looked at all pregnancy-associated ferritin tests for a given patient, excluding abnormally elevated ferritin tests (>150 µg/L). Of these 25 880 patients, 45.6% had normal iron stores, 25.2% were iron insufficient, and 52.8% were iron deficient on at least 1 occasion in pregnancy. A total of 23.8% of patients were severely iron deficient (ferritin <15 µg/L) at least once in pregnancy; 30.2% of patients had never demonstrated iron insufficiency or ID in pregnancy (ie, all ferritin levels 45-150 µg/L).
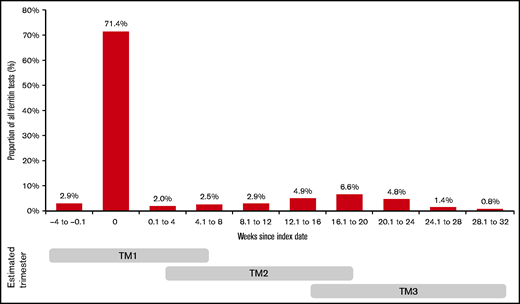
We evaluated the timing of the initial ferritin test in pregnancy (as an indicator of when ID screening occurs). A total of 71.4% of tests were ordered at the index date. Most other ferritin ordering occurred at a rate of <3% per month throughout the remainder of pregnancy, with a slight increase in frequency (4.7% to 6.6% per month) between 12 and 24 weeks following the index date (Figure 4).
Proportion of all ferritin tests ordered per 4-week interval relative to index date. Trimesters are estimated based on an assumed gestational age of 8 to 12 weeks at the index date (first prenatal visit). Areas where the gray bars overlap indicate lower confidence in the estimated trimester.
Proportion of all ferritin tests ordered per 4-week interval relative to index date. Trimesters are estimated based on an assumed gestational age of 8 to 12 weeks at the index date (first prenatal visit). Areas where the gray bars overlap indicate lower confidence in the estimated trimester.
Screening for anemia
Of the 44 552 patients in our cohort, 33 446 (75.1%) had a “baseline” hemoglobin level checked within 4 weeks before or following the index date. The mean baseline hemoglobin value was 126.9 g/L (SD 9.2 g/L). A total of 23 752 (71.0%) had at least 1 subsequent hemoglobin check following the baseline hemoglobin. The mean “subsequent hemoglobin” value was 116.6 g/L (SD 8.7). Among the 34 034 patients with at least 1 hemoglobin check in pregnancy, 2835 (8.3%) were anemic at least once. The frequencies of anemic test results and anemic patients, stratified by severity are presented in Table 1 and Table 2, respectively.
Severity of anemia as a percentage of all hemoglobin tests
| Hemoglobin level, g/L . | No. of tests (% of all hemoglobin tests) . |
|---|---|
| 100-104 | 2298 (3.28) |
| 90-99 | 1371 (1.96) |
| 80-89 | 228 (0.33) |
| 70-79 | 35 (0.05) |
| <70 | 8 (0.01) |
| Hemoglobin level, g/L . | No. of tests (% of all hemoglobin tests) . |
|---|---|
| 100-104 | 2298 (3.28) |
| 90-99 | 1371 (1.96) |
| 80-89 | 228 (0.33) |
| 70-79 | 35 (0.05) |
| <70 | 8 (0.01) |
Tests were ordered any time between 4 weeks before and 32 weeks following the index date. A total of 70 255 hemoglobin tests were ordered representing 34 034 patients; 185 ordered tests were missing results.
Ferritin checks following a diagnosis of anemia
| Hemoglobin level . | No. of pregnant patients (% of all patients with a CBC test) . | No. of pregnant patients with subsequent ferritin (% of anemia severity category) . |
|---|---|---|
| 100-104 g/L | 2014 (5.92) | 447 (22.19) |
| 90-99 g/L | 1046 (3.07) | 365 (34.89) |
| 80-89 g/L | 176 (0.52) | 68 (38.64) |
| 70-79 g/L | 26 (0.08) | 11 (42.31) |
| <70 g/L | 6 (0.02) | 4 (66.67) |
| Hemoglobin level . | No. of pregnant patients (% of all patients with a CBC test) . | No. of pregnant patients with subsequent ferritin (% of anemia severity category) . |
|---|---|---|
| 100-104 g/L | 2014 (5.92) | 447 (22.19) |
| 90-99 g/L | 1046 (3.07) | 365 (34.89) |
| 80-89 g/L | 176 (0.52) | 68 (38.64) |
| 70-79 g/L | 26 (0.08) | 11 (42.31) |
| <70 g/L | 6 (0.02) | 4 (66.67) |
The middle column shows the percentage of patients who had ever been anemic in pregnancy (at least 1 hemoglobin <105), stratified according to severity of anemia. The denominator is the total number of patients who had a hemoglobin test result in pregnancy (34 028). Multiple anemic hemoglobin levels for a single patient were accounted for separately. The far right column shows the frequency of ferritin checks stratified by anemia severity category. The denominator is the total number of patients in that anemia severity category. Tests were ordered any time between the index date and 32 weeks following it.
Investigating anemia
Of the 2835 patients with anemia, 774 (27.3%) had a subsequent ferritin test ordered in that pregnancy (up to 32 weeks following the index date). These ferritin tests were ordered at a median of 51 days (IQR 29, 81) from the initial hemoglobin that identified anemia. The proportion of anemic patients with a subsequent ferritin test increased with worsening anemia severity, ranging from 22% to 67% of patients in the lowest and highest anemia severity categories, respectively (Table 2).
Income quintiles and ferritin testing
The median after-tax household income of our cohort was CAD$82 448. The number of patients in each of quintile 1 (lowest income) to quintile 5 (highest income) is listed in supplemental Table 2. Quintiles (Qs) 1, 2, and 3 each had >20% of patients, with only 6.9% in Q4 and 4.1% in Q5. Compared with patients in Q5, the odds of a ferritin test were significantly lower for those in Q1, Q2, and Q4, but not for Q3. For patients in Q1, the odds of a ferritin test in pregnancy were 17.6% lower compared with patients in Q5 (Figure 5).
Odds of a ferritin test based on income quintile. The highest quintile (Q5) is the reference group. Annual household income was estimated using the patient’s postal code. Income quintiles were derived from provincial census data.
Odds of a ferritin test based on income quintile. The highest quintile (Q5) is the reference group. Annual household income was estimated using the patient’s postal code. Income quintiles were derived from provincial census data.
Discussion
We evaluated the prevalence of ID screening among a large cohort of pregnant Ontarian patients with outpatient prenatal testing, and identified laboratory and demographic variables associated with the likelihood of ID screening. Several key findings emerge from our data. First, ID screening occurred in only 59.4% of our cohort, despite a high prevalence of ID (52.8%) identified among those tested. The prevalence of ID was generally higher than that reported in previous North American studies, two of which provided estimates of 16% to 18% using overly restrictive ferritin cutoff levels of <12 to 15 µg/L.4,6 Using a similar ferritin threshold, we found the prevalence of severe ID to be 24%. A single-center Canadian study estimated the prevalence of ID in pregnancy to be 77% using a ferritin cutoff of <30 µg/L.7
Sixty-two percent of patients had only 1 ferritin test in pregnancy, and the vast majority (>70%) were ordered early in pregnancy, within the first trimester. These practices in Ontario suggest that a ferritin test should be included as part of the “routine bloodwork” at the first prenatal visit. However, although first trimester ID screening allows ample time for antenatal iron supplementation, failing to reevaluate iron stores in the second and/or third trimester misses the periods of highest ID risk, when intravenous iron replacement may be considered.2,3
Nearly one-half of the ferritin tests were ordered by primary care physicians, followed by obstetrician/gynecologists. Without knowing the proportion of overall obstetrical care provided by each specialty, we cannot infer whether one specialty is more likely to screen for ID than another. Nevertheless, primary care providers and obstetricians are likely the optimal targets for interventions to optimize ID screening behaviors in pregnancy.
It is standard of care in Ontario to check a complete blood count (CBC) at the first prenatal visit. Only 75% of women had a baseline CBC, indicating that 1 in 4 patients received substandard care. In some cases, a CBC may have been done before pregnancy in a patient actively attempting to conceive. Nearly 30% of patients with a baseline CBC did not have a subsequent CBC in pregnancy, although our outpatient laboratory data miss hospital blood work done at admission to a labor and delivery ward.
Only 1 in 4 women diagnosed with anemia had a subsequent ferritin test to confirm ID as a cause, and to risk stratify according to severity. Although some may have been treated empirically with oral iron, hemoglobin concentration is an inaccurate indicator of iron stores.21 Pregnant patients with severe anemia were more likely to have a ferritin check; however, absolute rates of ferritin testing remained suboptimal even with severe anemia.
The median after-tax household income of our cohort (CAD$82 448) was similar to that reported for Ontario families in the 2016 federal census (CAD$85 589) (available at www.statcan.gc.ca). However, compared with census data, our cohort underrepresented patients at both extremes of income; the proportion of patients with less than CAD$40 000 annual household income was 4.7% in our cohort vs 8.4% in the census cohort. Similarly, the proportion of patients with an annual household income greater than CAD$125 000 was 11.02% and 33.6% in our cohort and the census cohort, respectively. Therefore, the effects of income distribution on the overall prevalence of ferritin testing in our cohort is likely to be balanced.
We found that pregnant patients in lower income quintiles have a lower odds of ferritin testing than those in the highest income quintile. It is well-established that ID and IDA are associated with lower socioeconomic status (SES), even in high-income countries.28,29 Furthermore, pregnant patients of lower SES are less likely to receive iron supplementation30 and are more likely to receive peripartum blood transfusions.31 To our knowledge, this is the first study to demonstrate an association between SES and the likelihood of ID screening in pregnancy, and thus highlights an important gap in prenatal care. The harms of screening for ID in pregnancy are minor to nonexistent. In a public health care system, the cost of screening is of relevance but not prohibitive (a single ferritin test costs CAD$2.97).
The suboptimal ID screening practices described in this study are likely a reflection of the heterogeneity in recommendations for ferritin testing from obstetrical and hematologic societies locally and internationally. Briefly, Canadian guidelines recommend therapeutic doses of iron if the ferritin is less than 30 μg/L, but stop short of recommending routine ferritin testing in pregnancy.32 The American Academy of Pediatrics suggests ferritin testing in asymptomatic pregnant patients with anemia,33 and the Institute of Medicine recommends checking hemoglobin and ferritin levels in both the first and second trimesters.34 Australian guidelines recommend ID screening in pregnant women with microcytosis,35 whereas Nordic guidelines consider routine ferritin screening in pregnant women “good clinical practice.”36 UK guidelines suggest that nonanemic women at risk for ID either be treated empirically with oral iron or have a ferritin checked.37
In 2015, the US Preventative Services Task Force reversed its 2006 recommendation in favor of screening pregnant patients for ID, on the basis of “insufficient to assess the balance of benefits and harms of screening for iron deficiency anemia in pregnant women.”38 This decision was informed by a systematic review that highlighted a paucity of high-quality randomized trials demonstrating significant improvements in fetal outcomes in iron-supplemented pregnant patients.39 Among the included studies, there was substantial heterogeneity in iron supplementation doses and adherence rates (ranging from 54% to 98%). However, a meta-analysis of 5 of the included studies demonstrated a significant decrease in rates of maternal IDA at term among iron-supplemented patients (relative risk 0.29; 95% CI, 0.17-0.49), an undeniably positive outcome given evidence that such patients are less likely to received peripartum red cell transfusions.18 The conclusions of the US Preventative Services Task Force have therefore been met with skepticism.5
There are important limitations to this study. First, in using outpatient laboratory testing to define pregnancy, our cohort excludes patients referred to a hospital-based obstetrical practice, those with laboratory testing at other community laboratories, those who delivered before the GBS vaginal swab, those who had fragmented care, miscarried, or terminated their pregnancies. Our laboratory definition identifies patients who received prenatal care largely consistent with provincial standards, and may therefore poorly represent marginalized patients and overestimate the prevalence of ID screening in the general population. We used ferritin testing as the sole indicator of ID screening, although the addition of a transferrin saturation would have increased sensitivity. Our data are lacking pertinent demographic variables, including ethnicity and education. Last, in using laboratory data only, we were unable to identify women treated empirically with iron therapy.
In conclusion, among pregnant patients tested at a nonhospital-based Ontario laboratory, ID affected more than one-half of pregnancies, with 1 in 4 complicated by severe ID. Despite this, 40% of pregnant patients were not screened for ID with a ferritin test. The vast majority of ID screening occurred in the first trimester, when the risk is lowest. Anemia affected 8% of pregnancies, yet the underlying etiology was rarely investigated unless severe. Lower annual household income was significantly associated with decreased odds of ferritin testing in pregnancy. These important gaps in care should be addressed by harmonizing obstetrical guidelines to recommend routine ferritin testing in pregnancy, and by highlighting the need for more deliberate testing and management of ID among those of lower SES. Future studies are needed to better understand how social determinants of health influence ID screening and management practices in pregnant patients.
Acknowledgment
The authors thank Craig Upshaw and Peter Catomeris for their generous provision of data from Dynacare and Hina Hanif for her assistance with data extraction.
Authorship
Contribution: J.T., R.N., A.L., and M.S. contributed to study design; R.N. performed data mining and statistical analysis; J.T. wrote the manuscript and generated figures; and M.S., A.L., and R.N. contributed to manuscript revisions.
Conflict-of-interest disclosure: M.S. receives unrestricted research funding and honoraria from Pfizer. A.L. receives unrestricted honoraria from Pfizer and Seaford Pharmaceuticals. The remaining authors declare no competing financial interests.
Correspondence: Jennifer Teichman, Hematology Division, University of Toronto, 700 University Ave, 6th Floor, Toronto, Ontario, Canada, M5G 1X6; e-mail: jennifer.teichman@mail.utoronto.ca.
References
Author notes
Requests for data can be e-mailed to the corresponding author: jennifer.teichman@mail.utoronto.ca.
The full-text version of this article contains a data supplement.